Abstract
Purpose
Despite recent advances in the treatment of ovarian cancer (OC), long-term remissions remain scarce. For a targeted approach, prognostic markers are indispensable for predicting survival and treatment response. Given their association with multiple hallmarks of cancer, histamine receptors (HR) are emerging as promising candidates. Here, we investigate their expression pattern and prognostic value in OC.
Methods
Specimens of 156 epithelial OC patients were collected during cytoreductive surgery at the Department of Obstetrics and Gynecology, LMU, between 1990 and 2002 and combined in a tissue microarray. Immunohistochemical staining of the HR H1, H2, H3 and H4 was quantified by an immunoreactive score and linked with clinico-pathological data by Spearman’s correlation. Via ROC curve analysis, optimal cut-off values for potential prognostic markers were defined. Overall survival (OS) was visualized in Kaplan–Maier curves and significances determined by log-rank testing. A Cox regression model was applied for multivariate analysis.
Results
HR H3 and H4 expression was restricted to the cytosol of OC cells, while H1 was also present in the nucleus. A significant association between HR H1, H3 and H4 expression with several clinico-pathological parameters was revealed. In addition, HR H1 and H3 expression correlated positively, HR H4 expression negatively with OS. In addition, HR H3 was identified as independent prognostic marker for OS. HR H2 expression had no prognostic value.
Conclusions
HR H1, H3 and H4 could serve as potential predictors for OS of OC patients. Further research is warranted to elucidate their pathophysiologic role and their predictive and therapeutic potential in OC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ovarian cancer (OC) ranks first in lethality in gynecologic cancers and is the seventh cause of tumor-associated morbidity and mortality among women worldwide (Siegel et al. 2020; Momenimovahed et al. 2019). In the last 20 years, the prevalence and incidence of OC has significantly increased, the latter of which is expected to rise further by about 47% by 2040 (Sung et al. 2021). Due to the relatively late onset of symptoms and a lack of reliable screening methods, OC is often diagnosed in an advanced stage with a risk of relapse of approximately 85% in the first 10 years after diagnosis (Redondo et al. 2021; Czogalla et al. 2019). A dramatic decline in 5 year survival rates from 86% in Fédération Internationale de Gynécologie et d’Obstétrique (FIGO) I to 26% in FIGO IV patients parallels this diagnostic delay (Torre et al. 2018).
Apart from FIGO stage, further prognostic factors include histological subtype, tumor grade, patient’s age at diagnosis and, most importantly, the presence of residual disease following primary debulking surgery (Du Bois et al. 2009; Aletti et al. 2006; Dembo et al. 1990). For several decades, first-line therapy has consisted of cytoreductive surgery prior to an adjuvant platinum-based chemotherapeutic regimen (Mahner and Pfisterer 2013). More recently, targeted therapies comprising, e.g., the anti-vascular endothelial growth factor (VEGF) antibody Bevacizumab or poly-adenosine–diphosphate–ribose–polymerase (PARP) inhibitors were included as maintenance therapies for a subgroup of patients with at least a partial response to platinum-based chemotherapy (Moore et al. 2018; Trillsch et al. 2022). Yet, despite those significant therapeutic advances, 5 year survival rates remain poor with only a modest increase from about 45 to 50% within the past 20 years (Shabir and Gill 2020).
Histamine receptors (HR) increasingly attract attention as they modulate cell proliferation, cell invasion, apoptosis, tumor vascularization and immune response (Nguyen and Cho 2021), which have become known as hallmarks of cancer (Medina and Rivera 2010; Hanahan and Weinberg 2011).
Histamine is a multifunctional endogenous biogenic monoamine, synthesized from the essential amino acid histidine by the enzyme histidine decarboxylase (Nguyen and Cho 2021). It acts as a neurotransmitter in the nervous system or as a local mediator of inflammation. Four G-protein coupled receptor subtypes, the HR H1, H2, H3 and H4, mediate histamine effects through multiple pathways (Parsons and Ganellin 2006).
Depending on various factors, such as the exact tumor entity, histamine concentration, HR exposition, and target cell type, histamine can exert pro- as well as antitumorigenic effects (Blaya et al. 2010; Massari et al. 2020). In cholangiocarcinoma, for example, HR H3 signaling was shown to sustain tumor growth by d-myo-inositol 1,4,5-trisphosphate (IP3)/Ca2+/protein kinase C (PKC)-dependent ERK1/2 dephosphorylation (Francis et al. 2009). In non-small cell lung cancer, on the contrary, it exerts antitumoral effects via the PI3K/Akt/mTOR and MEK/ERK signaling pathway (Zhao et al. 2021).
The context-dependent ambiguity of histamine function is reflected by diverging pre-clinical and clinical observations. In a phase III, multicenter, randomized clinical trial on the addition of histamines to Interleukin-2 based therapies of advance stage melanoma patients, for example, Agarwala et al. 2002) observed an increase in response rates from 20 to 38% and in median survival from 154 to 283 days. In contrast, systemic histamine supplementation in colorectal cancer bearing mice was reported to promote tumor growth (Tomita and Okabe 2005). Consistently, trials on the preoperative treatment of colorectal cancer patients with the HR antagonist famotidine during the week before surgery yielded decreased recurrence rates and an augmented overall survival (OS). These reports further underline the diverging roles of histamines and antihistamines in different cancers (Kapoor et al. 2005).
The effects of HRs on the development and growth of different cancer types are widely acknowledged yet context-dependent. Specifically in the context of epithelian ovarian cancer (EOC), further understanding of their functional role is lacking. Therefore, our work investigates the expression patterns and prognostic relevance of all four currently known HRs in 142 EOC patients.
Materials and methods
Tissue microarray
Tumor specimens of 156 EOC patients were collected during cytoreductive surgery, carried out at the Department of Obstetrics and Gynecology, LMU, between 1990 and 2002. Following histopathological diagnosis confirmation, they were combined in a tissue microarray (TMA). All patients in this study underwent standard therapy for OC. In detail, this consisted of debulking surgery followed by adjuvant therapy. Only patients with pathologically confirmed EOC were included. Corresponding clinical data was gathered from the patients’ charts. Regular follow-up data was obtained by the Munich Cancer Registry.
Following tissue sampling, tumors were formalin-fixed and paraffin-embedded (FFPE). Representative tumor areas were biopsied for assembly in the TMA and their histopathological subtype was assessed by gynecological pathologists at the Department of Pathology at the LMU Munich, Germany. The TMA comprises 110 serous, 21 endometrioid, 13 mucinous and 12 clear cell ovarian cancer specimens, which were graded according to the currently valid World Health Organization classification criteria. Endometrioid tumors were graded from G1 to G3 and mucinous ovarian cancer samples, which currently still lack distinct WHO-approved classification criteria, were graded analogously. Serous ovarian cancer specimens were subdivided into high- and low-grade tumors and clear cell carcinomas automatically classified as G3.
Details on the distribution of selected clinico-pathological characteristics of our TMA-cohort can be found in Table 1.
Immunohistochemistry
For immunohistochemical staining the FFPE tissue microarrays were dewaxed in xylol for 20 min and subsequently washed in 100% ethanol. To avoid unspecific binding of the staining antibodies, tissue sections were blocked in methanol containing 3% H2O2 for 20 min and then carefully rehydrated in serial dilutions of ethanol (100, 70 and 50%) prior to a final washing step in distilled water. Next, the tissue slides were autoclaved for 5 min in sodium citrate buffer (0.1 M citric acid in 0.1 M sodium citrate, pH = 6) and washed twice for 2 min, respectively, in distilled water and phosphate buffered saline (PBS). To avoid unspecific staining reactions, the tissue specimens were incubated in a blocking solution for 5 min at room temperature (RT) prior to a staining step at RT for 16 h with the following primary antibodies: anti-Histamine H1 R Immunoglobulin G (IgG) antibody (GeneTex, Irvine, USA), anti-HR H2 IgG antibody (Abcam, Cambridge, UK), anti-HR H3 IgG antibody (Origene, Rockville, USA) and anti-HR H4 IgG antibody (Origene, Rockville, USA). Following this, the samples were washed twice in PBS and a post-block reagent (Reagent 2, ZytoChem Plus horseradish peroxidase (HRP) Polymer System [mouse/rabbit], Zytomed, Berlin, Germany) was applied for 20 min at RT, followed by another washing cycle in PBS. The slides were, finally, incubated with an HRP-polymer conjugated anti-mouse/anti-rabbit antibody (Reagent 3, ZytoChem Plus HRP Polymer System [mouse/rabbit], Zytomed, Berlin, Germany). After another washing step in PBS, 3’3 diaminobenzidine (DAB) and the corresponding substrate buffer (Liquid DAB and Substrate Chromogen System, DAKO, Munich, Germany) were added to the tissue specimens. The staining reaction was halted by another washing step with distilled water. Mayer’s acidic haemalum (Waldeck, Münster, Germany) was applied for counterstaining. For dehydration, the tissue sections were washed with increasing concentrations of ethanol (first 70, then 96 and 100% ethanol) and, subsequently, with xylol. To ensure staining specificity and as an inherent quality control for the staining reaction, hepatic, colonic and placental tissue served as negative and positive controls, respectively (online resource). As a second method to monitor for unspecific antibody binding, additional tumor sections were stained with the corresponding isotype controls.
Staining evaluation and statistical analysis
On the basis of the immunohistochemical staining, the immunoreactive (IR) score (Remmele and Stegner 1987) was applied for the semi-quantitative assessment of protein expression using a Leitz photomicroscope (Wetzlar, Germany). The percentage of stained cells (with 0: = unstained; 1:= \(\le\) 10%; 2: = 11–50%; 3: = 51–80%; 4\(:= \ge\) 81%) was multiplied with the predominant optical staining intensity (with 0: = no staining intensity; 1: = weak; 2: = moderate; 4: = strong). For each immunohistochemical staining a separate IR score was calculated, taking into account the different distribution patterns of the protein within each cell. Therefore, the score values differ with respect to the cellular compartment assessed, i.e., nucleus and cytoplasm. In order not only to represent the median staining intensity but also its variation within one tissue specimen as realistically as possible, we indicate the statistical data range in brackets in addition to the median IRS using the following format: median IR score (minimum score; maximum score).
Statistical analysis was carried out using International Business Machines Corporation (IBM) Statistical Package for Social Sciences (SPSS) Statistics 28.0 (IBM Corporation, Armonk, New York, USA). Bivariate correlations between protein expression and clinico-pathological patient data were calculated using Spearman’s analysis (Spearman 1987). For visualization of the OS, Kaplan–Meier curves were used. Log-rank testing was performed to check for statistical significance (Dinse and Lagakos 1982). Optimal cut-off values in survival analysis, stratified for the suggested prognostic markers, were estimated via a receiver operating characteristic (ROC) curve analysis, which is deemed a reliable and recognized method for cut-off value definition. By means of the Youden Index, cut-off values were additionally optimized to balance the sensitivity and specificity of the prognostic marker (Youden 1950; Fluss et al. 2005). A Cox regression model of the investigated parameters was employed for multivariate analyses (Cox 1972). Differences between experimental groups were considered statistically significant at a p value of \(\le\) 0.05.
Ethical approval
All tissue samples derive from material collected during cytoreductive surgery and stored in the archives of the Department of Gynecology and Obstetrics, Ludwig–Maximilians-University (LMU), Munich, Germany. Tumor tissue was only cleared for scientific use after the completion of a histopathological assessment and the full anonymization of patient data during all experimental and analytical stages. This study design, in accordance with the guidelines of the Ethics Committee of the LMU, made it possible to waive individual written consent as well as individually signed permission to publish. Ethical approval was granted under the numbers 227–09, 18–392 and 19–972. Moreover, all experiments were carried out in compliance with the standards of the Declaration of Helsinki in 1975.
Results
Histamine receptor expression pattern in epithelial ovarian cancer cells varies between different cellular compartments and correlates with clinico-pathological characteristics
To investigate the prognostic and therapeutic value of the HR subtypes H1–H4 for EOC patients, immunohistochemical staining of all 156 tissue sections of our TMA was examined. HR expression intensity and distribution pattern could be assessed in 142 cases (91%), while 14 tissue samples had to be excluded due to poor tissue quality. The selected patient cohort had a median age of 58.8 ± 12.9 years, ranging from 20.7 to 88.0 years, while their median OS amounted to 60 ± 56.5 months. Immunohistochemistry revealed localization-dependent differences in intracellular HR H1 expression. For cytosolic HR H1, the median (range) IR score amounted to 5 (0; 12) and to 1 (0; 12) for nuclear HR H1. No relevant nuclear expression of the HR H2, H3 and H4 could be detected. The median (range) IR scores for cytosolic HR H2, H3 and H4 reached 5 (2; 12), 7 (0; 12) and 9 (4; 12), respectively (Fig. 1).
Immunohistochemical staining of the histamine receptors H1 (A), H2 (B), H3 (C) and H4 (D). As a positive (negative) control, hepatic (placental) tissue was used for the HR H1 staining, placental tissue for the HR H2 staining and colonic (placental) tissue for the HR H3 and HR H4 staining (online resource)
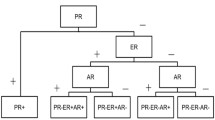
Cut-off values for marker positivity were determined for each HR via ROC-curve analysis and defined as follows (Table 2).
For HR H2 no cut-off value was deemed significant based on Log-rank analysis. A significant correlation of nuclear with cytosolic HR H1 positivity (p = 0.026; Cc = 0.206), just as of cytosolic HR H1 with HR H3 positivity (p = 0.001; Cc = 0.310) was detected. No correlation could be found of HR H2 or H4 expression with any other HR subtype.
In addition, a correlation analysis of HR expression and clinico-pathological features revealed a significant inverse correlation between a positive nuclear HR H1 expression (IRS > 1) and high-grade histology, pathological tumor staging, patient age at diagnosis and FIGO stage. A positive nuclear HR H1 expression, in contrast, directly correlated with a mucinous histopathological subtype. Moreover, a positive cytosolic HR H1 expression (IRS > 6) is significantly correlated with a young age at diagnosis and low-grade histology. Furthermore, a significant positive correlation could be detected between HR H3 expression (IRS > 8) and endometrioid or low-grade serous subtype. Positive cytoplasmatic HR H4 staining (IRS > 6) was positively correlated with a high-grade serous subtype and FIGO stage (Table 3).
Overall survival of epithelial ovarian cancer patients correlates positively with nuclear HR H1 and cytosolic HR H1 and HR H3 staining and inversely with cytosolic HR H4 expression.
To further delineate the prognostic relevance of the HR-expression for the OS of EOC patients, univariate analysis was performed. For a positive nuclear HR H1 staining (median OS = 131.4 months vs. 70.6 months in nuclear HR H1 negative tumors; p = 0.016; Fig. 2A), as well as for a positive cytosolic HR H1 (median OS = 145.5 months vs. 80.6 months; p = 0.007; Fig. 2B), and for a positive HR H3 staining (median OS = 121.2 vs. 75.6 months; p = 0.017; Fig. 2C) we found a significantly prolonged OS as compared to EOC patients with HR scores below the cutoffs. For HR H4 positivity (IRS > 6), we found a significantly reduced median OS of only 80.3 months vs. 125.2 months in the HR H4 negative cohort (p = 0.047; Fig. 2D).
Positive nuclear (A) and cytosolic (B) HR H1 staining as well as positive cytosolic HR H3 (C) staining positively correlate with an increased overall survival. HR H4 positivity, in contrast, is inversely correlated with overall survival (D). Histamine receptor positivity and negativity was defined according to the cutoffs established in Table 2. For statistical analysis a log-rank test was performed. Censoring events were marked in the graphs ( +)
Positive cytosolic HR H3 expression and clinico-pathological parameters are independent prognostic factors for overall survival
For the identification of independent factors prognostic for OS, a multivariate Cox regression analysis was performed (Table 4). Thereby, FIGO state (I, II vs. III, IV; p < 0.001) and histological grading (1 and 2 vs. 3; p = 0.023) were confirmed as independent prognostic factors. In addition, cytosolic HR H3 expression (IRS > 8) could be identified as a novel and statistically independent marker for a reduced OS (p = 0,005). In contrast, this analysis did not yield significant results with regards to the patients’ age at diagnosis, nuclear HR H1 expression and the cytosolic HR H1 and H4 expression (Fig. 3).
Immunohistochemical staining controls: As a positive (negative) control for immunohistochemical analysis, hepatic (A) (placental (B)) tissue was used for the HR H1 staining, placental tissue as both, the positive (C) and negative (D) control for the HR H2 staining and colonic (E) (placental (F)) tissue for the HR H3 staining. For the HR H4 staining, too, colonic (G) and placental (H) tissue were employed.
Discussion
Despite its unequivocal influence on tumor cell proliferation, de-differentiation and immune surveillance, the exact role of histamine and its receptors remains ambiguous. In multiple in vitro studies and clinical trials, histamine was shown to exert either a pro- or an anti-tumorigenic effect. Influencing factors include the exact histamine dose, the respective HR involved, its consecutive signaling pathways, as well as the individual tumor or target cell type (Perz and Ho 2008; Kapoor et al. 2005). Given their controversial roles, further studies will be required to assess the actual diagnostic, prognostic and therapeutic value of HR for oncologic patients. Interestingly, literature on the relevance of HR for EOC patients remains particularly scarce. In 1995, Chanda and Ganguly showed that histamine concentrations were significantly elevated in human ovarian, endometrial and cervical carcinoma compared to their adjacent tissues (Chanda and Ganguly, 1995). In a large population-based study, however, Lacey et al. (2004) postulated that the regular use of HR-antagonists for more than 5 years increases the lifetime risk for ovarian cancer.
Due to the context-dependent ambiguity of earlier HR-data and a lack of further EOC-specific literature, the clinical relevance of the abovementioned findings and especially the prognostic significance of the HR H1 to H4 expression remain largely inconclusive.
In our present analysis we report a positive correlation between high HR H1 expression (IRS > 6 for cytosolic and IRS > 1 for nuclear HR H1 positivity) and prognostic relevant clinico-pathological features, such as FIGO stage, age at diagnosis and recurrence free or overall survival. In addition, the significant correlation of HR H1 expression with mucinous and high-grade serous histology shown in our experiments might serve as a tool to enhance the diagnostic certainty for the histological distinction between high- and low-grade serous subgroups.
In contrast to the newly-established link between HR H1 expression and pathological subtype described here, a functional link between histological grading and HR H1 signaling has already been postulated and is said to trigger tumor growth differently in low- and high-grade OC cells (Batra and Fadeel 1994). In 1994, Batra and Fadeel reported an HR H1-activation dependent rise of intracellular calcium concentration with a subsequent increase in the proliferation of SKOV-3 ovarian cancer cells. Analogous experiments were repeated in the more differentiated OVCAR-3 cell line. In contrast to the SKOV-3 model, calcium ions in OVCAR-3 cells are not exclusively freed from intracellular storage pools, but also derive from the extracellular space through a transmembranous influx into the cancer cells. Additional in vitro experiments will be necessary to further differentiate the exact signaling pathways leading to cell proliferation in response to the activation of certain HR subtypes.
Moreover, histamine receptors, such as HR H1, are not only exposed on the cell surface and expressed in the cytosol but can also be detected in the nucleus. This nuclear HR H1 expression was, much like a positive staining for cytosolic HR H1, significantly associated with an augmented OS. Although the nuclear localization of HRs to date has been poorly investigated, a strong association between HR density on the cell surface and its ability to trigger and regulate certain signaling pathways could be established (Medina and Rivera 2010; Mitsuhashi et al. 1989; Fitzsimons et al. 2002). This might at least partly explain the sometimes-opposing effects of histamines on cancer cell proliferation, depending on the amount of available HR on the cell surface and their consecutive signaling potency. Analogously, in vitro experiments with hepatocellular carcinoma cells showed that, depending on the exact histamine dosage and its subsequent signaling strength, histamine exerts either a pro- or an anti-proliferative effect on tumor cells (Lampiasi et al. 2007).
In consistence with the strong association of cytosolic HR H1 with HR H3 expression, not only HR H1 but also HR H3 positivity (IRS > 8) is significantly correlated with an increased OS. Interestingly, HR H3 has mostly been investigated in the context of certain neurological conditions, such as Alzheimer’s or Parkinson’s, cerebral ischemia or sleep/wake disorders (Nieto-Alamilla et al. 2016; Tiligada et al. 2009; Hu and Chen 2012). Yet, although its signaling cascades, including cAMP formation, calcium accumulation and MAPK pathway stimulation, might be of ubiquitous importance, only little is known about the role of HR H3 in OC (Dimitriadou et al. 1994).
It is of note that, while HR H1 and HR H3 expression mostly seems to be positively correlated with the patients’ survival, a significant negative correlation between HR H4 (IRS > 6) expression and patient survival prevailed in our studies. This finding corresponds with the paradoxical effects of histamines even within one tumor entity. It could at least partly be explained by intercellular differences in the signaling pathways employed by each HR with regard to the wide spectrum of different cell types within the tumor microenvironment.
The tumor microenvironment consists of a complex combination of extracellular matrix and non-transformed cells. The latter include immune cells, stromal cells and endothelial cells, which do not only interact with each other, but also with the tumor cells themselves and vice versa (Nguyen and Cho 2021). Therefore, understanding the impact of the histamine receptor signaling on non-tumorous cells within the tumor microenvironment might also lead to indirect but nevertheless effective anti-cancer strategies (Hirata and Sahai 2017; Quail and Joyce 2013; Lee et al. 2020). In this context, the negative prognostic value of high HR H4 expression as opposed to the positive correlation between high HR H1 and HR H3 expressions and an increased OS might be explicable insofar as HR H4 plays a key role in mast cell chemotaxis and degranulation (Hofstra et al. 2003). Mast cells, in turn, have been reported to exert both a pro- and antitumoral function, depending on the individual tumor type and exact experimental or clinical conditions. For high-grade serous OC patients, Hodeib et al. (2016) demonstrated a strong association between the amount of activated stromal mast cells and a poor OS. This is paralleled by a particularly immunoreactive tumor microenvironment, characterized by an augmented regulatory T cell (Treg) infiltrate and M2 polarized macrophages, which might explain the low response rates to immunotherapeutic treatment approaches in these patients.
In summary, our work confirms the expression of the HR subtypes H1, H2, H3 and H4 in EOC. We could reveal a significant prognostic advantage for patients with HR H1 or H3 positive tumors, as a strong cytosolic and nuclear HR H1 expression as well as a high cytosolic HR H3 expression are associated with a significant survival benefit. In contrast, HR H4 positivity was correlated with decreased OS in our analysis.
However, these findings are, at least to a certain extent, subject to methodological limitations. Our TMA comprises specimens from 156 patients who were diagnosed between 1990 and 2002, thus potentially hindering the analysis of effects induced by recently implemented therapeutic changes. Nevertheless, our cohort, therefore, benefits from a long period for follow-ups. In addition, statistically significant effects observed in our first-line treatment cohort might eventually prove to be fundamental and robust and thus worth further investigation.
Additional studies will be needed to delineate the characteristics of different HR pathways further and might be the base for new OC therapies that rely on a specific modulation of HR signaling. Several HR-antagonists and -agonists have already been approved for clinical use, thus potentially narrowing the gap between bench and bedside. Given that radio sensitizing (Soule et al. 2010) and/or hormone modulating effects (Rossing et al. 2000) of antihistamines have already been established in the past, further in vitro and in vivo experiments are warranted not only to investigate the therapeutic potency of HR modulation, but also to unveil potentially synergistic effects of histamine receptor modulators with other treatment modalities.
References
Agarwala SS, Glaspy J, O’Day SJ, Mitchell M, Gutheil J, Whitman E, Gonzalez R, Hersh E, Feun L, Belt R, Meyskens F, Hellstrand K, Wood D, Kirkwood JM, Gehlsen KR, Naredi P (2002) Results from a randomized phase III study comparing combined treatment with histamine dihydrochloride plus Interleukin-2 versus Interleukin-2 alone in patients with metastatic melanoma. J Clin Oncol 20(1):125–133. https://doi.org/10.1200/JCO.2002.20.1.125
Aletti GD, Gostout BS, Podratz KC, Cliby WA (2006) Ovarian cancer surgical resectability: relative impact of disease, patient status, and surgeon. Gynecol Oncol 100(1):33–37. https://doi.org/10.1016/j.ygyno.2005.07.123
Batra S, Fadeel I (1994) Release of intracellular calcium and stimulation of cell growth by ATP and histamine in human ovarian cancer cells (SKOV-3). Cancer Lett 77(1):57–63. https://doi.org/10.1016/0304-3835(94)90348-4
Blaya B, Nicolau-Galmes F, Jangi SM, Ortega-Martinez I, Alonso-Tejerina E, Burgos-Bretones J, Perez-Yarza G, Asumendi A, Boyano MD (2010) Histamine and histamine receptor antagonists in cancer biology. Inflamm Allergy Drug Targets 9(3):146–157. https://doi.org/10.2174/187152810792231869
Chanda R, Ganguly AK (1995) Diamine-oxidase activity and tissue di- and poly-amine contents of human ovarian, cervical and endometrial carcinoma. Cancer Lett 89(1):23–28. https://doi.org/10.1016/0304-3835(95)90153-1
Cox DR (1972) Regression models and life-tables. J Roy Stat Soc: Ser B (methodol) 34(2):187–202
Czogalla B, Kahaly M, Mayr D, Schmoeckel E, Niesler B, Hester A, Zeder-Goss C, Kolben T, Burges A, Mahner S, Jeschke U, Trillsch F (2019) Correlation of NRF2 and progesterone receptor and its effects on ovarian cancer biology. Cancer Manag Res 11:7673–7684. https://doi.org/10.2147/CMAR.S210004
Dembo AJ, Davy M, Stenwig AE, Berle EJ, Bush RS, Kjorstad K (1990) Prognostic factors in patients with stage I epithelial ovarian cancer. Obstet Gynecol 75(2):263–273
Dimitriadou V, Rouleau A, Dam Trung Tuong M, Newlands GJ, Miller HR, Luffau G, Schwartz JC, Garbarg M (1994) Functional relationship between mast cells and C-sensitive nerve fibres evidenced by histamine H3-receptor modulation in rat lung and spleen. Clin Sci (lond) 87(2):151–163. https://doi.org/10.1042/cs0870151
Dinse GE, Lagakos SW (1982) Nonparametric estimation of lifetime and disease onset distributions from incomplete observations. Biometrics 38(4):921–932
Du Bois A, Reuss A, Pujade-Lauraine E, Harter P, Ray-Coquard I, Pfisterer J (2009) Role of surgical outcome as prognostic factor in advanced epithelial ovarian cancer: a combined exploratory analysis of 3 prospectively randomized phase 3 multicenter trials: by the arbeitsgemeinschaft gynaekologische onkologie studiengruppe ovarialkarzinom (AGO-OVAR) and the groupe d’investigateurs nationaux pour les etudes des cancers de l’ovaire (GINECO). Cancer 115(6):1234–1244. https://doi.org/10.1002/cncr.24149
Fitzsimons C, Engel N, Policastro L, Duran H, Molinari B, Rivera E (2002) Regulation of phospholipase C activation by the number of H(2) receptors during Ca(2+)-induced differentiation of mouse keratinocytes. Biochem Pharmacol 63(10):1785–1796. https://doi.org/10.1016/s0006-2952(02)00975-9
Fluss R, Faraggi D, Reiser B (2005) Estimation of the Youden Index and its associated cutoff point. Biom J 47(4):458–472. https://doi.org/10.1002/bimj.200410135
Francis H, Onori P, Gaudio E, Franchitto A, DeMorrow S, Venter J, Kopriva S, Carpino G, Mancinelli R, White M, Meng F, Vetuschi A, Sferra R, Alpini G (2009) H3 histamine receptor-mediated activation of protein kinase Calpha inhibits the growth of cholangiocarcinoma in vitro and in vivo. Mol Cancer Res 7(10):1704–1713. https://doi.org/10.1158/1541-7786.MCR-09-0261
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144(5):646–674. https://doi.org/10.1016/j.cell.2011.02.013
Hirata E, Sahai E (2017) Tumor microenvironment and differential responses to therapy. Cold Spring Harb Perspect Med. https://doi.org/10.1101/cshperspect.a026781
Hodeib M, Walsh C, Knudsen B, Karlan B (2016) Activated stromal mast cells in high grade serous ovarian cancers (HGSC) are associated with poor overall survival. Gynecol Oncol 143(1):195. https://doi.org/10.1016/j.ygyno.2016.08.243
Hofstra CL, Desai PJ, Thurmond RL, Fung-Leung WP (2003) Histamine H4 receptor mediates chemotaxis and calcium mobilization of mast cells. J Pharmacol Exp Ther 305(3):1212–1221. https://doi.org/10.1124/jpet.102.046581
Hu WW, Chen Z (2012) Role of histamine and its receptors in cerebral ischemia. ACS Chem Neurosci 3(4):238–247. https://doi.org/10.1021/cn200126p
Kapoor S, Pal S, Sahni P, Dattagupta S, Kanti Chattopadhyay T (2005) Effect of pre-operative short course Famotidine on tumor infiltrating lymphocytes in colorectal cancer: a double blind, placebo controlled, prospective randomized study. J Surg Res 129(2):172–175. https://doi.org/10.1016/j.jss.2005.02.030
Lacey JV Jr, Sherman ME, Hartge P, Schatzkin A, Schairer C (2004) Medication use and risk of ovarian carcinoma: a prospective study. Int J Cancer 108(2):281–286. https://doi.org/10.1002/ijc.11538
Lampiasi N, Azzolina A, Montalto G, Cervello M (2007) Histamine and spontaneously released mast cell granules affect the cell growth of human hepatocellular carcinoma cells. Exp Mol Med 39(3):284–294. https://doi.org/10.1038/emm.2007.32
Lee CH, Cho J, Lee K (2020) Tumour regression via integrative regulation of neurological, inflammatory, and hypoxic tumour microenvironment. Biomol Ther (seoul) 28(2):119–130. https://doi.org/10.4062/biomolther.2019.135
Mahner S, Pfisterer J (2013) Towards individualised treatment in ovarian cancer. Lancet Oncol 14(2):101–102. https://doi.org/10.1016/S1470-2045(13)70006-8
Massari NA, Nicoud MB, Medina VA (2020) Histamine receptors and cancer pharmacology: an update. Br J Pharmacol 177(3):516–538. https://doi.org/10.1111/bph.14535
Medina VA, Rivera ES (2010) Histamine receptors and cancer pharmacology. Br J Pharmacol 161(4):755–767. https://doi.org/10.1111/j.1476-5381.2010.00961.x
Mitsuhashi M, Mitsuhashi T, Payan DG (1989) Multiple signaling pathways of histamine H2 receptors Identification of an H2 receptor-dependent Ca2+ mobilization pathway in human HL-60 promyelocytic leukemia cells. J Biol Chem 264(31):18356–18362
Momenimovahed Z, Tiznobaik A, Taheri S, Salehiniya H (2019) Ovarian cancer in the world: epidemiology and risk factors. Int J Womens Health 11:287–299. https://doi.org/10.2147/IJWH.S197604
Moore K, Colombo N, Scambia G, Kim B-G, Oaknin A, Friedlander M, Lisyanskaya A, Floquet A, Leary A, Sonke GS, Gourley C, Banerjee S, Oza A, González-Martín A, Aghajanian C, Bradley W, Mathews C, Liu J, Lowe ES, Bloomfield R, DiSilvestro P (2018) Maintenance olaparib in patients with newly diagnosed advanced ovarian cancer. N Engl J Med 379(26):2495–2505. https://doi.org/10.1056/NEJMoa1810858
Nguyen PL, Cho J (2021) Pathophysiological roles of histamine receptors in cancer progression: implications and perspectives as potential molecular targets. Biomolecules. https://doi.org/10.3390/biom11081232
Nieto-Alamilla G, Marquez-Gomez R, Garcia-Galvez AM, Morales-Figueroa GE, Arias-Montano JA (2016) The histamine H3 receptor: structure, pharmacology, and function. Mol Pharmacol 90(5):649–673. https://doi.org/10.1124/mol.116.104752
Parsons ME, Ganellin CR (2006) Histamine and its receptors. Br J Pharmacol 147(Suppl 1):S127-135. https://doi.org/10.1038/sj.bjp.0706440
Perz JB, Ho AD (2008) Histamine dihydrochloride for the treatment of acute myeloid leukemia, malignant melanoma and renal cell carcinoma. Future Oncol 4(2):169–177. https://doi.org/10.2217/14796694.4.2.169
Quail DF, Joyce JA (2013) Microenvironmental regulation of tumor progression and metastasis. Nat Med 19(11):1423–1437. https://doi.org/10.1038/nm.3394
Redondo A, Guerra E, Manso L, Martin-Lorente C, Martinez-Garcia J, Perez-Fidalgo JA, Varela MQ, Rubio MJ, Barretina-Ginesta MP, Gonzalez-Martin A (2021) SEOM clinical guideline in ovarian cancer (2020). Clin Transl Oncol 23(5):961–968. https://doi.org/10.1007/s12094-020-02545-x
Remmele W, Stegner HE (1987) Recommendation for uniform definition of an immunoreactive score (IRS) for immunohistochemical estrogen receptor detection (ER-ICA) in breast cancer tissue. Pathologe 8(3):138–140
Rossing MA, Scholes D, Cushing-Haugen KL, Voigt LF (2000) Cimetidine use and risk of prostate and breast cancer. Cancer Epidemiol Biomarkers Prev 9(3):319–323
Shabir S, Gill PK (2020) Global scenario on ovarian cancer—Its dynamics, relative survival, treatment, and epidemiology. Adesh Uni J Med Sci Res 2:17–25. https://doi.org/10.25259/aujmsr_16_2019
Siegel RL, Miller KD (2020) Jemal a (2020) cancer statistics. CA Cancer J Clin 70(1):7–30. https://doi.org/10.3322/caac.21590
Soule BP, Simone NL, DeGraff WG, Choudhuri R, Cook JA, Mitchell JB (2010) Loratadine dysregulates cell cycle progression and enhances the effect of radiation in human tumor cell lines. Radiat Oncol 5:8. https://doi.org/10.1186/1748-717X-5-8
Spearman C (1987) The proof and measurement of association between two things. By C. Spearman, 1904. Am J Psychol 100(3–4):441–471
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249. https://doi.org/10.3322/caac.21660
Tiligada E, Zampeli E, Sander K, Stark H (2009) Histamine H3 and H4 receptors as novel drug targets. Expert Opin Investig Drugs 18(10):1519–1531. https://doi.org/10.1517/14728220903188438
Tomita K, Okabe S (2005) Exogenous histamine stimulates colorectal cancer implant growth via immunosuppression in mice. J Pharmacol Sci 97(1):116–123. https://doi.org/10.1254/jphs.fp0040691
Torre LA, Trabert B, DeSantis CE, Miller KD, Samimi G, Runowicz CD, Gaudet MM, Jemal A (2018) Siegel RL (2018) Ovarian cancer statistics. CA Cancer J Clin 68(4):284–296. https://doi.org/10.3322/caac.21456
Trillsch F, Mahner S, Ataseven B, Asher R, Aryal N, Dubot C, Clamp A, Penson RT, Oza A, Amit A, Huzarski T, Casado A, Scambia G, Friedlander M, Colombo N, Fujiwara K, Sonke GS, Denys H, Lowe ES, Lee CK, Pujade-Lauraine E (2022) Efficacy and safety of Olaparib according to age in BRCA1/2-mutated patients with recurrent platinum-sensitive ovarian cancer: analysis of the phase III SOLO2/ENGOT-Ov21 study. Gynecol Oncol 165(1):40–48. https://doi.org/10.1016/j.ygyno.2022.01.024
Youden WJ (1950) Index for rating diagnostic tests. Cancer 3(1):32–35. https://doi.org/10.1002/1097-0142(1950)3:1%3c32::aid-cncr2820030106%3e3.0.co;2-3
Zhao YY, Jia J, Zhang JJ, Xun YP, Xie SJ, Liang JF, Guo HG, Zhu JZ, Ma SL, Zhang SR (2021) Inhibition of histamine receptor H3 suppresses the growth and metastasis of human non-small cell lung cancer cells via inhibiting PI3K/Akt/mTOR and MEK/ERK signaling pathways and blocking EMT. Acta Pharmacol Sin 42(8):1288–1297. https://doi.org/10.1038/s41401-020-00548-6
Funding
Open Access funding enabled and organized by Projekt DEAL. The authors declare that no funds, grants, or other financial support were received to fund this project.
Author information
Authors and Affiliations
Contributions
ED, IH and NET: carried out the experiments and prepared the figures. FBTK: designed the figures and wrote the manuscript. DM, ACR, SB, TK, AB, SM, FT, UJ and BC: supervised the research. All authors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
TK holds stock of Roche AG. AB has received advisory board and honoraria from AstraZeneca, Clovis, Roche and Tesaro. Research support, advisory board, honoraria and travel expenses from AbbVie, AstraZeneca, Clovis, Eisai, GlaxoSmithKline, Medac, MSD, Novartis, Olympus, PharmaMar, Pfizer, Roche, Sensor Kinesis, Teva, Tesaro have been received by SM. FT reports grants and personal fees from AstraZeneca, Clovis, Eisai, Medac, MSD, PharmaMar, Roche, and Tesaro/GSK, outside the submitted work. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki (1975). Approval was granted by the Ethics Committee of the Ludwig-Maximilians-University Munich (approval number 227–09, 18–392 and 19–972).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kraus, F.B.T., Topalov, N.E., Deuster, E. et al. Expression pattern and prognostic potential of histamine receptors in epithelial ovarian cancer. J Cancer Res Clin Oncol 149, 2501–2511 (2023). https://doi.org/10.1007/s00432-022-04114-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-022-04114-x