Abstract
This study aimed to investigate the effects of 0.6% hyaluronic acid (HA) gel on the healing process and postoperative pain levels after diode laser-assisted labial frenectomy in pediatric patients. Ninety-six pediatric patients (females, 50 and males, 46) aged 8–14 years were randomly divided into four groups as follows: (1) conventional frenectomy with 0.6% topically administered HA (CFH, n = 24); (2) conventional frenectomy with placebo gel (CFP, n = 24); (3) frenectomy performed by diode laser with 0.6% topically administered HA (DLH, n = 24); and (4) frenectomy performed by diode laser with placebo gel (DLP, n = 24). HA application was continued for 1 week thrice daily after the frenectomy. Visual analog scale forms were collected from patients 1 week after the operation. In addition, the plaque index, gingival index, periodontal probing depth, and keratinized tissue width and thickness were recorded. This process was repeated 1 and 3 months after the first visit. The DLH group revealed significant differences in the probing depth, bleeding on probing, keratinized gingiva width, and attached gingiva width according to dual comparisons of the initial, first, and third-month values (p = 0.010, p = 0.007, p<0.001, and p = 0.001, respectively). Significant differences were observed between the CFP and CFH groups according to the initial and initial third-month values with regard to the bleeding on probing (p=0.019 and p = 0.019, respectively). The attached gingival thickness revealed significant differences between the CFP and CFH groups for the initial and initial-third-month comparisons (p = 0.005 and p = 0.007, respectively). The mean values of the initial and initial-third-month differences were significantly higher in the CFH group than those in the CFP group. HA- and laser-assisted labial frenectomies revealed better outcomes in terms of the probing depth, attached gingiva width, keratinized gingiva width, healing process, and postoperative comfort.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The labial frenulum is an anatomical structure between the maxillary and mandibular central incisors and canine/premolar region. The frenulum is enclosed by a mucosal membrane and comprises fibrous, muscular, and fibromuscular tissues. This formation extends from the alveolar mucosa or attached gingiva to the underlying periosteum [1,2,3]. The labial frenulum attachments can be classified into four main categories according to the attachment level of the muscle fibers: mucosal, gingival, papillary, and papillary-penetrating (Table 1) [4].
Papillary and papillary-penetrating types are identified as pathological when clinically diagnosed. Pathological labial frenulum attachments may lead to plaque accumulation, depending on the difficulty of tooth brushing due to muscle pulling, and may also cause diastema [5, 6]. Furthermore, papillary loss, gingival recession, midline diastema, and, in severe cases, periodontal pocket formation and tooth loss may occur due to the strong pulling of the muscle fibers over time [5]. If plaque control is poor, periodontal tissue loss may be more pronounced, especially in older individuals. High frenulum attachment combined with shallow sulcus may also create difficulties in tooth brushing [1, 7, 8]. In addition, high labial frenulum attachment in children with mixed dentition may cause more complicated problems, such as midline diastema, difficulty maintaining plaque control, and gingival recession [9]. Frenulectomy or frenectomy is recommended during the mixed dentition period, when the permanent teeth first erupt, to facilitate better oral hygiene, close midline diastemas spontaneously, and reduce the risk of caries [7, 8, 10]. It is used to surgically remove high frenulum attachments at the tissue level. Frenulectomy is characterized by a simple incision to release the frenulum attachment. However, frenectomy involves the removal of the entire frenulum, including attachments to the peritoneum and alveolar bone, in the cases having high frenulum [7]. The conventional technique of frenectomy involves using a scalpel [11]. Lasers are frequently used in frenectomy [3, 12]. In recent years, diode lasers have become more popular in frenectomies [2, 13]. In pediatric patients, diode lasers are commonly used for labial and lingual frenectomy because of the associated advantages such as reduced operation time, reduced need for infiltration anesthesia, hemostasis, and elimination of the need for suturing [2, 8]. The portability, ease of the setup process, and low price among the currently available lasers are other advantages of diode lasers [12].
In recent years, hyaluronic acid (HA) has been applied as an adjunct to oral soft tissues to enhance the healing process [4, 14, 15]. HA is a non-sulfated polysaccharide component of the glycosaminoglycans family. It is a high-molecular-weight polymer in various body fluids, such as synovial fluid, saliva, gingival crevicular fluid, and serum. HA is a significant component of the synovial joints, extracellular matrix of the skin, connective tissue, and various other tissues [16].
HA has bacteriostatic, fungistatic, anti-inflammatory, anti-edematous, and pro-angiogenetic effects on tissues. These properties suggest that HA may enhance wound healing in oral soft tissues, such as in the healing process following frenectomy operations [14, 16, 17]. Additionally, HA reduces plaque and sulcus bleeding indices in patients with gingivitis [18].
To the best of our knowledge, no previous studies assessed the advantages of the use of HA compared to control in laser and conventional frenectomy operations in pediatric patients. Accordingly, this study aimed at examining the effects of frenectomy and HA on clinical periodontal parameters. The primary purpose of this study was to evaluate the effects of HA on the healing process following different frenectomy methods using visual analog scale (VAS) scores and periodontal clinical parameters.
Materials and methods
This study was a prospective, examiner-blind, randomized, and controlled clinical trial. The local ethics committee approved the study protocol (Approval 2019/220). The clinical phases of the study were performed at the Department of the Periodontology Clinic between August 2019 and May 2021. The conducted research followed the ethical principles outlined in the Declaration of Helsinki. G-Power (version 3.1; Informer Tech Inc., Germany) was used to determine the number of research participants [19]. It was determined that each group must have a minimum of 16 individuals to achieve 95% power at a 5% significance level. To accommodate potential dropouts and non-compliance, 96 participants were recruited. The randomization sequence was generated using an online computer-based tool (www.random.org). The allocation of participants was independently conducted by individuals designated as OD, ensuring the concealment of allocation. Ninety-six pediatric patients (females, 50 and males, 46) aged 8–14 years were randomly divided into four groups: (1) conventional labial frenectomy with 0.6% topically administered HA (CFH, n = 24); (2) conventional labial frenectomy with placebo gel (CFP, n = 24); (3) labial frenectomy performed by diode laser with 0.6% topically administered HA (DLH, n = 24); and (4) labial frenectomy performed by diode laser with placebo gel (n = 24; Fig. 1).
Systemically healthy and non-medicated individuals (for at least 6 months) with gingival (n = 31; 32.29%), papillary (n = 39; 40.62%), and papillary penetrating (n = 26; 27.08%) labial frenulum attachments were included in the study. The parents signed a written informed consent form for their children’s participation in this study, and the children were given a brief description of the process. The study included frenectomy treatments performed by researchers SSAD and CA. The researchers performed frenectomy treatments on the children without knowing which group they belonged to (placebo or HA). Another researcher, other than the surgeon, performed control and postoperative measurements for each patient.
All the patients underwent dental treatment and initial periodontal therapy and followed the oral hygiene instructions. Before the labial frenectomy procedure, 10% lidocaine was topically applied to all the patients to reduce the pain before administering local anesthesia (Avixa İlaç San. Tic Ltd. Şti., Başakşehir, İstanbul, Turkey). Local infiltration anesthesia with 4% articaine, including epinephrine (epinephrine:articaine, 1:100,000), was applied to the vestibular oral mucosa and right and left regions of the frenulum (Ultracaine D-S Fort Ampul, Avixa İlaç San. Başakşehir, İstanbul, Turkey). The usage protocol for the diode laser was initiated after a waiting time of around 10 min.
The diode laser used in this study was the BIOLASE Epic10™ (BIOLASE INC., CA, USA). The laser interface was set to the “Frenectomy” mode. The features of the frenectomy mode are shown in Table 1. Frenectomy was performed using a 940-nm indium gallium arsenide phosphide (InGaAsP) semiconductor diode laser. The laser was operated in pulseCP2 wave mode at a power of 1.0 watt (W), and a 400-μm diameter optical fiber tip was used (Fig. 2). After the patient and operator wore protective glasses, the environmental safety measures were taken before carrying out the frenectomy procedure following the guidelines in Table 2.
Using brushing movements, the laser was applied to the upper and lower parts of the frenulum near the hemostat. Moreover, the remaining muscular attachments of the periosteum were removed to eliminate the periosteal adhesion. The remaining ablated tissue was cleared using a moistened gauze with a sterile saline solution [2, 13]. The average time taken for the procedure with the diode laser was 60 s. After the surgical procedure, the participants were instructed on how to apply the HA gel. The patients in the 0.6% HA group were given seven blister disposable packages containing 0.6% HA (Aftamed Shield Gel, Aktident, Üsküdar, İstanbul, TURKEY). The participants in the HA group were instructed to apply HA Gel to the wound area thrice a day for 1 min after opening a new blister pack and refrain from eating or drinking for 10–15 min [4] (Fig. 2).
In conventional techniques, the upper lip is extended, and a straight hemostat is attached to the frenulum into the depth of the vestibular fold. Triangular-shaped incisions were made above and below the hemostat using a no. 15 scalpel (HM0240, Beybi, Ümraniye, İstanbul, Turkey) until the labial frenulum was released from the soft tissue. Muscle fiber dissection was performed on the submucosa of the lateral walls after excision of the frenulum with curved forceps to detach them from the periosteum. A 4/0 silk suture was used for primary wound closure (DOGSAN, Beşiktaş, İstanbul, Turkey). After surgical frenectomy was performed, the patients and their parents were advised to be cautious and avoid the exposure to mechanical trauma, flossing, and chewing movements. Gentle tooth brushing was permitted using a surgical toothbrush (Surgical Mega Soft, Curaprox, Kriens, Switzerland). The interrupted sutures were removed 1 week after surgery [1, 2, 13] (Fig. 3).
The Silness–Löe plaque index (PI), gingival index (GI), pocket depth (PD), bleeding on probing (BOP), keratinized gingival width (KGW), attached gingival width (AGW), and attached gingival thickness (AGT) were measured using a Williams periodontal sond (122-006, HuFriedy, Chic, IL, USA). They were recorded prior to the labial frenectomy operations and at 1 and 3 months after the operations [2, 13].
The VAS was used to evaluate the pain and discomfort levels of the patients, with scores between 0 and 10, where the score of “0” indicated no pain and discomfort and the score of “10” indicated severe pain and discomfort. The participants were requested to complete the questionnaire once daily for 1 week following the operation [2, 4, 13, 20].
Statistical analyses were performed using SPSS for Windows software package (version 20.0). For descriptive statistics, the mean ± standard deviation and median (minimum–maximum) were used for the quantitative variables, while the number of patients (percentage) was used for the qualitative variables. To determine whether there was a difference between the two categories of the qualitative and quantitative variables, Mann-Whitney U test was used as the normal distribution hypothesis was not provided. Repeated-measures analysis of variance (ANOVA) and two-way repeated-measures analysis of variance were used to examine the change in variables with repeated measures over time and between groups. A significance level of 0.05 was set for statistical analyses.
Results
A total of 74 (77.08%) pediatric patients out of the 96 enrolled patients completed this study. Thus, 22 patients were excluded. One child did not correctly complete the VAS, another child did not use the placebo gel, and a third child missed the control appointment. Six children from the CFH group were excluded, where three children did not correctly use the 0.6% HA gel, two did not complete the VAS, and one missed the appointment. Seven children from the DFP group were excluded, where seven participants were excluded due to improper use of the placebo gel and two were excluded for incorrectly filling out the VAS. Six children were excluded from the DFH group, where three children were excluded due to improper use of HA, two did not appropriately fill out the VAS, and one missed the control appointment.
Periodontal parameter assessments
In the CFP group, no significant differences were observed according to the dual comparisons of the measurements of the initial, first, and third months when all the variables were compared (p>0.05). There were significant differences in the CFH group for BOP between the values of the initial, first, and third months when dual comparisons were performed (p<0.001). According to the dual comparisons in the CFH group, the initial-first, initial-third, and first-third month comparisons showed significant differences (p = 0.004, p = 0.001, and p = 0.012, respectively; Table 3).
The DLP group did not show significant differences in the variables when dual comparisons of the initial, first, and third months were performed (p>0.05). However, in the DLH group, significant differences were observed in the PD, BOP, KGW, and AGW according to the dual comparisons of the values of the initial, first, and third months (p = 0.010, p = 0.007, p<0.001, and p = 0.001, respectively). Dual comparisons of the probing depth values displayed significant differences between the first and third months (p = 0.028). The BOP value was significantly different between the initial and first months only (p = 0.011). The KGW values were significantly different between the initial-first and initial-third months (p = 0.034 and p = 0.030, respectively). Dual-time comparisons of the AGW values revealed significant differences between the initial and first months (p = 0.002; Table 4).
Significant differences were observed in the BOP values between the CFP and CFH groups according to the initial-first and initial-third months (p = 0.019 and p = 0.019, respectively). The CFP and CFH groups revealed differences in the mean values ( ± SD) of 0.00 ± 0.23 and 0.23 ± 0.57, respectively, of the initial-first month. Moreover, the CFP and CFH groups revealed differences in the mean values ( ± SD) of 0.03 ± 0.28 and 0.34 ± 0.78, respectively, of the initial-first month. The KGW values of initial-first month were significantly different between the CFP and CFH groups (p = 0.017). The CFP and CFH groups revealed differences in the mean values ( ± SD) of −0.03 ± 1.26 and −0.06 ± 0.41, respectively, of the initial-first month (Table 5).
The AGW was significantly different between the CFP and CFH groups in the initial-first month (p = 0.031). The mean value of the initial-first month difference in the CFP group was significantly higher than that in the CFH group (Table 5).
The AGT values revealed significant differences between the CFP and CFH groups for the initial-first and initial-third month comparisons (p = 0.005 and p = 0.007, respectively). The differences in the mean values of the initial-first and initial-third months were significantly higher in the CFH group than those in the CFP group (Table 5).
Significant differences between the DLP and DLH groups were observed only for the PD according to the comparisons of the initial-third and first-third months (p = 0.029 and p = 0.029, respectively). The differences in the mean values (±SD) of the initial-third month in the DLP and DLH groups were 0.07 ± 0.38 and −0.19 ± 0.59, respectively. The difference in the mean value of the first-third month was significantly higher in the DLP group than that in the DLH group (Table 6).
Only the KGW parameter showed a significant difference between the CFP and DLP groups in the first month (p = 0.016). The initial-first month difference for KGW was −0.03±1.26 in the CFP group and −0.11±0.28 in the DLP group (Table 7).
The difference in PD between the CFH and DLH groups was significantly higher in the initial-third month than that in the CFH group (p = 0.002). There was a difference in the probing depth between the CFH and DLH groups, with average values of 0.06±0.38 and −0.22±0.60, respectively, during the first-third month. The difference in BOP between the CFH and DLH groups was significant during the first 3 months (p = 0.003). While the CFH group had a difference in the average value for BOP in the first-third month of 0.11±0.32, the mean value for the DLH group was −0.04±0.19. The CFH and DLH groups showed a significant difference in KGW in the initial-first month (p = 0.034). The KGW value showed a difference of −0.06±0.41 in the CFH group and −0.22±0.42 in the DLH group during the initial-first month (Table 8).
Although time comparisons did not show a significant difference between the CFH and DLH groups, the CFH group exhibited worse PI, GI, PD, and BOP values. The treatment did not cause any significant changes in the KGW, ATW, or AGT values. Using HA reduces periodontal inflammation in diode laser-assisted frenectomy procedures, especially within the first month, where the patients showed increased attention to plaque cleaning, especially in the DLH group, when evaluating the time-dependent differences. The use of diode laser and HA gel had a positive impact on PI, GI, PD, BOP, KGW, and AGW values, particularly in the first month.
VAS results
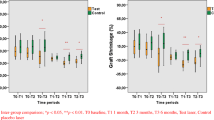
VAS data showed significant differences in the CFP group between days 1–7 (p<0.001) and 2–7 (p<0.001). Additionally, there was a significant difference between days 2–4 (p = 0.007), 2–5 (p<0.001), and 2–6 (p = 0.001; Fig. 4).
Significant differences were observed in the CFH group between various pairs of days, including the 1st–7th (p<0.001), 2nd–7th (p<0.001), and 4th–7th days (p<0.001; Fig. 4).
There were significant differences in the DLP group between several days (1st–2nd, 1st–3rd, 1st–4th, 1st–5th, 1st–6th, 1st–7th, 2nd–4th, 2nd–5th, 2nd–6th, 2nd–7th, 3rd–6th, and 3rd–7th; all p<0.005; Fig. 5) The DLH group showed significant differences between days 1–7, with the most significant differences observed between days 1–5 and 3–7 (all p<0.005; Fig. 5).
The study analyzed the changes in the VAS measurements between the paired groups over time. There was no significant change between the CFP and CFH groups (p = 0.183). At each time, the VAS values of the CFH method were on average 0.08 units higher than those of the CFP method. There was a significant difference between the two groups only in the VAS value on day 4 (p = 0.041). No significant difference was observed between the DLP and DLH groups at all the time points (p = 0.088). The VAS values of the DLH method were on average 0.12 units higher than those of the DLP method at all the time points. There was no significant difference in the VAS values between the two groups at all the time points (p>0.05). No significant differences were observed between the CFP and DLP groups at all the time points (p = 0.231). The VAS values were consistently 0.07 units higher with the CFP method than those with the DLP method. There was no significant difference in the VAS values between the two groups at all the time points (p>0.05). There was a significant difference in the rate of change over time between the CFH and DLH groups (p = 0.009). The two groups showed different trends in the increase or decrease of VAS over time. The VAS values of the CFH method were consistently 0.03 units higher than those of the DLH method. There was no significant difference in the VAS values between the two groups at all the time points (p>0.05; Figs. 1 and 2).
It is understood that using HA gel can reduce pain levels by suppressing inflammation, particularly on the first day. However, it was determined that inflammation was suppressed from the 4th day onwards, and the pain level was less. However, the same situation is not valid for days 2 and 3.
Discussion
The labial frenulum abnormalities may cause midline diastema, gingival recession, and speech problems depending on the size and location of the frenulum [9]. Excision of the labial frenulum attachment is occasionally required in patients at the mixed-dentition stage to eliminate the incidence of these abnormalities [10]. The primary purpose of frenectomy is to minimize the tension of the soft tissue attachment to the underlying alveolar bone by excising the collagen fibers. Scalpels are commonly used to remove soft tissues using conventional techniques [13]. However, conventional techniques can cause postoperative pain and discomfort [7]. Laser-assisted frenectomy is a suitable alternative method for reducing the postoperative discomfort experienced by the patients [4].
Furthermore, laser-assisted surgery eliminates bleeding and the need for suturing [1, 6]. Previous studies reported that laser-assisted frenectomy yielded better outcomes than those of the scalpel technique for postoperative pain and functional complications [1, 13, 21]. In contrast, no significant differences were observed between the Nd-YAG laser and conventional frenectomy groups regarding postoperative pain or oral functions [3, 21]. The VAS, which is commonly used to evaluate the levels of pain and discomfort, is a reliable method that can be easily performed by patients and researchers [1, 21]. Recently, diode lasers have exhibited better outcomes than CO2 lasers for wound healing, clinical attachment level, gingival recession improvement, and postoperative comfort in labial frenectomy [12]. The diode laser has a superior advantage in terms of not interacting with hard tissues [22].
Furthermore, diode lasers reduce the need for infiltration anesthesia and, consequently, reduce anxiety in pediatric patients [8]. In this study, the pain levels were reduced in all the groups over time, but no significant differences were observed. As predicted, the most evident differences were observed after the first day.
The HA concentration in the commercially available products containing high molecular weight HA is in the range of 0.2–0.8% [16, 18]. The concentration, treatment protocol, and frequency may have affected the different clinical results reported in the previous studies [23]. Significant pain reduction was observed in a study in which 0.2% and 0.8% HA were used to reduce pain and burning sensation and accelerate palatal epithelial wound healing following a free gingival graft operation [15]. Subgingival administration of 0.2 mL 0.8% HA gel significantly reduced gingival bleeding [24] and gingival crevicular fluid flow rate [25] compared to the control groups in the patients with chronic periodontitis. Similarly, applying 0.2-mL 0.8% HA gel for 1 week after scaling and root planning significantly reduced BOP, PI, pocket PD, clinical attachment level, and colony-forming units [26]. The topical administration of 0.8% HA twice daily for 3 weeks significantly enhanced the plaque index and bleeding when probing the gingival crevicular fluid flow rate parameters in patients with gingivitis [27]. Local application of 0.8% HA twice daily for 4 weeks revealed similar results for the gingival index compared to those of the placebo gel group [26]. In a similar study, topical application of 0.2% HA as an adjunct to initial periodontal therapy in patients with chronic periodontitis revealed significantly better results when compared with those of the control group [28]. In a study investigating the effects of 0.2% HA on recurrent aphthous ulcers and oral ulcers that occur in Behçet disease, HA had positive effects on the number of ulcerative lesions, healing period, VAS, pain level, maximum area of ulcers, and inflammatory symptoms [29]. In the present study, 0.6% HA was applied following labial frenectomy operations. This dosage was selected based on similar previous studies. Moreover, the effect of 0.6% HA gel on the periodontal parameters after diode-laser-assisted frenectomy has not been previously reported in the literature.
HA may accelerate wound healing through blood clot stabilization, decreased inflammatory responses, neovascularization, angiogenesis, increased fibroblast migration, and wound closure [16, 18]. A meta-analysis reported that the laser-assisted labial frenectomy decreased the need for the administration of postoperative analgesics; however, no significant difference was observed between the laser-assisted frenectomy and conventional technique. On the other hand, the operation time, pain level, and discomfort during speech and chewing revealed better results with the laser-assisted frenectomy than those with the conventional technique [11]. Only one study reported that a better and faster healing process was observed in the patients who underwent labial frenectomy using the conventional scalpel technique [30]. This outcome may be explained by the carbonization effect of the laser, which retarded the healing process in the early stages [4]. In addition, primary closure using the conventional techniques may provide better outcomes during the early healing period [30].
Pain is a subjective condition that is difficult to evaluate objectively because the threshold level shows interindividual variations. Self-report measures are considered the most accurate and reliable method for assessing pain in children [20]. There are different methods of verbal self-report measures, including structured interviews, questionnaires, self-rating scales, and pain adjective descriptors. These methods can help individuals describe and communicate their pain experiences more accurately [31]. A child’s ability to self-report pain effects emerges later than pain intensity. These measures are typically introduced at the age of 5 years or older [32]. The VAS, which is frequently used to determine the pain level, is an easy and practical method that reveals specific outcomes depending on the clear explanation of the study and pain level evaluation process for the patient. Children are capable of assessing pain intensity at an approximate age of 8 years [33]. Children aged 8–14 years completed the VAS under parental supervision in the present study [34].
Only one previous study compared two different frenectomy techniques that evaluate the KGW, AGW, and AGT [13]. The HA- and laser-assisted frenectomy interactions were evaluated in adults without using conventional techniques in one study only [4]. In the present study, the PI, GI, BOP, and probing depth were included, and the VAS values were assessed. Furthermore, to our knowledge, no previous studies evaluated the HA effect on diode laser-assisted and conventional frenectomy techniques using these parameters in the healing process in pediatric patients.
BOP showed a significant time-dependent reduction in the CFH and DLH groups, which can be explained by the effects of HA on the inflammation phase and wound healing process rather than the enhancement of oral hygiene habits [18]. Enhancement of the probing depth, AGW, and KGW values was prominently observed in the groups that underwent HA and laser application. HA- and laser-assisted labial frenectomy displayed better tendencies than the conventional techniques regarding the postoperative patient comfort and periodontal soft tissue healing process.
This study has some limitations. First, there was a limited number of enrolled patients. The researchers faced a notable challenge while conducting studies with a larger group of participants. Second, keeping children calm and relaxed during dental procedures was challenging, especially when using laser. This could be attributed to the requirement of administering sedation to the patients. Third, the behavioral disorder caused by wearing protective equipment, including glasses, was another contributing factor. The behavioral management technique was applied to all patients (by OD). Fourth, some patients tend to avoid using HA gel regularly as communicated by some parents to the researchers. These patients were excluded from the study. Fifth, the study was concluded with a follow-up duration of 3 months. After the frenectomy procedure, many patients missed their appointments and were excluded from the study. Due to uncertainty about the COVID-19 pandemic duration, the follow-up period was short. Studies with longer follow-up durations focus on the KGW parameter; only one study by Uraz et al. reported recurrence in a few patients following diode laser-assisted frenectomy for 3 months of follow-up [13]. However, Pie-Sanchez et al. [35], Sezgin et al. [6], and Öztürk Özener et al. [2] stated that there was no recurrence in the KGW parameter after a follow-up period of 12 months. It is worth noting that all the studies were solely conducted on adult patients. If the follow-up period was longer, it may be easier to understand parameter changes in pediatric patients as they grow and develop. Finally, our results were obtained from pediatric patients. Although the VAS forms were filled out under parental supervision, the effectiveness of this measure depended on the accuracy of reporting by the family and children at home. However, this limitation can be eliminated by increasing the number of participants in future studies.
Conclusion
Diode laser-assisted labial frenectomy can be performed in pediatric patients to reduce the postoperative pain levels. Using 0.6% HA as an adjunct to diode laser-assisted frenectomy can have positive alleviating effects on the postoperative pain levels, soft tissue healing, and periodontal parameters. Evaluating the long-term development of patients under the supervision of an orthodontist will enhance the evaluation of changes in the value of the KGW parameter in future studies.
References
Haytac MC, Ozcelik O (2010) Evaluation of patient perceptions after frenectomy operations: a comparison of carbon dioxide laser and scalpel techniques. J Periodontol 77:1815–1819. https://doi.org/10.1902/jop.2006.060043
Öztürk Özener H, Meseli SE, Sezgin G, Kuru L (2020) Clinical efficacy of conventional and diode laser-assisted frenectomy in patients with different abnormal frenulum insertions: a retrospective study. Photobiomodulation, Photomedicine, Laser Surg 38:565–570. https://doi.org/10.1089/photob.2020.4841
Júnior RM, Gueiros LA, Silva IH, de Albuquerque CA, Leão JC (2015) Labial frenectomy with Nd: YAG laser and conventional surgery: a comparative study. Lasers Med Sci 30:851–856. https://doi.org/10.1007/s10103-013-1461-8
Turgut Çankaya Z, Gürbüz S, Bakirarar B, Ünsal B, Kurtiş B (2020) Evaluation of the effect of the application of hyaluronic acid following laser-assisted frenectomy: an examiner-blind, randomized, controlled clinical study. Quintessence Int 51:188–201. https://doi.org/10.3290/j.qi.a43667
Dioguardi M, Ballini A, Quarta C (2023) Labial frenectomy using laser: a scoping review. Bacci C, ed. Int J Dent 2023:1–7. https://doi.org/10.1155/2023/7321735
Sezgin G, Öztürk Özener H, Meseli SE, Kuru L (2020) Evaluation of patient’s perceptions, healing, and reattachment after conventional and diode laser frenectomy: a three-arm randomized clinical trial. Photobiomodulation, Photomedicine, Laser Surg 38:552–559. https://doi.org/10.1089/photob.2019.4783
Devishree D (2012) Frenectomy: a review with the reports of surgical techniques. J Clin Diagnostic Res Published online 2012. https://doi.org/10.7860/JCDR/2012/4089.2572
Viet DH, Ngoc VTN, Anh LQ (2019) Reduced need of infiltration anesthesia accompanied with other positive outcomes in diode laser application for frenectomy in children. J Lasers Med Sci 10:92–96. https://doi.org/10.15171/jlms.2019.15
Baxter RT, Zaghi S, Lashley AP (2022) Safety and efficacy of maxillary labial frenectomy in children: a retrospective comparative cohort study. Int Orthod 20:100630. https://doi.org/10.1016/j.ortho.2022.100630
American Academy of Pediatric Dentistry (2023) Policy on management of the frenulum in pediatric patients. Ref Man Pediatr Dent Chicago, III Am Acad Pediatr Dent Published online 71-76.
Protásio ACR, Galvão EL, Falci SGM (2019) Laser techniques or scalpel incision for labial frenectomy: a meta-analysis. J Maxillofac Oral Surg 18:490–499. https://doi.org/10.1007/s12663-019-01196-y
Sfasciotti GL, Zara F, Vozza I, Carocci V, Ierardo G, Polimeni A (2020) Diode versus CO2 laser therapy in the treatment of high labial frenulum attachment: a pilot randomized, double-blinded clinical trial. Int J Environ Res Public Health 17:7708. https://doi.org/10.3390/ijerph17217708
Uraz A, Çetiner FD, Cula S, Guler B, Oztoprak S (2018) Patient perceptions and clinical efficacy of labial frenectomies using diode laser versus conventional techniques. J Stomatol Oral Maxillofac Surg 19:182–186. https://doi.org/10.1016/j.jormas.2018.01.004
Eliezer M, Imber J-C, Sculean A, Pandis N, Teich S (2019) Hyaluronic acid as adjunctive to non-surgical and surgical periodontal therapy: a systematic review and meta-analysis. Clin Oral Investig 23:3423–3435. https://doi.org/10.1007/s00784-019-03012-w
Yıldırım S, Özener HÖ, Doğan B, Kuru B (2018) Effect of topically applied hyaluronic acid on pain and palatal epithelial wound healing: an examiner-masked, randomized, controlled clinical trial. J Periodontol 89:36–45. https://doi.org/10.1902/jop.2017.170105
Casale M, Moffa A, Vella P (2016) Hyaluronic acid: perspectives in dentistry. A systematic review. Int J Immunopathol Pharmacol 29:572–582. https://doi.org/10.1177/0394632016652906
Dahiya P, Kamal R (2013) Hyaluronic acid: a boon in periodontal therapy. N Am J Med Sci 5:309–315. https://doi.org/10.4103/1947-2714.112473
Alpan AL, Cin GT (2023) Comparison of hyaluronic acid, hypochlorous acid, and flurbiprofen on postoperative morbidity in palatal donor area: a randomized controlled clinical trial. Clin Oral Investig 27:2735–2746. https://doi.org/10.1007/s00784-022-04848-5
Faul F, Erdfelder E, Buchner A, Lang A-G (2009) Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav Res Methods 41:1149–1160. https://doi.org/10.3758/BRM.41.4.1149
Jain A, Yeluri R, Munshi AK (2012) Measurement and assessment of pain in children—a review. J Clin Pediatr Dent 37:125–136. https://doi.org/10.17796/jcpd.37.2.k84341490806t770
Akpınar A, Toker H, Lektemur Alpan A, Çalışır M (2016) Postoperative discomfort after Nd:YAG laser and conventional frenectomy: comparison of both genders. Aust Dent J 61:71–75. https://doi.org/10.1111/adj.12333
Tancredi S, De Angelis P, Marra M et al (2022) Clinical comparison of diode laser assisted “v-Shape Frenectomy” and conventional surgical method as treatment of ankyloglossia. Healthcare 10:89. https://doi.org/10.3390/healthcare10010089
Asparuhova MB, Kiryak D, Eliezer M, Mihov D, Sculean A (2019) Activity of two hyaluronan preparations on primary human oral fibroblasts. J Periodontal Res 54:33–45. https://doi.org/10.1111/jre.12602
Johannsen A, Tellefsen M, Wikesjö U, Johannsen G (2009) Local delivery of hyaluronan as an adjunct to scaling and root planing in the treatment of chronic periodontitis. J Periodontol 80:1493–1497. https://doi.org/10.1902/jop.2009.090128
Xu Y, Höfling K, Fimmers R, Frentzen M, Jervøe-Storm PM (2004) Clinical and microbiological effects of topical subgingival application of hyaluronic acid gel adjunctive to scaling and root planing in the treatment of chronic periodontitis. J Periodontol 75:1114–1118. https://doi.org/10.1902/jop.2004.75.8.1114
Polepalle T, Srinivas M, Swamy N, Aluru S, Chakrapani S, Chowdary B (2015) Local delivery of hyaluronan 0.8% as an adjunct to scaling and root planing in the treatment of chronic periodontitis: a clinical and microbiological study. J Indian Soc Periodontol 19:37. https://doi.org/10.4103/0972-124X.145807
Al-Shammari NM, Shafshak SM, Ali MS (2018) Effect of 0.8% hyaluronic acid in conventional treatment of moderate to severe chronic periodontitis. J Contemp Dent Pract 19:527–534. https://doi.org/10.5005/JP-JOURNALS-10024-2294
Gontiya G, Galgali S (2012) Effect of hyaluronan on periodontitis: a clinical and histological study. J Indian Soc Periodontol 16:184. https://doi.org/10.4103/0972-124X.99260
Lee J, Jung J, Bang D (2008) The efficacy of topical 0.2% hyaluronic acid gel on recurrent oral ulcers: comparison between recurrent aphthous ulcers and the oral ulcers of Behçet’s disease. J Eur Acad Dermatology Venereol 22:590–595. https://doi.org/10.1111/j.1468-3083.2007.02564.x
Binti Zaaba NAA (2021) Evaluation of healing following frenectomy. Bioinformation 17:1138–1143. https://doi.org/10.6026/973206300171138
McGrath PJ, Unruh AM (1999) Measurement and asessment of paediatric pain. in Textbook of pain, Wall PD and Melzack R, Eds., pp. 371–384, Churchill Livingstone, New York, USA, 4th edition
McGrath PA, deVeber LLHM (1985) Multidimensional pain assessment in children. In: Fields H, Dubner R, Cervero F (eds) Advances in Pain Research and Therapy. Baven Press, pp 387–393
McGrath PAGJ (2001) Pain assessment in children and adolescents. In: Turk DCMR (ed) Handbook of Pain Assessment, 2nd edn. Guilford Press, pp 97–118
Bringuier S, Dadure C, Raux O, Dubois A, Picot M-C, Capdevila X (2009) The perioperative validity of the visual analog anxiety scale in children: a discriminant and useful instrument in routine clinical practice to optimize postoperative pain management. Anesth Analg 109:737–744. https://doi.org/10.1213/ane.0b013e3181af00e4
Pié-Sánchez J, España-Tost A-J, Arnabat-Domínguez J, Gay-Escoda C (2012) Comparative study of upper lip frenectomy with the CO2 laser versus the Er, Cr:YSGG laser. Med Oral Patol Oral Cir Bucal 17:e228–e232. https://doi.org/10.4317/medoral.17373
Acknowledgements
All authors thank Dr. Batuhan Bakırarar (PhD) for providing statistical assistance in the preparation of the manuscript.Thanks to Dr. Büşra Yıldız for reviewing and preparing the article for submission.
Funding
Open access funding provided by the Scientific and Technological Research Council of Türkiye (TÜBİTAK).
Author information
Authors and Affiliations
Contributions
Dr. Suat Serhan ALTINTEPE DOĞAN performed frenectomy operations and contributed to interpreting the results. Dr. Nebi Cansın Karakan conducted frenectomy procedures and contributed to the manuscript’s writing. Dr. Özgür Doğan provided behavioral management during frenectomy for pediatric patients and contributed to the result interpretation. After completing the article, Dr. Suat Serhan ALTINTEPE DOĞAN and Dr. Nebi Cansın KARAKAN worked collaboratively to conduct the final check procedures.
Corresponding author
Ethics declarations
Ethical approval
The Human Ethics Committee of approved the study protocol (2019/220). The study protocol followed the principles of the Helsinki Declaration.
Competing ınterests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Doğan, S.S.A., Karakan, N.C. & Doğan, Ö. Effects of topically administered 0.6% hyaluronic acid on the healing of labial frenectomy in conventional and 940-nm indium gallium arsenide phosphide (InGaAsP) diode laser techniques in pediatric patients: a randomized, placebo-controlled clinical study. Lasers Med Sci 39, 48 (2024). https://doi.org/10.1007/s10103-024-03983-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10103-024-03983-7