Abstract
Acetabular fracture surgery follows the primary aim of anatomic reduction and rigid stable fixation of the fracture. Infraacetabular screws (IAS) allow for an increased stability of the acetabular fixation by closing the periacetabular fixation frame without requiring an additional posterior approach. The osseous screw corridor for infraacetabular screws use the transition zone between the acetabular ring and the obturator ring. The infraacetabular screw corridor (IAC) shows a double-cone shape with an isthmus located near the acetabular fovea. The iliopectineal eminence (IE) is mainly used as a clinical landmark for the intraoperative assessment of the entry point of IAS. The inlet view, the combined obturator oblique outlet view and a 1/3 iliac oblique outlet view may be used for the intraoperative radiological assessment for both the entry point and the screw trajectory of IAS. Several biomechanical studies have shown that IAS increase the stiffness of the internal fixation. Scientific proof for an improved clinical outcome is still missing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Anatomy
Anatomy of the hip bone
From an anatomical point of view, the hip bone (os coxae) may be considered as a ring construction consisting of three rings: (a) an iliac wing ring, (b) an acetabular ring and (c) an obturator ring (Fig. 1 [1]), . The iliac wing ring consists of dense cortical bone with the iliac crest serving as its superior border. This ring surrounds a very thin central bone plate, which is interrupted by the gluteus medius pillar. In some patients an osseous void in this central bone plate posterior to the gluteus medius pillar is observed. Following Wolf´s law from 1870 [2], it is reasonable to assume that there will be an ubiquitous ring structure with a central void in the future of human mankind. The acetabular ring consists of the lunate surface with its surrounding bone, namely the anterior wall, the thicker posterior wall and the superior dome. The ground floor of the central acetabular fossa consists of bone with a thickness of 3–4 mm [3]. This second ring is internally rotated in relation to the iliac wing ring. The obturator ring is the actual ring structure revolving the obturator foramen.
The consideration of the hip bone as a combined ring structure allows for the assessment of osseous screw corridors in acetabular fracture surgery. In general, overlapping zones between two rings represent areas suitable for periacetabular screw fixation. For example, supraacetabular screws use the transition zone between the iliac wing ring and the acetabular ring, while infraacetabular screws (IAS) use the transition zone between the acetabular ring and the obturator ring. The superolateral part of the obturator foramen is therefore part of the infraacetabular screw corridor [4, 5]. Adaequately stable screw fixation within these rings is generally not feasible. Based on these ring considerations, Isler has summarized eight screw corridors suitable for screw fixation of acetabular fractures [6].
The infraacetabular screw corridor (IAC)
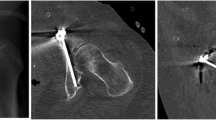
Three potential screw orientations near the quadrilateral surface were described by Letournel in the 1990s (Fig. 2 [5]), . The IAC (Fig. 2, right) is one of them and requires a screw orientation strictly parallel to the quadrilateral plate. The infaacetabular screws (IAS) may be totally embedded in the osseous floor of the acetabular fossa in the presence of a thick bony layer. Otherwise, slight thread penetration in the acetabular fossa without damaging the femoral head or the cartilage of the lunate surface may occur. Bastian described a mean distance between the screw corridor and the femoral head of 5 (1–14) mm at the level of the inferior acetabular fossa [7]. The distance depended on the lateral center edge (LCE) angle in this study. The IAC shows a double-cone shape with an isthmus located near the acetabular fovea (Fig. 3 [8]), . With an increasing diameter of the IAC a more tubular shape of the IAC was observed. The end point is located near the ischial tuberosity. The mean diameter of the IAC at the level of the isthmus was stated between 4.7 mm [9] and 7.4 mm [10]. Sex differences with larger mean diameters in men were also noted [10, 11]. Gras reported that an adequate IAC with a minimum diameter of at least 5 mm was present in 93% of all patients [10]. Zhao found rates of 94% in male and 86% in female indicating gender differences [12]. Kanezaki reported that 21.8% of the IAC in Asian people were not suitable for 3.5 mm IAS due to the anatomical shape of the IAC [13]. Yoshida decribed a rate of 68% of IAC allowing an all-inside screw trajectory [14]. In the other patients, an in-out-in screw trajectory would be feasible only.
The iliopectineal eminence (IE) is mainly used as the anatomical landmark for the intraoperative clinical assessment of the entry point of IAS. Culemann described the entry point to be located 1 cm anterior to the top of the IE in the midline of the upper pubic ramus [4]. Gras decribed the entry point to be located mediocaudal to the IE [10]. Baumann showed that the ideal entry point for the IAS was located 10 mm caudal and 10 mm medial to the iliopectineal eminence (Fig. 4 [15]), . In contrast, Kanezaki stated that the intraoperative clinical assessment of the entry point based on anatomical landmarks such as the iliopectineal eminence is of minor relevance due to the narrowness of the IAC [13]. An intraoperative radiological assessment was therefore recommended by the authors.
Entry-point of the infraacetabular screw approximately 1 cm caudal and 1 cm medial to the iliopectineal eminence (marked in red) according to Baumann [3]
Screw angles for the intraoperative drill bit orientation were reported to be approximately 55° inclination on a lateral view from superoanterior to inferoposterior and 1–2° inclination on an outlet or AP view from superomedial to inferolateral (Fig. 5 [10, 11, 14]), . Slightly higher angles of up to 10° in the outlet or AP view were reported in Asian patients [14, 16].
Maximum screw lengths of IAS were found to be dependent both on the sex and the ethnicity of the patients with smaller screw length in women [14, 16] and in Asian people [12,20,31] compared to Causasians [9]. The mean maximum screw lengths were reported to be between 85 mm and 103 mm [4, 9, 10, 12,13,14, 16, 17].
Radiology
Three radiographic views were recommended by Culemann for the intraoperative assessment of the entry point and the screw trajectory of IAS [18].
-
Inlet view (Fig. 6): The C-arm is tilted 30° cranially. The inlet view allows for the assessment of the entry point of AIS. The entry point (Fig. 6, red dot) should be in the center of the teardrop figure. The teardrop in the inlet view is formed medially by the quadrilateral plate, laterally by the acetabular fossa, and inferiorly by the acetabular notch [19].
-
Combined Obturator Oblique Outlet view (COOO, Fig. 7): The C-arm is rotated approximetaly 40° to the fracture side with an additional 30°-50° caudal tilting of the C-arm. The COOO view allows for the assessment of the intraosseous screw trajectory mainly at the superior border of the obturator ring.
-
1/3 Iliac Oblique Outlet view (1/3 IOO, Fig. 8): The C-arm is rotated approximately 15° to the uninjured side with an additional 30°-50° caudal tilting of the C-arm. The 1/3 IOO allows for the assessment of the extraarticular screw positioning.
Lu confirmed the assessment of the optimal entry point within the teardrop figure in the inlet plane [11]. Other authors, however, recommended different views for the radiological assessment of IAS. Gras, for example, recommended the COOO, a ½ IOO and an AP view of the pelvis [20]. Lim found that the outlet view allowed for the assessment of the screw trajectory in approximately 90° of the cases [19]. In general, Elmhiregh showed that the probabilty of an intraarticular screw trajectory in a concave surface such as the acetabulum is very low, if one particular view shows a distinct extraarticular trajectory [21].
Biomechanics
From a biomechanical point of view, infraacetabular screws should allow for an increased stability of the acetabular fixation by closing the periacetabular fixation frame without requiring an additional posterior approach (Fig. 9). A periacetabular fixation frame consists of a supraacetabular screw, an infraacetabular screw and a suprapectineal plate. Accordingly, several biomechanical studies confirmed this concept.
Culemann performed a biomechanical study using a model of anterior column and posterior hemitransverse (ACPHT) fractures in a single leg stance model [22]. It was shown that a suprapectineal plate combined with long periarticular screws, i.e. supra- and infracetabular screws, showed the highest stiffness by closing the periacetabular fixation frame. These findings were confirmed in a similar study by Spitler in a model simulating a standing position [23] and in a study by Chen [24]. Marintschev performed a biomechanical study applying a model of high anterior column (AC) fractures in a single leg stance model [25]. Different non-locking and locking suprapectineal plates were tested with and without IAS. Additional IAS increased the stiffness of the fixation constructs by up to 50%, while locking plates had no signficant effect. These findings were confirmed in similar biomechanical study by Gras [26]. Graul compared a standard suprapectineal plate with an anatomically pre-shaped suprapectineal plate with integration of an internal posterior column part [27]. The anatomically pre-shaped suprapectineal plate provided higher fixation stiffness than the standard plate. Adding an IAS to the standard plate resulted in comparable stiffness to the preshaped plate, while adding an IAS to this plate did not further increase the stiffness of the construct.
In contrast, Hinz found in a biomechanical study using a model of anterior column and posterior hemitransverse (ACPHT) fractures in a single leg stance model that suprapectineal plate fixation with an additional posterior column screw [28] showed higher fixation stiffness than a suprapectineal plate fixation with an additional IAS [29]. IAS do not cross the transverse posterior hemitransverse fracture, while posterior column screws cross this fracture component nearly perpendicular and may therefore act as lag screws.
Clinics
IAS have gained increasing interest and are used more and more often in the last decade. The available clinical studies, however, mainly focus on the safety of the intraoperative application of IAS using different modalities. Studies showing the additional clinical value of IAS, however, are still missing.
Gras reported in 2012 the use of a 3D navigation system for the insertion of IAS [20]. Cao compared robotic-assisted versus free-hand insertion of IAS. Robotic-assistance resulted in less surgical time (14.4 min vs. 26.3 min). There were, however, no differences in the clinical follow-up [30]. Pagano compared navigation-assisted application versus conventional application of IAS with no clinical differences between the study groups during the follow-up [9].
Conclusion
In conclusion, several biomechanical studies have shown that the additional use of IAS resulted in an increase fixation stiffness in AC and ACPHT fractures by closing the periacetabular fixation frame without requiring an additional posterior approach. Clinical studies, however, mainly focused on the safety of the screw insertion. The scientific evidence for an improved clinical outcome following the use of IAS is still missing.
References
Gänsslen A, Hildebrand F, Klebingat M, Nerlich M, Lindahl J (2018) Acetabular fractures - special screws and views. Thieme, Stuttgart, pp 292–312
Wolff J (1870) Ueber die innere Architectur Der Knochen und ihre Bedeutung für die Frage Vom Knochenwachsthum. Virchows Arch Pathol Anat Physiol 50:389–450
Dienstknecht T, Müller M, Sellei R, Nerklich M, Pfeifer C, Krutsch W, Fuechtmeier B, Berner A (2014) Percutaneous screw placement in acetabular posterior column surgery- gender differences in implant positioning. Injury 45(4):715–720
Culemann U, Marintschev I, Gras F, Pohlemann T (2011) Infra-acetabular corridor - technical tip for an additional screw placement to increase the fixation strength of acetabular fractures. J Trauma 70(1):244–246
Letournel E, Judet R (1993) Fractures of the acetabulum. 2nd edition, Berlin Heidelberg New York: Springer-Verlag
Isler B (1994) Anatomic Considerations for Screw Placement in Acetabular Fractures. Handout AO Pelvic Course, 161. AO/ASIF Pelvic Course Davos, 11.–16. December, 1994
Bastian J, Näf D, Cullmann J, Keel M, Giannoudis P (2021) Does increased acetabular depth affect safe infra–acetabular screw placement in acetabular fracture fixation? Eur J Trauma Emerg Surg 47(5):1319–1326
Arlt S, Noser H, Wienke A, Radetzki F, Hofmann G, Mendel T (2018) Secure corridor for infraacetabular screws in acetabular fracture fixation-a 3-D radiomorphometric analysis of 124 pelvic CT datasets. J Orthop Surg Res 13(1):119
Pagano S, Müller K, Alt V, Maderbacher G, Holzapfel D, Baumann F, Freigang V (2024) Navigiert Oder Konventionell in Der Acetabulumchirurgie. Vergleich Der Positionsgenauigkeit am Beispiel Der infraazetabulären Schraube. Unfallchirurgie 127:44–53
Gras F, Gottschling H, Schroder M, Marintschev I, Reimers N, Burgkart R (2015) Sex-specific differences of the infraacetabular corridor: a biomorphometric CT-based analysis on a database of 523 pelves. Clin Orthop Relat Res 473(1):361–369
Lu Q, Zhou R, Gao S, Liang A, Yang M, Yang H (2021) CT-scan based anatomical study as a guidance for infra-acetabular screw placement. BMC Musculoskelet Disord 22(1):576
Zhao B, Zhang W, Li H, Han L, Han S, Yang X, Yan J, Mu W (2021) The largest secure corridor of the infra-acetabular screw - a 3-D axial perspective analysis. BMC Musculoskelet Disord 22(1):551
Kanezaki S, Miyazaki M, Notani N, Ishihara T, Sakamoto T, Abe T, Kataoka M, Tsumura H (2020) Analysis of computed tomography-based infra-acetabular morphometry to assess the feasibility of infra-acetabular screws. Arch Orthop Trauma Surg 140(3):359–364
Yoshida M, Sato K, Ando T, Haruta M, Iwase H (2020) Analysis of the infra-acetabular corridor: sex-specific differences in the secure area and insertion angle in infra-acetabular screw placement. Fujita Med J 6(2):27–30
Baumann F, Schmitz P, Mahr D, Kerschbaum M, Gänsslen A, Nerlich M (2018) A guideline for placement of an infraacetabular screw based on anatomic landmarks via an intra-pelvic approach. J Orthop Surg Res 13(1):77
Fukuoka S, Yorimitsu M, Uehara T, Naniwa S, Hata T, Sato K, Noda T, Sato, Ozaki T (2024) Ideal insertion point and projection of the infra-acetabular screw in acetabular fracture surgery. Injury 55(6):111264
Lehmann W, Rueger J, Nuechtern J, Grossterlinden L, Kammal M, Hoffmann M (2015) A novel electromagnetic navigation tool for acetabular surgery. Injury 46(Suppl 4):71–74
Chen K, Huang G, Wan Y, Yao, Su Y, Li L, Guo X (2023) Biomechanical study of different fixation constructs for anterior column and posterior hemi-transverse acetabular fractures: a finite element analysis. J Orthop Surg Res 18(1):294
Lim E, Sakong S, Son W, Kim H, Cho J, Oh J (2021) Usefulness of the obturator hook technique for guiding the initial trajectory control in infra-acetabular screw placement. J Orthop Surg (Hong Kong) 29(1):2309499021996838
Gras F, Marintschev I, Klos K, Mückley T, Hofmann G, Kahler D (2012) Screw placement for acetabular fractures: which navigation modality (2-dimensional vs. 3-dimensional) should be used? An experimental study. J Orthop Trauma 26(8):466–473
Elmhiregh A, Hantouly A, Alzoubi O, George B, Ahmadi M, Ahmed G (2024) The optimal fluoroscopic views to rule out intra-articular screw penetration during acetabular fracture fixation. Int Orthop 48(1):243–252
Culemann U, Holstein J, Kohler D, Tzioupis C, Pizanis A, Tosounidis G, Burkhardt M, Pohlemann T (2010) Different stabilisation techniques for typical acetabular fractures in the elderly - a biomechanical assessment. Injury 41(4):405–410
Spitler C, Kiner D, Swafford R, Doty D, Goulet R, Jones L, Hydrick J, Nowotarski P (2017) Generating stability in elderly acetabular fractures - a biomechanical assessment. Injury 48(10):2054–2059
Chen K, Yang F, Yao S, Xiong Z, Sun T, Guo X (2020) Biomechanical comparison of different fixation techniques for typical acetabular fractures in the elderly: the role of special quadrilateral surface buttress plates. J Bone Joint Surg Am 102(14):81
Marintschev I, Gras F, Schwarz C, Pohlemann T, Hofmann G, Culemann U (2012) Biomechanical comparison of different acetabular plate systems and constructs - the role of an infra-acetabular screw placement and use of locking plates. Injury 43:470–474
Gras F, Marintschev I, Schwarz C, Hofmann G, Pohlemann T, Culemann U (2012) Screw- versus plate-fixation strength of acetabular anterior column fractures: a biomechanical study. J Trauma Acute Care Surg 72(6):1664–1670
Graul I, Marintschev I, Pizanis A, Herath S, Pohlemann T, Fritz T (2022) The effect of an infra-acetabular screw for anatomically shaped three-dimensional plate or standard plate designs in acetabulum fractures: a biomechanical analysis. Eur J Trauma Emerg Surg 48(5):3757–3764
Krappinger D, Gänsslen A, Wilde L, Lindtner RA (2024) Acetabular posterior column screws via an anterior approach. Online ahead of print, Arch Orthopedic Trauma Surgery
Hinz N, Baumeister D, Dehoust J, Munch M, Frosch K, Augat P, Hartel MJ (2024) The infraacetabular screw versus the antegrade posterior column screw in acetabulum fractures with posterior column involvement: a biomechanical comparison. Arch Orthop Trauma Surg 144(6):2573–2582
Cao W, Wang Z, Li J, Qi L, Qi H, He P, He J, Liu H, Yi C, Chen H (2024) [A clinical study of HoloSight Orthopaedic Trauma surgery Robot-assisted infra-acetabular screw placement for acetabular fractures]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 38(6):696–702
Funding
Open access funding provided by University of Innsbruck and Medical University of Innsbruck.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No author has a conflict of interest that related to the content discussed in this manuscript. All authors have contributed to and read the paper and have given permission for their names to be included as an author. The manuscript has not already been published and will not be submitted or published simultaneously elsewhere.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gänsslen, A., Lindahl, J., Lindtner, R.A. et al. The infraacetabular screw – anatomy, radiology, biomechanics and clinics. Arch Orthop Trauma Surg (2024). https://doi.org/10.1007/s00402-024-05528-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00402-024-05528-7