Abstract
Aim
In the field of healthcare, the paramount concern is the safety of patients. Demographic and socioeconomic factors that can influence patient safety are often overlooked in the context of clinical protocols, which receive considerable attention. The objective of this review was to examine the relationship between demographic and socioeconomic variables and their impact on patient involvement in safety measures.
Subject and methods
This scoping review followed the PRISMA-ScR guidelines. The literature search was conducted in the APA PsycInfo, Cochrane Library, MEDLINE, PSYNDEX, PubMed, and Web of Science Core Collection databases from 1970 to 2023. The titles and abstracts of the identified studies were first screened, followed by a review of relevant full texts to extract information on demographic and socioeconomic factors, patient involvement, and patient safety.
Results
A total of 17 articles were selected and subjected to analysis from the initial 278 studies. The findings of this study indicate that the patient involvement and safety in healthcare are substantially influenced by demographic and socioeconomic factors. It was observed that there were differences in patient communication, perception of medical errors, and willingness to actively participate in healthcare.
Conclusion
As healthcare providers and policymakers strive to enhance patient safety and care quality, it is crucial to acknowledge and consider the various factors that have been studied. In the future, it will be important to prioritize personalized and culturally sensitive approaches to ensure equitable access to safe and effective medical treatment for all individuals, regardless of their demographic or social background.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Patient involvement is crucial for ensuring the safety and efficacy of medical treatments. Healthcare providers should adopt a patient-centered approach that considers patients’ opinions, preferences, and values when providing comprehensive care. A collaborative partnership between medical professionals and patients is imperative, especially in the context of patient safety measures (Hrisos and Thomson 2013). Furthermore, barriers between patients and healthcare providers can be reduced if healthcare providers encourage patient involvement and engagement in safety measures (World Health Organization 2006).
The marginalization of individuals from lower socioeconomic backgrounds in treatment decision-making processes is a disconcerting trend (Thompson et al. 1993). This is frequently compounded by healthcare providers presuming a diminished need for comprehensive information, which is further compounded by social disparities. These social disparities, which encompass age, gender, ethnicity/race, income, education, and occupational status, underscore pervasive inequalities within healthcare systems and have a particular impact on demographics such as racial and ethnic minorities, as well as those who are grappling with limited income and educational opportunities (Sheiham 2009; Williams et al. 2010). People with low socioeconomic status often face serious chronic diseases. These individuals are at increased risk of several health problems (Marmot and Bell 2012). Some of the most common diseases in this population include heart attack, stroke, diabetes, and chronic obstructive pulmonary disease (Lampert et al. 2016; Robert Koch-Institut 2017).
Previous studies have not thoroughly examined the relationship between demographic and socioeconomic factors and patient involvement in patient safety measures. The preliminary search did not identify any additional systematic reviews or scoping reviews on the topics listed above. Reviews have examined patients’ willingness and ability to actively participate in patient safety (Berger et al. 2014; Butterworth et al. 2019; Doherty and Stavropoulou 2012; Duhn et al. 2020; Fonhus et al. 2018; Hall et al. 2010; Kim et al. 2018; Longtin et al. 2010; Mackintosh et al. 2020; Merner et al. 2023; Ocloo et al. 2021; Schubert et al. 2009; Yousif 2002), but none of them focused on the impact of demographic and socioeconomic barriers. According to Ocloo et al., additional research is necessary in this area (Ocloo et al. 2021). Currently, only individual studies are available, and no reviews have been conducted on this topic. Therefore, this study aimed to answer the following research question: What is the impact of demographic and socioeconomic factors on patient involvement in patient safety measures?
To effectively address the research question, the variable definitions were carefully crafted by drawing upon the findings and definitions found in the literature. The involvement of patients in safety measures is evidenced by various aspects of the healthcare process. This includes examining patient, staff, and organizational factors, as well as various dimensions of patient involvement, such as decision-making, health service design, and empowerment strategies (Snyder and Engstrom 2016). (For a comprehensive list of enablers for patient involvement and patient involvement measures, please refer to Table 1.) The National Patient Safety Goals for Hospitals, established by The Joint Commission are crucial tools for evaluating patient safety practices (The Joint Commission 2023). It is of the utmost importance to adhere to these goals to ensure patient safety. The goals encompass several domains, including drug safety, infection prevention, staff communication, and patient identification. Please refer to Table 2 for a comprehensive list of patient safety measures. The objective of this study was to address this research question by analyzing several demographic factors, including age, gender, and ethnicity/race, as well as a range of socioeconomic variables, such as income, education level, and occupational status.
The objective of this scoping review is to provide a comprehensive overview of demographic and socioeconomic factors affecting patient involvement in safety interventions and to identify existing challenges and promising approaches in outpatient and inpatient healthcare settings. The literature on the subject is presented, and various aspects of the topic are highlighted to address the identified knowledge gap.
These findings can serve as a foundation for additional research aimed at improving the equity of healthcare. This analysis identified research gaps and areas for future systematic reviews, which will ultimately improve healthcare for all.
Methods
A scoping review is a method to comprehensively understand a topic, with less strict inclusion criteria and a focus on mapping existing research to identify key concepts and potential gaps. It follows the Joanna Briggs Institute guidelines, and this review’s objectives and methods are outlined in a protocol (Peters et al. 2020). We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) checklist to comply with these guidelines (Tricco et al. 2018). The study protocol collected various data on the results, such as the lead author, year of the study, location, purpose of the research, whether it was a single-center or multicenter study, number of participants, duration, and key findings. This study also provided detailed observations regarding the context in which the trial occurred, the interventions used, and the precautions taken to ensure patient safety. The protocol is available upon submission of a reasonable request from the authors.
Eligibility criteria (PCC framework)
The PCC framework (which stands for “population-concept–context”) constituted the foundation for the variables to be examined. This framework defines the criteria for selecting studies that could be subjected to further analysis. The criteria included the population for patient selection, the concept of patient involvement, and patient safety measures, with demographic and socioeconomic characteristics serving as the context.
Population
This review examines the personal experiences of outpatient and inpatient healthcare patients aged 18 years or older. Note that studies on patients under the age below 18 years are also included if their experiences are reported by a family member or third party. Studies are also conducted in inpatient, outpatient, and ambulatory settings.
Concept
For inclusion in the review, at least two aspects from Table 1, enablers for patient involvement and patient involvement measures, should be assessed. The following areas of patient involvement were considered (Snyder and Engstrom 2016).
In addition, at least one category of patient safety measures from Table 2 had to be included in the comprehensive literature review. As a result, each study was assessed based on these patient safety measures (The Joint Commission 2023).
Context
To be included in this review, studies must consider at least two indicators of demographic or socioeconomic factors: age, gender, ethnicity/race, income, educational level, and occupational status.
Literature databases
To ensure a collection of relevant findings, we deliberately defined search terms broadly. This approach ensures that literature and studies with different methodologies and in different languages are included. As a result, the search covers a wide range of content as well as methodological and linguistic components, making it extensive and comprehensive.
Inclusion criteria
Following database selection, a search query was developed in line with the PCC framework. This query was supplemented with parameters such as “study design,” “language” (English and German), and “year” (1970–2023) to facilitate an accurate search.
Our scoping review included various experimental and quasiexperimental study designs, including randomized controlled trials, nonrandomized trials, prepost studies, and interrupted time series studies. Additionally, we considered analytical observational studies (prospective/retrospective cohort, case‒control, and analytical cross-sectional studies), as well as descriptive observational studies, such as case series, reports, and descriptive cross-sectional studies. We also included qualitative studies. However, all articles or texts identified must meet the eligibility criteria defined by the PCC framework.
Search strategy
The search was conducted using the PCC framework to guide the targeted selection of keywords and Medical Subject Headings (MeSH) terms. These variables were used in various configurations with Boolean operators (AND, OR) and truncating variables to perform a comprehensive search. To further refine the search, experts were consulted to identify synonymous terms through brainstorming (Wachtel and Dexter 2013). The results of the preliminary search were thoroughly reviewed and systematically expanded, culminating in the formulation of the final search term (Hirt and Nordhausen 2019).
The search string developed (Table 3: Example search string in MEDLINE) was divided into the following three main sections:
-
Topic 1: Patient involvement.
-
Topic 2: Patient safety measures.
-
Topic 3: Demographic and socioeconomic factors.
A search was conducted using a database information system (DBIS) to select the six most relevant databases in the fields of medicine and sociology.
We searched the following databases between January 01, 2024, and February 01, 2024: APA PsycInfo, Cochrane Library, MEDLINE, PSYNDEX, PubMed, and Web of Science Core Collection. This focused selection ensured comprehensive coverage of the medical and social science aspects related to our research question and allowed for a thorough exploration of the relevant literature.
In the third stage, we searched the reference lists of the identified reports and articles to identify additional sources. We reviewed the reference lists of all identified sources to identify additional relevant literature sources.
To potentially discover additional relevant data to complement our primary search results, we conducted an extended search on Google Scholar, reviewing the first 50 results.
This structured approach ensured comprehensive coverage of relevant literature on the relationships among patient involvement, patient safety, and demographic and socioeconomic factors.
Study selection process
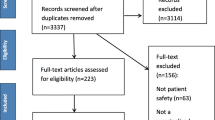
The collected information was organized as a study protocol in a structured Excel spreadsheet (Microsoft 2024) with the help of EndNote software (Clarivate Analytics 2023) to manage the search results. The titles and abstracts were independently assessed by a research member (CM). Duplicates were eliminated, and the formal criteria were checked. The final studies were selected by an extensive review of the articles using predefined inclusion and exclusion criteria (see Fig. 1). To identify further relevant studies, the reference lists of the selected articles were also examined. Two research members (CM and AH) jointly evaluated each study. In cases of disagreement, a consensus discussion was held to reach a consensus. This rigorous selection process guarantees the reliability and quality of the research findings included in this study. A review of 151 articles was conducted. In total, 134 articles, including 38 literature reviews, were excluded.
Synthesis was conducted by systematically reviewing identified studies and sources using both qualitative and quantitative approaches to provide comprehensive answers to the research questions. To extract key information, the PCC framework was applied to each final study. In addition to the PCC framework, we also considered the associated level of evidence (OCEBM Levels of Evidence Working Group 2012) in our assessment of these studies. This approach enabled the evaluation of methodological quality, scope, relevance, and suitability for our analysis. The findings were synthesized according to the framework outlined in the study protocol, and each study was evaluated directly against the developed research questions and objectives.
Results
A total of 295 articles were initially retrieved, with 278 remaining after duplicate removal (Fig. 1). On the basis of our predefined criteria, a review of 151 articles was conducted. In total, 134 articles, including 38 literature reviews, were excluded. In total, 17 articles were ultimately eligible for inclusion. These articles describe patient involvement in patient safety measures or study the views of patients who are actively involved in the safety of their care, considering demographic and socioeconomic factors.
Study description
The selected studies were conducted between 2002 and 2018. Eight were from the United States (n = 8) (Adams and Boscarino 2004; Bell et al. 2017; Bell et al. 2016; Burroughs et al. 2007; Clare et al. 2013; Miller et al. 2011; Pandhi et al. 2008; Tai-Seale et al. 2016), and three were from Great Britain (Davis et al. 2008; Davis et al. 2012; Gray et al. 2017). In addition, there was one study in each of the following countries: Italy (Abbate et al. 2008), Switzerland (Schwappach et al. 2011), Taiwan (Wang et al. 2013), Australia (Eassey et al. 2016), and Canada (Backman et al. 2018). One study captured 26 European Union countries (Nikoloski and Mossialos 2013).
The study populations varied widely, with some studies consisting of small groups of as few as nine people (Backman et al. 2018) and others containing large samples of up to 26,000 participants (Nikoloski and Mossialos 2013). Table 4 provides a comprehensive overview outlining the characteristics of the selected studies.
The review identified a range of designs, consisting of cross-sectional studies (59%) (n = 10) (Abbate et al. 2008; Adams and Boscarino 2004; Burroughs et al. 2007; Clare et al. 2013; Davis et al. 2008; Eassey et al. 2016; Gray et al. 2017; Miller et al. 2011; Nikoloski and Mossialos 2013; Schwappach et al. 2011), two randomized controlled trials (Bell et al. 2016; Wang et al. 2013), and two quasiexperimental studies (Bell et al. 2017; Tai-Seale et al. 2016), each accounting for 12%. Before and after studies (Davis et al. 2012), prospective cohort studies (Pandhi et al. 2008), and qualitative studies (Backman et al. 2018) were counted once (6%). The use of questionnaires administered online, by mail, by telephone, or in person was the most commonly used data collection method in 82% of the studies (n = 14) (Abbate et al. 2008; Adams and Boscarino 2004; Bell et al. 2017; Bell et al. 2016; Burroughs et al. 2007; Clare et al. 2013; Davis et al. 2008; Davis et al. 2012; Eassey et al. 2016; Miller et al. 2011; Pandhi et al. 2008; Schwappach et al. 2011; Tai-Seale et al. 2016; Wang et al. 2013). Personal interviews were used in 18% (n = 3) of the studies (Backman et al. 2018; Gray et al. 2017; Nikoloski and Mossialos 2013). Twenty-four percent (n = 4) used a combination of two different methods to collect data (Abbate et al. 2008; Pandhi et al. 2008; Schwappach et al. 2011; Tai-Seale et al. 2016).
A visual representation of the frequency of each aspect mentioned in the PCC variables was created to provide a clear picture of how often certain characteristics occurred in the examined studies. This graphical representation enables the identification of trends in the data, which in turn facilitates a more comprehensive understanding of the importance and influence of each variable. This is demonstrated in Table 5 and Table 6.
Patient involvement and patient safety measures
Enablers of patient involvement and patient involvement measures
Various approaches to patient involvement have been studied, with each study considering patient involvement in development and research. The studies analyzed in this review primarily focused on patient empowerment (82%, n = 14), which was the main focus of the studies analyzed in this review (Abbate et al. 2008; Adams and Boscarino 2004; Backman et al. 2018; Burroughs et al. 2007; Clare et al. 2013; Davis et al. 2008; Davis et al. 2012; Eassey et al. 2016; Gray et al. 2017; Miller et al. 2011; Nikoloski and Mossialos 2013; Schwappach et al. 2011; Tai-Seale et al. 2016; Wang et al. 2013). Additionally, staff communication for involvement was a key area of focus (59%, n = 10) (Abbate et al. 2008; Bell et al. 2016; Burroughs et al. 2007; Clare et al. 2013; Davis et al. 2008; Davis et al. 2012; Eassey et al. 2016; Miller et al. 2011; Schwappach et al. 2011; Tai-Seale et al. 2016), while healthcare delivery was also addressed by 41% (n = 7) of the participants (Adams and Boscarino 2004; Backman et al. 2018; Bell et al. 2016; Eassey et al. 2016; Gray et al. 2017; Schwappach et al. 2011; Wang et al. 2013). Forty-six percent (n = 6) of the studies focused on promoting patient involvement through measures such as education (Bell et al. 2017; Bell et al. 2016; Davis et al. 2012; Eassey et al. 2016; Schwappach et al. 2011; Wang et al. 2013). Organizational factors, including service systems and technology (Backman et al. 2018; Bell et al. 2017; Davis et al. 2012; Tai-Seale et al. 2016) and patient involvement in decision-making (Adams and Boscarino 2004; Miller et al. 2011; Pandhi et al. 2008; Tai-Seale et al. 2016), were examined in 24% of the participants (n = 4). Three investigations examined staff factors specifically related to training (18%, n = 3) (Davis et al. 2012; Schwappach et al. 2011; Wang et al. 2013).
Patient safety measures
The studies analyzed various aspects of patient safety, with most examining multiple interventions. Staff communication was analyzed in 65% (n = 11) of all studies (Abbate et al. 2008; Backman et al. 2018; Burroughs et al. 2007; Clare et al. 2013; Davis et al. 2008; Davis et al. 2012; Eassey et al. 2016; Miller et al. 2011; Schwappach et al. 2011; Tai-Seale et al. 2016; Wang et al. 2013), followed by medication safety support in 59% (n = 10) of all studies (Adams and Boscarino 2004; Backman et al. 2018; Bell et al. 2017; Bell et al. 2016; Burroughs et al. 2007; Davis et al. 2012; Eassey et al. 2016; Gray et al. 2017; Schwappach et al. 2011; Wang et al. 2013), preventing infections in 29% (n = 5) of all studies (Abbate et al. 2008; Clare et al. 2013; Davis et al. 2008; Davis et al. 2012; Schwappach et al. 2011) and preventing surgical mistakes in 18% (n = 3) of all studies (Burroughs et al. 2007; Miller et al. 2011; Schwappach et al. 2011). Improving equity of care (Adams and Boscarino 2004; Nikoloski and Mossialos 2013) and patient identification (Burroughs et al. 2007; Schwappach et al. 2011) were analyzed in 15% (n = 2) of the studies. None of the studies considered identifying safety risks or alarm safety. We also examined measures that have a substantial impact on patient safety that are not addressed in the Joint Commission’s National Patient Safety Goals for Hospitals (The Joint Commission 2023), including transitions and continuity of care (18%, n = 3) (Backman et al. 2018; Pandhi et al. 2008; Schwappach et al. 2011) and documentation errors (6%, n = 1) (Bell et al. 2017).
Demographic and socioeconomic factors (context)
All studies considered age and gender as demographic factors.
Age
Patients’ age plays a pivotal role in their involvement in patient safety measures. Different age groups may have different needs and challenges. In the studies, age was reported in two ways: individually (59%) (n = 10) (Backman et al. 2018; Bell et al. 2017; Bell et al. 2016; Burroughs et al. 2007; Clare et al. 2013; Davis et al. 2008; Davis et al. 2012; Nikoloski and Mossialos 2013; Tai-Seale et al. 2016; Wang et al. 2013) or in groups (n = 7) (Abbate et al. 2008; Adams and Boscarino 2004; Eassey et al. 2016; Gray et al. 2017; Miller et al. 2011; Pandhi et al. 2008; Schwappach et al. 2011). A literature review revealed that patient safety concerns were most common among parents of pediatric patients and patients aged 30–59 years. In contrast, patients aged 20–29 years had the lowest level of concern (Burroughs et al. 2007). Moreover, the 30–64-year-old age group was found to be more vulnerable to medical errors in healthcare (Adams and Boscarino 2004). The likelihood of experiencing an adverse event (Nikoloski and Mossialos 2013) and the frequency of worry regarding medical errors and safety incidents (Burroughs et al. 2007) both increase with age. Schwappach et al. (Schwappach et al. 2011) found that active participation in system transitions had significant benefits for older individuals, resulting in a marked improvement in their healthcare experience. Adverse event reporting rates increase with age (Gray et al. 2017), indicating that patient safety is more critical in older patients. However, Pandhi et al. (Pandhi et al. 2008) found no significant association between age and feelings of unsafety. According to a study by Wang et al. (Wang et al. 2013), volunteer support was found to be particularly beneficial in promoting patient safety measures for individuals with lower educational attainment, particularly elderly individuals. A study on shared decision-making (Tai-Seale et al. 2016) revealed that older patients had positive experiences. According to (Clare et al. 2013), younger respondents were more likely than older respondents to request that healthcare staff wash their hands.
Gender
Gender-based differences can influence the perception of healthcare services and willingness to participate, which in turn can impact various safety measures. In most studies, gender was conventionally categorized as male or female. However, Clare et al. (Clare et al. 2013) deviated from this norm by surveying only women. This decision was made owing to the thematic focus of the study on a specific topic. Overall, the reviewed literature indicates that women are more prone to criticism and insecurity (Nikoloski and Mossialos 2013), particularly when changing their doctor or medical facility (Pandhi et al. 2008). Additionally, women are more likely to report adverse events (Gray et al. 2017), whereas men tend to fill out medical error statistics and appear to be less concerned about their healthcare overall. Notably, no significant associations were identified between gender and medication reporting or concern regarding medication errors (Burroughs et al. 2007; Eassey et al. 2016). According to Davis et al. (2012), female patients who had completed a university degree were more likely to ask nurses factual and challenging questions. Male patients were less likely than female patients to ask questions of medical staff.
Level of education
Educational achievement impacts one’s comprehension of health and ability to process complex health information. Consequently, individuals with diverse educational backgrounds may exhibit varying levels of engagement. In 82% (n = 14) of the studies (Abbate et al. 2008; Adams and Boscarino 2004; Bell et al. 2017; Clare et al. 2013; Davis et al. 2008; Davis et al. 2012; Eassey et al. 2016; Gray et al. 2017; Miller et al. 2011; Nikoloski and Mossialos 2013; Pandhi et al. 2008; Schwappach et al. 2011; Tai-Seale et al. 2016; Wang et al. 2013), the level of education was considered. The research covered vocational education and training across various categories, encompassing a broad range of educational qualifications. These categories included commonly known qualifications such as GCSE/O-Level/CSE as well as qualifications ranging from primary school education to master’s degrees or equivalent qualifications. This method facilitated a thorough examination of the varied educational backgrounds of the participants. Schwappach et al. (2011) divided the educational path into primary, secondary, and tertiary education to enable a detailed analysis of the different stages of educational attainment. Additionally, Abbate et al. (2008) differentiated educational levels based on the number of years of education they completed, allowing for a more precise evaluation of educational background and duration. Research has demonstrated that individuals with higher education levels are more likely to actively participate in healthcare (Bell et al. 2017). For instance, Miller et al. (2011) reported that patients with higher education levels tend to ask more questions about medical procedures and report greater well-being after the procedure. The importance of patient education and empowerment in healthcare was highlighted by Davis et al. (2008) found that patients without university degrees were less likely to ask challenging or factual questions from physicians and nurses. Furthermore, Clare et al. (2013) indicated that individuals with a university degree are almost twice as likely to ask medical staff to wash their hands than those with less formal education. Additionally, a study by Abbate et al. (2008) revealed that patients with higher education levels had a better understanding of the definition, risk groups, and risk factors of hospital-acquired infections. Individuals with lower incomes and education levels are at greater risk of adverse events and tend to have a more negative perception of the healthcare system. Furthermore, those with lower health literacy levels and poorer health are more likely to experience medication-related issues (Eassey et al. 2016).
Ethnicity/race
Ethnicity/race can influence access to healthcare services and trust in the healthcare system. These factors can influence the degree of active participation exhibited by patients. In 59% (n = 10) (Adams and Boscarino 2004; Bell et al. 2017; Bell et al. 2016; Burroughs et al. 2007; Clare et al. 2013; Davis et al. 2008; Davis et al. 2012; Gray et al. 2017; Miller et al. 2011; Tai-Seale et al. 2016) of the analyzed studies, ethnicity/race was identified as an important factor. The studies considered various ethnic groups, including white people, African Americans, and Hispanics. Ethnicity/race data were collected using different categories that reflect the diversity of the population, such as Caucasian, non-Caucasian, and specific ethnic groups, such as Asian, people of color, Hispanic, and others. Gray et al. analyzed the geographical distribution of participants in the UK to capture regional differences in ethnic composition. Ethnicity/race may influence perceptions of inaccuracies and errors in patient records, according to a study from Bell et al. (2017). The study revealed that individuals who identified such errors were more likely to be white. Clare et al. (2013) found no statistically significant differences in willingness to ask staff to wash their hands, while examining differences by ethnicity/race. However, the frequency of concern about medical errors and safety incidents differed substantially by ethnicity/race. According to Burroughs et al. ( 2007), people of color feel significantly less safe and have more concerns than Asian or white individuals.
Occupational status
The occupational status of an individual can influence their access to specific healthcare services. Moreover, it may influence the amount of time available to participate in training or decision-making processes. In 41% (n = 7) of the analyzed studies (Abbate et al. 2008; Clare et al. 2013; Davis et al. 2008; Davis et al. 2012; Eassey et al. 2016; Gray et al. 2017; Wang et al. 2013), participants’ occupational status was identified as an important indicator of their socioeconomic situation. A wide range of occupations were considered, from senior and middle management to unskilled manual work and unemployment. Work status was evaluated using various categories that reflect different employment relationships, including casual work, part-time and full-time employment, sick leave, and retirement. Additionally, occupational positions, including employed, unemployed, retired, student, and non-specialized occupational activities, were classified. In one study (Clare et al. 2013), detailed questions were asked about the professional situation to obtain a comprehensive picture. For instance, participants were asked to indicate their primary occupation and whether they were self-employed. Davis et al.’s (2008) study showed that professional status has a significant impact on communication with patients. Compared with retired patients, unemployed patients were less likely to ask questions from doctors and nurses, whereas working patients were more willing to ask factual questions and follow medical professionals’ instructions.
Income
The financial status of an individual may influence the accessibility of healthcare resources. Low-income individuals may encounter obstacles in engaging in safety measures. Income data were collected for 29% (n = 5) (Adams and Boscarino 2004; Bell et al. 2016; Clare et al. 2013; Gray et al. 2017; Nikoloski and Mossialos 2013) of the studies. Participants were categorized into income groups ranging from less than $25,000 to $100,000 or more. Notably, one study (Nikoloski and Mossialos 2013) did not directly measure income but instead examined participants’ challenges in paying their monthly bills. This study focused on the financial burden of monthly expenses in the past 12 months rather than solely on income levels. Adams and Boscarino (2004) reported that individuals from higher-income households experienced fewer medical errors than those from lower-income households. Similarly, people of color reported fewer medical errors than did those who did not identify as people of color. On the other hand, individuals with lower incomes and less education reported more adverse events (Gray et al. 2017) and negative perceptions of the quality of their healthcare (Nikoloski and Mossialos 2013). These findings suggest a correlation between income and medical errors, as well as between adverse events and negative perceptions of healthcare quality. The willingness to ask staff to wash their hands was not significantly different based on income (Clare et al. 2013).
Discussion
This review identified 17 primary studies that investigated the correlation between demographic and socioeconomic factors and patient involvement in patient safety interventions. The studies considered were conducted between 1970 and 2023, and only a small number explored the effects of demographic and socioeconomic factors on patient safety. The findings of this scoping review underscore the consequences of inequalities in the healthcare system and highlight the pressing need for action to bridge gaps in quality and equity.
Age is a crucial factor in the overall health and well-being of patients. Our findings suggest that older adults have greater resilience despite potential health problems, which shapes their positive attitudes. In addition, older patients may have greater awareness of safety concerns due to comorbidities and a higher risk of adverse events. A study by Ricci-Cabello et al. suggested that younger patients are more likely to express negative experiences regarding patient safety (Ricci-Cabello et al. 2017). This may indicate heightened awareness and a stronger motivation to advocate for themselves. Age-related differences in safety concerns and patient involvement may be explained by several factors. Older individuals may be more sensitive to safety concerns in healthcare given their advanced age and potential health issues. Women generally exhibit greater interest in their health, leading to increased engagement in seeking treatment information. This is reflected in their higher health literacy and awareness of their own health. Furthermore, this indicates that women with higher education levels may exhibit a more pronounced degree of patient involvement. Various sociocultural and biological factors may make women more sensitive to criticism and uncertainty. This sensitivity is especially noticeable when changes occur, such as those occurring in the treating physician or medical facility (Pandhi et al. 2008). In contrast, men tend to ask fewer questions, suggesting a potential gender gap in patient communication with healthcare professionals (Davis et al. 2012). The impact of demographic and socioeconomic status on health experiences and outcomes is profound. Individuals with higher incomes have greater access to healthcare resources and receive more comprehensive care, which can reduce the risk of medical errors (Adams and Boscarino 2004). Additionally, those with higher education levels possess a better understanding of health information, enabling them to make informed decisions and actively participate in their healthcare (Willems et al. 2005). This leads to improved communication with healthcare providers and reduces misunderstandings. Furthermore, individuals from higher socioeconomic backgrounds often feel empowered to advocate for their healthcare needs and receive support from a wider social network. These factors collectively impact health experiences and outcomes by influencing access to resources, comprehension of health information, self-advocacy, and social support. Patients may lack confidence in their ability to make medical decisions, which could result in their reluctance to ask questions or voice safety concerns.
Overall, the study suggested that there are disparities in patient safety and the quality of healthcare interactions. The outcomes of these disparities may be attributable to structural inequalities within the healthcare system and potential bias or discrimination against specific groups within the healthcare sector. Other studies have demonstrated that individuals belonging to racial and ethnic minority groups and their caregivers receive less information from physicians and make fewer statements about active participation than white patients (Gordon et al. 2006). Furthermore, patients rated a participatory decision-making style more highly when they saw physicians of their own race (Cooper-Patrick et al. 1999).
To ensure that all patients receive adequate care, it is important to consider the needs and experiences of all patients, regardless of ethnicity/race. Targeted interventions are recommended to address healthcare disparities experienced by patients of different ethnic backgrounds. Implementing such interventions is crucial for addressing these disparities. To enhance healthcare equity and quality for all, interventions such as increasing healthcare providers’ awareness of cultural differences, implementing policies to combat biases and discrimination within the healthcare system, and improving access to healthcare resources and services for disadvantaged ethnic groups can be implemented. The data suggest that a person’s employment status may influence their level of interaction with medical staff (Davis et al. 2008). Specifically, employed patients tend to be more communicative and engaged in their healthcare, which may be indicative of greater self-confidence and a sense of control over their health. In contrast, unemployed patients are less likely to actively participate or ask questions. This could be due to challenges such as financial difficulties or social isolation, which can affect self-confidence and empowerment when making health decisions. Occupational status may have an impact on not only financial but also health behaviors and interactions with the healthcare system. It is important to consider these factors when evaluating this relationship.
Several factors, such as patient-related issues and the attitudes, skills, and training of healthcare professionals, can create barriers to safe healthcare. Maintaining a balanced and objective healthcare approach is important. It is crucial to recognize each patient as an active partner in their healthcare to promote better outcomes. Doctor–patient relationships can encourage patients’ willingness to participate in their healthcare, whereas patients who feel subordinate can hinder this willingness (Berger et al. 2014). Promoting patient engagement is crucial for healthcare (Trier et al. 2015). Outdated practices must be abandoned, and healthcare providers must improve their attitudes and communication. It is concerning that paternalistic attitudes still exist in healthcare. The medical community must proactively distance itself from outdated perspectives. To achieve the best outcomes, educational approaches should improve students’ self-confidence and understanding of the effectiveness of recommended interventions (Hibbard et al. 2005). The success of this approach depends on patient willingness and ability to report clinical errors and communicate with healthcare professionals. It is imperative to maintain an objective stance and refrain from making subjective evaluations. Moreover, in the perioperative setting, the implementation of health literacy-based techniques, such as the teach-back method, can promote patient participation. Numerous studies have highlighted the teach-back method as highly beneficial in collaborative healthcare (Miller et al. 2011; Tai-Seale et al. 2016).
Incorporating patient safety into health professional training curricula and promoting professional engagement are two approaches to overcoming these barriers. Additionally, education and health initiatives that provide targeted support for people with lower levels of education are important for promoting healthcare participation and improving patient safety. Measures are necessary to overcome barriers at different levels to promote active patient participation. This can improve health outcomes and patient safety.
Limitations
This scoping review covers a wide range of studies. However, limitations may arise owing to the focus on published research, which could exclude relevant unpublished data. The included studies varied in quality, methodology, and reporting, which may have affected the comparability and interpretability of the results. The aim of this scoping review is to provide a comprehensive overview of a broad field of research, but it does not include meta-analyses. The purpose of assessing the level of evidence is to offer guidance rather than make conclusive statements. It is possible that there may be variations in the effectiveness of the search strategies and coverage of the research field, which could result in the exclusion of relevant studies and affect the comprehensiveness of the review. In addition, the results may have been influenced by subjective assessments made by the authors and differences in interpretation. Efforts were made to reduce limitations by agreeing to the search strategy and continuously updating the assessment. The review focused only on published studies and did not include a systematic search of gray literature (unpublished or nontraditionally published sources), which may have resulted in the omission of important information.
Conclusion
This study provides insights into the impact of demographic and socioeconomic factors on patient involvement and patient safety in healthcare. Although patient-centered care is a top priority, barriers related to demographic and socioeconomic factors continue to impede equal access to information and decision-making. Research has highlighted the importance of clear and accessible communication between healthcare providers and patients. Providing quality information can increase the likelihood that patients will report medical errors. Unbiased information is essential to ensure fair access to healthcare for all individuals, regardless of demographic and socioeconomic factors. The implementation of tailored educational initiatives can enhance the accessibility of information to individuals from disadvantaged backgrounds.
Implications of the findings
-
Gender-Specific Approaches: It is of the utmost importance to recognize gender-specific differences in healthcare and adjust treatments and information accordingly.
-
Active Engagement of Elderly Patients: It is of particular importance to engage actively with elderly patients because they are a resilient population that values participation in healthcare decision-making processes.
-
Awareness of Ethnic Differences: It is of paramount importance to acknowledge and address ethnic disparities that can influence healthcare perceptions. It is of paramount importance to provide tailored support to enhance patient safety and well-being.
-
Education and Income as Healthcare Indicators: Education and income are two key indicators of healthcare status. Education and income can be used as indicators of an individual’s healthcare status. Higher education levels and income are correlated with a reduced incidence of medical errors. Therefore, improving access to education and health information is of utmost importance.
-
Promoting Health Literacy: Health literacy techniques, such as the teach-back approach, can enhance patient engagement and should be increasingly employed in healthcare.
-
Enhancing Health Literacy: Healthcare institutions should develop personalized educational and support programs for individuals with low health literacy or poor health, including medication management.
-
Building Partnership Relationships: It is of the utmost importance for open communication and partnerships between patients and healthcare providers to enhance patient safety.
-
Incorporating Social Factors into Healthcare Policies: Social factors must be incorporated into healthcare policies. It is of utmost importance for policy makers to acknowledge the pivotal role of social determinants in healthcare and allocate resources to programs designed to enhance care for diverse population groups.
-
Updating and Development of Practice: It is of the utmost importance to conduct regular reviews and updates of policies and practices to ensure their relevance in the context of evolving social dynamics and healthcare requirements within the population.
Data availability
The protocol is available upon submission of a reasonable request from the authors .
Code availability (software application or custom code)
Not applicable.
References
Abbate R, Di Giuseppe G, Marinelli P et al (2008) Patients’ knowledge, attitudes, and behavior toward hospital-associated infections in Italy. Am J Infect Control 36:39–47. https://doi.org/10.1016/j.ajic.2007.01.006
Adams RE, Boscarino JA (2004) A community survey of medical errors in New York. Int J Qual Health Care 16:353–362. https://doi.org/10.1093/intqhc/mzh063
Backman C, Stacey D, Crick M et al (2018) Use of participatory visual narrative methods to explore older adults’ experiences of managing multiple chronic conditions during care transitions. BMC Health Serv Res 18:482. https://doi.org/10.1186/s12913-018-3292-6
Bell SP, Schnipper JL, Goggins K et al (2016) Effect of pharmacist counseling intervention on health care utilization following hospital discharge: a randomized control trial. J Gen Intern Med 31:470–477. https://doi.org/10.1007/s11606-016-3596-3
Bell SK, Gerard M, Fossa A et al (2017) A patient feedback reporting tool for opennotes: implications for patient-clinician safety and quality partnerships. BMJ Qual Saf 26:312–322. https://doi.org/10.1136/bmjqs-2016-006020
Berger Z, Flickinger TE, Pfoh E et al (2014) Promoting engagement by patients and families to reduce adverse events in acute care settings: a systematic review. BMJ Qual Saf 23:548–555. https://doi.org/10.1136/bmjqs-2012-001769
Burroughs TE, Waterman AD, Gallagher TH et al (2007) Patients’ concerns about medical errors during hospitalization joint commission. J Qual Patient Safety 33:5–14. https://doi.org/10.1016/s1553-7250(07)33002-x
Butterworth JE, Hays R, McDonagh ST et al (2019) Interventions for involving older patients with multi-morbidity in decision-making during primary care consultations. The cochrane database of systematic reviews 2019. https://doi.org/10.1002/14651858.CD013124.pub2
Clare CA, Afzal O, Knapp K et al (2013) Determining a patient’s comfort in inquiring about healthcare providers’ hand-washing behavior. J Patient Safety 9:68–74. https://doi.org/10.1097/PTS.0b013e31827819d2
Clarivate Analytics (2023) EndNote (Version 21) [Computer software]. Clarivate Analytics. https://www.endnote.com. Accessed 15 Dec 2023
Cooper-Patrick L, Gallo JJ, Gonzales JJ et al (1999) Race, gender, and partnership in the patient-physician relationship. JAMA 282:583–589. https://doi.org/10.1001/jama.282.6.583
Davis RE, Koutantji M, Vincent CA (2008) How willing are patients to question healthcare staff on issues related to the quality and safety of their healthcare? an exploratory study. Qual Saf Health Care 17:90–96. https://doi.org/10.1136/qshc.2007.023754
Davis RE, Pinto A, Sevdalis N et al (2012) Patients’ and health care professionals’ attitudes towards the PINK patient safety video. J Eval Clin Pract 18:848–853. https://doi.org/10.1111/j.1365-2753.2011.01688.x
Doherty C, Stavropoulou C (2012) Patients’ willingness and ability to participate actively in the reduction of clinical errors: a systematic literature review. Soc Sci Med 75:257–263. https://doi.org/10.1016/j.socscimed.2012.02.056
Duhn L, Godfrey C, Medves J (2020) Scoping review of patients’ attitudes about their role and behaviours to ensure safe care at the direct care level. Health Expect: Int J Public Participation Health Care Health Policy 23:979–991. https://doi.org/10.1111/hex.13117
Eassey D, Smith L, Krass I et al (2016) Consumer perspectives of medication-related problems following discharge from hospital in Australia: a quantitative study. Int J Qual Health Care 28:391–397. https://doi.org/10.1093/intqhc/mzw047
Fonhus MS, Dalsbo TK, Johansen M et al (2018) Patient-mediated interventions to improve professional practice. Cochrane Database System Rev 9:CD012472. https://doi.org/10.1002/14651858.CD012472.pub2
Gordon HS, Street RL Jr, Sharf BF et al (2006) Racial differences in doctors’ information-giving and patients’ participation. Cancer 107:1313–1320. https://doi.org/10.1002/cncr.22122
Gray AM, Fenn P, Rickman N et al (2017) Changing experience of adverse medical events in the national health service: comparison of two population surveys in 2001 and 2013. Soc Sci Med 195:83–89. https://doi.org/10.1016/j.socscimed.2017.11.016
Hall J, Peat M, Birks Y et al (2010) Effectiveness of interventions designed to promote patient involvement to enhance safety: a systematic review. Qual Saf Health Care 19:e10. https://doi.org/10.1136/qshc.2009.032748
Hibbard JH, Peters E, Slovic P et al (2005) Can patients be part of the solution? Views on their role in preventing medical errors. Med Care Res Review: MCRR 62:601–616. https://doi.org/10.1177/1077558705279313
Hirt J, Nordhausen T (2019) Methoden und Theorienecke. Annu Rev Public Health 35:29–45
Hrisos S, Thomson R (2013) Seeing it from both sides: do approaches to involving patients in improving their safety risk damaging the trust between patients and healthcare professionals? An Inter Study PloS One 8:e80759. https://doi.org/10.1371/journal.pone.0080759
Kim JM, Suarez-Cuervo C, Berger Z et al (2018) Evaluation of patient and family engagement strategies to improve medication safety. Patient 11:193–206. https://doi.org/10.1007/s40271-017-0270-8
Lampert T, Richter M, Schneider S et al (2016) [Social inequality and health: status and prospects of socio-epidemiological research in Germany]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 59:153–165. https://doi.org/10.1007/s00103-015-2275-6
Longtin Y, Sax H, Leape LL et al (2010) Patient participation: current knowledge and applicability to patient safety. Mayo Clin Proc 85:53–62. https://doi.org/10.4065/mcp.2009.0248
Mackintosh NJ, Davis RE, Easter A et al (2020) Interventions to increase patient and family involvement in escalation of care for acute life-threatening illness in community health and hospital settings. Cochrane Database Syst Rev 12:CD012829. https://doi.org/10.1002/14651858.CD012829.pub2
Marmot M, Bell R (2012) Fair society, healthy lives. Public Health 126(Suppl 1):S4–S10. https://doi.org/10.1016/j.puhe.2012.05.014
Merner B, Schonfeld L, Virgona A et al (2023) Consumers' and health providers' views and perceptions of partnering to improve health services design, delivery and evaluation: a co-produced qualitative evidence synthesis. Cochrane Database System Rev 3:CD013274. https://doi.org/10.1002/14651858.CD013274.pub2
Microsoft (2024) Microsoft excel (Version 16) [Computer software]. Microsoft. https://www.microsoft.com. Accessed 15 Dec 2023
Miller MJ, Abrams MA, Earles B et al (2011) Improving patient-provider communication for patients having surgery: patient perceptions of a revised health literacy-based consent process. J Patient Safety 7:30–38. https://doi.org/10.1097/PTS.0b013e31820cd632
Nikoloski Z, Mossialos E (2013) Corruption, inequality and population perception of healthcare quality in Europe. BMC Health Serv Res 13:472. https://doi.org/10.1186/1472-6963-13-472
OCEBM Levels of Evidence Working Group (2012) “The oxford levels of evidence 2” Oxford centre for evidence–based medicine. https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence
Ocloo J, Garfield S, Franklin BD et al (2021) Exploring the theory, barriers and enablers for patient and public involvement across health, social care and patient safety: a systematic review of reviews. Health Res Policy Syst 19:8. https://doi.org/10.1186/s12961-020-00644-3. Accessed 15 Dec 2023
Pandhi N, Schumacher J, Flynn KE et al (2008) Patients’ perceptions of safety if interpersonal continuity of care were to be disrupted. Health Expect: Int J Public Participation Health Care Health Policy 11:400–408. https://doi.org/10.1111/j.1369-7625.2008.00503.x
Peters MD, Godfrey C, McInerney P et al (2020) Chapter 11: scoping reviews (2020 version). In: Aromataris E MZ (ed) Joanna Briggs Institute reviewer’s manual. https://doi.org/10.46658/JBIMES-20-12
Ricci-Cabello I, Reeves D, Bell BG et al (2017) Identifying patient and practice characteristics associated with patient-reported experiences of safety problems and harm: a cross-sectional study using a multilevel modelling approach. BMJ Qual Saf 26:899–907. https://doi.org/10.1136/bmjqs-2016-006411
Robert Koch-Institut (2017) Gesundheitliche Ungleichheit in verschiedenen Lebensphasen. Gesundheitsberichterstattung des Bundes. Berlin. https://doi.org/10.17886/RKI-GBE-2017-003
Schubert I, Egen-Lappe V, Heymans L et al (2009) “To read” does not imply “to act upon”: indicators of the acceptance of general practice guidelines. Results of a survey among quality circles of general practitioner centred care (Hausarztzentrierte Versorgung; HZV). Z Evid Fortbild Qual Gesundhwes 103:5–12. https://doi.org/10.1016/j.zefq.2008.12.017
Schwappach DL, Frank O, Koppenberg J et al (2011) Patients’ and healthcare workers’ perceptions of a patient safety advisory. Int J Qual Health Care 23:713–720. https://doi.org/10.1093/intqhc/mzr062
Sheiham A (2009) Closing the gap in a generation: health equity through action on the social determinants of health. A report of the WHO Commission on Social Determinants of Health (CSDH) 2008. Commun Dent Health 26:2–3
Snyder H, Engstrom J (2016) The antecedents, forms and consequences of patient involvement: a narrative review of the literature. Int J Nurs Stud 53:351–378. https://doi.org/10.1016/j.ijnurstu.2015.09.008
Tai-Seale M, Elwyn G, Wilson CJ et al (2016) Enhancing shared decision making through carefully designed interventions that target patient and provider behavior. Health Aff (millwood) 35:605–612. https://doi.org/10.1377/hlthaff.2015.1398
The Joint Commission (2023) National patient safety goals®. Effective January 2024 for the hospital program. Joint Commission. https://www.jointcommission.org/standards/national-patient-safety-goals/hospital-national-patientsafety-goals/. Accessed 15 Dec 2023
Thompson SC, Pitts JS, Schwankovsky L (1993) Preferences for involvement in medical decision-making: situational and demographic influences. Patient Educ Couns 22:133–140. https://doi.org/10.1016/0738-3991(93)90093-c
Tricco AC, Lillie E, Zarin W et al (2018) PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 169:467–473. https://doi.org/10.7326/M18-0850
Trier H, Valderas JM, Wensing M et al (2015) Involving patients in patient safety programmes: a scoping review and consensus procedure by the LINNEAUS collaboration on patient safety in primary care. Eur J Gen Pract 21(Suppl):56–61. https://doi.org/10.3109/13814788.2015.1043729
Wachtel RE, Dexter F (2013) Difficulties and challenges associated with literature searches in operating room management, complete with recommendations. Anesth Analg 117:1460–1479. https://doi.org/10.1213/ANE.0b013e3182a6d33b
Wang CJ, Fetzer SJ, Yang YC et al (2013) The impacts of using community health volunteers to coach medication safety behaviors among rural elders with chronic illnesses. Geriatr Nurs 34:138–145. https://doi.org/10.1016/j.gerinurse.2012.12.013
Willems S, De Maesschalck S, Deveugele M et al (2005) Socio-economic status of the patient and doctor–patient communication: does it make a difference? Patient Educ Couns 56:139–146
Williams DR, Mohammed SA, Leavell J et al (2010) Race, socioeconomic status, and health: complexities, ongoing challenges, and research opportunities. Ann N Y Acad Sci 1186:69–101. https://doi.org/10.1111/j.1749-6632.2009.05339.x
World Health Organization (2006) London declaration: patients for patient safety. Geneva, Switzerland
Yousif MA (2002) In-home drug storage and utilization habits: adanese study. East Mediterr Health J 8:422–431
Funding
Open Access funding enabled and organized by Projekt DEAL. No funds, grants, or other support were received.
Author information
Authors and Affiliations
Contributions
Clara Monaca: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing, Idea for the article, Literature search and data analysis, and Drafted the work. Antje Hammer: Conceptualization, Investigation, Methodology, Software, Supervision, Validation, Writing – review & editing, Literature search and data analysis Matthias Weigl: Methodology, Supervision, Writing – review & editing. Holger Pfaff: Methodology , Supervision, Writing – review & editing.
Corresponding author
Ethics declarations
Ethic approval
Not applicable. No ethical approval was required for this scoping review because it did not include involved active (patient) participants.
Consent to publish the study
Not applicable.
Consent to participate
Not applicable.
Conflict of interest
The authors declare no competing interests relevant to the content of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Monaca, C., Weigl, M., Pfaff, H. et al. Patient involvement in patient safety measures: the impact of demographic and socioeconomic factors – a scoping review. J Public Health (Berl.) (2024). https://doi.org/10.1007/s10389-024-02340-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10389-024-02340-w