Abstract
Purpose
Pro-angiogenic factors are positively associated with breast tumor staging and poorer prognosis, but their role in the etiology of breast cancer has not been assessed.
Methods
We measured serum levels of the pro-angiogenic vascular endothelial growth factor A (VEGF), and placental growth factor (PlGF) and anti-angiogenic soluble fms-like tyrosine kinase-1 (sFlt-1) in 352 incident breast cancer cases [mean age at diagnosis 67 (range 55–83)] and 352 non-cases in the prostate, lung, colorectal, and ovarian screening trial (women enrolled 1993–2001, followed through 2005) matched on age and date of enrollment. Cases were followed on average 4.2 years from blood draw to diagnosis, range 3.9–12.8 years; 53 % were estrogen receptor positive/progesterone receptor positive (ER+/PR+), and 13 % were ER−/PR−. Quartile-specific hazard ratios (HR) and 95 % confidence intervals (CI) were estimated using weighted Cox proportional hazards regression models adjusted for known breast cancer risk factors. An ordinal variable for the angiogenic markers was used to test for trend in the HR.
Results
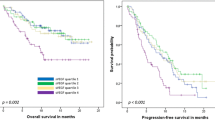
Comparing the highest to lowest quartile, multivariable HR were 0.90 for VEGF (95 % CI 0.33–2.43, p trend = 0.88), 1.38 for sFlt-1 (95 % CI 0.63–3.04, p trend = 0.63), and 0.62 for PlGF (95 % CI 0.19–2.00, p trend = 0.73). Risk patterns were not altered when all angiogenic markers were included in the model simultaneously, or by restricting analyses to invasive breast cancers, to cases diagnosed two or more years after blood collection or to ER+ tumors.
Conclusions
There was no evidence of an increased breast cancer risk associated with circulating levels of pro-angiogenic markers VEGF and PlGF or a reduced risk with circulating levels of anti-angiogenic marker sFlt-1.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Numerous studies show poorer survival in women with breast cancer tumors that overexpress angiogenesis-promoting proteins including VEGF (also known as VEGF-A) [1–4] and PlGF (a member of the VEGF family) [5, 6], but the prognostic utility of these markers in newly diagnosed cancer is not clear [1, 7, 8], and their potential etiologic roles in breast cancer have not been well studied. A few studies have compared circulating levels of some of these factors in breast cancer cases to non-cases [9–12], but none have done so in prospectively collected bloods.
While angiogenesis is a quiescent process in most adult tissues, it is critical to normal physiologic processes such as inflammation, wound healing, embryogenesis, and the menstrual cycle, as well as to the pathologic processes of tumor growth and metastasis. It entails a complex coordination between pro- and anti-angiogenic factors, and increasing evidence suggests that sex steroids may regulate their production in a tissue-specific manner. Additionally, women with a history of preeclampsia, who during their pregnancy experience pronounced elevations in the anti-angiogenic factor sFlt-1 (also known as soluble VEGF receptor 1) along with low circulating VEGF and PlGF, have a reduced risk of subsequent breast cancer [13–16]. Elevated levels of sFlt-1 have been noted in uncomplicated pregnancies, although to a lesser degree [16], and some studies suggest altered levels of this marker may persist long after parturition in formerly preeclamptic women [17]. Thus, we speculated that an altered angiogenic profile, which may be induced by hormone-related risk factors and/or dietary and lifestyle choices or persist in women with a history of preeclampsia, may be linked to breast cancer development. Using prospectively collected, pre-diagnostic serum samples from the screening arm of the prostate, lung, colon, and ovary cancer trial (PLCO) [18], we assessed whether healthy women with high levels of VEGF and PlGF along with low circulating sFlt-1 would be at elevated risk of breast cancer.
Materials and methods
Study population
Incident breast cancer cases and non-cases were drawn from the 39, 116 female participants, aged 55–74 years, who were randomly assigned from 1993 through 2001, to the screening arm of the multicenter prostate, lung, colorectal, and ovarian cancer screening trial (PLCO) [18]. This study was approved by Institutional Review Boards at the US National Cancer Institute and the 10 participating screening centers. For our study, women were a subset of the participants selected for several previous breast cancer biomarker studies using a stratified case–cohort study design [19], which drew from the population of women in the screening arm who at baseline provided a blood sample; completed the questionnaire and at least one study update; reported no prior history of breast cancer; and provided DNA and gave written informed consent. From this population, we identified 1,141 incident breast cancers diagnosed through 30 June 2005 and matched them to 1,141 non-cases who were alive and free of breast cancer by the end of the follow-up. The non-cases were randomly selected, frequency matched to cases on age at study entry (55–59, 60–64, 65–69, and 70–74 years) and period of blood collection (before or after the median collection date, 30 September 1997). Of these 2,282 women, 424 (37.1 %) breast cancer cases and 506 (44.3 %) non-cases were postmenopausal, were not using hormone therapy in the 4 months prior to the baseline collection, did not have a history of bilateral mastectomy, and had no other cancer other than non-melanoma skin cancer diagnosed during the follow-up period. Additional exclusions included the following: insufficient baseline serum (57 cases, 70 non-cases), unreliable values for earlier assays of serum estrogen metabolites (13 cases, 13 non-cases), and two breast cancer cases that could not be histologically confirmed. This left 352 breast cancer cases and 423 non-cases for study. From this group, we selected all 352 cases and 352 non-cases to study angiogenic markers.
Ascertainment of breast cancer cases
Participants were contacted annually by mail regarding cancer diagnoses occurring within the previous year. Breast cancers obtained from self-reports, next-of-kin, physicians, death certificates, and National Death Index linkage were confirmed by medical records, and tumor characteristics, including histology and hormone receptor status, were abstracted. Only confirmed cases were included in the analysis. Cases were grouped as ductal [International Classification of Diseases for Oncology, 2nd Edition histology code] (8,500), lobular (8,520), and tubular/other/unknown. When quantitative immunohistochemical results were available, tumors were considered estrogen receptor (ER) or progesterone receptor (PR) positive if at least 1 % of cells stained positive [20].
Serological measurements
Measurement of VEGF, sFlt-1, and PlGF in sera of non-pregnant women is limited, and in preliminary efforts, commercially available assays could not detect PlGF in sera of healthy postmenopausal women. We obtained a more sensitive assay (available for research purposes only) and measured these proteins at the Clinical and Epidemiologic Research Laboratory, Children’s Hospital, Boston, as follows: sFlt-1 was measured via Elecsys chemiluminescent immunoassay (Roche, Germany) [21], and VEGF and PlGF measured by sandwich ELISAs (Quantikine; R&D Systems, Minneapolis MN, USA). The VEGF assay detected the most biologically active isoform VEGF165. The limits of detection were 5, 7, and 6 pg/ml for VEGF, PlGF, and sFlt-1, respectively. To monitor the assay reliability, duplicate blinded quality control samples were included in each batch. Within and between batch, CVs were ≤15 % for all markers.
Statistical methods
Differences between cases and non-cases in baseline characteristics and angiogenic factors were assessed by t tests or Wilcoxon rank sum tests, with VEGF, sFlt-1, and PlGF analyzed on the natural logarithmic scale. To evaluate the association between quartiles of levels of each marker and breast cancer risk, HR and 95 % confidence intervals (CI) were estimated using weighted Cox proportional hazards regression models. Quartile cutpoints of marker concentrations were based on the non-case distribution. Non-cases were weighted by the inverse sample fraction to represent the study cohort; cases were given a weight of 1.0 because no sampling occurred, i.e., all women diagnosed with breast cancer who met the inclusion criteria were selected. Tests for trend were calculated using an ordinal variable for the quartiles. To assess potential confounding, we assessed whether inclusion of known or suspected breast cancer risk factors altered HR from the full model by more than 10 %, using a backwards elimination strategy. All factors meeting this criterion remained in the final model. Variables considered included age at study entry (55–59, 60–64, 65–69, and 70+); family history of breast cancer; personal history of benign breast disease; ages at menarche (<12. 12–13, and 14+), first birth (nulliparous, <20, 20–24, 25–29, and 30+), and menopause (<45, 45–49, 50–54, and 55+); and body mass index (BMI). Sensitivity analyses assessed potential tumor influences on marker levels by excluding women diagnosed with breast cancer within 2 years of blood donation. For women with available pathology information, we evaluated whether HR varied by breast tumor characteristics, including estrogen and progesterone receptor status, histology, and invasive vs in situ behavior. Analyses were performed with SAS Version 9, and proportional hazards ratios were calculated using Proc Surveyphreg [22]. All tests were two-sided, and p values <0.05 were considered statistically significant; no adjustment for multiple comparisons was made.
Results
Study population characteristics
Table 1 presents the distributions of demographic, medical history, and breast cancer risk factor characteristics of the study participants. Cases and matched non-cases were predominantly Caucasian (87 and 90 % of cases and non-cases, respectively) and were similar with respect to age (by study design), other demographic characteristics, and most medical conditions and reproductive risk factors. However, cases were more likely to have a history of benign breast disease (p = 0.045), and of smoking (p = 0.008), to have higher BMI at blood draw (p = 0.015), and were less likely to report regular aspirin use (p = 0.006). Cases were somewhat younger at menarche (p = 0.060), and used postmenopausal hormones for a longer duration than non-cases (p = 0.066). When the analysis was limited to invasive breast cancers, similar patterns of results were observed.
Most breast tumors were ductal (75.9 %) or lobular (10.5 %) histology and diagnosed with stage 1 or in situ disease (71.9 %). Overall, 52.8 % were ER+/PR+, 13.1 % ER−/PR−, and 8.2 % ER+/PR−; among invasive cancers (n = 277), 62.5 % were ER+/PR+ and 15.2 %, ER−/PR− (Table 2).
Angiogenic profile
Overall, weighted, age-adjusted geometric mean levels of PlGF (pg/ml) were similar for cases and non-cases (\({\bar{{\text{x}}}}\) cases = 19.4, \({\bar{{\text{x}}}}\) non-cases = 19.7; p = 0.293), VEGF (pg/ml) (\({\bar{{\text{x}}}}\) cases = 290.8, \({\bar{{\text{x}}}}\) non-cases = 288.4; p = 0.945), and sFlt-1 (pg/ml) (\({\bar{{\text{x}}}}\) cases = 88.9, \({\bar{{\text{x}}}}\) non-cases = 83.9; p = 0.915). No trends in HR were observed for any of the markers (Table 3), and quartile-specific HR were not significant. Including all markers in the model simultaneously did not change the pattern of results (Table 1). Similarly, restricting analysis to cases diagnosed two or more years after blood collection (supplemental Table 1a), to invasive breast cancers (supplemental Table 1b) or to ER+ cancers only (supplemental Table 1c) did not alter the interpretation of findings. HR for all levels of PlGF were nonsignificantly elevated among ER+ cancers, but no trend was evident. Adjustment for circulating estradiol did not alter our findings for VEGF or the other angiogenic markers studied (results not shown).
Among women with invasive cancer, VEGF levels were lowest in those diagnosed within the first year after blood collection, and values tended to increase nonsignificantly the longer the time between blood draw and diagnosis (Fig. 1a, p = 0.099). On average, levels in those diagnosed within the first year after blood donation were 250 pg/ml; this increased to 350 pg/ml in women diagnosed eight or more years after blood donation. sFlt-1 and PlGF did not vary consistently by recency of blood collection (Fig. 1b, c). Among non-cases, levels of all the markers were similar across the age groupings (supplemental Fig. 1a–c).
Discussion
This first study to evaluate pre-diagnostic serum levels of pro- and anti-angiogenic factors did not demonstrate a link between these biomarkers and postmenopausal breast cancer risk. Circulating angiogenic markers have been used for breast cancer staging and prognosis [3], but efforts to study their role as etiologic agents or early diagnostic markers of breast cancer are limited, and to our knowledge, no epidemiologic study has assessed risks using samples collected several years prior to postmenopausal breast cancer diagnosis. In studies comparing marker levels in newly diagnosed cases to non-cases, most [9, 11, 12], but not all [10, 23–25], found higher levels of circulating VEGF or PlGF in breast cancer cases than in non-cases, which may reflect local tumor production [26]. Contrary to this, we found VEGF was lowest in women diagnosed with invasive breast cancer close to the time of blood donation (within the year of enrollment in the cohort), and unexpectedly, levels tended to be higher among women diagnosed several years after blood donation. For the relatively small number of women with DCIS (n = 75), no discernible pattern was observed between VEGF and recency of blood donation, and overall, VEGF levels were comparable among women with invasive and in situ disease. Since the majority of women with invasive cancer were diagnosed with stage 1 disease, our study does not support a role for serum VEGF as a marker of early progression from DCIS to invasive breast cancer. No studies have evaluated a similar role for sFlt-1 and PlGF in breast cancer etiology, in part because previous assays have not been sensitive enough to detect the low levels found in postmenopausal or non-pregnant women.
The close physiologic relationship between endocrine function and angiogenesis, and suggestions that sex steroids regulate the balance of angiogenic factors, particularly VEGF, in a tissue-specific manner [3, 27], provide some support for angiogenic imbalance in breast cancer development. In healthy premenopausal women, VEGF levels in breast tissue are high during the luteal phase of the menstrual cycle when neovascularization occurs and both progesterone and estradiol levels are high [28, 29]. Circulating VEGF is elevated during ovulation [30], in women using exogenous hormones [31], and in those undergoing IVF [32]. We did not observe strong correlations between circulating estradiol and VEGF, and adjustment for this did not alter our findings for any of the angiogenic markers. Finally, recent investigations have linked circulating angiogenic factors to several breast cancer risk factors thought to operate at least in part by hormonal mechanisms, including physical exercise and postmenopausal obesity. Exercise causes a transient but significant increase in circulating levels of sFlt-1 and decrease in VEGF [33], while overweight and obese women have higher VEGF levels than normal weight women [34].
Why pregnancies complicated by preeclampsia attenuate maternal breast cancer risk later in life is not fully understood [14, 15], but may involve changes in mammographic density [35] or circulating sex steroids and/or growth factors [36], or reflect underlying biologic characteristics that are associated with both pregnancy complications and reduced breast cancer risk [17]. We could not assess whether women with a preeclamptic pregnancy experienced a reduced breast cancer risk in this population since this information was not available, although given the rarity of the condition (5–8 % of pregnancies), the number of women in the PLCO cohort with such a history should be low. Similar to our findings, the one study to measure serum PlGF and sFlt-1 during pregnancy did not link these markers to subsequent breast cancer risk [23], although the follow-up time was short (10 years after the index pregnancy) and case accrual was low since most women were still premenopausal.
Reasons for our lack of findings are not clear, but the ongoing debate regarding the clinical utility of circulating VEGF as a prognostic marker in breast cancer may provide some insight [1, 37–39]. Findings across studies are not consistent [40] in part because VEGF has been measured in both serum and plasma, and the absolute values of this marker in these different blood components are very divergent. Since VEGF is sequestered in platelets [39], assay measurements in serum, which is likely contaminated by platelets, are substantially higher than in plasma [41, 42]. While platelet activation has long been recognized in women with breast cancer [37] and higher levels of VEGF are sequestered in platelets of breast cancer cases compared to healthy women [43], it is not known to what extent serum levels of VEGF capture non-tumor vs tumor-derived sources of this marker.
This study had notable strengths, including that the study population was drawn from the PLCO cohort, which provided prospectively collected serum samples, and angiogenic markers were measured using assays available for research purposes that can detect the low values, particularly of PlGF and sFlt-1, found in postmenopausal women. This study also had several weaknesses. The measurement of angiogenic factors occurred at one point in time, which is a common limitation in studies of circulating biomarkers, and the representativeness and stability of these markers over time is not known. We did not have the opportunity to evaluate temporal changes in these markers in individual women; however, our finding of little differences in marker levels in non-cases across the age groups provides some confidence of the stability of these markers in the postmenopause. Additionally, inferences from this study are limited, since only women who were postmenopausal and not using menopausal hormone therapy at the time of blood collection were eligible for study. Finally, as discussed earlier, both the study population and specimen used may not be optimal for assessing the role of angiogenic markers in breast cancer risk, particularly in women who experienced pregnancy complications. Nevertheless, this study does not support the proposition that a pro-angiogenic profile is associated with excess breast cancer risk.
References
Gasparini G (2000) Prognostic value of vascular endothelial growth factor in breast cancer. Oncologist 5(supplement 1):37–44
Brown LF, Berse B, Jackman RW, Tognazzi K, Guidi AJ, Dvorak HF et al (1995) Expression of vascular permeability factor (vascular endothelial growth factor) and its receptors in breast cancer. Hum Pathol 26:86–91
Hyder SM (2006) Sex-steroid regulation of vascular endothelial growth factor in breast cancer. Endocr Relat Cancer 13:667–687
Ghosh S, Sullivan CA, Zerkowski MP, Molinaro AM, Rimm DL, Camp RL et al (2008) High levels of vascular endothelial growth factor and its receptors (VEGFR-1, VEGFR-2, neuropilin-1) are associated with worse outcome in breast cancer. Hum Pathol 39:1835–1843
Maae E, Olsen DA, Steffensen KD, Jakobsen EH, Brandslund I, Sørensen FB et al (2012) Prognostic impact of placenta growth factor and vascular endothelial growth factor A in patients with breast cancer. Breast Cancer Res Treat 133(1):257–265. doi:10.1007/s10549-012-1957-0
Parr C, Watkins G, Boulton M, Cai J, Jiang WG (2005) Placenta growth factor is over-expressed and has prognostic value in human breast cancer. Eur J Cancer 4:2819–2827
Thielemann A, Baszczuk A, Kopczyński Z, Kopczyński P, Grodecka-Gazdecka S (2013) Clinical usefulness of assessing VEGF and soluble receptors sVEGFR-1 and sVEGFR-2 in women with breast cancer. Ann Agric Environ Med 20:293–297
Bachelot T, Ray-Coquard I, Menetrier_Caux C, Rastkha M, Duc A, Blay JY (2003) Prognostic value of serum levels of interleukin 6 and or serum and plasma levels of vascular endothelial growth factor in hormone-refractory metastatic breast cancer patients. Br J Cancer 88:1721–1726
Byrne GJ, McDowell G, Agarawal R, Sinha G, Kumar S, Bundred NJ (2007) Serum vascular endothelial growth factor in breast cancer. Anticancer Res 27:3481–3487
Reeves KW, Ness RB, Stone RA, Weissfeld JL, Vogel VG, Powers RW et al (2009) Vascular endothelial growth factor and breast cancer risk. Cancer Causes Control 20:375–386
Heer K, Kumar H, Read JR, Fox JN, Monson JRT, Kerin MJ (2001) Serum vascular endothelial growth factor in breast cancer: its relation with cancer type and estrogen receptor status. Clin Cancer Res 7:3491–3494
Hoar FJ, Lip GYH, Belgore F, Stonelake PS (2004) Circulating levels of VEGF-A, VEGF-D and soluble VEGF-A receptor (sFlt-1) in human breast cancer. Int J Biol Markers 19:229–235
Opdahl S, Romundstad PR, Alsaker MDK, Vatten LJ (2012) Hypertensive diseases in pregnancy and breast cancer risk. Br J Cancer 107(1):176–182. doi:10.1038/bjc.2012.195
Vatten LJ, Romundstad PR, Trichopoulos D, Skjaerven R (2002) Pre-eclampsia in pregnancy and subsequent risk for breast cancer. B J Cancer 87:971–973
Troisi R, Weiss HA, Hoover RN (1998) Pregnancy characteristics and maternal risk of breast cancer. Epidemiology 9:641–647
Troisi R, Braekke K, Harsem NK, Hyer M, Hoover RN, Staff AC (2008) Blood pressure augmentation and maternal circulating concentrations of angiogenic factors at delivery in preeclamptic and uncomplicated pregnancies. Am J Obstet Gynecol 199(6):653e.1–653e.10
Carbillon L, Delahosseraye C (2015) Preeclampsia and subsequent breast cancer risk. Cancer Causes Control 26(6):955–956
Hayes RB, Sigurdson A, Moore L, Peters U, Huang WY, Pinsky P et al (2005) Methods for etiologic and early marker investigations in the PLCO trial. Mutat Res 592(1–2):147–154
Fuhrman BJ, Schairer C, Gail MH, Boyd-Morin J, Xu X, Sue LY et al (2012) Estrogen metabolism and risk of breast cancer in postmenopausal women. J Natl Cancer Inst 104(4):326–339. doi:10.1093/jnci/djr531
Hammond MEH, Hayes DF, Dowsett M, Allred DC, Hagerty KL, Badve S et al (2010) American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Oncol Pract 28:2784–2795
Verlohren X, Galindo A, Schlembach D, Zeisler H, Herraiz I, Moertl MG et al (2010) An automated method for the determination of the sFlt-1/PlGF ratio in the assessment of preeclampsia. Am J Obstet Gynecol 202(2):161.3–161.e11. doi:10.1016/j.ajog.2009.09.016
SAS Institute Inc. (1999) SAS/STAT user’s guide, version 8. SAS Institute Inc., Cary
Vatten LJ, Romundstad PR, Jenum PA, Eskild A (2009) Angiogenic balance in pregnancy and subsequent breast cancer risk and survival: a population study. Cancer Epidemiol Biomarkers Prev 18:2074–2078
Zhang J, Yin L, Wu J, Zhang Y, Xu T, Ma R et al (2014) Detection of serum VEGF and MMP-9 levels by Luminex multiplexed assays in patients with breast infiltrative ductal carcinoma. Exp Ther Med 8(1):175–180. doi:10.3892/etm.2014.1685
Stathopoulos J, Armakolas A, Stathopoulos GP, Gomatos IP (2010) Plasma VEGF levels in breast cancer patients with and without metastases. Oncol Lett 1(4):739–741. doi:10.3892/ol_00000129
Kerbal RS (2008) Molecular origins of cancer: tumor angiogenesis. N Engl J Med 358:2039–2049
Garvin S, Nilsson UW, Huss FRM, Kratz G, Dabrosin C (2006) Estradiol increases VEGF in human breast studied by whole-tissue culture. Cell Tissue Res 325:245–251
Dabrosin C (2005) Sex steroid regulation of angiogenesis in breast tissue. Angiogenesis 187:103–108
Losordo DW, Isner JM (2001) Estrogen and angiogenesis: a review. Arterioscler Thromb Vasc Biol 21:115–121
Benoy I, Vermeulen P, Wuyts H, Dirix L (1998) Vascular endothelial cell growth factor (VEGF) serum concentrations change according to the phase of the menstrual cycle. Eur J Cancer 34:1298–1299
Agrawal R, Prelevic G, Conway GS, Payne NN, Ginsburg J, Jacobs HS (2000) Serum vascular endothelial growth factor concentrations in postmenopausal women: the effect of hormone replacement therapy. Fertil Steril 73:56–60
Monteleone P, Artini PG, Simi G, Casarosa E, Cela V, Genazzani AR (2008) Follicular fluid VEGF levels directly correlate with perifollicular blood flow in normoresponder patients undergoing IVF. J Assist Reprod Genet 25:183–186
Bailey AP, Shparago M, Gu JW (2006) Exercise increases soluble vascular endothelial growth factor receptor-1 (sFlt-1) in circulation of healthy volunteers. Med Sci Monit 12:CR45–CR50
Silha JV, Krsek M, Sucharda P, Murphy LJ (2005) Angiogenic factors are elevated in overweight and obese individuals. Int J Obes 29:1308–1314
Prebil LA, Ereman RR, Powell MJ, Jamshidian F, Kerlikowske K, Shepherd JA et al (2014) First pregnancy events and future breast density: modification by age at first pregnancy and specific VEGF and IGF1R gene variants. Cancer Causes Control 25:859–868. doi:10.1007/s10552-014-0386-2
Terry MB, Perrin M, Salafia CM, Zhang FF, Neugut AI, Teitelbaum SL et al (2006) Preeclampsia, pregnancy-related hypertension, and breast cancer risk. Am J Epidemiol 165:1007–1012. doi:10.1093/aje/kwk105
Verheul HM, Pinedo HM (2003) The importance of platelet counts and their contents in cancer. Clin Cancer Res 9:3219–3221
Lee JK, Hong YJ, Han CJ, Hwang DY, Hong SI (2000) Clinical usefulness of serum and plasma vascular endothelial growth factor in cancer patients: which is the optimal specimen? Int J Oncol 17:149–152
Jelkmann W (2001) Pitfalls in the measurement of circulating vascular endothelial growth factor. Clin Chem 47:617–623
Adams J, Carder PJ, Downey S, Forbes MA, MacLennan K, Allgar V et al (2000) Vascular endothelial growth factor (VEGF) in breast cancer: comparison of plasma, serum, and tissue VEGF and microvessel density and effects of tamoxifen. Cancer Res 60:2898–2905
McIlhenny C, George WD, Doughty JC (2002) A comparison of serum and plasma levels of vascular endothelial growth factor during the menstrual cycle in healthy female volunteers. Br J Cancer 86:1786–1789
George ML, Eccles SA, Tutton MG, Abulafi AM, Swift RI (2000) Correlation of plasma and serum vascular endothelial growth factor levels with platelet count in colorectal cancer: clinical evidence of platelet scavenging? Clin Cancer Res 6:3147–3152
Han H, Cao F-L, Wang B-Z, Mu X-R, Li G-Y, Wang X-W (2014) Expression of angiogenesis regulatory proteins and epithelial-mesenchymal transition factors in platelets of the breast cancer patients. Sci World J. doi:10.1155/2014/878209
Acknowledgments
The authors gratefully acknowledge Dr. Robert Hoover for manuscript review and comments.
Author’s contributions
R.T. Falk, A.C. Staff, S.A. Karumanchi, and R. Troisi were involved in conception and design. G. Bradwin and S.A. Karumanchi developed the methodology. R.T. Falk and R. Troisi analyzed and interpreted the data (statistical analysis, biostatistics, and computational analysis). R.T. Falk, A.C. Staff, G. Bradwin, S.A. Karumanchi, and R. Troisi wrote, reviewed, and/or revised the manuscript. G. Bradwin, S.A. Karumanchi, and A.C. Staff involved in administrative, technical, or material support.
Funding
This study was supported by the National Cancer Institute, NIH, U.S. Department of Health and Human Services through contract # HHSN261201200327P.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest regarding this publication.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10552_2016_779_MOESM1_ESM.pptx
Box-plots of Angiogenic Factors by Age Group (VEGF, sFlt-1 and PlGF, supplemental figures 1a–1c, respectively.) (PPTX 43 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Falk, R.T., Staff, A.C., Bradwin, G. et al. A prospective study of angiogenic markers and postmenopausal breast cancer risk in the prostate, lung, colorectal, and ovarian cancer screening trial. Cancer Causes Control 27, 1009–1017 (2016). https://doi.org/10.1007/s10552-016-0779-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-016-0779-5