Abstract
Background
The infectious disease phenotype of acute stroke associated with COVID-19 has been poorly characterized.
Objective
We investigated the neurovascular and infectious disease phenotype of stroke patients with and without COVID-19 infection, and their effect on in-hospital mortality.
Methods
This is a retrospective cohort study of consecutive patients with acute stroke, admitted to any ward of a hub hospital for stroke in Lombardy, Italy, during the first wave of COVID-19. Demographic, neurovascular, infectious disease, and respiratory characteristics were collected. The effect of clinical variables on survival was evaluated using logistic regression models.
Results
One hundred thirty-seven patients with acute stroke were recruited; 30 (21.9%) patients had COVID-19 and represented 2.5% of the 1218 COVID-19 patients hospitalized in the study period. Demographics, comorbidities, stroke type, stroke severity, and etiology did not differ between COVID + stroke patients and non-COVID stroke patients, except for an excess of multi-embolic ischemic stroke in the COVID + group. Most COVID + stroke patients had symptomatic infection (60%) and interstitial pneumonia (70%). COVID + stroke patients required more frequently respiratory support (77% versus 29%; p < 0.0001) and had higher in-hospital mortality (40% versus 12%; p = 0.0005) than non-COVID stroke patients. Mortality was independently associated with symptomatic interstitial pneumonia (aOR 6.7; 95% CI 2.0–22.5; p = 0.002) and, to a lesser extent, with NIHSS on admission (aOR 1.1; 95% CI 1.03–1.2; p = 0.007) and recanalization therapies (aOR 0.2; 95% CI 0.04–0.98; p = 0.046).
Conclusion
Symptomatic interstitial pneumonia was the major driver of in-hospital mortality in COVID + stroke patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Coagulopathy is a well-established feature of SARS-CoV-2 infection and its associated disease, COVID-19 [1]. Nonetheless, the relationship between SARS-CoV-2 infection and acute stroke is still unsettled [2, 3]. Several reports consistently showed a reduction of hospital admission for stroke during COVID-19 pandemic, especially in case of transient ischemic attacks and minor strokes, possibly due to fear of coming to hospital and getting infected [4, 5]. However, other studies reported an increased risk of acute ischemic stroke in patients with SARS-CoV-2 infection [6, 7]. Multi-national registries and pooled data analysis reported increased stroke severity and in-hospital mortality and a high proportion of cryptogenic etiology in COVID-associated stroke [8,9,10].
The infectious disease phenotype of acute stroke associated with COVID-19 has been poorly characterized. Nonetheless, presentations of COVID-19 may critically influence disease course and outcome of COVID + stroke patients.
In this study, we compared the neurovascular and infectious disease features of concurrent acute stroke patients with and without COVID-19 infection, consecutively admitted to a hub hospital for stroke during the first wave of COVID-19 in Lombardy, Italy, and we investigated their effect on in-hospital mortality.
Methods
Study design
This is a retrospective cohort study of consecutive patients with acute cerebrovascular diseases (acute ischemic stroke, intracerebral hemorrhage, transient ischemic attack), admitted to any hospital department (acute stroke unit, general medical wards, COVID wards, intensive care unit [ICU], or COVID-ICU) of San Gerardo Hospital, Monza, Lombardy, Italy, a hub hospital for stroke, during the first COVID wave (February 22 to 10 May 2020; 11 weeks).
To be included in the cohort, patients had to be diagnosed with acute cerebrovascular disease by the attending neurologist based on medical history, physical examination, and neuroimaging. Patients with subarachnoid hemorrhage (n = 15 in the study period) were excluded. Detailed demographic, neurovascular, infectious disease and respiratory characteristics, date of onset of COVID symptoms, date of onset of stroke symptoms, and in-hospital mortality were collected by review of medical records and compared for patients with and without COVID-19 infection.
Study definitions
COVID + cases were defined according to the WHO COVID-19 case definition (December 2020) [11], including both confirmed cases of SARS-CoV-2 infection (positive molecular/antigenic virological test ± clinical and epidemiological criteria) and probable cases of SARS-CoV-2 infection (clinical, radiological, and epidemiological criteria; without molecular/antigenic virological testing).
COVID-related symptoms were defined according the WHO COVID-19 case definition as fever, cough, general weakness, fatigue, headache, myalgia, sore throat, coryza, dyspnea, anorexia, nausea, vomiting, diarrhea, anosmia, ageusia, or altered mental status.
Interstitial pneumonia was defined as typical chest imaging findings suggestive of COVID-19, including hazy opacities with peripheral and lower lung distribution on chest radiography and multiple bilateral ground glass opacities with peripheral and lower lung distribution on chest computed tomography (CT).
Transient ischemic attack (TIA) was defined as a transient episode of neurological dysfunction caused by focal brain, spinal cord, or retinal ischemia, without acute infarction [12].
Cryptogenic stroke was defined as acute ischemic stroke of undetermined cause after performing extracranial and intracranial vascular imaging, transthoracic and transesophageal echocardiography, electrocardiography (ECG), ECG telemetry, and hypercoagulable testing or leading to death before completing diagnostic investigations.
Charlson index was used as a well-established summary comorbidity measure associated with short-term mortality [13].
Statistical analysis
Descriptive statistics were performed for the main demographic and clinical variables. Data were reported as frequencies and percentages for categorical variables, or as medians and interquartile ranges (IQR) for continuous variables. A Kaplan–Meier survival curve was used to describe the probability of occurrence of stroke over time in COVID + patients starting from COVID onset. Selected clinical variables were compared between COVID + and non-COVID patients using the chi-square or the Fisher’s exact test for categorical variables and the Wilcoxon-Mann–Whitney test for continuous variables. Survival probability over time, starting from hospital admission, was compared in COVID + and non-COVID patients using Kaplan–Meier curves and the log-rank test. The effect of selected clinical variables on survival at discharge was evaluated using univariable and multivariable logistic regression models. The choice of variables to be included in both univariable and multivariable analyses was based on clinical reasons. Given the small sample size, we decided to analyze variables that could be considered as potential risk or protective factors for in-hospital mortality in stroke patients. The Hosmer–Lemeshow test was used to evaluate the goodness of fit of the risk prediction model.
The significance level was set at 0.05. Statistical analyses were performed with the SAS statistical package (version 9.4; SAS Institute, Cary, NC, USA). Given the exploratory observational nature of the study, that was based on data collected during the first COVID-19 wave (February 22 to 10 May 2020; 11 weeks), a sample size calculation was not performed, and all consecutive patients complying with the inclusion criteria were recruited.
Results
Study population
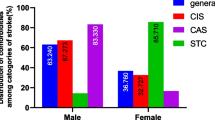
In the study period (11 weeks), 137 consecutive patients with acute cerebrovascular diseases were admitted to hospital: 30 (21.9%) patients had COVID-19 infection and represented 2.5% of the 1218 hospitalized COVID-19 patients. Among COVID + patients, 24 (80%) were confirmed COVID cases and 6 (20%) were probable COVID cases. Acute ischemic stroke was the most common stroke type in both COVID + and non-COVID populations (90% versus 83.2%), with no between-group differences in the overall proportion of stroke types (Table 1). Age (median; range min–max: 73; 39–89 vs 79; 36–92), proportion of men (53.3% versus 52.3%), risk factors, comorbidities, and previous antiplatelet/anticoagulant therapy were not different between COVID + and non-COVID stroke populations (Table 1).
Acute ischemic stroke etiology, severity, and acute treatments
The proportion of acute ischemic lesions in multiple vascular territories (25.9% versus 5.6%; p = 0.0048) was higher in COVID + patients than in non-COVID patients, whereas NIHSS on admission, the proportion of large vessel occlusion and etiology did not differ between the two groups (Table 1). COVID + patients with acute ischemic stroke received less commonly acute recanalization treatments (18.5 versus 38.2; p = 0.019; Table 1).
COVID symptoms and timing between COVID symptoms and stroke
The majority of COVID + stroke patients had symptomatic COVID infection (60%) prior to stroke onset, characterized by fever (56.7%) and less commonly by respiratory symptoms (40%), whereas COVID infection was asymptomatic in 40% of stroke patients (Table 2). The cause of hospital admission was acute stroke in 77% of cases and COVID-related symptoms in 23%. The median time between onset of COVID-related symptoms and stroke was 7 days; stroke onset occurred within the first week of COVID symptom onset in approximately 50% of patients, in the second week in 30%, and between the third and fourth week in < 20% (Fig. 1A).
Infectious disease and respiratory phenotype of stroke patients
On admission, COVID + stroke patients presented the typical COVID-associated alterations of lymphocytes (1210 versus 1700 per mcL; p = 0.015), D-dimer (2030 versus 466 ng/mL; p = 0.006), fibrinogen (510 versus 312 mg/dL; p = 0.003), C-reactive protein (4.13 versus 0.37 mg/dL; p < 0.0001), and lactate dehydrogenase (330 versus 263 U/L; p = 0.045), compared to non-COVID stroke patients (Table 3). Interstitial pneumonia occurred in the majority of COVID + stroke patients (70%), whereas it was absent in non-COVID stroke patients. Deep venous thrombosis and pulmonary embolism were rare complications (< 10%) in both groups. Non-COVID infections, including bacterial pneumonia and urinary tract infections, were more common in non-COVID stroke patients (57% versus 15%; p = 0.0004). Respiratory failure was significantly more common in COVID + stroke patients, compared to non-COVID stroke patients, with need of supplemental oxygen in 77% versus 29% of cases (p < 0.0001; Table 3). Nonetheless, both rate of ICU admission and use of mechanical ventilation did not differ between COVID + and non-COVID stroke patients (13.3% versus 10.3%; 6.7% versus 10.3%, respectively).
Neurovascular and infectious disease determinants of in-hospital mortality
In-hospital mortality was significantly higher in COVID + stroke patients than in non-COVID stroke patients (40% versus 12.2%; p = 0.0005) and in most cases occurred within 7–10 days of admission (Table 3 and Fig. 1B). Multivariable analysis showed that in-hospital mortality was independently associated with symptomatic interstitial pneumonia (adjusted odds ratio: 6.7; 95% CI: 2.0–22.5; p = 0.002) and, to a lesser extent, with NIHSS on admission (adjusted odds ratio for each additional point: 1.1; 95% CI: 1.03–1.2; p = 0.007) and recanalization therapies (adjusted odds ratio: 0.2; 95% CI: 0.04–0.98; p = 0.046). Conversely, age, Charlson comorbidity index, and involvement of multiple vascular territories did not influence in-hospital mortality, after adjustment for confounders (Table 4). The Hosmer–Lemeshow test showed that this risk prediction model was well calibrated, with no evidence of a poor fit (p = 0.7161).
Discussion
Although the causal relationship between COVID-19 and acute stroke is a highly controversial issue [14, 15], multiple studies agree to indicate an excess mortality of COVID + stroke patients compared to non-COVID stroke patients [16, 17].
COVID-related clinical features and respiratory involvement in patients with concomitant stroke and SARS-CoV-2 infection are poorly characterized, despite their potential relevance on neurological outcome. Moreover, most large studies published on this topic are systematic reviews of pooled case series, with an inherent risk of bias in case ascertainment and data collection [18].
In this study, we investigated the neurovascular and infectious disease characteristics of consecutive patients with acute stroke, with and without COVID-19 infection, admitted to a stroke hub during the first COVID wave in Lombardy, Italy, and their effect on in-hospital mortality and cause of death. The COVID + stroke population represented 2.5% of the total COVID-19 population and 22% of the total stroke population admitted to the San Gerardo Hospital in the study period, in agreement with previous studies conducted in areas hit hardest by the pandemic [19, 20]. Our results showed that COVID + stroke patients did not differ from non-COVID ones in terms of pre-stroke status and neurovascular phenotype, even though an apparent excess of ischemic versus hemorrhagic stroke emerged (which was not statistically significant with our sample size). COVID + patients showed a larger proportion of acute ischemic stroke in multiple vascular districts, compared to non-COVID ones. This finding is in agreement with previous reports, suggesting that embolic etiology is prevalent in COVID + patients [21]. However, our results showed a remarkably similar stroke severity, proportion of large vessel occlusion, and cryptogenic etiology in the two groups, in contrast with previous series [8,9,10]. Notably, a lower access to recanalization therapies was observed in COVID + patients with acute ischemic stroke than in non-COVID ones, due to either delayed presentation or longer delay in intra-hospital management of acute stroke. This result is in line with other published cohort studies [22].
Our findings indicate that the majority of COVID + stroke patients had symptomatic COVID-19 infection approximately 1 week before stroke onset and developed interstitial pneumonia associated with respiratory failure in more than three-quarters of cases (resulting in a 2.5-fold increased rate of respiratory failure compared to non-COVID patients). Although COVID + stroke patients developed pneumonia and respiratory failure more frequently than non-COVID ones, admission to ICU was similar in the two groups. Moreover, the use of CPAP in COVID + stroke patients was approximately a half of that reported for non-stroke COVID patients [23].
In accordance with previous studies, our results confirmed an exceedingly higher mortality in COVID + stroke patients (more than a threefold increase) than in non-COVID ones. Furthermore, the strongest driver of mortality was symptomatic COVID pneumonia, which predicted in-hospital mortality independently from well-established stroke-related factors associated with survival, such as stroke severity at presentation [24] and recanalization therapies [25, 26].
Two specific factors contributed to poor outcome in COVID + stroke patients during the first COVID-19 wave: (i) the combination of two serious conditions, i.e., acute stroke and COVID-19 pneumonia, that proved to be life-threatening and required multi-disciplinary management; (ii) a limited access to non-invasive and invasive ventilation of COVID + stroke patients in the setting of saturated hospital capacity.
The study has strengths and limitations. The first strength is the consecutive enrollment of concurrent COVID + and non-COVID patients with acute stroke admitted to any hospital department of a large stroke hub, generating a representative cohort and reducing sampling bias. The second strength is the multi-disciplinary nature of this study, with the contribution of both stroke neurologists and infectious disease specialists that allowed systematic collection of infectious disease and respiratory data not reported in previous works on this topic. The major limitation is the small sample size that leads to a lack of power for detecting some potential associations between risk factors and outcomes that were investigated in this study. Post hoc power calculations for selected outcomes are shown in the Online Resource 1. However, our results are supported by the remarkable consistency with other larger cohorts on the baseline characteristics of the study population. Although further confirmatory studies are required, our findings indicate that the infectious disease phenotype, characterized by a high rate of symptomatic interstitial pneumonia, was the major driver of in-hospital mortality of COVID + stroke patients.
Change history
22 August 2022
Missing Open Access funding information has been added in the Funding Note.
References
Connors JM, Levy JH (2020) COVID-19 and its implications for thrombosis and anticoagulation. Blood 135:2033–2040
Sagris D, Papanikolaou A, Kvernland A, Korompoki E, Frontera JA, Troxel AB et al (2021) COVID-19 and ischemic stroke. Eur J Neurol 28:3826–3836
Stein LK, Mayman NA, Dhamoon MS, Fifi JT (2021) The emerging association between COVID-19 and acute stroke. Trends Neurosci 44:527–537
Uchino K, Kolikonda MK, Brown D, Kovi S, Collins D, Khawaja Z et al (2020) Decline in stroke presentations during COVID-19 surge. Stroke 51:2544–2547
Sacco S, Ricci S, Ornello R, Eusebi P, Petraglia L, Toni D (2020) Reduced admissions for cerebrovascular events during COVID-19 outbreak in Italy. Stroke 51:3746–3750
Katsanos AH, Palaiodimou L, Zand R, Yaghi S, Kamel H, Navi BB et al (2021) The impact of SARS-CoV-2 on stroke epidemiology and care: a meta-analysis. Ann Neurol 89:380–388
Nannoni S, de Groot R, Bell S, Markus HS (2021) Stroke in COVID-19: a systematic review and meta-analysis. Int J Stroke 16:137–149
Ntaios G, Michel P, Georgiopoulos G, Guo Y, Li W, Xiong J et al (2020) Characteristics and outcomes in patients with COVID-19 and acute ischemic stroke: the global COVID-19 stroke registry. Stroke 51:e254-258
Siegler JE, Cardona P, Arenillas JF, Talavera B, Guillen AN, Chavarría-Miranda A et al (2021) Cerebrovascular events and outcomes in hospitalized patients with COVID-19: the SVIN COVID-19 multinational registry. Int J Stroke 16:437–447
Khandelwal P, Al-Mufti F, Tiwari A, Singla A, Dmytriw AA, Piano M et al (2021) Incidence, characteristics and outcomes of large vessel stroke in COVID-19 cohort: an international multicenter study. Neurosurgery 89:E35-41
World Health Organization (WHO) (2020) WHO COVID-19 case definition. https://www.who.int/publications/i/item/WHO-2019-nCoV-Surveillance_Case_Definition-2020.2.
Easton JD, Saver JL, Albers GW, Alberts MJ, Chaturvedi S, Johnston SC (2009) Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. Stroke 40:2276–2293
de Groot V, Beckerman H, Lankhorst GJ, Bouter LM (2003) How to measure comorbidity. A critical review of available methods. J Clin Epidemiol 56:221–229
Siepmann T, Sedghi A, Simon E, Winzer S, Barlinn J, de With K et al (2021) Increased risk of acute stroke among patients with severe COVID-19: a multicenter study and meta-analysis. Eur J Neurol 28:238–247
Bekelis K, Missios S, Ahmad J, Labropoulos N, Schirmer CM, Calnan DR et al (2020) Ischemic stroke occurs less frequently in patients with COVID-19: a multicenter cross-sectional study. Stroke 51:3570–3576
Tan YK, Goh C, Leow AST, Tambyah PA, Ang A, Yap ES et al (2020) COVID-19 and ischemic stroke: a systematic review and meta-summary of the literature. J Thromb Thrombolysis 50:587–595
Dmytriw AA, Dibas M, Schirmer CM, Settecase F, Heran MKS, Efendizade A et al (2021) North American Neurovascular COVID-19 (NAN-C) Consortium. Age and acute ischemic stroke outcome in North American patients with COVID-19. J Am Heart Assoc 10(14):e021046
Delgado-Rodríguez M, Llorca J (2004) Bias J Epidemiol Community Health 58:635–641
Merkler AE, Parikh NS, Mir S, Gupta A, Kamel H, Lin E et al (2020) Risk of ischemic stroke in patients with coronavirus disease 2019 (COVID-19) vs patients with influenza. JAMA Neurol 77:1–7
Pezzini A, Grassi M, Silvestrelli G, Locatelli M, Rifino N, Beretta S et al (2021) SARS-CoV-2 infection and acute ischemic stroke in Lombardy, Italy. J Neurol 24:1–11
Frisullo G, Scala I, Bellavia S, Broccolini A, Brunetti V, Morosetti R et al (2021) COVID-19 and stroke: from the cases to the causes. Rev Neurosci 32:659–669
Fridman S, Bres Bullrich M, Jimenez-Ruiz A, Costantini P, Shah P, Just C et al (2020) Stroke risk, phenotypes, and death in COVID-19: systematic review and newly reported cases. Neurology 95:e3373-3385
Brusasco C, Corradi F, Di Domenico A, Raggi F, Timossi G, Santori G et al (2021) Continuous positive airway pressure in COVID-19 patients with moderate-to-severe respiratory failure. Eur Respir J 57:2002524
Weimar C, Ziegler A, König IR, Diener HC (2002) Predicting functional outcome and survival after acute ischemic stroke. J Neurol 249:888–8895
Katsanos AH, Malhotra K, Goyal N, Palaiodimou L, Schellinger PD, Caso V et al (2019) Mortality risk in acute ischemic stroke patients with large vessel occlusion treated with mechanical thrombectomy. J Am Heart Assoc 8:e014425
Karamchandani RR, Rhoten JB, Strong D, Chang B, Asimos AW (2021) Mortality after large artery occlusion acute ischemic stroke. Sci Rep 11:10033
Funding
Open access funding provided by Università degli Studi di Milano - Bicocca within the CRUI-CARE Agreement. This study was funded by a grant from Lombardy Region as part of the call “Bando per il finanziamento di progetti di ricerca in ambito sanitario connessi all’emergenza del COVID-19” (DGR N. XI/3017, 30.03.2020).
Author information
Authors and Affiliations
Contributions
SB, FI, and EBe designed the study. SB wrote the manuscript with SD and EBi. SB, FI, SD, LD, CE, AR, CMC, PB, and CF acquired, analyzed, and interpreted the data. PB and CF were involved in protocol development, ethical approval, and data interpretation. EBi performed the statistical analysis. All authors critically reviewed the manuscript for intellectual content, approved this version of the paper, and participated sufficiently in the work to take public responsibility for its content.
Corresponding author
Ethics declarations
Ethical approval
The study adheres to the ethical principles of the Declaration of Helsinki as well as GCP guidelines. The study protocol was approved by the Ethics Committee Brianza (#3522 on 10th December 2020). A written informed consent to the use of anonymized data for epidemiological or research purposes was obtained by study participants or a legally responsible person.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Beretta, S., Iannuzzi, F., Diamanti, S. et al. Neurovascular and infectious disease phenotype of acute stroke patients with and without COVID-19. Neurol Sci 43, 4619–4625 (2022). https://doi.org/10.1007/s10072-022-06133-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-022-06133-5