Abstract
Background
The relationship between fecal incontinence (FI) and type 2 diabetes (T2D) has been well recognized, but a comprehensive understanding of this relationship is lacking, taking into account demographic factors and lifestyle variables.
Methods
Using a cross-sectional approach, 13,510 adults aged 20 years and older were identified from the 2005–2010 National Health and Nutrition Examination Survey. Multivariate logistic regression models were used to calculate the adjusted odds ratios (ORs), and further subgroup analyses and propensity score analysis were performed to ensure stable results.
Results
Among 13,510 adults, 11.2% had T2D, and 8.8% had FI. We found a strong T2D-FI link (OR: 1.30; 95% CI: 1.09–1.54, P < 0.001), even after adjusting for covariates. Age > 45 was a critical factor, with a stronger T2D-FI association. Sedentary behavior (OR: 1.41; 95% CI: 1.15–1.73) in T2D patients were associated with FI.
Conclusions
Our study highlights the significant T2D-FI link in US adults, especially in older T2D patients. Lifestyle changes may reduce FI risk. More research is needed for causality and mechanisms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Fecal incontinence (FI) is characterized by the unexpected loss of liquid, solid, or mucous feces occurring at least once a month, leading to a subjective inability to control bowel movements [1, 2]. Studies since 1995 have highlighted the prevalence of FI in both nursing homes and the community, with a global prevalence of ≤ 7% among community-dwelling adults, significantly impacting their quality of life [3]. In the United States, FI affects 8.39% of non-hospitalized adults, with an estimated annual direct cost of $17,166 per person [4]. Despite its substantial burden, there remains limited understanding of the risk factors for FI and the potential for targeted prevention strategies [3]. Some studies have identified individuals with diabetes as a high-risk group for FI [5]. Currently, one in ten adults has diabetes mellitus, with predictions suggesting that one in three adults will have type 2 diabetes by 2050 [6,7,8].
Previous research has demonstrated that FI is significantly associated with high bowel frequency among women with diabetes [9]. Another prospective study in older women revealed that higher levels of physical activity were linked to a 25% reduction in FI risk [10]. However, there is a lack of studies examining the relationship between type 2 diabetes (T2D) and FI in nationally representative samples. Furthermore, it remains unclear whether this association varies among subgroups based on factors such as age, sex, lifestyle, and common comorbidities. Therefore, this study utilized data from the National Health and Nutrition Examination Survey (NHANES) to investigate the association between T2D and FI, considering factors such as age, comorbidities, body weight, and physical activity consistency, in a representative sample of non-hospitalized adults aged 20 to 85 years. The identification of high-risk subgroups within the T2D population is crucial for targeted preventive interventions.
This study used data from the nation's largest National Health and Nutrition Examination Survey conducted in 2005––2010 because the digestive health questionnaire only included information for these three two-year time periods, all of which came from the official website 1, which is based on NHANES data available to the general public, which included detailed data on demographics, health behaviors, and medical comorbidities, primarily to determine whether T2D was associated with FI reporting. The association between T2D and other known FI-related factors, such as age, comorbidities, body weight, and physical activity consistency, was assessed in a representative sample of non-hospitalized adults aged 20–85 years.
Methods
Data sources and study population
This study utilized data from the National Health and Nutrition Examination Survey (NHANES), a comprehensive survey designed to assess the health and nutritional status of non-institutionalized individuals in the United States. The NHANES employs a multistage stratified probability sampling method to select participants, ensuring representation of the U.S. population across different demographic groups [11, 12].
Data for this analysis were drawn from NHANES surveys conducted between 2005 and 2010, as these cycles included detailed information on demographics, health behaviors, and medical comorbidities. Participants in this study were required to be aged 20 years or older and had completed interviews and evaluations at mobile examination centers (MECs). All participants provided informed consent, and the study was approved by the NCHS Ethics Review Committee. Subjects with missing data on FI, covariates, or T2D status were excluded from the analysis.
FI assessment
Fecal incontinence (FI) was assessed using the Bowel Health Questionnaire, which collected information on any unintentional bowel leakage that occurred within the past month, including episodes of solid stool, gas, liquid, or mucus leaks [13, 14]. Participants reported the frequency of these events, ranging from "never" to "once a day or more." FI was defined as any involuntary mucous, liquid, or solid stool loss occurring within the past 30 days, categorized as either "Yes" or "No" for analysis [15,16,17].
T2D assessment
The presence of type 2 diabetes (T2D) was determined based on self-report questionnaires administered before the physical examination [18]. Participants were classified as having T2D if they reported a prior diagnosis of T2D by a physician, in accordance with the American Diabetes Association criteria [19].
Other covariates
A range of covariates were considered in this study, including age, sex, marital status, race/ethnicity, body mass index (BMI), education level, poverty income ratio (PIR), smoking status, drinking status, and physical activity. BMI was calculated as weight in kilograms divided by height in meters squared, categorized into three groups using thresholds of 25 and 30 kg/m2. Smoking status was categorized as current smokers, former smokers, and never smokers. Participants who had never smoked or had smoked fewer than 100 cigarettes were categorized as "Unknown never smokers." Drinking status was defined based on the reported consumption of 12 or more alcoholic drinks annually, classifying participants as drinkers or non-drinkers.
Additionally, common comorbidities such as liver disease, heart disease, lung disease, hypertension, arthritis, and cancer were assessed using specific questions and dichotomous variables.
Statistical analyses
Descriptive analyses were conducted to summarize participant characteristics. Continuous data were presented as means with standard deviations, while categorical variables were expressed as proportions (%). Chi-square tests and t-tests were used to compare categorical and continuous variables, respectively.
Logistic regression models were employed to examine the association between T2D and FI.The models included both non-adjusted and multivariate-adjusted models, progressively accounting for demographic factors, health behaviors, and comorbidities. Subgroup analyses were performed to assess the stability of the T2D-FI association across different demographic and clinical subgroups.All statistical analyses were performed using R (version http://www.R-project.org) and Free Statistics software (version 1.8), with statistical significance defined as p < 0.05.
We conducted a series of sensitivity analyses to evaluatethe robustness of the findings of the study and how ourconclusions can be affected by applying various asso-ciation inference models. In the sensitivity analysis, weapplied four more association inference models: a doubly robust model adjusting for all covariates, a propen-sity score-based IPW model, a propensity score-basedpatient-matching model, and a logistic regression-basedmultivariate analysis model. The calculated effect sizesand p values from all these models were reported andcompared.This study adhered to STROBE Guidelines of reporting.
Results
Study population
A total of 17,132 adults aged 20 years or older who completed interviews and underwent screening at mobile examination centers (MECs) were initially included in this study. After excluding participants with deficient fecal incontinence (FI) (n = 592) and those with missing covariate data (n = 3,030), a final sample of 13,510 participants was included in the analysis. Figure 1 illustrates the exclusion process.
Illustrates the exclusion process. A total of 17,132 adults aged 20 years or older who completed interviews and underwent screening at mobile examination centers (MECs) were initially included in this study. After excluding participants, a final sample of 13,510 participants was included in the analysis
Baseline characteristics
Table 1 presents the baseline characteristics of the study participants categorized by the presence or absence of type 2 diabetes (T2D). Among the participants, 1,518 individuals (11.2%) reported having T2D. The average age of the study participants was 49.1 years (standard deviation: 18.0), with 6,883 (50.9%) being female. A total of 1,192 participants (8.8%) reported experiencing FI, with 237 (15.6%) of them having T2D, which was significantly higher than the 955 (8.0%) individuals without T2D (P < 0.001). Participants aged over 45 years, of white ethnicity, widowed or separated, physically inactive, and obese had higher rates of T2D and were more likely to have other comorbidities, including high blood pressure, arthritis, heart disease, lung disease, liver disease, and cancer.
Association between T2D and FI
Univariate logistic regression analysis (Table 2) revealed that age, sex, race/ethnicity (non-Hispanic white and non-Hispanic black), living arrangements, overweight status, smoking, comorbidities, diabetes, and other variables were significantly associated with a higher probability of FI (P < 0.05). In contrast, participants who were married, cohabiting, and engaged in high, moderate, or vigorous physical activity had a reduced probability of FI (P < 0.05).
Table 2 displays the results of logistic multivariate regression models examining the association between T2D and FI. In the unadjusted model (Model 1), T2D was strongly associated with an increased risk of FI (odds ratio [OR]: 2.14, 95% confidence interval [CI]: 1.83–2.49, P < 0.001). This association remained significant after adjusting for demographics (Model II), risk behaviors (Model III), and common comorbidities (Model IV), with ORs of 1.54 (95% CI: 1.31–1.80, P < 0.001), 1.58 (95% CI: 1.34–1.85, P < 0.001), and 1.36 (95% CI: 1.15–1.61, P < 0.001), respectively. Even after further adjustment for BMI and physical activity (Model V), the association between T2D and FI remained significant (OR: 1.30, 95% CI: 1.09–1.54, P < 0.001).
Sensitivity analyses of association between T2D and FI
For the sensitivity analysis, as summarized in Table 3, all six estimation models (propensity score adjusted [PSA], propensity score matching [PSM], the inverse probability of treatment weighting [IPTW], the standardized mortality ratio weighting [SMRW], pairwise algorithmic [PA], overlap weight [OW]) led to the same conclusion: patients who had T2D had higher fecal incontinence risk (OR range 1.28 to 1.43, all P value < 0.005).
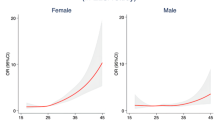
The subgroup analysis of the data is shown in Fig. 2. No statistically significant interactions were observed in the subgroup analyses according to age, Gender,BMI and physical activity (all P > 0.05). In two subgroups of subjects aged 45 years and older, T2D was significantly associated with FI, with an odds ratio (OR) and a 95% CI of 1.37(1.06–1.77) and 1.26(1.0–1.59), respectively. In the Gender,BMI and physical activity subgroups, no association was shown between T2D participants and FI in men, BMI < 25, and moderate and vigorous exercise subgroups.
Association between Type 2 diabetes and fecal incontinence. Subgroup analysis (Fig. 2) did not reveal statistically significant interactions based on age, BMI, physical activity, or smoking status (all P > 0.05). Notes: Adjusted for age, sex, race/ethnicity, marital status, education level, Family PIR, smoking status, alcohol consumption,, liver disease,heart disease, pulmonary disease, hypertension, arthritis and cancer
Discussion
This comprehensive study unveils several crucial facets of the relationship between type 2 diabetes (T2D) and fecal incontinence (FI) within a large and nationally representative cohort of American adults. Our findings carry significant implications for both clinical practice and the direction of future research.
Our study reaffirms and strengthens the well-established link between T2D and FI. Notably, this association remains substantial even after meticulous adjustments for various demographic variables, lifestyle factors, and with common comorbidities [20,21,22]. Specifically, our results indicate that T2D participants are associated an increased risk of FI (OR, 1.30; 95% CI: 1.09–1.54, P < 0.001). This robust connection underscores the clinical relevance of T2D as a meaningful risk factor for FI, suggesting that healthcare providers should integrate FI assessments as part of routine care for individuals with T2D.
One of our noteworthy observations is the significant interaction between age and the T2D-FI relationship. Individuals aged 45 years and older exhibit a particularly strong association between T2D and FI, with an odds ratio (OR) and a 95% CI of 1.37(1.06–1.77) and 1.26(1.0–1.59), respectively.This finding underscores age as a critical modifier in this relationship. The increased vulnerability to FI among older adults with T2D emphasizes the need for targeted screening and intervention efforts within this demographic. Age-related changes in pelvic floor muscles and other factors may contribute to the heightened susceptibility to FI in this age group [22,23,24,25].
Our study provides valuable insights into the role of lifestyle factors in shaping the T2D-FI connection. Sedentary behavior emerges as a potent risk factor for FI in individuals with T2D, with an OR and 95% CI of 1.41(1.15–1.73, P = 0.001). Encouraging T2D patients to adopt a physically active lifestyle may prove instrumental in mitigating the risk of FI.
Although previous studies have yielded varied results regarding the relationship between Body Mass Index (BMI) and Fecal Incontinence (FI), our study introduces new insights. We found that in the population with Type 2 Diabetes (T2D), participants with a BMI lower than 25 were not associated with FI (OR: 1.29, 95% CI: 0.82–2.01, P < 0.001). This lack of association in the T2D population with FI might be due to the lower incidence of diabetes among individuals with low body weight. While the mechanisms behind obesity predisposing individuals to FI are not entirely clear, obesity is a risk factor for diarrhea and accelerated colonic transit, possibly related to increased intra-abdominal pressure (which can damage the pelvic floor) and rectal pressures [23, 26, 27]. It is noteworthy that our study results demonstrate a strong association between FI and overweight and obese individuals within the T2D population [10, 17, 28] and suggests that patients with T2D and FI might benefit from modifying lifestyle factors such as exercise and reducing BMI, and further research is needed to understand the benefits of life style in improving patients with T2D and FI.In this study, we reported 8.8% participants suffering from fecal incontinence in T2D, which may be underreported in general population. FI should be screened in people with other chronic disease, not only in T2D.
Strengths and limitations
This study's strengths lie in its extensive, nationally representative dataset and the meticulous consideration of various covariates. By examining the T2D-FI relationship across diverse demographic and clinical subgroups, we provide a nuanced understanding of this connection. Nevertheless, our study is not without limitations, inherent to cross-sectional analyses, such as the inability to establish causation and susceptibility to reverse causality. Furthermore, the reliance on data from over a decade ago and self-reported medical conditions introduces potential reporting bias.
Clinical implications
The findings from this study carry essential implications for clinical practice. Healthcare providers should recognize the heightened risk of FI in individuals with T2D and incorporate FI assessments into routine evaluations, particularly for those aged 45 years and older. Encouraging lifestyle modifications, including increased physical activity and losing weight, can be pivotal for reducing FI risk in T2D patients, ultimately enhancing their quality of life.
Future research directions
Prospective research endeavors are warranted to elucidate causality and delve into the underlying mechanisms governing the T2D-FI relationship. Furthermore, investigations into the effectiveness of lifestyle interventions, such as structured exercise programs, in mitigating FI risk among T2D patients are of paramount importance. Longitudinal studies that account for dynamic changes in T2D management and comorbidities over time can provide a more nuanced understanding of FI risk factors in this population.
Conclusion
Our study reinforces the substantial connection between T2D and FI while shedding light on the role of age, lifestyle factors, and BMI in shaping this relationship. These findings underscore the imperative of targeted screening and intervention strategies for FI in T2D patients, particularly among older adults and those with sedentary lifestyles. Lifestyle modifications emerge as promising avenues for reducing FI risk among individuals grappling with both T2D and its associated complications, as highlighted by the data-driven correlations we've presented.
Data availability
No datasets were generated or analysed during the current study.
References
Bharucha AE, Knowles CH, Mack I et al (2022) Faecal incontinence in adults. Nat Rev Dis Primers 8(1):53. Published 2022 Aug 10. https://doi.org/10.1038/s41572-022-00381-7
Maeda K, Yamana T, Takao Y et al (2021) Fecal incontinence guideline preparation committee. Japanese practice guidelines for fecal incontinence part 1-definition, epidemiology, etiology, pathophysiology and causes, risk factors, clinical evaluations, and symptomatic scores and qol questionnaire for clinical evaluations-english version. J Anus Rectum Colon 5(1):52–66. https://doi.org/10.23922/jarc.2020-057
Menees SB, Almario CV, Spiegel BMR, Chey WD (2018) Prevalence of and factors associated with fecal incontinence: results from a population-based survey. Gastroenterology 154(6):1672-1681.e3. https://doi.org/10.1053/j.gastro.2018.01.062
Ditah I, Devaki P, Luma HN et al (2014) Prevalence, trends, and risk factors for fecal incontinence in United States adults, 2005–2010. Clin Gastroenterol Hepatol 12(4):636–43.e432. https://doi.org/10.1016/j.cgh.2013.07.020
Townsend MK, Matthews CA, Whitehead WE, Grodstein F (2013) Risk factors for fecal incontinence in older women. Am J Gastroenterol 108(1):113–119. https://doi.org/10.1038/ajg.2012.364
Li R, Zhang P, Barker LE, Chowdhury FM, Zhang X (2010) Cost-effectiveness of interventions to prevent and control diabetes mellitus: a systematic review. Diabetes Care 33(8):1872–1894. https://doi.org/10.2337/dc10-0843
Gregg EW, Boyle JP, Thompson TJ, Barker LE, Albright AL, Williamson DF (2013) Modeling the impact of prevention policies on future diabetes prevalence in the United States: 2010–2030. Popul Health Metr 11(1):18. Published 2013 Sep 18. https://doi.org/10.1186/1478-7954-11-18
Wu Y, Ding Y, Tanaka Y, Zhang W (2014) Risk factors contributing to type 2 diabetes and recent advances in the treatment and prevention. Int J Med Sci 11(11):1185–1200. Published 2014 Sep 6. https://doi.org/10.7150/ijms.10001
De La Luz NM, Wu JM, Matthews C, Whitehead WE, Markland AD (2015) Factors associated with fecal incontinence in a nationally representative sample of diabetic women. Int Urogynecol J 26(10):1483–1488. https://doi.org/10.1007/s00192-015-2730-9
Staller K, Song M, Grodstein F et al (2018) Physical activity, BMI, and risk of fecal incontinence in the Nurses' Health Study. Clin Transl Gastroenterol 9(10):200. Published 2018 Oct 25. https://doi.org/10.1038/s41424-018-0068-6
Zipf G, Chiappa M, Porter KS, Ostchega Y, Lewis BG, Dostal J (2013) National health and nutrition examination survey: plan and operations, 1999–2010. Vital Health Stat 1 (56):1–37
Rockwood TH, Church JM, Fleshman JW et al (1999) Patient and surgeon ranking of the severity of symptoms associated with fecal incontinence: the fecal incontinence severity index. Dis Colon Rectum 42(12):1525–1532. https://doi.org/10.1007/BF02236199
Rockwood TH (2004) Incontinence severity and QOL scales for fecal incontinence. Gastroenterology 126(1 Suppl 1):S106–S113. https://doi.org/10.1053/j.gastro.2003.10.057
Bharucha AE (2003) Fecal incontinence. Gastroenterology 124(6):1672–1685. https://doi.org/10.1016/s0016-5085(03)00329-9
Nelson RL, Furner SE (2005) Risk factors for the development of fecal and urinary incontinence in Wisconsin nursing home residents. Maturitas 52(1):26–31. https://doi.org/10.1016/j.maturitas.2004.12.001
Bordeianou LG, Thorsen AJ, Keller DS et al (2023) The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the management of fecal incontinence. Dis Colon Rectum 66(5):647–661
Whitehead WE, Borrud L, Goode PS et al (2009) Fecal incontinence in US adults: epidemiology and risk factors. Gastroenterology 137(2):512-517.e5172. https://doi.org/10.1053/j.gastro.2009.04.054
American Diabetes Association (2010) Standards of medical care in diabetes--2010 [published correction appears in Diabetes Care. 2010 Mar;33(3):692]. Diabetes Care 33 Suppl 1(Suppl 1):S11-S61. https://doi.org/10.2337/dc10-S011
Huang W, Ma X, Liang H et al (2021) Dietary magnesium intake affects the association between serum vitamin d and type 2 diabetes: a cross-sectional study. Front Nutr 8:763076. Published 2021 Nov 25. https://doi.org/10.3389/fnut.2021.763076
Matthews CA, Whitehead WE, Townsend MK, Grodstein F (2013) Risk factors for urinary, fecal, or dual incontinence in the Nurses’ Health Study. Obstet Gynecol 122(3):539–545. https://doi.org/10.1097/AOG.0b013e31829efbff
Burgio KL, Borello-France D, Richter HE et al (2007) Risk factors for fecal and urinary incontinence after childbirth: the childbirth and pelvic symptoms study. Am J Gastroenterol 102(9):1998–2004. https://doi.org/10.1111/j.1572-0241.2007.01364.x
Scarpello JH, Hodgson E, Howlett HC (1998) Effect of metformin on bile salt circulation and intestinal motility in type 2 diabetes mellitus. Diabet Med 15(8):651–656. https://doi.org/10.1002/(SICI)1096-9136(199808)15:8%3c651::AID-DIA628%3e3.0.CO;2-A
Malloy J, Meloni A, Han J (2013) Efficacy and tolerability of exenatide once weekly versus sitagliptin in patients with type 2 diabetes mellitus: a retrospective analysis of pooled clinical trial data. Postgrad Med 125(3):58–67. https://doi.org/10.3810/pgm.2013.05.2661
Brown HW, Wexner SD, Segall MM, Brezoczky KL, Lukacz ES (2012) Quality of life impact in women with accidental bowel leakage. Int J Clin Pract 66(11):1109–1116. https://doi.org/10.1111/ijcp.12017
Kalantar JS, Howell S, Talley NJ (2002) Prevalence of faecal incontinence and associated risk factors; an underdiagnosed problem in the Australian community? Med J Aust 176(2):54–57
Mitrani C, Chun A, Desautels S, Wald A (1998) Anorectal manometric characteristics in men and women with idiopathic fecal incontinence. J Clin Gastroenterol 26(3):175–178. https://doi.org/10.1097/00004836-199804000-00005
Williams AB, Cheetham MJ, Bartram CI et al (2000) Gender differences in the longitudinal pressure profile of the anal canal related to anatomical structure as demonstrated on three-dimensional anal endosonography. Br J Surg 87(12):1674–1679. https://doi.org/10.1046/j.1365-2168.2000.01581.x
Cichowski SB, Dunivan GC, Rogers RG, Murrietta AM, Komesu YM (2015) Standard compared with mnemonic counseling for fecal incontinence: a randomized controlled trial. Obstet Gynecol 125(5):1063–1070. https://doi.org/10.1097/AOG.0000000000000755
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
Lun-chao LI and Li-Ming LIANG performed all the acquisition of the data. Man WANG helped to interpret the results. Hong-ye JI and Can ZHANG helped to find literature and data when making peer-to-peer revisions to the article. Hong-sheng LIU designed the experiments, analyzed the data, wrote the manuscript and had full responsibility for final content. All authors read and approved the final manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The CDC Institutional Research Ethics Review Committee approved the protocol for the NHANES. The NCHS Ethics Review Committee approved the program, and all participants provided informed consent. This study was not funded by any public, commercial, or nonprofit agency.
Consent for publication
Not applicable.
Approval of the research protocol
The CDC Institutional Research Ethics Review Committee approved the protocol for the NHANES.
Informed consent
The NCHS Ethics Review Committee approved the program, and all participants provided informed consent.
Approval date of registry and the registration no. of the study/trial
Not applicable.
Animal studies
N/A
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
384_2024_4697_MOESM2_ESM.docx
Table 2 Univariate regression analysis of the association between Type 2 diabetes and fecal incontinence. Univariate logistic regression analysis (Table 2) revealed that age, sex, race/ethnicity (non-Hispanic white and non-Hispanic black), living arrangements, overweight status, smoking, comorbidities, diabetes, and other variables were significantly associated with a higher probability of FI (P < 0.05) (DOCX 14 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, Lc., Liang, LM., Ji, Hy. et al. Exploring the association between type 2 diabetes and fecal incontinence in american adults: insights from a large cross-sectional study. Int J Colorectal Dis 39, 121 (2024). https://doi.org/10.1007/s00384-024-04697-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s00384-024-04697-6