Abstract
Purpose
The effectiveness of current follow-up guidelines after breast cancer treatment is uncertain. Tailored surveillance based on patient age and tumor characteristics may be more adequate. This study aimed to analyze the frequency of ipsilateral locoregional recurrences (LR) and second primary breast cancers (SP) detected outside of scheduled surveillance and to analyze risk factors associated with these events.
Methods
Patients with surgically treated early-stage breast cancer from the Malmö Diet and Cancer Study (MDCS), 1991–2014 (n = 1080), and the Västernorrland region, 2009–2018 (n = 1648), were included. Clinical and pathological information on the primary tumor and recurrences was retrieved from medical records. The mode of recurrence detection was defined as detection within (planned) or outside (symptomatic) of scheduled surveillance.
Results
The median follow-up was 6.5 years. Overall, 461 patients experienced a recurrence. The most common initial event was distant metastasis (47%), followed by locoregional recurrence (LR) (22%) and second primary (SP) (18%). 56% of LR and 28% of SP were identified outside of scheduled surveillance. Logistic regression analysis revealed that younger age (under 50 years) (OR 2.57, 95% CI 1.04–6.88), lymph node-positive breast cancer (OR 2.10, 95% CI 1.03–4.39) and breast cancer of the HER2 positive subtype (OR 5.24, 95% CI 1.40–25.90) were correlated with higher odds of detecting a recurrence outside of planned surveillance.
Conclusion
Most recurrent events were detected outside of scheduled surveillance, particularly for locoregional recurrences. Risk-based surveillance, which takes into account patient and tumor characteristics, might be more suitable for specific patient subsets.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of breast cancer is escalating due to both an increased incidence and improved 5-year survival rates, which surpass 90% in high-income countries [1, 2]. The surveillance of individuals after breast cancer treatment aims to detect curable recurrences, provide psychosocial support, and monitor side effects of completed and ongoing adjuvant treatments [3,4,5]. However, there is a paucity of evidence-based data to optimally design surveillance programs concerning frequency, modality, and duration of follow-up care in cancer survivors [6]. Observational studies imply that early detection of ipsilateral recurrences or secondary primary breast cancers in the contra-lateral breast confers survival benefits [7, 8]. A meta-analysis involving thirteen studies indicated that survival improves by a hazard ratio of 1.68 (95% confidence interval (CI) 1.48–1.91) in patients with asymptomatic recurrences as compared to symptomatic ones, and it improves by 2.44 (95% CI 1.78–3.35) when the recurrence is identified via mammography rather than a physical examination [7]. Conversely, a 2019 Cochrane review of randomized trials suggested that less intensive follow-up compared to a more rigorous one probably delays the detection of recurrence without altering overall survival [6]. Most local and regional recurrences are detected outside of organized surveillance [9,10,11], and randomized controlled trials have failed to show that reduced in-hospital follow-up strategies negatively impact either patient-reported outcomes or the early detection of recurrence [4].
The overall risk of loco-regional recurrent breast cancer is low (0.3–0.5% per year after breast conserving therapy) [12], but, to detect a recurrence is of great importance to the affected women. The risk is highest in the first five years, peaking in the second year after treatment and varies based on the patient’s age, features of the initial breast cancer (such as tumor stage, nodal stage, tumor biological subtype), and adjuvant treatments [13,14,15,16,17]. Despite this, no individualized, risk-based follow-up is currently implemented. With increased knowledge, women may be subject to more intense follow-up, but importantly, also less intense follow-up because they are time-consuming and costly for both caregivers and patients.
With the aim of establishing a personalized surveillance system, a comprehensive retrospective analysis of current follow-up practices and patient outcomes is essential. The objective of this study was to examine the frequency of detecting ipsilateral locoregional recurrences (LR) and secondary primary breast cancers (SP) beyond scheduled surveillance, and to analyze risk factors associated with these events in patients suffering from recurring breast cancer.
Patients and methods
The study population was retrieved from two different cohorts.
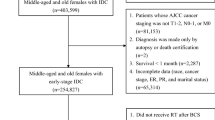
Malmö diet and cancer study (MDCS)
The Malmö Diet and Cancer Study (MDCS) [18, 19] encompassed inhabitants of Malmö from 1991 to 1996, of whom 17,035 were women. The cohort features data on vital status, causes of death, and cancer diagnoses, which are regularly updated through the Swedish Cancer Registry and the Swedish Cause of Death Registry. All women in the cohort diagnosed with breast cancer (from 1991 to 2014) were identified. Women with prevalent breast cancer at baseline (n = 576), bilateral breast cancer (n = 21), or cancer in situ (n = 105) were excluded. Additionally, 16 patients were excluded due to metastatic disease present at the initial breast cancer diagnosis, and 18 patients were excluded due to missing information regarding breast cancer recurrence. A total of 1080 women remained eligible for inclusion after implementing the exclusion criteria.
Information about clinicopathological factors in the MDCS has been described in detail in a previous publication [20]. The status of axillary lymph node involvement was obtained from medical records. Hormone receptor status, based on immunohistochemical (IHC) staining, was extracted from Tissue Microarray (TMA) evaluations from 1991 to 2004 and medical records from 2005 to 2014. The Human Epidermal Growth Factor Receptor 2 (HER2) status was gathered from TMA assessments from 1991 to 2007 and from medical records from 2008 to 2014. Information on IHC proliferation marker Ki67 expression was collected over three periods: from TMA assessments between 1991 and 2004 and 2005–2007, and from medical records from 2008 to 2014. The tumors were then classified into surrogate molecular breast cancer subtypes according to the St. Gallen 2013 guidelines (25). The classifications used: Luminal A-like (ER > 10%, HER2 negative, and Ki67 low), Luminal B-like (ER > 10%, HER2 negative and Ki67 high or Ki67 intermediate and PR < 10%), HER2 + subtype (any ER, PR, Ki67, and HER2 positive), and Triple Negative Breast Cancer (TNBC) (ER < 10%, PR < 10%, HER2 negative, and any Ki67).
The MDCS was conducted according to the Declaration of Helsinki and received approval from the Ethics Review Board in Lund, Sweden (Official Records Nos. 652/2005, 166/2007, and 2014/830) as well as the Swedish Ethical Review Authority (2022-04473-02). In the present study, a subset of women from the MDCS cohort was included, and they provided their informed consent at the baseline.
Region Västernorrland
Women with breast cancer in the Västernorrland region between 2009 and 2018 were identified from The Swedish National Breast Cancer Quality Registry (n = 2090). This registry has had national coverage since 2007 and includes all incident breast cancers in Sweden, with reported completeness close to 100% [21]. Women initially diagnosed with metastatic disease (n = 79), those who did not undergo surgery due to other reasons (n = 81), women with synchronous bilateral cancer (n = 29), and women with cancer in situ (n = 253) were excluded. These exclusions left 1648 women eligible for the analyses.
The age at diagnosis, nodal status, breast surgery, hormone receptor status, HER2 status, and Ki67 of the index breast cancer were obtained from medical records. The Swedish Ethical Review Authority approved the data collection for this study (2020-02165 and 2024-00428-02), waiving the need to secure informed consent.
Follow-up routines and outcomes
In MDCS, the recommended follow-up after breast cancer treatment included annual mammography for ten years for patients who underwent breast-conserving surgery (BCS). Patients treated with mastectomy were incorporated into the standard screening program. The schedule for in-hospital physical examinations varied during the study period, primarily comprising annual visits for the first three years and capped off with a final visit at five years post-diagnosis.
In Västernorrland, recommended follow-up included annual bilateral mammography for five years for all patients, regardless of whether BCS or mastectomy had been performed. Further, patients receiving adjuvant chemotherapy were also offered annual in-hospital physical examinations for a duration of 5 years.
Recurrent events were defined in accordance with the consensus on event definitions for classifying recurrence in breast cancer, as published in 2014 [22].
The time of follow-up initiated at the date of diagnosis and concluded at the date of the first relapse either in the ipsilateral breast, scar, chest wall, or ipsilateral regional lymph nodes (LR) or in the instance of a second primary breast cancer in the contralateral breast (SP) or distant metastasis including contralateral regional lymphnodes as the first event (DM). Patients experiencing synchronous bilateral locoregional events were designated as LR, and those with LR or SP and synchronous DM as the initial event were classified as LR + DM. HS (MDSC) and CW (Västernorrland) retrospectively reviewed the mode of recurrence detection (planned or symptomatic) within the scope of this present study. Recurrent events were deemed symptomatic when identified at a patient-oriented visit or breast imaging outside of scheduled surveillance.
Statistics
To investigate whether the variables - age at diagnosis, nodal stage, subtype, or type of surgery - were associated with a larger proportion of recurrences detected outside of scheduled surveillance, a multivariable logistic regression model was applied. This analysis included LR, SP and LR + DM but excluded patients with DM only because distant metastases are typically detected symptomatically and scheduled surveillance for detecting DM is not recommended. A composite model that used the type of recurrence (LR, SP and LR + DM) as a covariate was applied. Hence the result should be interpreted conditional on getting LR, SP or LR + DM. Given that this study focused on variables associated with the risk of symptomatic detection, no formal time-to-event analysis of the risk of recurrence was performed. Only summary measures of the size of the four groups - LR, SP, LR + DM, and DM - and the time from diagnosis to recurrence were provided.
Results
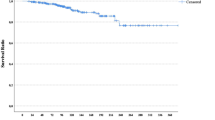
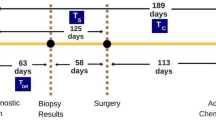
The years of breast cancer diagnosis for the two separate cohorts are displayed in Fig. 1. The women in the MDCS cohort received their breast cancer diagnoses during an earlier period compared to the women in the Västernorrland cohort, with a 6-year overlap. The median age at the time of breast cancer diagnosis was 66 years (interquartile range, IQR: 59–72), and the median follow-up period was 6.5 years (IQR: 3.8–10.0) (Table 1).
In total, 461 patients experienced a recurring event. The median time to recurrence was 4.31 years (IQR 2.05–8.19 years) (Suppl Table 1). The distribution of the first relapse in the two distinct cohorts is illustrated in Table 2. The most common initial event was DM (47%), followed by LR (22%) and SP (18%).
Table 3 illustrates the distribution of recurrences categorized by age at the time of primary breast cancer diagnosis, tumor subtype, nodal stage, and type of breast surgery. DM as the initial event was most prevalent in patients with Luminal B-like (81 of 126, 64.3%) and HER2 positive tumors (26 of 45, 57.8%), whereas it was least prevalent in patients with Luminal A-like tumors (49 of 144, 34.0%). Moreover, DM as the initial event was notably common in patients with lymph node-positive primary breast cancer (141 of 203, 69.5%) and in patients who had undergone a mastectomy, as opposed to those who had BCS (144 of 247, 58.3%).
Risk of recurrence detected outside of scheduled surveillance
Overall, 298 out of 417 (71.5%) first recurrent events were detected outside of scheduled surveillance (Table 4). Of the ipsilateral LR, 53 out of 95 (56%) were detected outside of scheduled surveillance, while 54 out of 75 (72%) SPs in the contralateral breast were identified during scheduled mammography appointments. Almost all DMs were detected due to symptoms, with 183 out of 193 (95%) cases.
Recurrence detection in relation to index breast cancer features
After excluding patients whose first event was DM, a logistic regression analysis was executed to identify risk factors for the detection of symptomatic LR and SP. This analysis revealed that young age (< 50 years) (OR 2.57, 95% CI 1.04–6.88), lymph node-positive breast cancer (OR 2.10, 95% CI 1.03–4.39), and HER2-positive subtype breast cancer (OR 5.24, 95% CI 1.40–25.90) were associated with an increased likelihood of recurrence detection outside of scheduled surveillance (Table 5).
Discussion
This study corroborates previous research, stating that a majority of all recurrences (71.5%), which includes distant metastasis, and 56.0% of ipsilateral locoregional recurrences are discovered outside of scheduled surveillance (9–11, 22–24). There were fewer overall recurrences in Västernorrland, reflecting the more contemporary period of breast cancer diagnoses in this population. However, the proportions of LR, SP and DM were notably similar between the two cohorts. Importantly, the probability of detecting a recurrence outside of surveillance was higher among younger patients, patients with lymph node-positive breast cancer, and cases of the HER2-positive breast cancer subtype.
Locoregional recurrences
The effectiveness of current surveillance programs has been previously examined, yielding mixed results. The reported proportion of ipsilateral recurrent events identified through scheduled annual mammography varies between 8% and 51% [9, 11, 23,24,25]. In contrast, recurrence detected during routine physical examinations is rare [9, 26, 27].
Governmental institutions and medical societies typically recommend annual bilateral mammography following breast-conservative surgery, while most suggest only contralateral mammography for patients who underwent a mastectomy [3, 4, 28,29,30]. Routine ultrasound, however, is not advised [28]. The benefits of digital breast tomography and magnetic resonance imaging (MRI) in routine surveillance remain unclear. MRI is suggested to be more beneficial for young women (i.e., those under 50 years) or women at higher risk of recurrence, such as those with dense breasts or a first-degree family history [29, 30]. The effectiveness of more frequent mammography intervals remains unconfirmed [31,32,33].
Advancements in breast cancer management have led to a decline in the overall rate of locoregional recurrences [12, 14, 16]. Currently, the estimated LR risk following breast-conserving surgery (BCS) coupled with whole breast radiotherapy is reported to be 0.3–0.5% per year. The annual risk of SP breast cancer is approximately 0.4% per year [12, 34]. This prompts the question of whether follow-up could be de-escalated, at least for certain subsets of patients. The preliminary results from the Mammo-50 trial in the UK were recently presented, where 5000 female patients aged over 50 who were relapse-free following 3 years of standard surveillance were randomized between less frequent mammograms and continued annual mammograms. After a median follow-up of 5.7 years, there was no difference in survival, recurrence rates, or quality of life [35]. This data suggests that less intensive surveillance is feasible for patients with a predicted low risk of recurrence.
Second primary
The effectiveness of mammography surveillance seems to be more significant for the detection of SP breast cancer, a result that aligns with this study [9, 11, 25, 36]. SP in the opposite breast often gets detected at an earlier stage compared to the initial breast cancer [36]. Nonetheless, the survival benefit of early SP detection remains uncertain due to the competing risk posed by the primary breast cancer [36].
Personalized risk-based surveillance
In the era of personalized precision medicine, specifically pertaining to breast cancer treatment, surveillance recommendations remain generalized. Despite the variations in recurrence risk by age, tumor subtype, and nodal stage [14,15,16,17], current surveillance methods lack individualization. Furthermore, it is not well-examined whether early detection of recurrences is more beneficial, contingent upon patient and tumor characteristics. In other words, it remains to be seen whether more intensive surveillance would be advantageous for certain individuals. A recent observational study suggested that asymptomatic imaging, compared to symptomatic presentation of DM, was associated with a lower risk of death for triple-negative and HER2-positive breast cancer. However, it did not make a significant difference for the luminal-like breast cancers [37]. Whether this also applies for in-breast recurrences is unclear. In the present study, young age, lymph node-positive breast cancer, and HER2-positive subtype were associated with symptomatic detection of recurrences. This possibly indicates that these patients could benefit from more intensive surveillance, including supplemental imaging, during the early follow-up years. To better assist personalized follow-up strategies, the INFLUENCE 1.0 nomogram was developed in the Netherlands in 2015. This nomogram underwent further development in 2021 (INFLUENCE 2.0) and 2024 (INFLUENCE 3.0) [15, 38, 39]. It estimates an individualized risk of recurrence based on age, mode of detection, type of surgery, grade, nodal stage, multifocality, hormone receptor status, HER2 status, and adjuvant treatments.
This tool ought to be advantageous for personalized follow-up regimes. With local recurrence rates decreasing, it presents an opportunity to lessen surveillance for patients with an exceptionally low risk of recurrence. Further refinement in the accuracy of risk prediction models, validated across a diverse set of breast cancer survivors, would be beneficial for the development of risk-based imaging surveillance. High breast density at the time of primary breast cancer diagnosis correlates with an increased risk of recurrence and could, therefore, be incorporated into a model for tailored surveillance in a prospective study design [40].
Several methodological issues require attention. Firstly, in the current study, data pertaining to follow-up and detection methods of recurrences were gathered retrospectively from a large combined study population spanning two distinct geographical areas. Covering a period from 1991 to 2019 means that the study displays both strengths and limitations–treatments have progressed, and surveillance routines have varied over this period and between the two cohorts, potentially impacting the interpretation of the results. The surveillance routines in the MDCS cohort and the Västernorrland cohort varied in both interval and duration. In the MDCS, surveillance interval was stratified by surgery while all breast cancer patients in Västernorrland underwent yearly mammography. Clinical examinations have been de-escalated over time in both cohorts. Secondly, one limitation is the retrospective gathering of data, which requires the retrospective assessment of medical journals and radiologic reports to determine if mammography was performed within or outside scheduled surveillance. Additionally, information on the adherence to scheduled surveillance among all patients in the study population was not available.
In conclusion, even though the risk of recurrence varies with patient age and tumor characteristics, surveillance recommendations remain generalized. Most recurrences are detected outside of scheduled surveillance. This study indicates that young age, lymph node-positive breast cancer, and breast cancer of the HER2-positive subtype may call for more intensive surveillance.
Data availability
No datasets were generated or analysed during the current study.
References
Arnold M, Morgan E, Rumgay H et al (2022) Current and future burden of breast cancer: global statistics for 2020 and 2040. Breast 66:15–23. https://doi.org/10.1016/j.breast.2022.08.010
Miller KD, Nogueira L, Devasia T et al (2022) Cancer treatment and survivorship statistics, 2022. CA Cancer J Clin 72:409–436. https://doi.org/10.3322/caac.21731
Senkus E, Kyriakides S, Ohno S et al (2015) Primary breast cancer: ESMO Clinical Practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 26:v8–v30. https://doi.org/10.1093/annonc/mdv298
Khatcheressian JL, Hurley P, Bantug E et al (2013) Breast Cancer Follow-Up and Management after Primary Treatment: American Society of Clinical Oncology Clinical Practice Guideline Update. J Clin Oncol 31:961–965. https://doi.org/10.1200/JCO.2012.45.9859
RCC Nationellt vårdprogram bröstcancer
Høeg BL, Bidstrup PE, Karlsen RV et al (2019) Follow-up strategies following completion of primary cancer treatment in adult cancer survivors. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD012425.pub2. 2019:
Lu WL, Jansen L, Post WJ et al (2009) Impact on survival of early detection of isolated breast recurrences after the primary treatment for breast cancer: a meta-analysis. Breast Cancer Res Treat 114:403–412. https://doi.org/10.1007/s10549-008-0023-4
Houssami N, Ciatto S, Martinelli F et al (2009) Early detection of second breast cancers improves prognosis in breast cancer survivors. Ann Oncol 20:1505–1510. https://doi.org/10.1093/annonc/mdp037
Geurts SME, De Vegt F, Siesling S et al (2012) Pattern of follow-up care and early relapse detection in breast cancer patients. Breast Cancer Res Treat 136:859–868. https://doi.org/10.1007/s10549-012-2297-9
Saltbæk L, Horsboel TA, Offersen BV et al (2020) Patterns in detection of recurrence among patients treated for breast cancer. Breast Cancer Res Treat 184:365–373. https://doi.org/10.1007/s10549-020-05847-4
Beltran-Bless A-A, Alshamsan B, Alzahrani MJ et al (2023) Regularly scheduled physical examinations and the detection of breast cancer recurrences. Breast 69:274–280. https://doi.org/10.1016/j.breast.2023.03.004
Aalders KC, Van Bommel ACM, Van Dalen T et al (2016) Contemporary risks of local and regional recurrence and contralateral breast cancer in patients treated for primary breast cancer. Eur J Cancer 63:118–126. https://doi.org/10.1016/j.ejca.2016.05.010
Colleoni M, Sun Z, Price KN et al (2016) Annual Hazard Rates of recurrence for breast Cancer during 24 years of Follow-Up: results from the international breast Cancer Study Group trials I to V. J Clin Oncol 34:927–935. https://doi.org/10.1200/JCO.2015.62.3504
Braunstein LZ, Taghian AG, Niemierko A et al (2017) Breast-cancer subtype, age, and lymph node status as predictors of local recurrence following breast-conserving therapy. Breast Cancer Res Treat 161:173–179. https://doi.org/10.1007/s10549-016-4031-5
Witteveen A, Vliegen IMH, Sonke GS et al (2015) Personalisation of breast cancer follow-up: a time-dependent prognostic nomogram for the estimation of annual risk of locoregional recurrence in early breast cancer patients. Breast Cancer Res Treat 152:627–636. https://doi.org/10.1007/s10549-015-3490-4
Schumacher JR, Wiener AA, Greenberg CC et al (2023) Local/Regional Recurrence Rates after breast-conserving therapy in patients enrolled in legacy trials of the Alliance for clinical trials in Oncology (AFT-01). Ann Surg 277:841–845. https://doi.org/10.1097/SLA.0000000000005776
Cheun J-H, Kim H-K, Moon H-G et al (2023) Locoregional recurrence patterns in patients with different molecular subtypes of breast Cancer. JAMA Surg 158:841. https://doi.org/10.1001/jamasurg.2023.2150
Manjer J, Carlsson S, Elmståhl S et al (2001) The Malmö diet and cancer study: representativity, cancer incidence and mortality in participants and non-participants. Eur J Cancer Prev 10:489–499. https://doi.org/10.1097/00008469-200112000-00003
Manjer J, Elmstahl S, Janzon L, Berglund G (2002) Invitation to a population-based cohort study: differences between subjects recruited using various strategies. Scand J Public Health 30:103–112. https://doi.org/10.1177/14034948020300020401
Sturesdotter L, Sandsveden M, Johnson K et al (2020) Mammographic tumour appearance is related to clinicopathological factors and surrogate molecular breast cancer subtype. Sci Rep 10:20814. https://doi.org/10.1038/s41598-020-77053-7
Löfgren L, Eloranta S, Krawiec K et al (2019) Validation of data quality in the Swedish National Register for Breast Cancer. BMC Public Health. https://doi.org/10.1186/s12889-019-6846-6
Moossdorff M, Van Roozendaal LM, Strobbe LJA et al (2014) Maastricht Delphi Consensus on Event Definitions for Classification of Recurrence in Breast Cancer Research. JNCI J Natl Cancer Inst. https://doi.org/10.1093/jnci/dju288
Voogd AC, Van Tienhoven G, Peterse HL et al (1999) Local recurrence after breast conservation therapy for early stage breast carcinoma: detection, treatment, and outcome in 266 patients. Cancer 85:437–446
Montgomery DA, Krupa K, Jack WJL et al (2007) Changing pattern of the detection of locoregional relapse in breast cancer: the Edinburgh experience. Br J Cancer 96:1802–1807. https://doi.org/10.1038/sj.bjc.6603815
Houssami N, Ciatto S (2010) Mammographic surveillance in women with a personal history of breast cancer: how accurate? How Effective? Breast 19:439–445. https://doi.org/10.1016/j.breast.2010.05.010
Montgomery DA, Krupa K, Cooke TG (2007) Follow-up in breast cancer: does routine clinical examination improve outcome? A systematic review of the literature. Br J Cancer 97:1632–1641. https://doi.org/10.1038/sj.bjc.6604065
Lu W, De Bock GH, Schaapveld M et al (2011) The value of routine physical examination in the follow up of women with a history of early breast cancer. Eur J Cancer 47:676–682. https://doi.org/10.1016/j.ejca.2010.11.006
Swinnen J, Keupers M, Soens J et al (2018) Breast imaging surveillance after curative treatment for primary non-metastasised breast cancer in non-high-risk women: a systematic review. Insights Imaging 9:961–970. https://doi.org/10.1007/s13244-018-0667-5
Cho N, Han W, Han B-K et al (2017) Breast Cancer Screening with Mammography Plus Ultrasonography or magnetic resonance imaging in women 50 years or younger at diagnosis and treated with breast conservation therapy. JAMA Oncol 3:1495. https://doi.org/10.1001/jamaoncol.2017.1256
Houssami N, Abraham LA, Kerlikowske K et al (2013) Risk factors for second screen-detected or interval breast cancers in women with a personal history of breast Cancer participating in Mammography Screening. Cancer Epidemiol Biomarkers Prev 22:946–961. https://doi.org/10.1158/1055-9965.EPI-12-1208-T
McNaul D, Darke M, Garg M, Dale P (2013) An evaluation of post-lumpectomy recurrence rates: is follow‐up every 6 months for 2 years needed? J Surg Oncol 107:597–601. https://doi.org/10.1002/jso.23298
Arasu VA, Joe BN, Lvoff NM et al (2012) Benefit of Semiannual Ipsilateral Mammographic Surveillance following breast conservation therapy. Radiology 264:371–377. https://doi.org/10.1148/radiol.12111458
Gunia SR, Merrigan TL, Poulton TB, Mamounas EP (2012) Evaluation of appropriate short-term mammographic surveillance in patients who undergo breast-conserving surgery (BCS). Ann Surg Oncol 19:3139–3143. https://doi.org/10.1245/s10434-012-2578-x
Giannakeas V, Lim DW, Narod SA (2021) The risk of contralateral breast cancer: a SEER-based analysis. Br J Cancer 125:601–610. https://doi.org/10.1038/s41416-021-01417-7
Dunn J (2023) Mammographic surveillance in early breast cancer patients aged 50 years or over: results of the Mammo-50 non-inferiority trial of annual versus less frequent mammography. In: SABCS. https://aacrjournals.org/cancerres/article/84/9_Supplement/GS03-02/743392/Abstract-GS03-02-Mammographic-surveillance-in
Grunfeld E, Noorani H, McGahan L et al (2002) Surveillance mammography after treatment of primary breast cancer: a systematic review. Breast 11:228–235. https://doi.org/10.1054/brst.2001.0404
Schumacher JR, Neuman HB, Yu M et al (2022) Surveillance Imaging vs Symptomatic Recurrence Detection and survival in stage II-III breast Cancer (AFT-01). JNCI J Natl Cancer Inst 114:1371–1379. https://doi.org/10.1093/jnci/djac131
Völkel V, Hueting TA, Draeger T et al (2021) Improved risk estimation of locoregional recurrence, secondary contralateral tumors and distant metastases in early breast cancer: the INFLUENCE 2.0 model. Breast Cancer Res Treat 189:817–826. https://doi.org/10.1007/s10549-021-06335-z
Maaren MV, Hueting T, Uden DV et al (2024) The INFLUENCE 3.0 model: updated predictions of locoregional recurrence and contralateral breast cancer, now also suitable for patients treated with neoadjuvant systemic therapy
Lång K, Sturesdotter L, Bengtsson Y et al (2024) Mammographic features at primary breast cancer diagnosis in relation to recurrence-free survival. Breast 75:103736. https://doi.org/10.1016/j.breast.2024.103736
Acknowledgements
Anders Dahlin, MDCS, for data managing.
Funding
Open access funding provided by Umea University. This work was supported by the Swedish governmental funding for clinical research (ALF), RegionVästernorrland (Visare Norr) and The Swedish Breast Cancer Association.
Author information
Authors and Affiliations
Contributions
Hanna Sartor: Conceptualization, Data curation, Methodology, Writing - original draft, Writing—review & editing. Oskar Hagberg: Methodology, Formal analysis, Writing—review & editing. Oskar Hemmingsson: Conceptualization, Writing—review & editing. Kristina Lång: Conceptualization, Methodology, Writing—review & editing. Charlotta Wadsten: Conceptualization, Data curation, Methodology, Writing—original draft, Writing—review & editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study was conducted according to the Declaration of Helsinki. The Malmö Diet Cancer Study received approval from the Ethics Review Board in Lund, Sweden (Official Records Nos. 652/2005, 166/2007, and 2014/830) as well as the Swedish Ethical Review Authority (2022-04473-02). The women from the MDCS cohort included in this study provided their informed consent at the baseline. For the Västernorrland region, the Swedish Ethical Review Authority approved the data collection (2020–02165 and 2024-00428-02), waiving the need to secure informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sartor, H., Hagberg, O., Hemmingsson, O. et al. Breast cancer recurrence in relation to mode of detection: implications on personalized surveillance. Breast Cancer Res Treat (2024). https://doi.org/10.1007/s10549-024-07475-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10549-024-07475-8