Abstract
Gastrointestinal (GI) cancers are common cancers that are responsible for a large portion of global cancer fatalities. Due to this, there is a pressing need for innovative strategies to identify and treat GI cancers. MicroRNAs (miRNAs) are short ncRNAs that can be considered either cancer-causing or tumor-inhibiting molecules. MicroRNA-155, also known as miR-155, is a vital regulator in various cancer types. This miRNA has a carcinogenic role in a variety of gastrointestinal cancers, including pancreatic, colon, and gastric cancers. Since the abnormal production of miR-155 has been detected in various malignancies and has a correlation with increased mortality, it is a promising target for future therapeutic approaches. Moreover, exosomal miR-155 associated with tumors have significant functions in communicating between cells and establishing the microenvironment for cancer in GI cancers. Various types of genetic material, such as specifically miR-155 as well as proteins found in cancer-related exosomes, have the ability to be transmitted to other cells and have a function in the advancement of tumor. Therefore, it is critical to conduct a review that outlines the diverse functions of miR-155 in gastrointestinal malignancies. As a result, we present a current overview of the role of miR-155 in gastrointestinal cancers. Our research highlighted the role of miR-155 in GI cancers and covered critical issues in GI cancer such as pharmacologic inhibitors of miRNA-155, miRNA-155-assosiated circular RNAs, immune-related cells contain miRNA-155. Importantly, we discussed miRNA-155 in GI cancer resistance to chemotherapy, diagnosis and clinical trials. Furthermore, the function of miR-155 enclosed in exosomes that are released by cancer cells or tumor-associated macrophages is also covered.
Graphical Abstract
Various mechanisms can be affected by miNA-155 and exosomal miR-155. Various molecular processes linked to angiogenesis and apoptosis in GI cancers.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Researchers projected that in 2019, the United States would see more than 1.7 million newly diagnosed individuals facing cancer and over 607,000 deaths due to the disease (Siegel et al. 2019). The WHO Classification of Tumors sets the global benchmarks for tumor classification and diagnosis. It allows for direct comparisons to be made between nations. Diagnosing tumors is not exclusively the pathologists’ domain; nowadays some patients are being treated considering their clinical, liquid biopsy, and radiological results even before tissue samples are obtained. This relevance extends the cataloging to various medical care of individuals with gastrointestinal tumors (Washington et al. 2021). The GI tract is the location of occurrence of many cancers as the highest incidence of cancers and second highest mortality are related to this system. The gastrointestinal (GI) tract's cells have a very brief lifespan. The stomach's epithelial cells, colon, and small intestine that are reproduced of stem cells, are usually replaced within a few days, and are among the tissues, which easily regenerate in the body. These tissues continue to sustain physical, chemical, and biological damage, necessitating this conversion. The rapid proliferation of these cells increases the possibility of pre-cancer mutations, which ends up with malignant tumors (Anderson et al. 2019).
GI cancers
At present, most patients with colorectal cancer (CRC), gastric cancer (GC), and esophageal cancer (EC) primarily undergo surgical removal as their main form of treatment. Notwithstanding advancements in adjuvant and neoadjuvant chemoradiotherapy (CRT), a big patient population, however, creates far-off metastases and is resistant to treatment (Smyth and Moehler 2019). One of the oncogenic pathways linked to gastrointestinal cancers is chronic inflammation. For example, intestinal disorders due to inflammation like ulcerative colitis (UC) and Crohn's disease (CD), as well as other inflammatory bowel conditions and chronic atrophic gastritis (mainly caused by Helicobacter pylori), are risk factors for both small bowel cancer and CRC (Hata et al. 2003; Parsonnet et al. 1991). Intestinal cancer progression is also associated with genetic factors. Every now and then, one watches the genealogy of a family that includes GI cancer cases. According to details, the prevalence of familial GC and CRC is between 10 and 20% (Corso et al. 2011; Chapelle 2004), which is not negligible.
MicroRNAs
MicroRNAs (miRNAs) are controllers of genes that code proteins. miRNAs can tightly bind to the 3'-untranslated part (3'-UTR) of their specific mRNA, influencing protein expression by degrading the mRNAs or by translation inhibition (Ha and Kim 2014; Bartel 2009; Preethi et al. 2022; Anees et al. 2023; Selvakumar et al. 2024). miRNAs are single-stranded RNAs (ssRNAs), which are composed of 20–25 nucleotides, are important in different major cellular mechanisms, including proliferation, angiogenesis, apoptosis, and differentiation (Rashed et al. 2017; Mangala et al. 2016; Kanlikilicer et al. 2016; Bayraktar et al. 2017). MiRNA genes made up of approximately 1% of the human genome, which are post-transcriptionally regulated over 33% of translated proteins (Bentwich et al. 2005).
Previous research has examined the variability in miRNA levels within an individual (Yoon et al. 2017). It is crucial to determine the degree of variation in miRNA levels within an individual in order to establish effective clinical biomarkers. This is because miRNAs with inconsistent levels of expression are not likely to serve as dependable biomarkers. The fluctuations seen in profiling studies of individuals may be connected to external environmental elements or undisclosed diseases (Wu et al. 2018). In conclusion, our findings strongly indicate that the inherent fluctuation in the expression of miRNAs could be the underlying factor for the contradictory outcomes observed in other biomarker research. (Yoon et al. 2017).
During cancer development and the associated genetic mutations, there is a noteworthy reduction in the production of essential miRNAs, disrupting their normal regulatory functions. Consider the scenario of a genetic alteration in XPO5 that leads to the retention of precursor miRNA molecules within the cell's nucleus (Melo et al. 2010). Furthermore, genomic analyses have shown that mutant XPO5 significantly contributes to tumor growth by increasing the expression of genes that may cause cancers like EZH2, MYC, and KRAS. This surge in gene expression is directly due to the lack of the corresponding regulatory microRNAs (Rupaimoole et al. 2016). Moreover, substantial findings shows that the cancer cells microenvironment is vital in regulating processes such as miRNA production, methylation, and transcriptional modifications (Rupaimoole et al. 2016).
Since Calin et al. (Calin et al. 2002) showed a link in miRNAs and human cancer. In many investigations, miRNAs were found as tumor suppressor miRNAs or as once-miRNAs in human cancer. MiRNAs are considered ideal potential human cancer biomarkers due to their stability. On the other hand, miRNA-targeted treatment has many challenges, such as the delivery system. Additionally, a few clinical trials are underway at the moment. In addition, miRNAs expressed in bodily fluids that are circulated potentially forecast the growth of a tumor, like metastasis to lymph nodes, and also may contribute to the prognosis and reaction to cancer treatment in ill people with GIC (Takahashi et al. 2019; Xu et al. 2018; Khoury and Tran 2015; Mitchell et al. 2008; Gallo et al. 2012; Ortiz-Quintero 2016). The accumulation of data has demonstrated that miRNAs are able to remain stable in bodily fluids, including blood (Gallo et al. 2012; Arroyo et al. 2011; Hu et al. 2010), urine (Lv et al. 2013), saliva (Gallo et al. 2012; Michael et al. 2010), and breast milk (Zhou et al. 2012).
Numerous forms of human cancer show increased production of miR-155. It was found that miR-155 expression levels rise and function as a driver for cancer development in cancerous tissues and cell models, such as those related to gastrointestinal cancer (Qu et al. 2018; Shi et al. 2020a; Wu et al. 2020). Markedly elevated miR-155 levels were related to a notably reduced existence rate in individuals with esophageal squamous cell carcinoma. MiR-155 might function as a separate prognostic sign for this disease (Zheng et al. 2020). Furthermore, miR-155 is crucial in promoting the progression and attack of gastric tomur cells (Qu et al. 2018). But still the exact role and fundamental machineries of miR-155 in gastrointestinal cancer remain insufficiently understood.
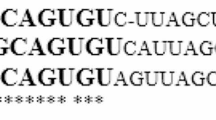
Considering that miR-155 and exosomal miR-155 have a crucial function in different molecular processes linked to cancer, including angiogenesis and apoptosis (Fig. 1). The primary miRNA that controls immune responses is miR-155 (O'Connell et al. 2009). The miRNA-155 is formed by activated T or B cells, monocytes, and macrophages (Tili et al. 2008a; Tili et al. 2008b). MiR-155 plays an essential function at some stage in hematopoiesis and controls tolerance and lymphocyte homeostasis. Slight growth in miR-155 ranges is found in lots of kinds of malignancies of myeloid origin B cell, as well as miR-155 transgene overexpression in mice is effective in most cancers (Tili et al. 2009). So, there is an urgent need for a review that mention various functional aspects of miR-155 in GI tumors. However, a review discussing the role of miR-155 in GI tomurs was published in 2016. Therefore, we present an updated summary of miR-155's function in gastrointestinal cancers in Table 1. Additionally, we highlight the role of exosomal miR-155 in GI malignancies.
Various mechanisms can be affected by miNA-155 and exosomal miR-155. Various molecular processes linked to angiogenesis and apoptosis in GI cancers. miR-155 is considered as primary miRNA that controls immune responses. The miRNA-155 is produced by activated B or T cells, monocytes, and macrophages. Moreover, miR-155 plays an essential function at some stage in hematopoiesis and controls tolerance and lymphocyte homeostasis
miRNA-155 and GI Cancer
Types of GI Cancer
Pancreatic cancer (PC) is the fourth top reason of deaths due to cancer globally, accountable for approximately 227,000 deaths each year (Raimondi et al. 2009). A family history of prolonged pancreatitis(chronic) (Klein et al. 2004) smoking, patients with higher ages, men compared with women, diabetes mellitus, weight problems, blood types other than O (Wolpin et al. 2009; Amundadottir et al. 2009), exposure to special materials due to the job, African-American ancestry, a diet high protein and fat, with not enough fibers and folate, and most likely H.pylori and oral and dental diseases such as periodontal ones are risk factors for this cancerous disease (Raimondi et al. 2009). According to preliminary studies, metformin may protect against PC progression (Li et al. 2009). Coffee drinking isn't always seen as a risk factor for the illness. Cigarette smoking and family history are the main contributing factors to pancreatic cancer, despite the fact that the cause is complex and multifactorial. Smoking causes about 20% of pancreatic tumors, and smokers' cancers have more genetic mutations than non-smokers' cancers (Blackford et al. 2009).
Gastric cancer could be a universally imperative illness. With an estimated one million novel cases every year, the fifth most often studied malignancy worldwide is gastric cancer. Usually, this cancer is diagnosed lately as at primary stages its signs and symptoms are non-specific, gastric cancer ranked third in the world for cancer-related deaths in 2018, accounting for 784,000 deaths worldwide (Wang et al. 2002). South America, Eastern Europe, and East Asia have the uppermost mortality and incidence all over the world. The possibility of stomach malignancy in men is twice that of women (Wang et al. 2002). There has been a steady decrease in this cancer's incidence and fatality rates over the last century. In spite of declining incidence rates in most countries, physicians should anticipate an increase in gastric cancer incidence in the future because of an aging population. Improvements in living standards and economic advancement have led to the reduction of H.pylori incidence, the main risk factor of stomach malignancy (Vartiainen et al. 2007). In high-prevalence places, for instance, Korea and Japan, screening programs have moreover driven considerable decreases in gastric cancer-related mortality (Chew and Gallo 2009; Gubbay et al. 1990; Guan et al. 2014). A detected increment within the rate in more youthful individuals from high-pay countries recommends an alteration in illness chance and the study of gastric cancer epidemiology. Future cancer prevention and clinical research should take into account recent developments in gastric cancer epidemiology (Sarkar and Hochedlinger 2013).
Colorectal cancers rank as the third most prevalent cancer globally (Schreiner et al. 2020; Hansen et al. 2013). Rectal cancer occurs more frequently than colon cancer, particularly in industrialized countries, where the ratio of colon to rectum cases is 2:1 or higher, with a slightly higher incidence in females. By contrast, non-industrialized countries exhibit comparable rates of both forms of cancer. Annually, roughly 250,000 new colon cases are diagnosed in Europe, constituting approximately 9% of all malignancies. With the advent of industrialization and urbanization, there has been a corresponding rise in the incidence of this malignancy. The prevalence of the described phenomenon has historically been greater in nations possessing higher levels of income, yet presently it is experiencing an escalation within middle and low-income countries. The prevalence of the aforementioned phenomenon in Africa and a significant portion of Asia is still comparatively limited. The occurrence of the aforementioned phenomenon exhibits a marginal increase in the geographic regions of Western and Northern Europe, as compared to the regions of Southern and Eastern Europe. Europe, North America, and Australia comprise additional regions of increased susceptibility. Asia, Africa, and Central and South America are regions that exhibit a significantly low level of risk (Hansen et al. 2013).
Most esophagus malignancies are histologically divided into two main categories: squamous cell carcinoma (SCC) and adenocarcinoma (ADCA). In the United States, the incidence of one type of carcinoma has declined by less than 30% in recent thirty years, whereas the rate of another sort has risen by over 60% (Schlottmann et al. 2018; Takeuchi et al. 2018; Sah et al. 2019). Familial Barrett's esophagus tends to be related to uncommon, hereditary dominant susceptibility alleles that follow an autosomal inheritance pattern. Its diagnosis should be considered in patients diagnosed with esophageal or gastroesophageal junction (GEJ) adenocarcinoma. Specifically, in Caucasian men over 40 years old and with a record of gastroesophageal reflux disease (GERD), this consideration may be more appropriate. Adopt a regimen abundant in fruits, grains, and vegetables, and include folate, proton-pump inhibitors, vitamin C, and NSAIDs. It's essential to consider that while these factors may reduce the risk of Barrett's esophagus and, consequently, esophageal malignancy, none have yet been validated as effective preventive interventions. In spite of these correlations, none of these measures have been validated as preventive interventions thus far (Tramontano et al. 2018; Cheng et al. 2018). Esophageal cancer is among the most prevalent gastroenterological cancers, with over 16,000 cases identified annually in the USA. Globally, they are the top sixth prevalent sort of malignancies. The "esophageal cancer belt," which refers to the region most at risk, includes parts of northern China, the south of Russia, the north of Iran, and Central Asian countries. Ninety percent of cases in this area are squamous cell carcinomas (Solinas et al. 2009).
Mechanisms of action
Tumor-associated macrophages (TAMs) are a prevalent subset of inflammatory cells located in the hypoxic regions of various tumors (Martinez et al. 2008). Tumor-associated macrophages (TAMs) have been confirmed to differentiate into the M2 form of macrophages in the microenvironment of tumors. Two distinct subtypes of macrophages can be identified within the population: M1 macrophages, pro-inflammatory type, and M2 macrophages, immunomodulatory type. Tumor-associated macrophages (TAMs) have been revealed to promote angiogenesis linked to cancer progression, accelerate the multiplying of cancer cells, and improve cancer migration and invasion (Cai et al. 2012; Zhang et al. 2014). As such, it is imperative to acknowledge TAMs as a crucial immunological cell target in the inhibition of esophageal cancer advancement and promotion.
Based on current studies, the induction of miR155 has been observed to mitigate the generation of cytokines in tumor-associated macrophages (TAMs) and shift the polarization of M2 TAMs towards M1 type (Zhou et al. 2013). Nevertheless, the exact function of miR-155 in TAMs derived from endometrial cancer (EC) remains unclear. Fibroblast growth factor-2 (FGF2), a member of the fibroblast growth factor family, promotes the growth and maturing of various cell categories, including fibroblasts and neoplastic cells (Nillesen et al. 2007). FGF2 is a fundamental molecule for signaling that has been revealed to be involved in initiating tumor generating new vessels (Donnem et al. 2012). Earlier studies have established that miR-155 controls the production of FGF2, influencing angiogenesis in non-small cell lung tumor (Wang et al. 2018b). Recent studies offer limited insight into the extent to which miR-155 can control FGF2 in TAMs derived from endometrial cancer (EC).
A 145 kDa protein called SHIP-1 controls the function of macrophages (Sly et al. 2007; Hibbs et al. 2018; Hamilton et al. 2011; Ghansah et al. 1950). Extrinsic soluble components including microenvironmental chemokines and cytokines influence the SHIP-1 in immune cells expression (Kalesnikoff et al. 2003). As demonstrated by us and others, In SHIP-1 knockout (KO) mice, the development of M2 macrophages. These macrophages modulate immune system and are favorable for tumor progression and has been noticeably increased, indicating the part SHIP-1 plays in controlling macrophage polarization (Ghansah et al. 1950; Rauh et al. 2005; Villalobos-Ayala et al. 2020). Furthermore, inhibition of SHIP-1 protein from translation and an upsurge in cancer burden are correlated with the growth of MDSC in PC-infected mice (Ghansah 2012; Pilon-Thomas et al. 2011). It has therefore been suggested that inhibiting the synthesis of miR-155 may stimulate the increase of SHIP-1 production, restore M-MDSC homeostasis, enhance the tumor-eradicating ability of M1-TAMs, and strengthen the immune system's capacity to combat pancreatic cancer.
A crucial component of cell division, migration, apoptosis, and multiplication is MRTF-A, also known as MKL1 (Zhou et al. 2014). Serum response factor (SRF) coactivator MRTF-A is expressed in different organs (Wang et al. 2008). To initiate transcription, the MRTF-A-SRF complex attaches to the CArG box on the specific gene's promoter located within the nucleus (Yin et al. 2020; Song et al. 2016; Rad et al. 2016; Rudin et al. 2012; Mathews et al. 2010). The translation factor family known as the Y (SRY)-box (SOX) protein family includes a very preserved high mobility group (HMG) DNA binding region (Rudin et al. 2012). The SOX family members are crucial for either fetal and postnatal growth, as well as for the regulation of stem cells (Yin et al. 2020; Song et al. 2016; Rad et al. 2016). Moreover, many family members of the SOX are involved in the advancement of cancer (Wilusz and Sharp 2013; Salzman et al. 2013; Jeck et al. 2013; Li et al. 2015a; Memczak et al. 2013; Vo et al. 2019).
Recent findings have revealed that changes in miR-155 levels are associated with various signaling pathways. As a consequence, miR-155 was recognized as a possible target for cancer therapy at the molecular stage (Moutabian et al. 2023). The levels of miR-155 expression differ among various types of cells and environmental conditions within tissues. Its activity is also influenced by several pathways, which work together to respond to signals within the cells. Various binding sites for transcription factors were recognized until now, including NF-κB, SMAD4, ISRE, IRF, and AP-1. Additionally, there are two Ets locations for binding in the transcription start site, two Foxp3 binding sites in intron 2, and three hypoxia-inducible factor-1 alpha binding sites in the gene's promoter Sect. (Mahesh and Biswas 2019). Several signaling pathways have a role in regulating the expression of miR-155, including its activation or inhibition by various regulatory cytokines like TGF-β. The anti-inflammatory protein IRF3 reduces the amounts of miR-155-5p and miR-155-3p. Typically, IL-10 reduces miR-155 levels by preventing the Ets2 transcription factor (Mahesh and Biswas 2019). Yin et al. have shown that the physical interaction between MRTF-A and miR-155 is linked to the triggering of the Wnt-β-catenin pathway, the involvement of RNA polymerase II, and an upsurge in histone acetylation (Zhong et al. 2018). MiR-155 stimulates the malignant behaviors of cancerous cells by targeting the 3′UTR to reduce SOX1 production, in both in vitro and animal models. Uncovering the MRTF-A/miR-155/SOX1 signaling pathway has resulted in the formulation of hypotheses regarding the origins and incidence of GC. Real-time PCR has established the production of miR-155 following plasmid and siRNA transfection with MRTF-A encoding. Yin et al. reported that MRTF-A interacts with the promoter of miR-155, subsequently recruiting the Wnt-β-catenin pathway to activate RNA Pol II and enhance histone acetylation (Zhong et al. 2018). By targeting the 3′UTR, miR-155 downregulates SOX1 expression both in cell lines and in animal models, thereby promoting the relocation of gastric tumor cells. The discovery of the MRTF-A/miR-155/SOX1 signaling pathway offers novel visions into the development and prevalence of gastric malignancy. Real-time PCR has revealed that miR-155 is expressed after plasmid and siRNA transfection with MRTF-A encoding. The Wnt/β-catenin signaling pathway has a vital role in cellular homeostasis by controlling numerous procedures. It is the key for promoting the cell cycle, reversing organ damage, driving embryonic development, and initiating as well as progressing various benign and malignant tumors (Liu et al. 2018; He et al. 2015; Al-Haidari et al. 2018; Al-Haidari et al. 2017).
Liu et al. investigate the impact of miR-155 on the Wnt/β-catenin pathway and the invasive capability of SW-480 colorectal cancer (CRC) cells. Their aim is to provide a comprehensive empirical basis for understanding the pathogenesis and developmental mechanisms associated with distant invasion and metastasis in colorectal cancer. This investigation substantially advanced current understanding by providing critical experimental evidence (Kapral et al. 2019). In the present study, RT-PCR was utilized to quantify miR-155 amounts in both colorectal cancer (CRC) tissues and the nearby normal tissues. The primary factor contributing to the increased invasive potential of colon tumor cells is the transcriptional control of β-catenin by miR-155. This effect can be related to the upregulation of β-catenin. Therefore, β-catenin and miR-155 offer distinct possibility as innovative investigative and treatment tools for addressing malignant tumor metastasis (Kapral et al. 2019).
Wang and colleagues observed that miR-155 amounts were meaningfully upper in tissues affected by colorectal cancer. Loss-of-function investigations showed that the absence of miR-155 significantly diminished the proliferation, attack, and movement abilities of CRC cells. Furthermore, a screening process identified the downstream target genes influenced by miR-155. In CRC cells, it was observed that miR-155 directly binds to FOXO3a, resulting in decreased FOXO3a expression. FOXO3a levels were reduced in colorectal cancer tissues and presented an inverse relationship with miR-155 expression in these tissues. Increasing FOXO3a levels in cells independently hindered the multiplying, movement, and attack of colorectal cancer cells. Moreover, experiments designed to rescue the cells from their current state demonstrated that the silencing of FOXO3a greatly countered the downregulating effect of miR-155 depletion on the aggressive actions of CRC cells. In summary, it has been determined that miR-155 has a significant function in promoting malignant characteristics of colorectal cancer cells e.g. increased cell growth, movement, and invasion. This is achieved by manipulating FOXO3a. These findings offer potential insights for developing targeted treatments for CRC (Wang et al. 2017).
CagA, an essential virulence factor of Hp, functions in the growth of tumor by contributing to its carcinogenesis. The abnormal production of miR-155-5p has been seen in individuals diagnosed with GC, thus showing a clear connection to the start and development of cancer. There is limited knowledge about the connection between CagA and miR-155-5p. In their study, Wu and colleagues discovered a substantial reduction in the presence of miR-155-5p in GC cells, and this decrease was even more significant following CagA induction. Both the cells with elevated levels of CagA and those with reduced levels of miR-155-5p exhibited an increased ability to undergo malignant transformation, while the cells with increased levels of miR-155-5p showed a suppressed ability to undergo malignant transformation when tested in laboratory settings. The impact of CagA may alter the act of miR-155-5p in GC cells. In addition, it was determined that the regulation of SMAD2 and SP1 by miR-155-5p may also be affected by CagA (Wu et al. 2022).
Pharmacologic inhibitors of miRNA-155 in GI cancers
Sulfuraphane
Sulforaphane is a natural isothiocyanate that exists richly due to epidemiological studies, in cruciferous vegetables including broccoli, have received a lot of interest in oncology. They proved that eating many sulforaphane-containing Brassicaceae vegetables could reduce the likelihood of getting certain cancers, including PC (Herr et al. 1946). Treatment resistance in PC has previously been demonstrated to be overcome by purified sulforaphane, both in vivo and in vitro, with outcomes comparable to those observed in individuals with prostate tumor (Kallifatidis et al. 2009; Kallifatidis et al. 2011) and breast tumor (Li et al. 2010; Burnett et al. 2017). In the meantime, 20 men with prostate cancer recurrence participated in a phase II clinical trial and it recommended Sulforaphane-rich bud extract had a negative impact on PSA expression, a prostate-specific tumor growth marker (Alumkal et al. 2015). In spite of these hopeful outcomes, the immunoregulatory effects of sulforaphane stay mainly unidentified. Immuneoctivating and immunosuppressive properties have been reported in limited research in numerous diseases and in vitro models. That is of the highest connection due to the proportion of immune suppression to immunological activation having a vital function in cancer therapy. Although sulforaphane-enriched dietary supplements can also aid in the management of individuals suffering from cancer, their ability to regulate the immune system is still up for debate (Park et al. 1950) and necessitates more clarification. Dendritic cells (DCs) have critical function in both initiation and development of immune response through recruitment of both general and specialized immunity, are a significant component of immunological activation. In inflammatory situations such as tumors, the uptake of antigens is specifically mediated by DCs, notably through those that are differentiated from blood-selected monocytes. DCs proceeded to activate the cell, aiming to eliminate the tumor, thereby inducing a strong anti-tumor response (Melillo et al. 1950).
DC cells' maximum ability to activate T cells is jointly focused on a variety of surface regulatory molecules that send out inhibitory signals. The structurally similar glycoproteins CD86 (B7-2) and CD80 (B7-1) are the main stimulatory molecules that increase the activating signaling of T cells (Smyth et al. 2015). CD83 membrane-bound, an indicator of DC maturation in the peripheral blood, has as well potentially stimulant capability. The immunological checkpoint molecule B7-H1 (CD274, PD-L1), which is present on the surface of DCs, is an important glycoprotein that suppresses the immune system and maintains autophagy. Immune response is also controlled partially through this protein (Dunand-Sauthier et al. 2011). But B7-H1 expression may be counterproductive in cancer (Zhou et al. 2010), as it reduces the excitability of DCs (Chen et al. 2005). Many signaling pathways have been explained to regulate the expression of monitoring molecules and the properties of DCs that activate them. The Janus family of tyrosine kinases (JAKs), and the family of signal transducers and transcriptional activators (STAT), organize an important signaling pathway that decreases DC activation potential, as well as in malignancies (Waddell et al. 2015). In particular, DC function needs to be inhibited by STAT3 activation (Katsanos et al. 2022), and increased immunological activity is displayed by STAT3-deficient DCs (Mann et al. 2000).
MicroRNAs are important in DC homeostasis as they regulates growth, maturation, expression of surface molecules, and cytokine release during the gene regulation stage (Arneth 2018). When DC stimulation was utilized to activate other functional miRNAs also discovered in DCs, miR-155 stood out as being especially significant because it was discovered to upregulate maturation markers and expression of various pro-inflammatory biomarkers (Valadi et al. 2007; Baradaran et al. 2019).
Wang et al. looked for the immunomodulatory influences of sulforaphane only in humans DC and in the existence of tumor antigens, along with the fundamental mechanisms of molecules (Wang et al. 2022; Kim et al. 2021). Human DC treated with sulforaphane produced a range of cytokines during their in vitro development, and the regulatory molecules levels were evaluated using flow cytometry. T cell increase and CD25 production have been used to further analyze the T cell response. DC cells were combined with cancer antigens derived from PC in order to validate the findings. The microRNA signaling pathway and DCs treated with sulforaphane were elucidated using different methods such as Western blot analysis, microRNA collection, dampen of different signaling pathways, and bioinformatics analysis. By regulating the production of inhibitory B7-H1 molecules and excitatory CD83 and CD80 molecules on DCs, sulforaphane promotes T-cell activation. Efficacy was shown in the existence of pancreatic cancer antigens. Sulforaphane lowers intracellular STAT3 phosphorylation in DCs, and JAK/STAT3 inhibition lowers B7-H1 expression. MiR-155-5p inhibition has substantial effects on the homologous promoters expression, while miR-194-5p induction targets the B7-H1 gene and is one of the top 100 identified major microRNA contenders. According to their findings, sulforaphane increases T-cell activation through DCs through JAK/STAT3 signaling pathway and microRNA, in addition to through the modification of controlling molecules in the nonexistence of derived antigens and in conditions typical of PC. They looked into sulforaphane's immunomodulatory effects and advocated for more study on dietary interventions in conjunction with concurrent cancer treatment (Wang et al. 2022; Kim et al. 2021).
Resveratrol
Resveratrol (Res), a natural polyphenolic composite found abundantly in many types of dietary foods and herbs, was demonstrated to possess potent anticancer properties these years. Studies reported the critical role of Res on cancer progression and metastasis in diverse kinds of cancer (Spaeth et al. 2008). Accordingly, it can be postulated that Res can be considered as a promising treatment or preventative medication for cancerous conditions (Yi and Song 2012). Additionally, some researches have demonstrated that Res displays its antineoplastic impact through the regulation of microRNAs (miRNAs) expression. As an illustration, The investigation carried out by Sheth et al. (Greco and Rameshwar 2012) indicated that prostate cancer cell growth and metastasis inhibition was facilitated via Res, which acted by regulating the expression of miRNA-21.
Studies have discovered an aberrant existence of miR-155-5p in diverse malignancies such as malignancies of breast, lung, and cervical regions, indicating a positive correlation with a poor prognosis (Klopp et al. 2007; Kidd et al. 2009; Rutkowski et al. 2015). The present literature does not provide a conclusive understanding regarding the possible upregulation of miR-155-5p in gastric tumor, or the extent to which Res may modulate miR-155-5p translation in stomach malignancies as a means of impeding tumor advancement. The current study examined the role that miR-155-5p plays in gastric malignancy as well as the effectiveness of Res in modifying the miR-155-5p transcription. Finding a new treatment target for this illness's treatment was the goal.
Apigenin
Numerous researches have recommended that gastrointestinal cancers such as PC can be prevented by increased consumption of dietary fruits, cereal grains and vegetables (Brandt and Goldbohm 2006; Taylor and Greenwald 2005; Silverman et al. 1998). In view of the increase in cancer cases, the anticancer effects of bioflavonoids, which are organic substances like apigenin (API), were investigated both in cell lines and in animal studies. Different malignancies such as lung, prostate, liver, breast, melanoma, prostate cancer, and osteosarcoma were evaluated through these studies (Villalobos-Ayala et al. 2020; Ujiki et al. 2006; Ashrafizadeh et al. 2020; Angulo et al. 2017; Zhao et al. 2017; Lee et al. 2014; Pan et al. 2013; Shukla et al. 2014; Qin et al. 2016; Perrott et al. 2017). Initiation of cell cycle arrest in autophagy is a consequence of induction of apoptosis by API. Additionally, API may reduce the motility of malignant cells, preventing cancer metastasis and incursion by controlling the molecular routes of NF-κB, p53, Wnt/β-catenin, JAK/STAT, MAPK/ERK, and PI3K/AKT (Ahmed et al. 2021; Yan et al. 2017). The ability of API to fight cancer and reduce gemcitabine resistance has been demonstrated (A chemotherapy medicine consumed for PC) within human PC cell lines (Johnson and Gonzalez de Mejia 2013). Additionally, both p53-dependent and p53-independent methods have been shown to be used by API to cause apoptosis (Jang et al. 2022). API causes apoptosis to be activated includes pathways in cancer cells that are both intrinsic and extrinsic (Chen et al. 2016; Oishi et al. 2013). Caspases 3–9, apoptosis related proteins such as Bax, Bad, Bim, Bak, Bid, XIAP, Bcl–xL, Mcl-1, and Bcl-2, along with other signaling pathways like m-TOR/PI3K/AKT, STAT3, p53, p21, and p27, as well as NF-B, Jun, FOXO3a, AIF, DR5, ERK/JNK/p38 MAPK, Noxa, Smac, Survivin, PUMA, FAS, and TRAIL are among the targets of apoptosis that API targets (Jang et al. 2022). It has been shown that API is the most efficient way to destroy cancer cells while sparing healthy cells (Shukla and Gupta 2010). According to some research, mice treated with a vehicle did not have the same tumor loads, better immune activation against malignancy and decreased death as mice with PCs (Villalobos-Ayala et al. 2020; Nelson et al. 2017).
In the bone marrow (BM) of PC-affected mice, Husain et al. report that API inhibits miRNA-155 to regulate SHIP-1 transcription, which affects the TME and anti-tumor immune response (Husain et al. 2022). They found that API boosted SHIP-1 expression and decreased miRNA-155 when PC was present. In the TME of heterotopic, orthotopic, and transgenic SHIP-1 deletion preclinical mouse models of PC, this promoted anti-tumor immune responses and helped restore myelopoiesis. According to the researchers' findings, PC healing interventions and enhancing anti-cancer immune responses can benefit from miR-155-based SHIP-1 manipulation (Husain et al. 2022).
Exopolysaccharides
Exopolysaccharides (EPSs) represent a diverse collection of biologically synthesized, natural heterogeneous sugar polymers, which can either be weakly attached to cellular surfaces or released into the surrounding habitat by a plethora of organisms (Uccello et al. 2012).
The antitumor properties of EPSs created by Lactobacillus strain have been the subject of numerous investigations. Different factors influence on this phenomenon, including the branching points, molecular weight, side chain and backbone structures of the polymers, and the composition of the monosaccharides. Existing research suggests that the branching sites and mannose and glucose residues inside the repeating units of EPS structures play a major role in enhancing their antitumor properties (Hotel and Cordoba 2001). The precise biological mechanisms by EPSs facilitate their antitumor properties have yet to be clearly elucidated.
Emam et al. investigate a hypothesis concerning the potential role of EPS in promoting its anti-tumorigenic effect by means of controlling the miR-155 expression and its related pathways (Iannitti and Palmieri 2010). The current research elucidated the miR-155 expression profile and a cohort of targeted genes via the utilization of real-time PCR. The researchers were able to successfully extract and purify an exopolysaccharide exhibiting significant cytotoxicity towards various malignancy derived cell lines including MCF-7, HepG II, and Caco-2, as stated in their study. The investigation revealed the inhibitory role of EPSs on the carcinogenic miR-155. Collectively, this study provides important insights into the biological pathways that mediate the effects of extracellular polymer suspensions (EPSs) and clarifies a different prospective mechanism of the anti-tumorigenic capability of EPSs in cancerous cells. Additionally, this finding creates opportunities for the development of novel cancer treatments, specifically those targeting miRNA through the use of anti-miRNA therapeutics (Iannitti and Palmieri 2010).
Probiotics
The typical gastrointestinal microflora is composed of distinct species that become established under specific conditions. Several environmental factors, including probiotics, have been reported to modify the gut microflora configuration and elicit advantageous effects on the host (Grajek et al. 2005; Quigley 2010). Several studies have shown that the ingestion of probiotics yields efficacy in a variety of illnesses' therapy, such as gastroenteritis, genitourinary infections, and cancers, (Khavari-Daneshvar et al. 2017; Agah et al. 2019; Singh et al. 1997; Ranji et al. 2015). Probiotic bacteria Bifidobacterium bifidum (B. bifidum) and Lactobacillus acidophilus (L. acidophilus) have been shown in previous research to have optimistic effects on individuals health. This study examines the effectiveness of probiotics containing Bifidobacterium bifidum in preventing colon cancer caused by azoxymethane (AOM) (Kreuzer-Redmer et al. 2016; Ohland and Macnaughton 2010). The viability and sustainability of the probiotics have been assessed within the gut microbiota at the initial and final phases of probiotic supplementation (Schetter and Harris 2009). Evaluation of specific tumor factors and critical immunity—specifically, T cells and cytokines—associated with colon cancer is very important (Kreuzer-Redmer et al. 2016). Hydrogen peroxide and bacteriocins, two antimicrobial agents, are among the several useful compounds produced by probiotics which made them beneficial for gastrointestinal tract (Heydari et al. 2019). Here, the effects of butyrate, a short-chain fatty acid, are shown to dramatically change the expression of the genetic code that codes for the synthesis of microRNAs and proteins. Probiotics may have a molecular mechanism through miRNAs (Ashihara et al. 2015), which are important in homeostasis along with pathological processes (Rosenbluh et al. 2014). Previous research has suggested as much.
Hence, an enhanced comprehension of the impact of probiotics on microRNAs implicated in colorectal carcinoma and their effector gene signaling pathways (e.g., PTEN, APC, KRAS, and PU.1) could potentially expedite the advancement of probiotic-centered protocols for the management and prevention of CRC (Rossini et al. 2013).
After induction of CRC in mouse by azoxymethane (AOM, Heydari et al. discovered the effects of probiotic administration, specifically Lactobacillus acidophilus and Bifidobacterium bifidum, on the regulation of microRNAs 26b, 135b, 18a, and 155, along with the modulation of their target proteins, like PTEN, APC, KRAS, and PU.1. (Sebio et al. 2014). A total of 38 male BALB/c mice have been subjected to random allocation into four distinct groups, comprising of control, AOM, Bifidobacterium bifidum, and Lactobacillus acidophilus. This was aimed at investigating the probiotics’ influence on miRNAs and their corresponding specific genes. Excluding the control group, each group was administered AOM (15 mg/kg, s.c) every week for three following weeks to cause mice to develop colon cancer. The test subjects have been administered 1.5 g of L powder. Co-culture of acidophilus and Bifidobacterium species at a concentration of 1 × 10^9 cfu/g was investigated in this study. The bifidobacterium bifidum strain was administered at a concentration of 1 × 109 colony-forming units per gram in 30 cubic centimeters of drinking water to the relevant groups for a duration of five months. Upon completing the study, the subjects were humanely euthanized, and biological specimens consisting of colon and blood tissue samples have been extracted to be used in upcoming molecular analyses. The results of this investigation show that the AOM cohort had substantial higher levels of miR-155, miR-135b, and KRAS than the control group. This was demonstrated by a notable upsurge in the expression patterns of these molecules in the colonic plasma and tissue specimens. Conversely, the administration of probiotics resulted in an inhibition of these molecular markers translation. Furthermore, the AOM-treated group exhibited a reduction in the expressions of miR-26b, miR-18a, pu.1, apc, and pten relative to the control group. Conversely, supplementation with probiotics significantly increased the expressions of the mentioned genes. Current research indicates that by upregulating tumor downregulating miRNAs and their specific target genes while reducinng oncogenes, Bifidobacterium bifidum and Lactobacillus acidophilus may improve the outcome of CRC (Sebio et al. 2014).
Zhang and colleagues analyzed the effects of administering Bifidobacterium triplex viable capsules before and after surgery on the levels of miR-155-5p in the blood of individuals with colorectal cancer. The objective of this research is to establish a basis for further investigation into the effectiveness of Bifidobacterium triplex live capsules in promoting healing after surgery among individuals with CRC. It was discovered that undergoing a significant surgical procedure decreases the levels of miR-155-5p in the blood serum of individuals with colorectal cancer. The utilization of Bifidobacterium triplex live capsules plays a crucial role in promoting faster healing after major CRC surgery, and the principal machinery may include the control of serum miR-155-5p levels. (Zhang et al. 2024).
Berberine
Berberine has been deemed suitable for addressing intestinal infections and diarrhea, and scientific evidence indicates its capacity to alleviate inflammation and combat tumors in diseased intestinal tissuesDespite evidence of the anti-inflammatory properties of berberine, it is still uncertain if this is a contributing factor to its efficacy in treating colitis-associated colorectal cancer (CACThe study conducted by Ling and colleagues presented that the amounts of miR-155-5p was decreased and the expression of suppressor of cytokine signaling 1 (SOCS1) was increased in cells treated with berberine. Significantly, the miR-155-5p inhibitor greatly reduced the impact of berberine on the SOCS1 pathway and the polarity of macrophages. In summary, their discoveries indicate that the suppressive impact of berberine on the growth of CAC is reliant on its ability to reduce inflammation. In addition, it is suggested that miR-155-5p may function in the improvement of CAC by controlling the polarization of M1 macrophages. In this regard, berberine shows potential as a protective agent against CAC triggered by miR-155-5p. The research offers a fresh perspective on the pharmacological actions of berberine and suggests that utilizing other medications targeting anti-miR-155-5p could potentially have positive effects on managing CAC (Ling et al. 2023).
miRNA-155 and circular RNAs in GI cancer
Circular RNAs,or circRNAs for short, are a novel class of RNA which attract scientists attention recently. They are closed in a circle and lack specific ends, due to their circular structure as linear RNAs are known as 5′ caps and 3′ poly (A) tails (Elton et al. 2013; Liang et al. 2019; Liang et al. 2019). CircRNAs are very stable due to their circular structure. Studies showed the specific expression of these molecules in particular cells or tissues, distributed throughout the body, and contained in exosomes and plasma (Mycko et al. 2012; Oertli et al. 1950; Murugaiyan et al. 1950). According to recent research, circRNA—a particular type of RNA—functions in both healthy bodily processes and illnesses like cancer. CircRNAs could be really good markers for cancers, and could help figure out what might be causing them. It has recently been discovered by scientists that circRNAs are acting as sponges for miRNAs to regulate transcription and react to microRNAs, or miRNA response elements (MREs). This is vital for the enlargement and spread of tumors (Xiao et al. 2009). Although investigations have shown that hsa_circ_0000592 and hsa_circ_006100 function in causing stomach tumors, more research is needed to understand how circular RNAs contribute to the development of GC caused by environmental factors.
Niu et al. found a new circRNA, called hsa_circ_0001829 that was more dynamic in human stomach cells that had ended up cancerous due to chemical introduction. They utilized a strategy called RNA-seq to identify this modern circRNA (Fassi Fehri et al. 2010). The researchers tried the GC cells and tissues to see how much hsa_circ_0001829 was display utilizing qRT-PCR and ISH measures. They tried the parts of hsa_circ_0001829 in GC by doing tests to see what happens when they increment or diminish its action. Researchers utilized computer expectation and a test called the luciferase test to consider how hsa_circ_0001829 might work. Subsequently, animal experiments showed the role of hsa_circ_0001829 in their bodies by considering the start and advancement of cancer. They found that both GC tissue and cell lines exhibit a noticeable expansion of hsa_circ_0001829. According to tests, hsa_circ_0001829 increases the growth, migration, and assault of stomach cancer cells. Because hsa_circ_0001829 affects both the regulation of apoptosis rates and the progression of the cell cycle, it may have an impact on the increase of gastric tumor cells. Furthermore, the employment of bioinformatic prediction techniques and subsequent luciferase-based assays have revealed that hsa_circ_0001829 exerts its mode of action serving as miR-155-5p's molecular sponge, and that SMAD2 serves as a prime target gene for miR-155-5p. Additionally, hsa_circ_0001829 effectively sequesters miR-155-5p, and modulates production of SMAD2 to regulate the GC promotion as a result of the miR-155-5p-SMAD2 pathway. In conclusion, the repression of the hsa_circ_0001829 gene expression effectively impeded neoplastic proliferation and potency within an in vivo setting. Collectively, the outcomes of their research have primarily exhibited that hsa_circ_0001829 has a novel oncogenic role in the development of stomach cancer via the miR-155-5p-SMAD2 axis. Furthermore, their research identifies possible treatment targets and biomarkers for gastric cancer (Fassi Fehri et al. 2010).
Globally, colorectal cancer is considered the top third widespread category of cancer (Schreiner et al. 2020; Hansen et al. 2013). Colon cancer is a widespread disease that occurs more frequently than colon cancer, especially in developed countries, where there are twice as many cases of colon cancer compared to rectal cancer. Additionally, there is a slightly higher number of females diagnosed with rectal cancer compared to males. In contrast, underdeveloped nations display similar levels of both types of cancer. Each year, an estimated 250,000 individuals in Europe are diagnosed with colon cancer, making up about 9% of all cancer diagnoses (Hansen et al. 2013).
It has been stated that numerous circRNAs are able to regulate the potential of metastatic CRC by functioning as sponges for miRNAs and RNA-binding proteins (Ren et al. 2020; Wang et al. 2019a; Chen et al. 2020). It has been demonstrated that the miR-145-5p-sponging circular RNAs circRUNX1 and circPVT1 promotes the upregulation of their individual target gene expressions and further potentiate colorectal cancer metastasis ability (Ji et al. 2022; Li et al. 2018a). Circ_0001178, has been found to augment the metastatic potential of CRC through impeding the activity of miR-382/587/616, which is responsible for targeting the transcriptional repressor, ZEB1 (Han et al. 2014). Through the miR-370-3p/NF1 signaling pathway, the current study has shown that circITGA7 can inhibit the lymphatic metastasis of colon cancer (Li et al. 2015b).
Ji et al. found hitherto undiscovered circRNAs that may exhibit control over colorectal cancer (CRC) liver metastasis (Emam et al. 2021). The current study aimed to identify circRNAs that were expressed differently in KM12L4 colon cancer cells metastasis to the liver compared to main KM12C ones using microarray analysis. CircRNAs have been counted utilizing semi-quantitative polymerase chain reaction (semi-qPCR) and RT-qPCR techniques. The malignant activities such as movement and attack abilities and the inclination toward liver metastasis, was investigated using intrasplenic injection and transwell assays, respectively. RNA-binding protein (RBP) and microRNA (miRNA) were screened for CircPPFIA1 association using antisense oligonucleotide (ASO) pulldown experimentation. RT-qPCR and western blot analyses were recruited for assessing circPPFIA1's regulatory role on its targets.
Utilizing analysis of circRNA-related microarray data, 2 distinct circRNA species exhibiting anti-metastatic properties were pinpointed, emerging from PPFIA1, and were designated as circPPFIA1-S (short) and circPPFIA1-L (long) on the basis of their respective lengths. In comparison to main KM12C cells, liver metastatic KM12L4 cells exhibited a noteworthy downregulation of the aforementioned markers. Such observations suggest particular molecular modifications occurring during metastatic progression. The silencing of circular RNA PPFIA1 in KM12C cells resulted in an augmented metastatic propensity and a heightened incidence of liver metastases. In contrast, the upregulation of circular RNA PPFIA1s was observed to attenuate the metastatic capacity and impede hepatic metastasis. An antisense oligonucleotide (ASO) pulldown test carried out in the study demonstrated that circPPFIA1s serve as molecular harbingers for oncogenic HuR and miR-155-5p. By decoying miR-155-5p and sequestering HuR, circPPFIA1s functionsed to increase the expression of tumor-suppressive CDX1, while simultaneously downregulating oncogenic RAB36.
According to their study's findings, circPPFIA1s can block the HuR/RAB36 and miR-155-5p/CDX1 pathways, which prevent colorectal cancer (CRC) from spreading to the liver (Emam et al. 2021).
miRNA-155 and immune-Related Cells in GI cancers
MiR-155 serves as a crucial controller of immune reactions towards malignancies. MiR-155 has a significant impact on adjusting both natural and learned defense mechanisms in diverse cells within the immune system. Therefore, miR-155 may be able to transfer of information between tumors and immune cells, potentially influencing the process of tumor immunoediting. Many research investigations have demonstrated the impact of this molecule on immune reactions against tumors, leading to its gradual utilization in cancer treatment (Kalkusova et al. 2022). MiR-155 has a vital role in controlling and modifying the immunoediting mechanisms at various stages, impacting both cancerous and immune cells. Its involvement in communication between these cells is also significant and can greatly influence the severity of the ailment and its reaction to therapy. The unique qualities of miR-155 indicate that it has great potential as a focus in the areas of cancer diagnosis, prediction of disease outcome, and therapeutic interventions (Kalkusova et al. 2022).
MiR-155 is a remarkable microRNA among the array implicated in gastric adenocarcinoma initiation, advancement, and immune checkpoint modulation. Its upregulation has been postulated as a critical indicator of prolonged gastric inflammation that incites the vulnerability of patients to gastric carcinogenesis. Furthermore, miR-155 is markedly overexpressed in activated T and B cells as well as in macrophages/ monocytes. Furthermore, current research advocates that several physiological systems, including immunology, oncogenesis, inflammation and cardiovascular diseases, depend critically on miR-155-5p. Pathologies that are attributed to miR-155 are of significant clinical importance due to the observed overexpression of this microRNA. The aforementioned observation proposes a prospective approach towards curbing miR-155-5p levels for the purpose of mitigating gastric cancer or/hand forestalling the development of chronic gastric inflammation into neoplasia (Tili et al. 1950).
An advantageous method for examining the effects of T-cell differentiation and stimulation is the in vivo model that lacks miR-155 expression. After careful analysis, it has been determined that miR-155 plays two roles: one inherent to T cells in TH17-cell differentiation, and the other indirect, influencing DCs' production of cytokines that polarize TH17 cells (Prinz and Weber 2020). In the nonexistence of miR-155 in T cells, an in vivo model of H has been demonstrated to display compromised TH17-cell reactions. In vivo studies of TH17-driven chronic colitis were conducted in conjunction with Helicobacter pylori infection (Varoni et al. 2016). The present study suggests that miR-155 exerts control over inflammatory tissue mediated by T cells by modulating the responses of not only TH1-cells but also TH17-cells. In contrast, the miR-301a upregulation has been found to increase TH17-cell differentiation. This might be explained by the targeting of PIAS3, a protein that inhibits STAT3 signaling and, in turn, TH17-cell differentiation (Zhang et al. 2018a). The information provided here clearly points to miR-155's possible importance in aiding in the elimination of immunological responses and the activation of Tregs (T regulatory).
When H. pylori infections occur in gastric epithelial cells, the body produces moremiR-155 (Sheth et al. 2012), and this expression is linked to a specific kind of stomach cancer known as gastric adenocarcinoma. The pathway known as activator protein 1 (AP-1) is essential to the regulation of miR-155. This happens in B cells (Fang et al. 2016) and in mice's defense cells called macrophages (Kong et al. 2014). Significantly, elevated Foxp3 has been demonstrated to regulate T cell miR-155 expression (Sheth et al. 2012). Furthermore, immune cells which counteract with LPS express different miRNAs like miR-132, miR-146a, and miR-155 (Yanaihara et al. 2006). Several studies using C57Bl6 mice and murine macrophages have shown that a range of toll-like receptor ligands can induce primary macrophages to produce miR-155 (Su et al. 2022). Given the considerable influence that miR-155 has on the gastric cancer progression, it is possible that this specific microRNA is involved in determining the date at which gastric cancer first appears before tumorigenesis and metastasis. Consequently, the study showed increase of different types of miRNAs, specifically miR-155, in immune cells located in the stomach region in the existence of H. pylori. infection with Helicobacter pylori. Patients with chronic inflammation showed increased incidence of gastric cancer and its subsequent metastasis. This could be explained by the positive association between Foxp3 + Tregs and noncoding miR-155 molecule activation with STAT3 triggering.
Noncoding microRNA dysregulation and further aberrant immune cells activation could explain the gastric inflammation induced by H. pylori and further gastric malignancy. The reduction of incompatible repair genes and potential disruption of immune checkpoint proteins have been connected to the high expression of antigens on stomach cancer cells. It has been explained that a multitude of miRNA molecules functions as markers and contributors in the development of gastric swelling and cancer. These miRNAs, miR-145, miR-21, miR-143, miR-335, and miR-201, are important players in the development of cell cycles and tumor invasion. It is proven that stomach tumors downregulate each of these miRNAs. MiR-155 is a distinct microRNA among the many involved in the controlling of immune checkpoints, gastric swelling, and the development of adenocarcinomas. It is distinct because of its overexpression, which suggests persistent stomach inflammation and makes people more likely to develop stomach cancer. Of the many different types of microRNAs (miRs), miR-155 is particularly noteworthy because of its significant upregulation in different immune cells such as monocytes, macrophages, activated B and T cells, which are found in prolonged gastric inflammation. Notably, miR-155 downregulates the expression levels of different genes elaborate in Mismatch Repair (MMR), namely MSH6, MSH2, and MLH1. Specifically, it is shown that the administration of antibodies targeting immune checkpoint proteins reinstated the expression of many previously downregulated miR-155 targets in CD8 + T cells missing tumor-infiltrating miR-155. These findings implicate miR-155 in the regulation of intersecting pathways that foster the advancement of antitumor immunity. The potential for significant clinical ramifications exists due to the mediation of gastric pathologies by miR-155 consequent to its excessive expression. The observation mentioned above suggests that reducing the levels of miR-155 therapeutically could be a feasible strategy for managing gastric cancer clinically and preventing chronic inflammation in the stomach from developing into carcinogenesis (Pittenger et al. 1999).
miRNA-155 and stem cells in GI cancer
Bone marrow derived mesenchymal stem cells (BM-MSCs) have innate characteristics, including self-renewal, pluripotent differentiation capacity, immunoregulatory abilities, and pronounced affinity towards inflamed regions (Jung et al. 2013; Barcellos-de-Souza et al. 2016; Haviv et al. 2009). BM-MSCs have been shown to be potential sources of cells for gene therapy in numerous diseases especially cancers (Mishra et al. 2008). Thanks to developments in the field of tumor microenvironment research, scientists now recognize that changes in cancer cells are not the only factors influencing the growth of tumors; the presence of cancer-associated stroma also plays a role (Peng et al. 2013). An increasing amount of data advocates that Mesenchymal Stem Cells Derived from Bone Marrow (BM-MSCs) can be activated and incorporated into the cancer tissue stroma, which in turn promotes the growth of neoplastic tissue (Cao et al. 2009; Weber et al. 2015; Shangguan et al. 2012).
Multiple stromal cell categories, like immune cells, endothelial cells, mesenchymal stem cells (MSCs), cancer-associated fibroblasts (CAFs), and other cell components, make up the tumor microenvironment. Of the various types of stromal cells, a noteworthy cell type is the cancer-associated fibroblasts (CAFs), which have been subject to growing attention with respect to their origins in current years (McLean et al. 2011). Increased evidences have been pointed to this point that MSCs of bone marrow can integrate into new tumors and differentiate into cancer-associated fibroblasts (CAFs) in vivo (Cao et al. 2009; Waghray et al. 2016; Yan et al. 2013). Cancer cell-conditioned medium has been identified as a critical signaling cue for the well-established in vitro phenomenon of bone marrow-derived mesenchymal stem cells (BM-MSCs) differentiating into cancer-associated fibroblast (CAF)-like cells (Mitra et al. 2012; Hu et al. 2005; Lin et al. 2016; Haga et al. 2015). In recent times, mesenchymal stem cells (MSCs of malignant tissues, have been effectively known and classified within many solid tumor variants, such as gastric cancer (Shen et al. 2016), ovarian carcinoma (Pang et al. 2015), hepatocellular carcinoma (Wang et al. 2018a), and PC (Yin et al. 2020). Research conducted in vitro has demonstrated that cancer cells have a major effect on the BM-MSCs differentiation, similar to the cells derived from cancer tissue, into MSCs. This transformation is mediated through paracrine mechanisms (Li et al. 2018b).
An investigation conducted pertaining to breast cancer stroma through a genome-wide analysis postulates that tumor stromal cells manifest frequent instances of epigenetic changes (Li et al. 2020). miRNAs are important epigenetic regulators for phenotypic transition of normal fibroblasts (NFs) into CAFs. An excellent example has been explored in the research work of Mitra et al. (Qu et al. 2018), where it was shown that NFs were transformed into CAFs as a result of the manipulation of deregulated miRNAs, specifically miR‑31, miR‑241, and miR‑155, during ovarian tumor progression. Shen et al. (Zare et al. 2019) clarified that normal fibroblasts (NFs) in lung cancer underwent a functional conversion process into cancer-associated fibroblasts (CAFs) due to the high expression of miR-206 and miR-1 and the decreased production of miR-31. Pancreatic neoplastic cells have been observed to release microvesicles carrying miR-155-5p which prompts the process by which healthy fibroblasts become CAF (cancer-associated fibroblasts) (Gironella et al. 2007). Notwithstanding the existence of research focused on miRNA's involvement in governing the evolve of BM-MSCs into cancer cells, the current knowledge base remains in its preliminary stages.
MSCs generated from murine bone marrow (BM-MSCs), also known as mMSCs, were cultivated in conditioned media obtained from the MFC, also known as MFC-CM, a malignant cell line in a study by Wang et al. (Ma et al. 2020). MSCs have ability in induction of neoplastic-accelerating properties and activities through the application of multiple established methodologies, such as the Transwell migration assay, qRT-PCR, immunofluorescence-based staining, and invasion assay. Luciferase assays and western blot studies have been performed to determine the association between the mmu-miR-155-5p and NF-κB-p65. Role of miR-155-5p-NF-κB signaling in the mMSCs through MFC-CM was assessed via pyrrolidine dithiocarbamic acid (PDTC), inhibitor, and miRNA mimics. The education model of murine mesenchymal stem cells was successfully established through employment of MFC-CM. The findings of the study reveal a notable reduction in the mmu-miR-155-5p production amounts within the mMSCs. The induction of deregulation in mMSCs through the transfection of miRNA inhibitor was found to elicit a comparable impact as that of MFC-CM on mMSCs. It has been determined that mmu-miR-155-5p affects NF-κB p65 and also has a negative modulatory effect on NF-κB activation. The impact of the miRNA inhibitor on murine mesenchymal stem cells (mMSCs) was found to be nullified upon the application of pyrollidine dithiocarbamate (PDTC), which resulted in the inhibition of the NF-Κb activation. The elevated expression of mmu-miR-155-5p demonstrated limited hindrance of the impact of MFC-CM in instructing mesenchymal stem cells (mMSCs), whereas treatment with PDTC led to the total abrogation of MFC-CM activity. The present study's findings rejected the mere role of this miRNA for the enhancement of the teaching capacity of gastric cancer cells on BM-MSCs. Instead, this phenomenon is largely dependent on downstream NF-κB signaling (Ma et al. 2020).
miRNA-155 as diagnostic/prognostic biomarker in GI Cancer
Nowadays, fluid biopsy may be a potential diagnostic methodology that complements instead of an elective to routine diagnostic strategies. Fluid biopsy may yield transcriptome and proteome data regarding the temporal and regional heterogeneity of a tumor (Liu et al. 2012b; Cote et al. 2014). A model for a single tissue biopsy can be one-sided and disputable, whereas fluid biopsy is generally not invasive, repeatable, and gives by and large tumor data. Molecular data gotten by fluid biopsy can give a specialist with more specific information to direct treatment and surgical planning. Therefore, screening, prognosis, diagnosis, and therapy for people with cancer could alter significantly in the close future via fluid biopsy. Available blood tests to use fluid biopsy to look for cancer hints incorporate the cancer screening and diagnosis biomarker circulating serum antigen 19–9 (CA19-9). Though, raised CA19-9 was observed in a few sufferers of mild pancreatobiliary diseases, recommending that CA19-9 isn’t highly exclusive for cancer marker (Pang et al. 2015; Lee et al. 2021). Fluid biopsy is limited by the fact that circulating biomarkers typically have low blood concentrations and might degrade quickly, in addition to false positives (Huang et al. 2013). Lately, broad researches affirmed that Patients with PC have dysregulated levels of numerous miRNAs. Hence, Early-stage PC and metastatic cancer may be distinguishable from one another in serum miRNA expression patterns (Liu et al. 2013). miRNAs exchange to adjoining cells is mainly mediated via extracellular vehicles (EVs), that load profitable markers (DNA, mRNA, miRNA, and protein) that show traits comparable to those of their parent cells (Wang et al. 2015). Evs are prevalent in the bloodstream, have a long circulation period, and shield stem cell-derived molecular information. Subsequently, it has been proposed that tumor-derived EVs could serve as possible cancer dignosis markers.
Kim et al. revealed that pancreatic ductal adenocarcinoma (PC)-derived extracellular vesicles (PDEs)had significantly upper production levels of five miRNAs: miR-10b, miR-155, miR-16, miR-429, and miR-1290 (Wang and Gao 2021). Additionally, PC patients is distinct from non-cancer controls using the combination markers (CMs) of the miRNA signature and serum carbohydrate antigen 19–9 (CA19-9). By using computed relapse, the miRNA markers and serum carbohydrate antigen 19–9 (CA19-9) were improved. In the end, the CMs reported high affectability (AUC of 0.964; 100% sensitivity; 80% specificity) and high specificity (AUC of 0.962; 85.71% sensitivity; 100% specificity). These results imply that five miRNAs present in PDEs and CA19-9 are useful indicators for fluid biopsy diagnosis and PC screening (Wang and Gao 2021). Identification and treatment in the primary stages of PC are the best ways to lower PC-related death rates. Regardless, high risk population such as those with prolonged forms of pancreatitis, the value of screening techniques is diminished by the need for reliable markers to identify PC (Husain et al. 2022). The common biomarkers measured during PC are carbohydrate antigen 19–9 (CA19-9) and carcinoembryonic antigen (CEA); however, for PC to be detected, these markers must be sufficiently affectable and specific. (Kim et al. 2021). The identification of symptomatic PC biomarkers is essential to enhancing the prospects of individuals’ condition with this type of malignancy. There aren't any invasive biomarkers that are extremely sensitive and specific available for PC detection right now (Papaconstantinou et al. 2013).
Lee et al. (Papaconstantinou et al. 2013) tried to develop a miRNA biomarker for primary identification of PC. Blood of 63 PC patients and 63 control subjects were taken and investigated. They chose 39 miRNA markers and used a support vector machine with unconditional deviation-based fine-cutting penalties to create a PC diagnosis model. The test's AUC with twofold cross-validation was 0.98, which is typical. In order to validate the diagnosis model, they used autonomous testing from PC patients and intrahepatic cholangiocarcinoma (ICC) ones, and used carbohydrate antigen 19–9 for diagnosis. Using tests from 8 ICC patients, 8 healthy people, and 17 independent PC patients, they conducted quantitative turn around translation PCR for the markers let-7b-5p, miR-4703-5p, miR-155-5p, miR-4284, miR-4284, miR-346, miR-5100, miR-7145-5p, miR-661, miR-4486, miR-22-3p, and miR-4486. When testing PC patients, they observed differences in expression. Excellent affectability and specificity for PC identification are demonstrated by the identified markers-based diagnostic model, indicating that it may be helpful for early PC diagnosis (Papaconstantinou et al. 2013).
In their study, Karimi and colleagues observed a notable increase in the levels of miR-146a and miR-155 in the entire blood of individuals diagnosed with both H. pylori and GC, when compared to those who were deemed healthy. Furthermore, they noted that these levels were slightly elevated among patients with a positive H. pylori identification and a negative GC identification, although this difference did not reach statistical significance. Additionally, the findings revealed a notable rise in miR-146a and miR-155 levels in the whole blood of H. pylori positive and GC negative patients, when in comparison to those of a control group consisting of healthy individuals. Moreover, an assessment of the ROC curve for the levels of miR-146a and miR-155 RNA revealed that these two miRNAs possess suitable sensitivity and specificity for achieving diagnostic objectives. To sum up, individuals with both H. pylori and GC positive diagnoses may experience an elevation in the levels of miR-146a and miR-155, potentially contributing to the suppression of GC advancement caused by H. pylori infection. Due to this factor, the increase in miR-146a and miR-155 levels in combination with H. pylori infection may have a function in the growth of GC, and potentially be utilized as indicators for the diagnosis and therapy of GC (Karimi et al. 2023).
miRNA-155 and resistance to chemotherapy
Continuous studying contributes to a more comprehensive comprehension of the molecular processes that result in resistance to chemotherapeutics in the majority of gastrointestinal cancer types. This is a main item in the inability of many currently available chemotherapeutic managements to be effective. Despite extensive research, the precise molecular processes and controlling systems underlying multidrug resistance (MDR) in several forms of cancer, including GI cancers, are yet to be comprehended (Fojo 2007). Ongoing studies have initially pinpointed a number of shared mechanisms that facilitate both natural and acquired immunity, such as changes in the structure of histones, abnormalities in the levels of miRNA expression, modifications to DNA through methylation, and modifications to pathways involved in drug metabolism. Postoperative chemotherapy is the most desirable method of treatment for individuals with gastrointestinal cancers after undergoing surgery (Magee et al. 2015).
Extensive measures have been taken to recognize individuals who may have a positive or negative reaction to chemotherapy, thus emphasizing the need for reliable indicators that can anticipate the efficacy of specific treatments. One potential solution for reversing resistance is to address the harmful changes in gene expression by specifically targeting and manipulating the miRNAs responsible for resistance in these cells. This approach has a strong potential for effectiveness (Kishikawa et al. 2015). The significance of the variability both among and within tumors in relation to anticipating the treatment response and overall outlook is commonly recognized. Evaluating the treatment response and conducting post-treatment monitoring are crucial elements in effectively managing patients with breast cancer. nowadays, many pieces of evidence have emerged indicating that miRNAs play a critical role in controlling both the development of cancer and its overall biological processes (Ye et al. 2018). The rising comprehension of miRNAs' involvement in tumor biology has the potential to guide the development of new treatments in the future. Thanks to advancements in cell biology and technology, miRNAs have gained significant attention as promising means and objectives for innovative therapeutic methods. The fundamental approach in research on miRNA-based therapy is to either counteract the influence of cancer-promoting miRNAs or to revive and enhance the activity of miRNAs that suppress tumor growth (Li et al. 2021a).
Previous study has established that dysregulated miRNAs significantly contribute to the development of chemoresistance and recurrent episodes in patients undergoing chemotherapy. One specific example is the association between miR-155 and a variety of physiological and pathological activities, like the development of chemoresistance. Gao and colleagues provided evidence that miR-155 plays a significant role in promoting the resistance of colon tumor to cisplatin treatment by specifically targeting forkhead box O3. After extensive research, it was determined that miR-155 exhibited a significant increase in expression levels within both colon cancer tissue and cell lines. Experiments on cells discovered that an increased amount of miR-155 meaningfully boosted resistance to cisplatin in colon cancer cells and also upheld the formation of tumors in vivo. Furthermore, upregulation of miR-155 was linked to reduced levels of FOXO3, mainly by suppressing its production, leading to boosted resistance of colon cancer to cisplatin. This research illustrated that miR-155 had a direct correlation with the improvement of drug resistance in colon cancer and also results in a decline in the production of FOXO3 in either animal models and laboratory experiments (Gao et al. 2018).
In their study, Li and colleagues found compelling evidence of a significant correlation between the levels of miR-155-5p and resistance to paclitaxel. By observing the upregulation of miR-155-5p in resistant cells, they established a clear link between its production and the development of resistance. In addition, the overexpression of TP53INP1, which is the target gene of miR-155-5p, helped to restore the sensitivity of resilient cells to paclitaxel. The following joint application of reducing miR-155-5p levels and increasing TP53INP1 expression resulted in increased sensitivity to paclitaxel in previously resistant cells (Li et al. 2021b).
According to Kirave and colleagues, exosomes have a function in significantly increasing the expression of miR-155 in oral squamous cell carcinoma (OSCC) cells that have developed resistance to cisplatin (known as cisRes cells). Significantly, it was discovered that the transmission of exosomes from cisRes cells to cisplatin sensitive (cisSens) cells resulted in a considerable increase in miR-155 expression in the receiving cisSens cells. Re-establishment of miR-155 levels in cisSens cells through treatment with miR-155 mimics resulted in the transformation from an epithelial to a mesenchymal state, increasing their ability to migrate and develop a resistant phenotype. Significantly, the transfer of exosomes from cisRes cells to cisSens cells resulted in comparable enhancements of migratory ability and resistance to chemo drugs (Kirave et al. 2020).
The research conducted by Roosbroeck and colleagues confirmed that miR-155 promotes conflict to a diversity of chemotherapy drugs in laboratory settings, and that reducing the levels of miR-155 can effectively restore tumor responsiveness to chemotherapy in real-life conditions. They have proven through their findings that anti-miR-155-DOPC does not have any harmful outcomes when used in living organisms. In addition, they displayed evidence that miR-155 and TP53 are interconnected in a process of mutual regulation and that having elevated levels of miR-155 and decreased levels of TP53 is strongly correlated with reduced existence rates in cases of lung malignancy (Roosbroeck et al. 2017).
miRNA-155 and associated Clinical Trials in GI cancers
According to Su et al. qRT-PCR has been executed to appraise the miR-155-5p expression within both clinical tissues and gastric cells. Furthermore, the effectiveness of the Res and miR-155-5p treatment in relation to the increase of gastric cancer cells was assessed through a diversity of experimental techniques, like the MTT assay, plate clone formation test, cell scratch test, flow cytometry, and Transwell assay (Quante et al. 2011). In this work, the expression of important proteins in a cohort of gastric tumor cell lines after being treated with Res and miR-155-5p was measured. These proteins include claudin 1, cyclin D1, c-Myc, caspase-3, and Bcl-2. Increased miR-155-5p in gastric cancer cells as well as clinical tissues was observed. On the other hand, the administration of Res effectively controlled the miR-155-5p levels and induced apoptosis in gastric tumor cells. The impact of miR-155-5p on the attack, proliferation, and metastasis dynamics of gastric cancer was investigated in cell studies. The transwell test, flow cytometry, plate clone formation test, MTT assay, and cell scratch test results proved that miR-155-5p concurrently inhibited apoptosis in the cells and significantly stimulated these processes. At the P < 0.05 level of statistical significance, the effects were effectively suppressed by the addition of Res. Upregulation of c-Myc, claudin 1, Bcl-2, cyclin D1, and downregulation of caspase-3 were observed upon higher levels of miR-155-5p. The study's overall conclusions propose that miR-155-5p could be considered as a promising target for treatment of gastric malignancy and resveratrol (Res) can control the production of miR-155-5p and it is a potential therapeutic agent (Quante et al. 2011).
In a study, miR-155 effects on TAMs drived from endometrial cancer (EC) were investigated (Liu et al. 2012c). The goal of the current study was quantification of the levels of miR-155 and fibroblast growth factor-2 (FGF2) in both tissues and in vitro samples. The employed methodologies for this investigation included both western blot assays and qRT-PCR. The aforementioned constructs have been further introduced into TAMs via transfection. Tumor-associated macrophage (TAM) culture media was then acquired in order to carry out additional research. Quantification of released FGF2 and inflammatory cytokines was measured by ELISA. Transwell analysis and CCK8 have been used to measure the levels of invasion, migration, and viability of cells. Using matrigel angiogenesis analysis, the process of vasculature formation in human umbilical vein endothelial cells (HUVEC) has been evaluated. The results of this study indicate that, compared to their normal control counterparts, both cell lines and EC tissue were found to have decreased levels of miR-155 expression but FGF2 overexpression. Furthermore, the transfection of tumor-associated macrophages (TAMs) with miR-155 mimic has been shown to up-regulate the interleukin (IL)-12, TNF-α, and inducible nitric oxide synthase (iNOS) while concurrently down-regulating the amounts of Arginase-1 (Arg-1), IL-10, and IL-22 in the culture media. Tumor-associated macrophages (TAMs) that had increased miR-155 representation reduced angiogenic activity and impeded the viability, motility, and infiltration of ECA109 cells. Nevertheless, the influence of miR-155 on cell survival, malignant behaviors, and angiogenic potential of malignant cells were neutralized by the upregulation of fibroblast growth factor 2 (FGF2). Based on the study's findings, TAM-regulated MiR-155 suppresses EC cell multiplying, migration, and attack in addition to inhibiting the formation of new blood vessels by controlling the expression of FGF2. One possible therapeutic strategy to stop the progression of EC could be to use miR-155 to regulate FGF2. (Liu et al. 2012c).
Previous studies have linked a quantity of miRNAs, like miR-20a, miR-155, and miR-183, to esophageal cancer. Such identification was achieved through the utilization of RT-qPCR technology and miRNAs chip, which examined tissue from people who had esophageal squamous cell cancer in Jiangsu, Huaian, China. Furthermore, both cancerous and adjacent noncancerous tissue samples were evaluated during this study.
Liu et al.’s study finds a strong relationship between the relative production of miR-183, miR-155, and miR-20a in esophagus tissue and increased susceptibility to esophageal cancer (Simons and Raposo 2009). The cancer patient exhibited a substantial decrease in the respective circulating miR-155 and miR-183 levels, relative to healthy individuals. After accounting for alcohol and cigarette use, the elevation of risk for esophageal cancer was found to be statistically significant for circulating miR-155. An area under the curve of 66% indicates the significant value of circulating miR-155 in esophageal cancer diagnosis. No noteworthy variance of miRNAs production between esophageal tumor samples and control ones have been seen. This finding suggests that the miRNAs that are currently in circulation come from sources other than tumor cells. Findings indicate that plasma levels of miR-155 is validate and non-invasive test for esophageal cancer early detection (Simons and Raposo 2009).
The researchers, Girolimetti et al., thoroughly examined the amounts of two types of miRNA groups (one related to resistance to chemotherapy and the other to oncogenic or tumor-suppressing activities) in a range of pancreatic cancer cells and liquid biopsies taken from a limited number of individuals. The researchers discovered that both the PC cell lines and the patients, even after undergoing gemcitabine treatment, exhibited small levels of miR-155-5p associated with cells and vesicles in comparison to the control group. The researchers found no discrepancies in their examination of the presence of miR-155-5p in the bloodstream, which was unexpected (Girolimetti et al. 2024).
Exosomal microRNA-155 in GI cancers
Exosomes are membrane-bound vesicles with differ from 40 to 100 nm sizes. They have been found in almost all biological fluid types (Fig. 2). Following their fusion with the membrane of plasma, they are secreted into the extracellular milieu from a vast majority of cellular lineages (Fig. 2). Exosome membranes predominantly comprise lipids and proteins, with a noteworthy enrichment of lipid rafts (Sato-Kuwabara et al. 2015; Gross et al. 2012; Mathivanan et al. 2010). As well as proteins, other nucleic acids have also been found to be present in the exosomal lumen recently e.g. messenger RNAs (mRNAs), miRNAs, and other non-coding RNAs (ncRNAs) (Zhang et al. 2015). Exosome circulation allows for the internalization of exosomal RNAs by nearby or distant cells. The recipient cells' physiology is then impacted by the absorbed exosomal RNAs. The increasing attention being paid to the functional properties of exosomes (Zhang et al. 2018b) indicates that the scientific community is becoming more and more interested in the role that these structures play in facilitating genetic transfer between cells. The biogenesis of exosomal miR-155 is depicted in Fig. 3.
A schema of biogenesis and function of exosomes. Exosomes are membrane-bound vesicles with different sizes from 40 to 100 nm. Following their fusion with the membrane of plasma, they are secreted into the extracellular milieu from a vast majority of cellular lineages. Exosome membranes predominantly comprise lipids and proteins, with a noteworthy enrichment of lipid rafts
A schema of exosomal miR-155 biogenesis and its function. The noncoding B cell integration cluster (BIC), which encodes miR-155, and transcribed by poly II into pri- miR-155 after stimuli, such as stimulation of toll-like receptors (TLRs). Ribonuclease—DROSHA and its cofactor binding protein cleaved pri-miR-155. GTP-dependent Exportin 5 transfers Pre- miR-155from the nucleus to the cytoplasm, where the ribonuclease Dicer1 processes it into mature but still double-stranded microRNA-155. Subsequently, argonaut 2 and miR-155 create an RISC. miR-155 in the RISC complex promotes target mRNA degradation and destabilization or inhibits its translation. This figure adapted from Kalkusova et al. 2022
The discharge of extracellular miRNAs can be separated into two key clusters, which are exosomal (being contained in extracellular vesicles) and non-exosomal. The characteristics of miRNAs not only influence their absorption into intended cells, but also present both a difficulty and a chance for the use of RNA treatments in treating cancer. Due to their capacity to serve as facilitators of communication between cells within the cancer tissue microenvironment, extracellular miRs can carry out both pro- and anti-tumor tasks, based on the targeted cell and its surroundings. Most of the miRs that originate from tumors have the function of promoting tumor growth, while those that come from host cells or the surrounding tissue have roles in inhibiting tumor growth (Syed and Brüne 2022). There are numerous benefits to utilizing exosomes as a means of transporting miR-155 to a specific cell. Exosomes act as vehicles for delivering miR-155 directly to recipient cells, thereby greatly increasing the potential for this information to cause changes in the function of the target cells. Exosomes enable cells to communicate with one another, regardless of the physical gap between them (Eshraghi et al. 2024). Exosomes, which have been recognized in bodily fluids and blood, suggest that exosomes could serve as the means for organ-to-organ communication. Moreover, exosomes could potentially possess specialized components that enable them to selectively identify and transport miR-155 to specific recipient cells, thereby increasing the efficacy of delivery (Eshraghi et al. 2024). New research suggests that variations in specific exosomal miRNAs could be indicative of certain diseases. This theory is bolstered by increasing findings that analyzing miRNA levels in exosomes obtained from bodily fluids could potentially aid in disease detection and diagnosis (Hu and Drescher 2012). Additionally, the presence of exosomal miR-155 has an impact on the regulation of genes after being taken up by cells nearby or far away. Once inside the target cell, it joins forces with the target mRNA molecule by utilizing its partial sequence complementarity. The process of protein synthesis is impeded by miRNAs, which establish a miRISC complex with particular proteins (Zheng et al. 2021).
Prior research has established a connection between colon cancers, specifically carcinoma, and the M2 macrophage phenotype. One such example is the M2 macrophage, which, according to recent research, has been connected to the development of CRC (Lan et al. 2019). It has been demonstrated that colon cancer metastasis is facilitated by TAMs exhibiting the M2 phenotype (Lan et al. 2019).
Remarkably, it has been shown that exosomes released by M2 macrophages possess the ability to induce colon cancer cells to migrate and invade (Wang et al. 2017). Furthermore, in situations involving cardiac injury, exosomes with miR-155 secreted from macrophages may alter the bioproperties of fibroblasts (Zheng et al. 2017). Moreover, an independent study demonstrated that miR-155-5p and miR-21-5p molecules were translocated towards colorectal cancer cells by exosomes released from M2 macrophages and more increase of movement and metastasis (Wang et al. 2017). Moreover, it has been shown that the transfer of miR-21 through M2 macrophage-produced exosomes influences the cisplatin susceptibility of malignant cancer cells of stomach (Wawro et al. 2019).
Zinc-finger-containing protein 12B (ZC3H12B), the ZC3H12 protein’s emerging family member, was implicated in inflammation. ZC3H12B is only functionally significant when Nedd4-BP1, YacP nucleases (NYN)/PilT N-terminal (PIN) RNase domain is intact, meaning that essential residues for RNA cleavage and binding are covered (Jolma et al. 2020). Further studies have demonstrated that the ZC3H12B protein interacts with motifs similar to the splice donor sequence, which leads to the depreciation of viral parts and useless transcripts such as unspliced ones (Ma et al. 2021). Furthermore, a digital platform has revealed that specific binding locales exist between miR-155-5p and ZC3H12B. Furthermore, in vivo studies have indicated that ZC3H12B possesses binding capabilities to the mRNA of interleukin (IL)-6, thereby governing its turnover, resulting in decreased expression of IL-6 protein following the administration of IL-1β (Jolma et al. 2020).
As stated by Ma and associates. The investigation of exosomal miR-155-5p from M2 macrophages in relation to CRC cells’ ability to evade immune responses has been conducted (Challagundla et al. 2015). Results from qRT-PCR and western blot analysis exhibited that these macrophages expressed miR-155-5p and interleukin (IL)-6 with strong expression, but ZC3H12B expression was weaker. Furthermore, exosomes—extracellular vesicles isolated from M2 polarized macrophages—have the capacity to deliver miR-155-5p to CRC cells. Via its 3 “ UTR, the ZC3H12B gene is the target of this miRNA, as determined by the dual luciferase reporter gene assay. Simultaneously, ZC3H12B and miR-155-5p have been studied in coculture with M2 macrophage-secreted exosomes on HT29 and SW48 cells using gain- and loss-of-function methods. These results showed that ZC3H12B silencing or miR-155-5p overexpression promoted the growth and antiapoptotic potential of HT29 cells and SW48, in addition to the proportion of CD3 + T cells and interferon-γ + T cells. The results of xenograft models confirm that miRNA-155-5p, which is derived from exosomes derived from M2 macrophages, downregulated ZC3H12B expression in order to promote the upregulation of IL-6. Consequently, this immune system reaction encouraged immune evasion and caused tumor development. According to the results of the collaborative research, exosomal miR-155-5p that are from M2 macrophages may help immune evasion in colonic cancer by blocking ZC3H12B-mediated interleukin-6 destabilization, which would then aid in the growth and progression of the malignancy (Challagundla et al. 2015).
The research findings indicate that miR-155-5p encapsulated in exosomes function in lowering cancer cells' susceptibility to chemotherapy. Challagundla et al. (Patel et al. 2017) have demonstrated that the intercellular communication between monocytes and neuroblastoma cells, which is facilitated by exosomal microRNA-155-5p, can promote resistance to chemotherapeutic agents within cancer cells. Furthermore, Patel et al. (Mikamori et al. 2017) and Mikamori et al. stated that following gemcitabine treatment, it was noted that both the exosomes and the cancerous cells' amounts of miR-155-5p were elevated. Gemcitabine-treated PC cells' exosomes encouraged the emergence of chemoresistance in vulnerable cells. These exosomes allowed miR-155-5p to spread, and further facilitated the development of such resistance (Mikamori et al. 2017; Santos et al. 2018). Santos et al. (Wang et al. 2019b) report that miR-155-5p might be delivered by exosomes to neighboring cancer cells by paclitaxel- and doxorubicin (DOX)-resistant breast cancer cells, enabling them to spread their chemoresistance. The study's conclusions imply that exosomal miR-155-5p might be vital in the signaling that allows chemoresistance tumor cells to carry over their conflict to cancer cells that are responsive to drugs.
In a research done by Wang and colleagues, they produced the MGC-803R gastric cancer cells, which is resilient to paclitaxel. This cells displayed improved production of microRNA (miR)-155-5p and an EMT phenotype. (Kogure et al. 2011) MGC-803S cells that were paclitaxel-susceptible were found to easily internalize exosomes from MGC-803R cells, exhibiting both the chemoresistance and epithelial-mesenchymal transition (EMT) phenotypes. Moreover, miR-155-5p molecule expression was improved and could transfer to the MGC-803S cells within the MGC-803R exosomes. MiR-155-5p was upregulated in MGC-803S cells by mimic transfection, which also amplified the level of miR-155-5p in MGC-803S exosomes and had phenotypic effects similar to those of MGC-803R exosome treatment. Previous non-cancerous MGC-803S cells are prone to malignant transformations via increased exosomal abundance. According to the current study, miR-155-5p modulates two tumor proteins: GATA binding protein 3 (GATA3) and TP53-inducible nuclear protein 1 (TP53INP1). Exosomal miR-155-5p directly targeted the targets' 3' untranslated regions to elicit an inhibitory response. According to the study's findings, MGC-803R cells' chemoresistance and epithelial-mesenchymal transition (EMT) phenotypes were reversed when miR-155-5p was downregulated. This outcome may be explained by the upregulation of TP53INP1 and GATA3, which eventually stopped MGC-803R exosomes from causing the malignancy. The outcome of this research showed that the transfer of miR-155-5p via exosomes could persuade chemoresistance and epithelial-mesenchymal transition (EMT) in stomach malignant cells resistant to paclitaxel in comparison to those that are drug-sensitive. This transfer could be attributed to the suppression of TP53INP1 and GATA3. As a result, directing attention towards miR-155-5p as a possible approach may exhibit potential in circumventing the resistance to paclitaxel in gastric cancer (Kogure et al. 2011).
Extracellular vesicles, specifically exosomes originated from hepatocellular carcinoma (HCC) cells, have been observed to transfer miRNAs that facilitate the augmentation of recipient cell proliferation (Wang et al. 2020). It has been observed that Exosome miR-567 exhibits a reversal of trastuzumab resistance, and it achieves this by restraining ATG5 (Munson et al. 2019). The exosomal miR-16-5p exhibits itself as an aim for the malignancy regarding mesothelioma (Li et al. 2018c). miR-21 (actually its 5p form) is responsible for increased peritoneal metastasis of gastric cancer (Liu et al. 2019b). It has been discovered that the induction of endoplasmic reticulum stress augments the discharge of exosomal miR-23a-3p in hepatocellular carcinoma cells, culminating in an upregulation of macrophages' expression of programmed death ligand 1 (PD-L1) (Shi et al. 2020c).
Exosomal miR-155-5p consequences on the GC progression was examined by Shi et al. in order to learn more about the underlying mechanisms (Matsumura et al. 2015). Using flow cytometry, the exosomes derived from the GES-1 and AGS were separated and identified using surface marker analysis. RT-qPCR, was then utilized to ascertain the miR-155-5p levels in isolated exosomes and tissues. The bioinformatics analysis results show that the miR-155-5p directly targets the 3'-UTR mRNA transcript of the tumor protein p53-induced nuclear protein 1. Researchers looked into how a lot of miR-155-5p exosomes might affect AGS cell migration, cell cycle development and more multiplication. According to the current study, there was a higher amounts of miR-155-5p in AGS cells and gastric cancer (GC) tissues. Additionally, it was possible to find that GC tissues had lower levels of TP53INP1 protein expression using immunohistochemistry (IHC) and immunofluorescence (IFC). The direct regulation of TP53INP1 by miR-155-5p has been observed via a reporter assay based on dual luciferase. AGS cells were found to co-culture with exosomes that had been chosen for their high concentration of miR-155-5p, which improved the cells' capacity to migrate and proliferate. According to the researchers' findings, exosomal miR-155-5p specifically influence the mRNA of TP53INP1 (Matsumura et al. 2015) in human gastric cancer cases, acting as an oncogenic agent.
Research exploring exosomal microRNA (miRNA) levels in blood have yielded disparate outcomes, with no homogenous miRNA outline identified for colon cancer. A case in point is provided by a novel study on serum, which found a positive correlation between a worse prognosis and the exosomal content of the miR-17–92 cluster in assimilation patients with colorectal cancer. In contrast, an alternative inquiry involving circulating exosomal microRNAs in sufferers of metastatic colorectal cancer identified an entirely distinct collection of microRNAs which did not comprise the miR-17–92 cluster (Ma et al. 2012).
The disparity in research findings regarding miRNAs in tumor, bio-fluids, and exosomes in the context of cervical cancer have been ascribed to varied factors, such as dissimilar patient cohorts, discrepancies in internal controls, and discrepancies in laboratory techniques (Monzo et al. 2017). Nonetheless, an anatomical pathway for exosomes and their corresponding biomarker payloads to successfully infiltrate a specific organ, remains an area of investigation that has yet to receive comprehensive analysis.
According to Monzo et al.'stheory (Shi et al. 2020c), blood from the tumor-draining vein has more evenly distributed data than from the peripheral vein. This is due to the likelihood that all of the molecular markers secreted from a malignant tumor will be found in blood from the vein that drains the tumor before they spread to a distant metastatic location. Plasma samples from mesenteric veins (MVs), of 15 CRC patients were analyzed for 754 miRNAs. An analysis of these samples revealed the identification of 13 microRNAs that are substantially related with the risk of relapse. 50 MV and 50 paired PV plasma samples from patients with stage I–III colon tumor were used in a cohort study to validate the prognostic significance of the aforementioned miRNAs. Comparing mesothelial vesicles (MV) to peritoneal vesicles (PV), four microRNAs were found to be more highly expressed including miR-328, let-7g, miR-15b and also miR-155. Moreover, patients exhibiting elevated levels of said microRNAs in MV plasma exhibited a shorter duration of relapse. Remarkably, it was observed that in individuals manifesting liver metastases, the miR-328 exosomal payload was significantly amplified in MV plasma compared to PV plasma, thereby postulating the plausibility of miR-328 in fostering hepatic metastases. According to their findings, elevated concentrations of miRNAs are discharged via the MV by the primary tumor in colon cancer, with a proportion of these being encapsulated within exosomes derived from the tumor (Shi et al. 2020c). A few investigations on the function of exosomal miR-155 in GI tumors are listed in Table 2.
Nanotechnology in miRNA-155 Delivery
Fully delivering naked miRNA is challenging due to several factors: negatively charged groups of miRNAs can impede miRNA uptake by cells, which can lead to undesired off-target or on-target effects. Additionally, miRNAs have a short half-life in physiological conditions, making it difficult to achieve long-term effects. Moreover, delivering naked miRNAs may trigger an unfavorable immune response, further complicating the process (Lee et al. 2019). Non-pathogenic NPs play a crucial role in protecting miRNAs by forming a protective layer around them, which effectively conceals charge groups and enables easier transport into cells. Incorporating specific receptor-binding molecules onto nanoparticles (NPs) enables targeted delivery of microRNAs (miRNAs) to specific cells, resulting in a decrease of unintended impacts on non-target cells (Blanco et al. 2015). NPs enable precise regulation of miRNA release, preventing overstimulation of numerous gene targets. Additionally, they prolong the in vivo stability of miRNA through safeguarding the therapeutic cargo against degradation. Additionally, incorporating a stealth coat on NPs inhibits their removal by the reticuloendothelial system (RES) and prevents any negative immune cell activation. NP-based techniques of introducing immunomodulatory factors have the possibility to improve the targeted delivery of these agents and reduce any unintended effects caused by poor specificity (Blanco et al. 2015).
Despite the significance of miR-155 in the management of GI tumor, some obstacles exist that need to be addressed, similar to those encountered in the therapeutic use of other genetic substances. These include preserving their stability, ensuring proper release, facilitating cellular absorption, and managing potential toxicity. This highlights the necessity for a suitable method of administering miR-155. Liyanage and colleagues utilized chitosan nanoparticles to encapsulate and administer mimics of dre-miR-155. Li et al. successfully achieved an impressive 98.80% encapsulation efficiency with their creation of polymerized dopamine and AS1411 aptamer-modified mesoporous silica nanoparticles loaded with anti-miR-155 (MSNs-anti-miR-155@PDA-Apt). This innovative development was specifically designed for effectively treating colorectal cancer. The findings from their work proved that the combination of MSNs-anti-miR-155@PDA-Apt was highly effective in suppressing the miR-155 in SW480 cells. This approach also demonstrated a remarkable ability to precisely target the cells and deliver improved therapeutic outcomes, as demonstrated through extensive in animal and cell line testing. Moreover, the use of MSNs-anti-miR-155@PDA-Apt effectively blocks miR-155 and ultimately improves the ability of SW480 cells to respond to 5-fluorouracil chemotherapy (Li et al. 2018d).
Conclusion and Future Perspective
The protein miR-155 is an essential player in controlling immunoediting activity through various means, impacting both cancerous and immune cells. It facilitates the communication between these cells and has a significant impact on the severity of the illness and its reaction to therapy. The traits possessed by miR-155 have the potential to be used as a focus in the realm of cancer detection, prediction, and therapy. This analysis revealed the positive prospects of miR-155 in treating gastrointestinal cancer. As we gain a deeper comprehension of miR-155's roles in tumor and immune cells, coupled with the ability to precisely target it through emerging technologies, it has the potential to emerge as a significant molecule in immune checkpoint research. Therefore, in the near future, its focus could potentially be integrated into innovative cancer treatment algorithms.
Because the prognosis for patients diagnosed too late is consistently poor, better techniques for the detection of digestive system cancers at primary stages are required. The biggest obstacles to treating GI cancer are drug resistance, metastasis, and late diagnosis. Consequently, the identification of more precise and advanced safe biomarkers will aid in the early detection and management of these patients. Because they control cell division, involvement of other organs by cancer cells, and migration, miRNAs are significant players in a range of cancer types. MiRNAs could be used for assessing tumor growth at their primary stages and even their metastasis. Several labs are creating clinical assays for miRNAs, which may be used extensively in the future, high stability of miRNAs structures in body fluids and their footsteps have been identified in extracellular vesicles. Many investigations into the function of miRNA-155 in various gastrointestinal cancers have showed its aberrant expression in different tumors. More than being a possible biomarker for the identification of these cancers, miRNA-155 may also be involved in therapeutic strategies. In contrast to other miRNAs, miR-155 regulates the behavior of M2 macrophages that enhance tumor growth and has a pivotal role in trigger of response against cancer. The development of appropriate drug delivery mechanisms for nucleic acid-based therapeutics is one of the numerous obstacles in the field of using miRNAs in cancer treatment. In order for particular miRNAs to serve as diagnostic markers for patients with GI tumor and to determine whether they can be employed in therapeutic strategies for digestive tract cancers further studies is required to refine the techniques for locating and measuring these miRNAs in different body liquids such as CSF and blood.
Extensive research in the area of cancer has consistently demonstrated that miR-155 functions in promoting the growth and enlargement of tumors Due to its high levels in various gastrointestinal cancers and contribution to the development and existence of cancer stem cells, which is a known predictor of negative outcomes, and its ability to enhance resistance to traditional cancer treatments, the deliberate reduction of miR-155 was initially seen as a convenient method for therapy. Even though miR-155 has major involvement in regulating the immune system and functions in the body's defense against tumors by influencing various types of immune cells, we must rethink the use of its regulatory capabilities for treating cancer. This is especially important when considering the use of new therapeutic approches. The algorithms must be based on more than just the seriousness of the illness, which includes the categorization and evaluation of tumors, but also on the immune patterns caused by the disease or its therapy. It is expected that these algorithms will need to specifically target miR-155 in particular cell types, specifically those involved in the immune system. One potential approach for precise targeting could involve utilizing cutting-edge techniques, such as nanovectors or adoptive cellular immunotherapy. In this method, specific types of immune cells could be created outside the body and then altered to effectively target a desired area. Targeting miR-155 in different ways has the potential to significantly boost the body's response to tumor cells and improve the effectiveness of malignancy treatment.
Furthermore, the absence of explicit regulations and protocols for ensuring quality and safety has hindered the progress of miR-155 in its journey towards successful application in clinical settings. Due to the rising quantity of newly developed polymeric nanomaterials, elaborate polymeric-based nanoformulations, and chemical alterations, it is imperative to establish regulatory guidelines to assist in evaluating miRNA drugs. These guidelines should cover areas such as good manufacturing practices, production procedures, and quality controls. Simplifying formulation design can play a crucial role in the assessment conducted by regulatory authorities. However, there is another factor that presents a challenge to the practical application of miR-155-based treatments in medicine—the cost–benefit ratio. This is because the expenses associated with both miRNA biological products and new nanocarriers are significantly higher compared to traditional anti-cancer treatments, making it a less viable option.
To conclude, it is vital to validate the findings of miRNA summarizing research works in separate samples as the diversity of gastric cancer samples and varying miRNA expression levels in different stages of the disease can impact the accuracy and relevance of these results. This confirmation is crucial in determining the dysregulation of miRNAs in different contexts within gastric cancer. More studies are necessary to thoroughly analyze the effects of dysfunctional miR-155 in a broader population of patients with varying backgrounds, to evaluate its probable utility as a diagnostic item for this particular type of cancer. In addition, due to the varied levels of miRNA in gastric malignancy, there is a need for the development of panels consisting of multiple miRNAs for diagnostic or prognostic purposes. This is because relying on the expression of a specific miRNA is unlikely to accurately assess the diagnosis or prognosis of all patients.
Data availability
No datasets were generated or analysed during the current study.
References
Agah S, Alizadeh AM, Mosavi M, Ranji P, Khavari-Daneshvar H, Ghasemian F, et al. More protection of lactobacillus acidophilus than bifidobacterium bifidum probiotics on azoxymethane-induced mouse colon cancer. Probiot Antimicrob Proteins. 2019;11(3):857–64.
Ahmed SA, Parama D, Daimari E, Girisa S, Banik K, Harsha C, et al. Rationalizing the therapeutic potential of apigenin against cancer. Life Sci. 2021;267:118814.
Al-Haidari AA, Syk I, Thorlacius H. MiR-155-5p positively regulates CCL17-induced colon cancer cell migration by targeting RhoA. Oncotarget. 2017;8(9):14887–96.
Al-Haidari A, Algaber A, Madhi R, Syk I, Thorlacius H. MiR-155-5p controls colon cancer cell migration via post-transcriptional regulation of Human Antigen R (HuR). Cancer Lett. 2018;421:145–51.
Ali S, Dubaybo H, Brand RE, Sarkar FH. Differential expression of MicroRNAs in tissues and plasma co-exists as a biomarker for pancreatic cancer. J Cancer Sci Ther. 2015;7(11):336–46.
Alumkal JJ, Slottke R, Schwartzman J, Cherala G, Munar M, Graff JN, et al. A phase II study of sulforaphane-rich broccoli sprout extracts in men with recurrent prostate cancer. Invest New Drugs. 2015;33(2):480–9.
Amundadottir L, Kraft P, Stolzenberg-Solomon RZ, Fuchs CS, Petersen GM, Arslan AA, et al. Genome-wide association study identifies variants in the ABO locus associated with susceptibility to pancreatic cancer. Nat Genet. 2009;41(9):986–90.
Anderson KJ, Cormier RT, Scott PM. Role of ion channels in gastrointestinal cancer. World J Gastroenterol. 2019;25(38):5732–72.
Anees FF, Preethi KA, Selvakumar SC, Murthykumar K, Ganapathy D, Sekar D. Prospective study: expression levels of microRNA-7-3p and its target STAT3 in head and neck cancer. Minerva Dent Oral Sci. 2023;72(6):326–31.
Angulo P, Kaushik G, Subramaniam D, Dandawate P, Neville K, Chastain K, et al. Natural compounds targeting major cell signaling pathways: a novel paradigm for osteosarcoma therapy. J Hematol Oncol. 2017;10(1):10.
Arneth B. Update on the types and usage of liquid biopsies in the clinical setting: a systematic review. BMC Cancer. 2018;18(1):527.
Arroyo JD, Chevillet JR, Kroh EM, Ruf IK, Pritchard CC, Gibson DF, et al. Argonaute2 complexes carry a population of circulating microRNAs independent of vesicles in human plasma. Proc Natl Acad Sci U S A. 2011;108(12):5003–8.
Ashihara E, Takada T, Maekawa T. Targeting the canonical Wnt/β-catenin pathway in hematological malignancies. Cancer Sci. 2015;106(6):665–71.
Ashrafizadeh M, Bakhoda MR, Bahmanpour Z, Ilkhani K, Zarrabi A, Makvandi P, et al. Apigenin as Tumor Suppressor in Cancers: Biotherapeutic Activity, Nanodelivery, and Mechanisms With Emphasis on Pancreatic Cancer. Front Chem. 2020;8:829.
Bakirtzi K, Hatziapostolou M, Karagiannides I, Polytarchou C, Jaeger S, Iliopoulos D, et al. Neurotensin signaling activates microRNAs-21 and -155 and Akt, promotes tumor growth in mice, and is increased in human colon tumors. Gastroenterology. 2011;141(5):1749-61.e1.
Baradaran B, Shahbazi R, Khordadmehr M. Dysregulation of key microRNAs in pancreatic cancer development. Biomed Pharmacother = Biomed Pharmacother. 2019;109:1008–15.
Barcellos-de-Souza P, Comito G, Pons-Segura C, Taddei ML, Gori V, Becherucci V, et al. Mesenchymal stem cells are recruited and activated into carcinoma-associated fibroblasts by prostate cancer microenvironment-derived TGF-β1. Stem Cells (Dayton, Ohio). 2016;34(10):2536–47.
Bartel DP. MicroRNAs: target recognition and regulatory functions. Cell. 2009;136(2):215–33.
Bayraktar R, Pichler M, Kanlikilicer P, Ivan C, Bayraktar E, Kahraman N, et al. MicroRNA 603 acts as a tumor suppressor and inhibits triple-negative breast cancer tumorigenesis by targeting elongation factor 2 kinase. Oncotarget. 2017;8(7):11641–58.
Bentwich I, Avniel A, Karov Y, Aharonov R, Gilad S, Barad O, et al. Identification of hundreds of conserved and nonconserved human microRNAs. Nat Genet. 2005;37(7):766–70.
Bera A, VenkataSubbaRao K, Manoharan MS, Hill P, Freeman JW. A miRNA signature of chemoresistant mesenchymal phenotype identifies novel molecular targets associated with advanced pancreatic cancer. PLoS ONE. 2014;9(9):e106343.
Blackford A, Parmigiani G, Kensler TW, Wolfgang C, Jones S, Zhang X, et al. Genetic mutations associated with cigarette smoking in pancreatic cancer. Can Res. 2009;69(8):3681–8.
Blanco E, Shen H, Ferrari M. Principles of nanoparticle design for overcoming biological barriers to drug delivery. Nat Biotechnol. 2015;33(9):941–51.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Burnett JP, Lim G, Li Y, Shah RB, Lim R, Paholak HJ, et al. Sulforaphane enhances the anticancer activity of taxanes against triple negative breast cancer by killing cancer stem cells. Cancer Lett. 2017;394:52–64.
Cai X, Yin Y, Li N, Zhu D, Zhang J, Zhang CY, et al. Re-polarization of tumor-associated macrophages to pro-inflammatory M1 macrophages by microRNA-155. J Mol Cell Biol. 2012;4(5):341–3.
Calin GA, Dumitru CD, Shimizu M, Bichi R, Zupo S, Noch E, et al. Frequent deletions and down-regulation of micro- RNA genes miR15 and miR16 at 13q14 in chronic lymphocytic leukemia. Proc Natl Acad Sci U S A. 2002;99(24):15524–9.
Cancer incidence in five continents. Volume VIII. IARC Sci Publ. 2002(155):1-781.
Cao H, Xu W, Qian H, Zhu W, Yan Y, Zhou H, et al. Mesenchymal stem cell-like cells derived from human gastric cancer tissues. Cancer Lett. 2009;274(1):61–71.
Cao H, Huang S, Liu A, Chen Z. Up-regulated expression of miR-155 in human colonic cancer. J Cancer Res Ther. 2018;14(3):604–7.
Challagundla KB, Wise PM, Neviani P, Chava H, Murtadha M, Xu T, et al. Exosome-mediated transfer of microRNAs within the tumor microenvironment and neuroblastoma resistance to chemotherapy. J Natl Cancer Inst. 2015;107(7):djv135.
Chen R, Pan S, Brentnall TA, Aebersold R. Proteomic profiling of pancreatic cancer for biomarker discovery. Mol Cell Proteomics : MCP. 2005;4(4):523–33.
Chen J, Liu X, Chen X, Guo Z, Liu J, Hao J, et al. Real-time monitoring of miRNA function in pancreatic cell lines using recombinant AAV-based miRNA Asensors. PLoS ONE. 2013;8(6):e66315.
Chen J, Wang W, Zhang Y, Chen Y, Hu T. Predicting distant metastasis and chemoresistance using plasma miRNAs. Med Oncol. 2014;31(1):799.
Chen M, Wang X, Zha D, Cai F, Zhang W, He Y, et al. Apigenin potentiates TRAIL therapy of non-small cell lung cancer via upregulating DR4/DR5 expression in a p53-dependent manner. Sci Rep. 2016;6:35468.
Chen ZL, Li XN, Ye CX, Chen HY, Wang ZJ. Elevated Levels of circRUNX1 in Colorectal Cancer Promote Cell Growth and Metastasis via miR-145-5p/IGF1 Signalling. Onco Targets Ther. 2020;13:4035–48.
Cheng YF, Chen HS, Wu SC, Chen HC, Hung WH, Lin CH, et al. Esophageal squamous cell carcinoma and prognosis in Taiwan. Cancer Med. 2018;7(9):4193–201.
Chew LJ, Gallo V. The Yin and Yang of Sox proteins: Activation and repression in development and disease. J Neurosci Res. 2009;87(15):3277–87.
Cholewinski G, Garczorz W, Francuz T, Owczarek AJ, Kimsa-Furdzik M, Blaszczynska M, et al. Expression of let-7a, miR-106b and miR-29b is changed in human gastric cancer. J Physiol Pharmacol. 2022;73(1). https://doi.org/10.26402/jpp.2022.1.03
Coleman MP, Gatta G, Verdecchia A, Estève J, Sant M, Storm H, et al. EUROCARE-3 summary: cancer survival in Europe at the end of the 20th century. Ann Oncol: Off J Eur Soc Med Oncol. 2003;14(Suppl 5):v128–49.
Corso G, Marrelli D, Roviello F. Familial gastric cancer: update for practice management. Fam Cancer. 2011;10(2):391–6.
Cote GA, Gore AJ, McElyea SD, Heathers LE, Xu H, Sherman S, et al. A pilot study to develop a diagnostic test for pancreatic ductal adenocarcinoma based on differential expression of select miRNA in plasma and bile. Am J Gastroenterol. 2014;109(12):1942–52.
de la Chapelle A. Genetic predisposition to colorectal cancer. Nat Rev Cancer. 2004;4(10):769–80.
Donnem T, Fenton CG, Lonvik K, Berg T, Eklo K, Andersen S, et al. MicroRNA signatures in tumor tissue related to angiogenesis in non-small cell lung cancer. PLoS ONE. 2012;7(1):e29671.
Dunand-Sauthier I, Santiago-Raber ML, Capponi L, Vejnar CE, Schaad O, Irla M, et al. Silencing of c-Fos expression by microRNA-155 is critical for dendritic cell maturation and function. Blood. 2011;117(17):4490–500.
El-Daly SM, Omara EA, Hussein J, Youness ER, El-Khayat Z. Differential expression of miRNAs regulating NF-κB and STAT3 crosstalk during colitis-associated tumorigenesis. Mol Cell Probes. 2019;47:101442.
Elton TS, Selemon H, Elton SM, Parinandi NL. Regulation of the MIR155 host gene in physiological and pathological processes. Gene. 2013;532(1):1–12.
Emam AA, Abo-Elkhair SM, Sobh M, El-Sokkary AMA. Role of exopolysaccharides (EPSs) as anti-Mir-155 in cancer cells. Heliyon. 2021;7(4):e06698.
Eshraghi R, Rafiei M, Hadian Jazi Z, Shafie D, Raisi A, Mirzaei H. MicroRNA-155 and exosomal microRNA-155: Small pieces in the cardiovascular diseases puzzle. Pathol – Res Pract. 2024;257:155274.
Fang H, Shuang D, Yi Z, Sheng H, Liu Y. Up-regulated microRNA-155 expression is associated with poor prognosis in cervical cancer patients. Biomed Pharmacother = Biomed Pharmacother. 2016;83:64–9.
Fassi Fehri L, Koch M, Belogolova E, Khalil H, Bolz C, Kalali B, et al. Helicobacter pylori induces miR-155 in T cells in a cAMP-Foxp3-dependent manner. PLoS ONE. 2010;5(3):e9500.
Ferlay J. Cancer incidence, mortality and prevalence worldwide. GLOBOCAN2002. IARC Press; 2004.
Fojo T. Multiple paths to a drug resistance phenotype: mutations, translocations, deletions and amplification of coding genes or promoter regions, epigenetic changes and microRNAs. Drug Resist Updat. 2007;10(1–2):59–67.
Gallo A, Tandon M, Alevizos I, Illei GG. The majority of microRNAs detectable in serum and saliva is concentrated in exosomes. PLoS ONE. 2012;7(3):e30679.
Gao Y, Liu Z, Ding Z, Hou S, Li J, Jiang K. MicroRNA-155 increases colon cancer chemoresistance to cisplatin by targeting forkhead box O3. Oncol Lett. 2018;15(4):4781–8.
Ghansah T. A novel strategy for modulation of MDSC to enhance cancer immunotherapy. Oncoimmunology. 2012;1(6):984–5.
Ghansah T, Paraiso KH, Highfill S, Desponts C, May S, McIntosh JK, et al. Expansion of myeloid suppressor cells in SHIP-deficient mice represses allogeneic T cell responses. J Immunol (Baltimore, Md: 1950). 2004;173(12):7324–30.
Girolimetti G, Pelisenco IA, Eusebi LH, Ricci C, Cavina B, Kurelac I, et al. Dysregulation of a Subset of Circulating and Vesicle-Associated miRNA in Pancreatic Cancer. Noncoding RNA. 2024;10(3):29.
Gironella M, Seux M, Xie MJ, Cano C, Tomasini R, Gommeaux J, et al. Tumor protein 53-induced nuclear protein 1 expression is repressed by miR-155, and its restoration inhibits pancreatic tumor development. Proc Natl Acad Sci U S A. 2007;104(41):16170–5.
Grajek W, Olejnik A, Sip A. Probiotics, prebiotics and antioxidants as functional foods. Acta Biochim Pol. 2005;52(3):665–71.
Greco SJ, Rameshwar P. Mesenchymal stem cells in drug/gene delivery: implications for cell therapy. Ther Deliv. 2012;3(8):997–1004.
Greither T, Grochola LF, Udelnow A, Lautenschläger C, Würl P, Taubert H. Elevated expression of microRNAs 155, 203, 210 and 222 in pancreatic tumors is associated with poorer survival. Int J Cancer. 2010;126(1):73–80.
Gross JC, Chaudhary V, Bartscherer K, Boutros M. Active Wnt proteins are secreted on exosomes. Nat Cell Biol. 2012;14(10):1036–45.
Guan Z, Zhang J, Wang J, Wang H, Zheng F, Peng J, et al. SOX1 down-regulates β-catenin and reverses malignant phenotype in nasopharyngeal carcinoma. Mol Cancer. 2014;13:257.
Gubbay J, Collignon J, Koopman P, Capel B, Economou A, Münsterberg A, et al. A gene mapping to the sex-determining region of the mouse Y chromosome is a member of a novel family of embryonically expressed genes. Nature. 1990;346(6281):245–50.
Ha M, Kim VN. Regulation of microRNA biogenesis. Nat Rev Mol Cell Biol. 2014;15(8):509–24.
Habbe N, Koorstra JB, Mendell JT, Offerhaus GJ, Ryu JK, Feldmann G, et al. MicroRNA miR-155 is a biomarker of early pancreatic neoplasia. Cancer Biol Ther. 2009;8(4):340–6.
Haga H, Yan IK, Takahashi K, Wood J, Zubair A, Patel T. Tumour cell-derived extracellular vesicles interact with mesenchymal stem cells to modulate the microenvironment and enhance cholangiocarcinoma growth. J Extracellular Vesicles. 2015;4:24900.
Hamashima C, Ogoshi K, Okamoto M, Shabana M, Kishimoto T, Fukao A. A community-based, case-control study evaluating mortality reduction from gastric cancer by endoscopic screening in Japan. PLoS ONE. 2013;8(11):e79088.
Hamilton MJ, Ho VW, Kuroda E, Ruschmann J, Antignano F, Lam V, et al. Role of SHIP in cancer. Exp Hematol. 2011;39(1):2–13.
Han PP, Sun Y, Wu XY, Yuan YJ, Dai YJ, Jia SR. Emulsifying, flocculating, and physicochemical properties of exopolysaccharide produced by cyanobacterium Nostoc flagelliforme. Appl Biochem Biotechnol. 2014;172(1):36–49.
Han S, Yang S, Cai Z, Pan D, Li Z, Huang Z, et al. Anti-Warburg effect of rosmarinic acid via miR-155 in gastric cancer cells. Drug Des Devel Ther. 2015;9:2695–703.
Hansen TB, Jensen TI, Clausen BH, Bramsen JB, Finsen B, Damgaard CK, et al. Natural RNA circles function as efficient microRNA sponges. Nature. 2013;495(7441):384–8.
Hata K, Watanabe T, Kawamura YJ, Ishigami H. CASE REPORT: K-ras mutation and loss of heterozygosity at 17p with [beta]-catenin accumulation in intramucosal carcinoma of the ileostomy in familial adenomatous polyposis: a case report. Dig Dis Sci. 2003;48(12):2310.
Haviv I, Polyak K, Qiu W, Hu M, Campbell I. Origin of carcinoma associated fibroblasts. Cell Cycle (Georgetown, Tex). 2009;8(4):589–95.
He YQ, Sheng JQ, Ling XL, Fu L, Jin P, Yen L, et al. Estradiol regulates miR-135b and mismatch repair gene expressions via estrogen receptor-β in colorectal cells. Exp Mol Med. 2012;44(12):723–32.
He B, Gao SQ, Huang LD, Huang YH, Zhang QY, Zhou MT, et al. MicroRNA-155 promotes the proliferation and invasion abilities of colon cancer cells by targeting quaking. Mol Med Rep. 2015;11(3):2355–9.
He Y, Wang Y, Liu L, Liu S, Liang L, Chen Y, et al. Circular RNA circ_0006282 contributes to the progression of gastric cancer by sponging miR-155 to upregulate the expression of FBXO22. Onco Targets Ther. 2020;13:1001–10.
Herr I, Lozanovski V, Houben P, Schemmer P, Büchler MW. Sulforaphane and related mustard oils in focus of cancer prevention and therapy. Wiener medizinische Wochenschrift (1946). 2013;163(3–4):80–8.
Heydari Z, Rahaie M, Alizadeh AM, Agah S, Khalighfard S, Bahmani S. Effects of lactobacillus acidophilus and bifidobacterium bifidum probiotics on the expression of MicroRNAs 135b, 26b, 18a and 155, and their involving genes in mice colon cancer. Probiotics Antimicrob Proteins. 2019;11(4):1155–62.
Hibbs ML, Raftery AL, Tsantikos E. Regulation of hematopoietic cell signaling by SHIP-1 inositol phosphatase: growth factors and beyond. Growth Factors (Chur, Switzerland). 2018;36(5–6):213–31.
Hongliang C, Shaojun H, Aihua L, Hua J. Correlation between expression of miR-155 in colon cancer and serum carcinoembryonic antigen level and its contribution to recurrence and metastasis forecast. Saudi Med J. 2014;35(6):547–53.
Hooi JKY, Lai WY, Ng WK, Suen MMY, Underwood FE, Tanyingoh D, et al. Global prevalence of helicobacter pylori infection: systematic review and meta-analysis. Gastroenterology. 2017;153(2):420–9.
Hotel ACP, Cordoba A. Health and nutritional properties of probiotics in food including powder milk with live lactic acid bacteria. Prevention. 2001;5(1):1–10.
Hu M, Yao J, Cai L, Bachman KE, van den Brûle F, Velculescu V, et al. Distinct epigenetic changes in the stromal cells of breast cancers. Nat Genet. 2005;37(8):899–905.
Hu Z, Chen X, Zhao Y, Tian T, Jin G, Shu Y, et al. Serum microRNA signatures identified in a genome-wide serum microRNA expression profiling predict survival of non-small-cell lung cancer. J Clin Oncol: Off J Am Soc Clin Oncol. 2010;28(10):1721–6.
Hu G, Drescher KM, Chen X. Exosomal miRNAs: biological properties and therapeutic potential. Front Genet. 2012;3:56.
Huang C, Li H, Wu W, Jiang T, Qiu Z. Regulation of miR-155 affects pancreatic cancer cell invasiveness and migration by modulating the STAT3 signaling pathway through SOCS1. Oncol Rep. 2013;30(3):1223–30.
Husain K, Villalobos-Ayala K, Laverde V, Vazquez OA, Miller B, Kazim S, et al. Apigenin targets MicroRNA-155, enhances SHIP-1 expression, and augments anti-tumor responses in pancreatic cancer. Cancers (Basel). 2022;14(15):3613.
Iannitti T, Palmieri B. Therapeutical use of probiotic formulations in clinical practice. Clin Nutr (Edinburgh, Scotland). 2010;29(6):701–25.
Jang JY, Sung B, Kim ND. Role of induced programmed cell death in the chemopreventive potential of apigenin. Int J Mol Sci. 2022;23(7):3757.
Jeck WR, Sorrentino JA, Wang K, Slevin MK, Burd CE, Liu J, et al. Circular RNAs are abundant, conserved, and associated with ALU repeats. RNA. 2013;19(2):141–57.
Ji H, Kim TW, Lee WJ, Jeong SD, Cho YB, Kim HH. Two circPPFIA1s negatively regulate liver metastasis of colon cancer via miR-155-5p/CDX1 and HuR/RAB36. Mol Cancer. 2022;21(1):197.
Jiang X, Zhou T, Xiao Y, Yu J, Dou S, Chen G, et al. Tim-3 promotes tumor-promoting M2 macrophage polarization by binding to STAT1 and suppressing the STAT1-miR-155 signaling axis. Oncoimmunology. 2016;5(9):e1211219.
Johnson JL, Gonzalez de Mejia E. Interactions between dietary flavonoids apigenin or luteolin and chemotherapeutic drugs to potentiate anti-proliferative effect on human pancreatic cancer cells, in vitro. Food Chem Toxicol Int J Publ Br Ind Biol Res Assoc. 2013;60:83–91.
Jolma A, Zhang J, Mondragón E, Morgunova E, Kivioja T, Laverty KU, et al. Binding specificities of human RNA-binding proteins toward structured and linear RNA sequences. Genome Res. 2020;30(7):962–73.
Jun JK, Choi KS, Lee HY, Suh M, Park B, Song SH, et al. Effectiveness of the korean national cancer screening program in reducing gastric cancer mortality. Gastroenterology. 2017;152(6):1319-28.e7.
Jung Y, Kim JK, Shiozawa Y, Wang J, Mishra A, Joseph J, et al. Recruitment of mesenchymal stem cells into prostate tumours promotes metastasis. Nat Commun. 2013;4:1795.
Jung J, Yeom C, Choi YS, Kim S, Lee E, Park MJ, et al. Simultaneous inhibition of multiple oncogenic miRNAs by a multi-potent microRNA sponge. Oncotarget. 2015;6(24):20370–87.
Kalesnikoff J, Sly LM, Hughes MR, Büchse T, Rauh MJ, Cao LP, et al. The role of SHIP in cytokine-induced signaling. Rev Physiol Biochem Pharmacol. 2003;149:87–103.
Kalkusova K, Taborska P, Stakheev D, Smrz D. The Role of miR-155 in Antitumor Immunity. Cancers (Basel). 2022;14(21):5414.
Kallifatidis G, Rausch V, Baumann B, Apel A, Beckermann BM, Groth A, et al. Sulforaphane targets pancreatic tumour-initiating cells by NF-kappaB-induced antiapoptotic signalling. Gut. 2009;58(7):949–63.
Kallifatidis G, Labsch S, Rausch V, Mattern J, Gladkich J, Moldenhauer G, et al. Sulforaphane increases drug-mediated cytotoxicity toward cancer stem-like cells of pancreas and prostate. Mol Ther : J Am Soc Gene Ther. 2011;19(1):188–95.
Kanlikilicer P, Rashed MH, Bayraktar R, Mitra R, Ivan C, Aslan B, et al. Ubiquitous release of exosomal tumor suppressor miR-6126 from ovarian cancer cells. Can Res. 2016;76(24):7194–207.
Kapral M, Wawszczyk J, Węglarz L. Regulation of MicroRNA-155 and its related genes expression by inositol hexaphosphate in colon cancer cells. Molecules. 2019;24(22):4153.
Karimi M, Mohammadnia A, Amini MA, Shamekh AG, Derakhshanfar E, Hosseini F. Overexpression of miR-146a and miR-155 are Potentially Biomarkers and Predict Unfavorable Relationship between Gastric Cancer and Helicobacter pylori Infection. Chonnam Med J. 2023;59(3):167–73.
Katsanos KH, Kitsanou M, Christodoulou DK, Tsianos EV. High CA 19–9 levels in benign biliary tract diseases. Report of four cases and review of the literature. Eur J Int Med. 2002;13(2):132–5.
Khavari-Daneshvar H, Mosavi M, Khodayari H, Rahimi E, Ranji P, Mohseni AH, et al. Modifications of mice gut microflora following oral consumption ofLactobacillus acidophilus and Bifidobacterium bifidum probiotics. Turk J Med Sci. 2017;47(2):689–94.
Khoury S, Tran N. Circulating microRNAs: potential biomarkers for common malignancies. Biomark Med. 2015;9(2):131–51.
Kidd S, Spaeth E, Dembinski JL, Dietrich M, Watson K, Klopp A, et al. Direct evidence of mesenchymal stem cell tropism for tumor and wounding microenvironments using in vivo bioluminescent imaging. Stem Cells (Dayton, Ohio). 2009;27(10):2614–23.
Kim H, Hwang Y, Sung H, Jang J, Ahn C, Kim SG, et al. Effectiveness of gastric cancer screening on gastric cancer incidence and mortality in a community-based prospective cohort. Cancer Res Treat. 2018;50(2):582–9.
Kim MW, Koh H, Kim JY, Lee S, Lee H, Kim Y, et al. Tumor-Specific miRNA signatures in combination with CA19–9 for liquid biopsy-based detection of PDAC. Int J Mol Sci. 2021;22(24):13621.
Kirave P, Gondaliya P, Kulkarni B, Rawal R, Garg R, Jain A, et al. Exosome mediated miR-155 delivery confers cisplatin chemoresistance in oral cancer cells via epithelial-mesenchymal transition. Oncotarget. 2020;11(13):1157–71.
Kishikawa T, Otsuka M, Tan PS, Ohno M, Sun X, Yoshikawa T, et al. Decreased miR122 in hepatocellular carcinoma leads to chemoresistance with increased arginine. Oncotarget. 2015;6(10):8339–52.
Klein AP, Brune KA, Petersen GM, Goggins M, Tersmette AC, Offerhaus GJ, et al. Prospective risk of pancreatic cancer in familial pancreatic cancer kindreds. Can Res. 2004;64(7):2634–8.
Klopp AH, Spaeth EL, Dembinski JL, Woodward WA, Munshi A, Meyn RE, et al. Tumor irradiation increases the recruitment of circulating mesenchymal stem cells into the tumor microenvironment. Can Res. 2007;67(24):11687–95.
Kogure T, Lin WL, Yan IK, Braconi C, Patel T. Intercellular nanovesicle-mediated microRNA transfer: a mechanism of environmental modulation of hepatocellular cancer cell growth. Hepatology (Baltimore, MD). 2011;54(4):1237–48.
Kong W, He L, Richards EJ, Challa S, Xu CX, Permuth-Wey J, et al. Upregulation of miRNA-155 promotes tumour angiogenesis by targeting VHL and is associated with poor prognosis and triple-negative breast cancer. Oncogene. 2014;33(6):679–89.
Kreuzer-Redmer S, Bekurtz JC, Arends D, Bortfeldt R, Kutz-Lohroff B, Sharbati S, et al. Feeding of Enterococcus faecium NCIMB 10415 Leads to Intestinal miRNA-423-5p-Induced Regulation of Immune-Relevant Genes. Appl Environ Microbiol. 2016;82(8):2263–9.
La X, Zhang L, Li Z, Li H, Yang Y. (-)-Epigallocatechin gallate (EGCG) enhances the sensitivity of colorectal cancer cells to 5-FU by inhibiting GRP78/NF-κB/miR-155-5p/MDR1 pathway. J Agric Food Chem. 2019;67(9):2510–8.
LaConti JJ, Shivapurkar N, Preet A, Deslattes Mays A, Peran I, Kim SE, et al. Tissue and serum microRNAs in the Kras(G12D) transgenic animal model and in patients with pancreatic cancer. PLoS ONE. 2011;6(6):e20687.
Lan J, Sun L, Xu F, Liu L, Hu F, Song D, et al. M2 macrophage-derived exosomes promote cell migration and invasion in colon cancer. Can Res. 2019;79(1):146–58.
Lee EJ, Gusev Y, Jiang J, Nuovo GJ, Lerner MR, Frankel WL, et al. Expression profiling identifies microRNA signature in pancreatic cancer. Int J Cancer. 2007;120(5):1046–54.
Lee Y, Sung B, Kang YJ, Kim DH, Jang JY, Hwang SY, et al. Apigenin-induced apoptosis is enhanced by inhibition of autophagy formation in HCT116 human colon cancer cells. Int J Oncol. 2014;44(5):1599–606.
Lee SWL, Paoletti C, Campisi M, Osaki T, Adriani G, Kamm RD, et al. MicroRNA delivery through nanoparticles. J Control Release. 2019;313:80–95.
Lee J, Lee HS, Park SB, Kim C, Kim K, Jung DE, et al. Identification of Circulating Serum miRNAs as Novel Biomarkers in Pancreatic Cancer Using a Penalized Algorithm. Int J Mol Sci. 2021;22(3):1007.
Li D, Yeung SC, Hassan MM, Konopleva M, Abbruzzese JL. Antidiabetic therapies affect risk of pancreatic cancer. Gastroenterology. 2009;137(2):482–8.
Li Y, Zhang T, Korkaya H, Liu S, Lee HF, Newman B, et al. Sulforaphane, a dietary component of broccoli/broccoli sprouts, inhibits breast cancer stem cells. Clin Cancer Res. 2010;16(9):2580–90.
Li CL, Nie H, Wang M, Su LP, Li JF, Yu YY, et al. microRNA-155 is downregulated in gastric cancer cells and involved in cell metastasis. Oncol Rep. 2012;27(6):1960–6.
Li H, Xie S, Liu M, Chen Z, Liu X, Wang L, et al. The clinical significance of downregulation of mir-124-3p, mir-146a-5p, mir-155-5p and mir-335-5p in gastric cancer tumorigenesis. Int J Oncol. 2014;45(1):197–208.
Li Y, Zheng Q, Bao C, Li S, Guo W, Zhao J, et al. Circular RNA is enriched and stable in exosomes: a promising biomarker for cancer diagnosis. Cell Res. 2015a;25(8):981–4.
Li W, Tang W, Ji J, Xia X, Rui X, Chen X, et al. Characterization of a novel polysaccharide with anti-colon cancer activity from Lactobacillus helveticus MB2-1. Carbohyd Res. 2015b;411:6–14.
Li X, Wang J, Zhang C, Lin C, Zhang J, Zhang W, et al. Circular RNA circITGA7 inhibits colorectal cancer growth and metastasis by modulating the Ras pathway and upregulating transcription of its host gene ITGA7. J Pathol. 2018a;246(2):166–79.
Li S, Zhang T, Zhou X, Du Z, Chen F, Luo J, et al. The tumor suppressor role of miR-155-5p in gastric cancer. Oncol Lett. 2018b;16(2):2709–14.
Li Q, Li B, Li Q, Wei S, He Z, Huang X, et al. Exosomal miR-21-5p derived from gastric cancer promotes peritoneal metastasis via mesothelial-to-mesenchymal transition. Cell Death Dis. 2018c;9(9):854.
Li Y, Duo Y, Bi J, Zeng X, Mei L, Bao S, et al. Targeted delivery of anti-miR-155 by functionalized mesoporous silica nanoparticles for colorectal cancer therapy. Int J Nanomedicine. 2018d;13:1241–56.
Li Y, Tian Z, Tan Y, Lian G, Chen S, Chen S, et al. Bmi-1-induced miR-27a and miR-155 promote tumor metastasis and chemoresistance by targeting RKIP in gastric cancer. Mol Cancer. 2020;19(1):109.
Li Y, Zhang L, Dong Z, Xu H, Yan L, Wang W, et al. MicroRNA-155-5p promotes tumor progression and contributes to paclitaxel resistance via TP53INP1 in human breast cancer. Pathol Res Pract. 2021a;220:153405.
Li Y, Zhang L, Dong Z, Xu H, Yan L, Wang W, et al. MicroRNA-155-5p promotes tumor progression and contributes to paclitaxel resistance via TP53INP1 in human breast cancer. Pathol – Res Pract. 2021b;220:153405.
Liang M, Liu Z, Lin H, Shi B, Li M, Chen T, et al. High-throughput sequencing reveals circular RNA hsa_circ_0000592 as a novel player in the carcinogenesis of gastric carcinoma. Biosci Rep. 2019;39(6):BSR20181900.
Liang M, Huang G, Liu Z, Wang Q, Yu Z, Liu Z, et al. Elevated levels of hsa_circ_006100 in gastric cancer promote cell growth and metastasis via miR-195/GPRC5A signalling. Cell Prolif. 2019;52(5):e12661.
Lin SZ, Xu JB, Ji X, Chen H, Xu HT, Hu P, et al. Emodin inhibits angiogenesis in pancreatic cancer by regulating the transforming growth factor-β/drosophila mothers against decapentaplegic pathway and angiogenesis-associated microRNAs. Mol Med Rep. 2015;12(4):5865–71.
Lin LY, Du LM, Cao K, Huang Y, Yu PF, Zhang LY, et al. Tumour cell-derived exosomes endow mesenchymal stromal cells with tumour-promotion capabilities. Oncogene. 2016;35(46):6038–42.
Ling Q, Fang J, Zhai C, Huang W, Chen Y, Zhou T, et al. Berberine induces SOCS1 pathway to reprogram the M1 polarization of macrophages via miR-155-5p in colitis-associated colorectal cancer. Eur J Pharmacol. 2023;949:175724.
Liu L, Chen Q, Lai R, Wu X, Wu X, Liu F, et al. Elevated expression of mature miR-21 and miR-155 in cancerous gastric tissues from Chinese patients with gastric cancer. J Biomed Res. 2010;24(3):187–97.
Liu J, Gao J, Du Y, Li Z, Ren Y, Gu J, et al. Combination of plasma microRNAs with serum CA19-9 for early detection of pancreatic cancer. Int J Cancer. 2012a;131(3):683–91.
Liu R, Chen X, Du Y, Yao W, Shen L, Wang C, et al. Serum microRNA expression profile as a biomarker in the diagnosis and prognosis of pancreatic cancer. Clin Chem. 2012b;58(3):610–8.
Liu R, Liao J, Yang M, Shi Y, Peng Y, Wang Y, et al. Circulating miR-155 expression in plasma: a potential biomarker for early diagnosis of esophageal cancer in humans. J Toxicol Environ Health A. 2012c;75(18):1154–62.
Liu WJ, Zhao YP, Zhang TP, Zhou L, Cui QC, Zhou WX, et al. MLH1 as a direct target of MiR-155 and a potential predictor of favorable prognosis in pancreatic cancer. J Gastrointest Surg. 2013;17(8):1399–405.
Liu N, Jiang F, Han XY, Li M, Chen WJ, Liu QC, et al. MiRNA-155 promotes the invasion of colorectal cancer SW-480 cells through regulating the Wnt/β-catenin. Eur Rev Med Pharmacol Sci. 2018;22(1):101–9.
Liu Y, Guo G, Zhong Z, Sun L, Liao L, Wang X, et al. Long non-coding RNA FLVCR1-AS1 sponges miR-155 to promote the tumorigenesis of gastric cancer by targeting c-Myc. Am J Transl Res. 2019a;11(2):793–805.
Liu J, Fan L, Yu H, Zhang J, He Y, Feng D, et al. Endoplasmic Reticulum Stress Causes Liver Cancer Cells to Release Exosomal miR-23a-3p and Up-regulate Programmed Death Ligand 1 Expression in Macrophages. Hepatology (Baltimore, MD). 2019b;70(1):241–58.
Lv LL, Cao Y, Liu D, Xu M, Liu H, Tang RN, et al. Isolation and quantification of microRNAs from urinary exosomes/microvesicles for biomarker discovery. Int J Biol Sci. 2013;9(10):1021–31.
Ma Y, Zhang P, Yang J, Liu Z, Yang Z, Qin H. Candidate microRNA biomarkers in human colorectal cancer: systematic review profiling studies and experimental validation. Int J Cancer. 2012;130(9):2077–87.
Ma Z, Ma Y, Xia Q, Li Y, Li R, Chang W, et al. MicroRNA-155 expression inversely correlates with pathologic stage of gastric cancer and it inhibits gastric cancer cell growth by targeting cyclin D1. J Cancer Res Clin Oncol. 2016;142(6):1201–12.
Ma HW, Xi DY, Ma JZ, Guo M, Ma L, Ma DH, et al. Long noncoding RNA AFAP1-AS1 promotes cell proliferation and metastasis via the miR-155-5p/FGF7 axis and predicts poor prognosis in gastric cancer. Dis Markers. 2020;2020:8140989.
Ma YS, Wu TM, Ling CC, Yu F, Zhang J, Cao PS, et al. M2 macrophage-derived exosomal microRNA-155-5p promotes the immune escape of colon cancer by downregulating ZC3H12B. Mol Ther Oncolytics. 2021;20:484–98.
Magee P, Shi L, Garofalo M. Role of microRNAs in chemoresistance. Ann Transl Med. 2015;3(21):332.
Mahesh G, Biswas R. MicroRNA-155: a master regulator of inflammation. J Interferon Cytokine Res. 2019;39(6):321–30.
Mangala LS, Wang H, Jiang D, Wu SY, Somasunderam A, Volk DE, et al. Improving vascular maturation using noncoding RNAs increases antitumor effect of chemotherapy. JCI Insight. 2016;1(17):e87754.
Mann DV, Edwards R, Ho S, Lau WY, Glazer G. Elevated tumour marker CA19-9: clinical interpretation and influence of obstructive jaundice. Eur J Surg Oncol: J Eur Soc Surg Oncol Br Assoc Surg Oncol. 2000;26(5):474–9.
Martinez FO, Sica A, Mantovani A, Locati M. Macrophage activation and polarization. Front Biosci. 2008;13:453–61.
Mathews LA, Hurt EM, Zhang X, Farrar WL. Epigenetic regulation of CpG promoter methylation in invasive prostate cancer cells. Mol Cancer. 2010;9:267.
Mathivanan S, Ji H, Simpson RJ. Exosomes: extracellular organelles important in intercellular communication. J Proteomics. 2010;73(10):1907–20.
Matsumura T, Sugimachi K, Iinuma H, Takahashi Y, Kurashige J, Sawada G, et al. Exosomal microRNA in serum is a novel biomarker of recurrence in human colorectal cancer. Br J Cancer. 2015;113(2):275–81.
McLean K, Gong Y, Choi Y, Deng N, Yang K, Bai S, et al. Human ovarian carcinoma–associated mesenchymal stem cells regulate cancer stem cells and tumorigenesis via altered BMP production. J Clin Investig. 2011;121(8):3206–19.
Melillo JA, Song L, Bhagat G, Blazquez AB, Plumlee CR, Lee C, et al. Dendritic cell (DC)-specific targeting reveals Stat3 as a negative regulator of DC function. J Immunology (Baltimore, Md : 1950). 2010;184(5):2638–45.
Melo SA, Moutinho C, Ropero S, Calin GA, Rossi S, Spizzo R, et al. A genetic defect in exportin-5 traps precursor microRNAs in the nucleus of cancer cells. Cancer Cell. 2010;18(4):303–15.
Memczak S, Jens M, Elefsinioti A, Torti F, Krueger J, Rybak A, et al. Circular RNAs are a large class of animal RNAs with regulatory potency. Nature. 2013;495(7441):333–8.
Michael A, Bajracharya SD, Yuen PS, Zhou H, Star RA, Illei GG, et al. Exosomes from human saliva as a source of microRNA biomarkers. Oral Dis. 2010;16(1):34–8.
Mikamori M, Yamada D, Eguchi H, Hasegawa S, Kishimoto T, Tomimaru Y, et al. MicroRNA-155 controls exosome synthesis and promotes gemcitabine resistance in pancreatic ductal adenocarcinoma. Sci Rep. 2017;7:42339.
Mishra PJ, Mishra PJ, Humeniuk R, Medina DJ, Alexe G, Mesirov JP, et al. Carcinoma-associated fibroblast-like differentiation of human mesenchymal stem cells. Can Res. 2008;68(11):4331–9.
Mitchell PS, Parkin RK, Kroh EM, Fritz BR, Wyman SK, Pogosova-Agadjanyan EL, et al. Circulating microRNAs as stable blood-based markers for cancer detection. Proc Natl Acad Sci U S A. 2008;105(30):10513–8.
Mitra AK, Zillhardt M, Hua Y, Tiwari P, Murmann AE, Peter ME, et al. MicroRNAs reprogram normal fibroblasts into cancer-associated fibroblasts in ovarian cancer. Cancer Discov. 2012;2(12):1100–8.
Mönig S, Chevallay M, Niclauss N, Zilli T, Fang W, Bansal A, et al. Early esophageal cancer: the significance of surgery, endoscopy, and chemoradiation. Ann N Y Acad Sci. 2018;1434(1):115–23.
Monzo M, Santasusagna S, Moreno I, Martinez F, Hernández R, Muñoz C, et al. Exosomal microRNAs isolated from plasma of mesenteric veins linked to liver metastases in resected patients with colon cancer. Oncotarget. 2017;8(19):30859–69.
Moutabian H, Radi UK, Saleman AY, Adil M, Zabibah RS, Chaitanya MNL, et al. MicroRNA-155 and cancer metastasis: Regulation of invasion, migration, and epithelial-to-mesenchymal transition. Pathol – Res Pract. 2023;250:154789.
Munson PB, Hall EM, Farina NH, Pass HI, Shukla A. Exosomal miR-16-5p as a target for malignant mesothelioma. Sci Rep. 2019;9(1):11688.
Murugaiyan G, Beynon V, Mittal A, Joller N, Weiner HL. Silencing microRNA-155 ameliorates experimental autoimmune encephalomyelitis. J Immunol (Baltimore, Md : 1950). 2011;187(5):2213–21.
Mycko MP, Cichalewska M, Machlanska A, Cwiklinska H, Mariasiewicz M, Selmaj KW. MicroRNA-301a regulation of a T-helper 17 immune response controls autoimmune demyelination. Proc Natl Acad Sci U S A. 2012;109(20):E1248–57.
Nelson N, Szekeres K, Iclozan C, Rivera IO, McGill A, Johnson G, et al. Apigenin: Selective CK2 inhibitor increases Ikaros expression and improves T cell homeostasis and function in murine pancreatic cancer. PLoS ONE. 2017;12(2):e0170197.
Nillesen ST, Geutjes PJ, Wismans R, Schalkwijk J, Daamen WF, van Kuppevelt TH. Increased angiogenesis and blood vessel maturation in acellular collagen-heparin scaffolds containing both FGF2 and VEGF. Biomaterials. 2007;28(6):1123–31.
O’Connell RM, Chaudhuri AA, Rao DS, Baltimore D. Inositol phosphatase SHIP1 is a primary target of miR-155. Proc Natl Acad Sci U S A. 2009;106(17):7113–8.
Oertli M, Engler DB, Kohler E, Koch M, Meyer TF, Müller A. MicroRNA-155 is essential for the T cell-mediated control of Helicobacter pylori infection and for the induction of chronic Gastritis and Colitis. J Immunol (Baltimore, Md : 1950). 2011;187(7):3578–86.
Ohland CL, Macnaughton WK. Probiotic bacteria and intestinal epithelial barrier function. Am J Physiol Gastrointest Liver Physiol. 2010;298(6):G807–19.
Oishi M, Iizumi Y, Taniguchi T, Goi W, Miki T, Sakai T. Apigenin sensitizes prostate cancer cells to Apo2L/TRAIL by targeting adenine nucleotide translocase-2. PLoS ONE. 2013;8(2):e55922.
Olivo-Marston SE, Hursting SD, Perkins SN, Schetter A, Khan M, Croce C, et al. Effects of calorie restriction and diet-induced obesity on murine colon carcinogenesis, growth and inflammatory factors, and microRNA expression. PLoS ONE. 2014;9(4):e94765.
Onyeagucha BC, Mercado-Pimentel ME, Hutchison J, Flemington EK, Nelson MA. S100P/RAGE signaling regulates microRNA-155 expression via AP-1 activation in colon cancer. Exp Cell Res. 2013;319(13):2081–90.
Ortiz-Quintero B. Cell-free microRNAs in blood and other body fluids, as cancer biomarkers. Cell Prolif. 2016;49(3):281–303.
Ou Y, Ren H, Zhao R, Song L, Liu Z, Xu W, et al. Helicobacter pylori CagA promotes the malignant transformation of gastric mucosal epithelial cells through the dysregulation of the miR-155/KLF4 signaling pathway. Mol Carcinog. 2019;58(8):1427–37.
Pan X, Yang Z, Yang Z, Zhou S, Zhang H, Zang L. Effect of apigenin on proliferation and apoptosis of human lung cancer NCI-H460 cells. Nan fang yi ke da xue xue bao = J South Med Univ. 2013;33(8):1137–40.
Pang W, Su J, Wang Y, Feng H, Dai X, Yuan Y, et al. Pancreatic cancer-secreted miR-155 implicates in the conversion from normal fibroblasts to cancer-associated fibroblasts. Cancer Sci. 2015;106(10):1362–9.
Pang L, Li Q, Zhang Y, Deng B, Wu F, Wang J, et al. Transcribed ultraconserved noncoding RNA uc.160 acts as a negative regulator in gastric cancer. Am J Transl Res. 2018;10(9):2822–33.
Papaconstantinou IG, Manta A, Gazouli M, Lyberopoulou A, Lykoudis PM, Polymeneas G, et al. Expression of microRNAs in patients with pancreatic cancer and its prognostic significance. Pancreas. 2013;42(1):67–71.
Park SJ, Nakagawa T, Kitamura H, Atsumi T, Kamon H, Sawa S, et al. IL-6 regulates in vivo dendritic cell differentiation through STAT3 activation. J Immunol (Baltimore, Md : 1950). 2004;173(6):3844–54.
Park JL, Kim M, Song KS, Kim SY, Kim YS. Cell-Free miR-27a, a potential diagnostic and prognostic biomarker for gastric cancer. Genomics Inform. 2015;13(3):70–5.
Parsonnet J, Friedman GD, Vandersteen DP, Chang Y, Vogelman JH, Orentreich N, et al. Helicobacter pylori infection and the risk of gastric carcinoma. N Engl J Med. 1991;325(16):1127–31.
Patel GK, Khan MA, Bhardwaj A, Srivastava SK, Zubair H, Patton MC, et al. Exosomes confer chemoresistance to pancreatic cancer cells by promoting ROS detoxification and miR-155-mediated suppression of key gemcitabine-metabolising enzyme. DCK Br J Cancer. 2017;116(5):609–19.
Pathak S, Meng WJ, Nandy SK, Ping J, Bisgin A, Helmfors L, et al. Radiation and SN38 treatments modulate the expression of microRNAs, cytokines and chemokines in colon cancer cells in a p53-directed manner. Oncotarget. 2015;6(42):44758–80.
Peng Y, Li Z, Li Z. GRP78 secreted by tumor cells stimulates differentiation of bone marrow mesenchymal stem cells to cancer-associated fibroblasts. Biochem Biophys Res Commun. 2013;440(4):558–63.
Perrott KM, Wiley CD, Desprez PY, Campisi J. Apigenin suppresses the senescence-associated secretory phenotype and paracrine effects on breast cancer cells. GeroScience. 2017;39(2):161–73.
Pilon-Thomas S, Nelson N, Vohra N, Jerald M, Pendleton L, Szekeres K, et al. Murine pancreatic adenocarcinoma dampens SHIP-1 expression and alters MDSC homeostasis and function. PLoS ONE. 2011;6(11):e27729.
Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, et al. Multilineage potential of adult human mesenchymal stem cells. Science (New York, NY). 1999;284(5411):143–7.
Popov A, Szabo A, Mandys V. Small nucleolar RNA U91 is a new internal control for accurate microRNAs quantification in pancreatic cancer. BMC Cancer. 2015;15:774.
Preethi KA, Selvakumar SC, Sekar D. Diagnostic and therapeutic application of exosomal microRNAs inducing inflammation in type 2 diabetes mellitus. Crit Rev Immunol. 2022;42(1):1–11.
Prinz C, Weber D. MicroRNA (miR) dysregulation during Helicobacter pylori-induced gastric inflammation and cancer development: critical importance of miR-155. Oncotarget. 2020;11(10):894–904.
Qin Y, Zhao D, Zhou HG, Wang XH, Zhong WL, Chen S, et al. Apigenin inhibits NF-κB and snail signaling, EMT and metastasis in human hepatocellular carcinoma. Oncotarget. 2016;7(27):41421–31.
Qu YL, Wang HF, Sun ZQ, Tang Y, Han XN, Yu XB, et al. Up-regulated miR-155-5p promotes cell proliferation, invasion and metastasis in colorectal carcinoma. Int J Clin Exp Pathol. 2015;8(6):6988–94.
Qu Y, Zhang H, Sun W, Han Y, Li S, Qu Y, et al. MicroRNA-155 promotes gastric cancer growth and invasion by negatively regulating transforming growth factor-β receptor 2. Cancer Sci. 2018;109(3):618–28.
Quante M, Tu SP, Tomita H, Gonda T, Wang SS, Takashi S, et al. Bone marrow-derived myofibroblasts contribute to the mesenchymal stem cell niche and promote tumor growth. Cancer Cell. 2011;19(2):257–72.
Quigley EM. Prebiotics and probiotics; modifying and mining the microbiota. Pharmacol Res. 2010;61(3):213–8.
Rad A, Esmaeili Dizghandi S, Abbaszadegan MR, Taghechian N, Najafi M, Forghanifard MM. SOX1 is correlated to stemness state regulator SALL4 through progression and invasiveness of esophageal squamous cell carcinoma. Gene. 2016;594(2):171–5.
Raimondi S, Maisonneuve P, Lowenfels AB. Epidemiology of pancreatic cancer: an overview. Nat Rev Gastroenterol Hepatol. 2009;6(12):699–708.
Ranji P, Akbarzadeh A, Rahmati-Yamchi M. Associations of Probiotics with Vitamin D and Leptin Receptors and their Effects on Colon Cancer. Asian Pac J Cancer Prevent: APJCP. 2015;16(9):3621–7.
Rashed MH, Kanlikilicer P, Rodriguez-Aguayo C, Pichler M, Bayraktar R, Bayraktar E, et al. Exosomal miR-940 maintains SRC-mediated oncogenic activity in cancer cells: a possible role for exosomal disposal of tumor suppressor miRNAs. Oncotarget. 2017;8(12):20145–64.
Rauh MJ, Ho V, Pereira C, Sham A, Sly LM, Lam V, et al. SHIP represses the generation of alternatively activated macrophages. Immunity. 2005;23(4):361–74.
Ren Y, Gao J, Liu JQ, Wang XW, Gu JJ, Huang HJ, et al. Differential signature of fecal microRNAs in patients with pancreatic cancer. Mol Med Rep. 2012;6(1):201–9.
Ren C, Zhang Z, Wang S, Zhu W, Zheng P, Wang W. Circular RNA hsa_circ_0001178 facilitates the invasion and metastasis of colorectal cancer through upregulating ZEB1 via sponging multiple miRNAs. Biol Chem. 2020;401(4):487–96.
Rosenbluh J, Wang X, Hahn WC. Genomic insights into WNT/β-catenin signaling. Trends Pharmacol Sci. 2014;35(2):103–9.
Rossini M, Gatti D, Adami S. Involvement of WNT/β-catenin signaling in the treatment of osteoporosis. Calcif Tissue Int. 2013;93(2):121–32.
Rovithi M, Avan A, Funel N, Leon LG, Gomez VE, Wurdinger T, et al. Development of bioluminescent chick chorioallantoic membrane (CAM) models for primary pancreatic cancer cells: a platform for drug testing. Sci Rep. 2017;7:44686.
Rudin CM, Durinck S, Stawiski EW, Poirier JT, Modrusan Z, Shames DS, et al. Comprehensive genomic analysis identifies SOX2 as a frequently amplified gene in small-cell lung cancer. Nat Genet. 2012;44(10):1111–6.
Rupaimoole R, Calin GA, Lopez-Berestein G, Sood AK. miRNA deregulation in cancer cells and the tumor microenvironment. Cancer Discov. 2016;6(3):235–46.
Rutkowski MR, Svoronos N, Perales-Puchalt A, Conejo-Garcia JR. The tumor macroenvironment: cancer-promoting networks beyond tumor beds. Adv Cancer Res. 2015;128:235–62.
Ryu JK, Hong SM, Karikari CA, Hruban RH, Goggins MG, Maitra A. Aberrant MicroRNA-155 expression is an early event in the multistep progression of pancreatic adenocarcinoma. Pancreatology. 2010;10(1):66–73.
Sah BR, Owczarczyk K, Siddique M, Cook GJR, Goh V. Radiomics in esophageal and gastric cancer. Abdomin Radiol (New York). 2019;44(6):2048–58.
Salzman J, Chen RE, Olsen MN, Wang PL, Brown PO. Cell-type specific features of circular RNA expression. PLoS Genet. 2013;9(9):e1003777.
Santos JC, Brianti MT, Almeida VR, Ortega MM, Fischer W, Haas R, et al. Helicobacter pylori infection modulates the expression of miRNAs associated with DNA mismatch repair pathway. Mol Carcinog. 2017;56(4):1372–9.
Santos JC, Lima NDS, Sarian LO, Matheu A, Ribeiro ML, Derchain SFM. Exosome-mediated breast cancer chemoresistance via miR-155 transfer. Sci Rep. 2018;8(1):829.
Sarkar A, Hochedlinger K. The sox family of transcription factors: versatile regulators of stem and progenitor cell fate. Cell Stem Cell. 2013;12(1):15–30.
Sato-Kuwabara Y, Melo SA, Soares FA, Calin GA. The fusion of two worlds: non-coding RNAs and extracellular vesicles–diagnostic and therapeutic implications (Review). Int J Oncol. 2015;46(1):17–27.
Schetter AJ, Harris CC. Plasma microRNAs: a potential biomarker for colorectal cancer? Gut. 2009;58(10):1318–9.
Schlottmann F, Molena D, Patti MG. Gastroesophageal reflux and Barrett’s esophagus: a pathway to esophageal adenocarcinoma. Updat Surg. 2018;70(3):339–42.
Schreiner S, Didio A, Hung LH, Bindereif A. Design and application of circular RNAs with protein-sponge function. Nucleic Acids Res. 2020;48(21):12326–35.
Sebio A, Kahn M, Lenz HJ. The potential of targeting Wnt/β-catenin in colon cancer. Expert Opin Ther Targets. 2014;18(6):611–5.
Selvakumar SC, Preethi KA, Sekar D. MicroRNA-510-3p regulated vascular dysfunction in Preeclampsia by targeting Vascular Endothelial Growth Factor A (VEGFA) and its signaling axis. Placenta. 2024;153:31–52.
Seux M, Peuget S, Montero MP, Siret C, Rigot V, Clerc P, et al. TP53INP1 decreases pancreatic cancer cell migration by regulating SPARC expression. Oncogene. 2011;30(27):3049–61.
Shangguan L, Ti X, Krause U, Hai B, Zhao Y, Yang Z, et al. Inhibition of TGF-β/Smad signaling by BAMBI blocks differentiation of human mesenchymal stem cells to carcinoma-associated fibroblasts and abolishes their protumor effects. Stem Cells (Dayton, Ohio). 2012;30(12):2810–9.
Shen H, Yu X, Yang F, Zhang Z, Shen J, Sun J, et al. Reprogramming of Normal Fibroblasts into Cancer-Associated Fibroblasts by miRNAs-Mediated CCL2/VEGFA Signaling. PLoS Genet. 2016;12(8):e1006244.
Sheth S, Jajoo S, Kaur T, Mukherjea D, Sheehan K, Rybak LP, et al. Resveratrol reduces prostate cancer growth and metastasis by inhibiting the Akt/MicroRNA-21 pathway. PLoS ONE. 2012;7(12):e51655.
Shi S-S, Zhang H-P, Yang C-Q, Li L-N, Shen Y, Zhang Y-Q. Exosomal miR-155-5p promotes proliferation and migration of gastric cancer cells by inhibiting TP53INP1 expression. Pathol – Res Pract. 2020a;216(6):152986.
Shi Q, Zhang Y, Liu W, Xiao H, Qi Y, Li J, et al. Latent membrane protein 2A inhibits expression level of Smad2 through regulating miR-155-5p in EBV-associated gastric cancer cell lines. J Med Virol. 2020b;92(1):96–106.
Shi SS, Zhang HP, Yang CQ, Li LN, Shen Y, Zhang YQ. Exosomal miR-155-5p promotes proliferation and migration of gastric cancer cells by inhibiting TP53INP1 expression. Pathol Res Pract. 2020c;216(6):152986.
Shukla S, Gupta S. Apigenin: a promising molecule for cancer prevention. Pharm Res. 2010;27(6):962–78.
Shukla S, Bhaskaran N, Babcook MA, Fu P, Maclennan GT, Gupta S. Apigenin inhibits prostate cancer progression in TRAMP mice via targeting PI3K/Akt/FoxO pathway. Carcinogenesis. 2014;35(2):452–60.
Siegel RL, Miller KD, Jemal A. Cancer statistics. CA: Cancer J Clin. 2019;69(1):7–34.
Silverman DT, Swanson CA, Gridley G, Wacholder S, Greenberg RS, Brown LM, et al. Dietary and nutritional factors and pancreatic cancer: a case-control study based on direct interviews. J Natl Cancer Inst. 1998;90(22):1710–9.
Simons M, Raposo G. Exosomes–vesicular carriers for intercellular communication. Curr Opin Cell Biol. 2009;21(4):575–81.
Singh J, Rivenson A, Tomita M, Shimamura S, Ishibashi N, Reddy BS. Bifidobacterium longum, a lactic acid-producing intestinal bacterium inhibits colon cancer and modulates the intermediate biomarkers of colon carcinogenesis. Carcinogenesis. 1997;18(4):833–41.
Sly LM, Ho V, Antignano F, Ruschmann J, Hamilton M, Lam V, et al. The role of SHIP in macrophages. Front Biosci. 2007;12:2836–48.
Smyth EC, Moehler M. Late-line treatment in metastatic gastric cancer: today and tomorrow. Ther Adv Med Oncol. 2019;11:1758835919867522.
Smyth LA, Boardman DA, Tung SL, Lechler R, Lombardi G. MicroRNAs affect dendritic cell function and phenotype. Immunology. 2015;144(2):197–205.
Smyth EC, Nilsson M, Grabsch HI, van Grieken NC, Lordick F. Gastric cancer. Lancet (London, England). 2020;396(10251):635–48.
Solinas G, Germano G, Mantovani A, Allavena P. Tumor-associated macrophages (TAM) as major players of the cancer-related inflammation. J Leukoc Biol. 2009;86(5):1065–73.
Song L, Liu D, He J, Wang X, Dai Z, Zhao Y, et al. SOX1 inhibits breast cancer cell growth and invasion through suppressing the Wnt/β-catenin signaling pathway. APMIS : Acta Pathol Microbiol Et Immunol Scandinavica. 2016;124(7):547–55.
Spaeth E, Klopp A, Dembinski J, Andreeff M, Marini F. Inflammation and tumor microenvironments: defining the migratory itinerary of mesenchymal stem cells. Gene Ther. 2008;15(10):730–8.
Su N, Li L, Zhou E, Li H, Wu S, Cao Z. Resveratrol downregulates miR-155-5p to block the malignant behavior of gastric cancer cells. Biomed Res Int. 2022;2022:6968641.
Sun S, Sun P, Wang C, Sun T. Downregulation of microRNA-155 accelerates cell growth and invasion by targeting c-myc in human gastric carcinoma cells. Oncol Rep. 2014;32(3):951–6.
Syed SN, Brüne B. Exosomal and non-exosomal micrornas: New kids on the block for cancer therapy. Int J Mol Sci. 2022;23(9):4493.
Takahashi RU, Prieto-Vila M, Kohama I, Ochiya T. Development of miRNA-based therapeutic approaches for cancer patients. Cancer Sci. 2019;110(4):1140–7.
Takeuchi M, Takeuchi H, Kawakubo H, Kitagawa Y. Update on the indications and results of sentinel node mapping in upper GI cancer. Clin Exp Metas. 2018;35(5–6):455–61.
Tan L, Sui X, Deng H, Ding M. Holoclone forming cells from pancreatic cancer cells enrich tumor initiating cells and represent a novel model for study of cancer stem cells. PLoS ONE. 2011;6(8):e23383.
Taylor PR, Greenwald P. Nutritional interventions in cancer prevention. J Clin Oncol: Off J Am Soc Clin Oncol. 2005;23(2):333–45.
Tili E, Michaille JJ, Cimino A, Costinean S, Dumitru CD, Adair B, et al. Modulation of miR-155 and miR-125b levels following lipopolysaccharide/TNF-alpha stimulation and their possible roles in regulating the response to endotoxin shock. J Immunol (Baltimore, Md : 1950). 2007;179(8):5082–9.
Tili E, Michaille JJ, Costinean S, Croce CM. MicroRNAs, the immune system and rheumatic disease. Nat Clin Pract Rheumatol. 2008a;4(10):534–41.
Tili E, Michaille JJ, Calin GA. Expression and function of micro-RNAs in immune cells during normal or disease state. Int J Med Sci. 2008b;5(2):73–9.
Tili E, Croce CM, Michaille JJ. miR-155: on the crosstalk between inflammation and cancer. Int Rev Immunol. 2009;28(5):264–84.
Tramontano AC, Nipp R, Mercaldo ND, Kong CY, Schrag D, Hur C. Survival disparities by race and ethnicity in early esophageal cancer. Dig Dis Sci. 2018;63(11):2880–8.
Tu J, Xing Y, Guo Y, Tang F, Guo L, Xi T. TanshinoneIIA ameliorates inflammatory microenvironment of colon cancer cells via repression of microRNA-155. Int Immunopharmacol. 2012;14(4):353–61.
Uccello M, Malaguarnera G, Basile F, D’Agata V, Malaguarnera M, Bertino G, et al. Potential role of probiotics on colorectal cancer prevention. BMC Surg. 2012;12 Suppl 1(Suppl 1):S35.
Ujiki MB, Ding XZ, Salabat MR, Bentrem DJ, Golkar L, Milam B, et al. Apigenin inhibits pancreatic cancer cell proliferation through G2/M cell cycle arrest. Mol Cancer. 2006;5:76.
Valadi H, Ekström K, Bossios A, Sjöstrand M, Lee JJ, Lötvall JO. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat Cell Biol. 2007;9(6):654–9.
van den Brandt PA, Goldbohm RA. Nutrition in the prevention of gastrointestinal cancer. Best Pract Res Clin Gastroenterol. 2006;20(3):589–603.
Van Roosbroeck K, Fanini F, Setoyama T, Ivan C, Rodriguez-Aguayo C, Fuentes-Mattei E, et al. Combining Anti-Mir-155 with Chemotherapy for the Treatment of Lung Cancers. Clin Cancer Res. 2017;23(11):2891–904.
Varoni EM, Lo Faro AF, Sharifi-Rad J, Iriti M. Anticancer Molecular Mechanisms of Resveratrol. Front Nutr. 2016;3:8.
Vartiainen MK, Guettler S, Larijani B, Treisman R. Nuclear actin regulates dynamic subcellular localization and activity of the SRF cofactor MAL. Science (New York, NY). 2007;316(5832):1749–52.
Velázquez KT, Enos RT, McClellan JL, Cranford TL, Chatzistamou I, Singh UP, et al. MicroRNA-155 deletion promotes tumorigenesis in the azoxymethane-dextran sulfate sodium model of colon cancer. Am J Physiol Gastrointest Liver Physiol. 2016;310(6):G347–58.
Villalobos-Ayala K, Ortiz Rivera I, Alvarez C, Husain K, DeLoach D, Krystal G, et al. Apigenin increases SHIP-1 expression, promotes tumoricidal macrophages and anti-tumor immune responses in murine pancreatic cancer. Cancers (Basel). 2020;12(12):3631.
Vo JN, Cieslik M, Zhang Y, Shukla S, Xiao L, Zhang Y, et al. The Landscape of Circular RNA in Cancer. Cell. 2019;176(4):869-81.e13.
Waddell N, Pajic M, Patch AM, Chang DK, Kassahn KS, Bailey P, et al. Whole genomes redefine the mutational landscape of pancreatic cancer. Nature. 2015;518(7540):495–501.
Waghray M, Yalamanchili M, Dziubinski M, Zeinali M, Erkkinen M, Yang H, et al. GM-CSF Mediates Mesenchymal-Epithelial Cross-talk in Pancreatic Cancer. Cancer Discov. 2016;6(8):886–99.
Wang S, Gao Y. Pancreatic cancer cell-derived microRNA-155-5p-containing extracellular vesicles promote immune evasion by triggering EHF-dependent activation of Akt/NF-κB signaling pathway. Int Immunopharmacol. 2021;100:107990.
Wang DZ, Li S, Hockemeyer D, Sutherland L, Wang Z, Schratt G, et al. Potentiation of serum response factor activity by a family of myocardin-related transcription factors. Proc Natl Acad Sci U S A. 2002;99(23):14855–60.
Wang H, Leav I, Ibaragi S, Wegner M, Hu GF, Lu ML, et al. SOX9 is expressed in human fetal prostate epithelium and enhances prostate cancer invasion. Can Res. 2008;68(6):1625–30.
Wang J, Chen J, Chang P, LeBlanc A, Li D, Abbruzzesse JL, et al. MicroRNAs in plasma of pancreatic ductal adenocarcinoma patients as novel blood-based biomarkers of disease. Cancer Prev Res (Phila). 2009;2(9):807–13.
Wang XY, Wu MH, Liu F, Li Y, Li N, Li GY, et al. Differential miRNA expression and their target genes between NGX6-positive and negative colon cancer cells. Mol Cell Biochem. 2010;345(1–2):283–90.
Wang P, Zhu CF, Ma MZ, Chen G, Song M, Zeng ZL, et al. Micro-RNA-155 is induced by K-Ras oncogenic signal and promotes ROS stress in pancreatic cancer. Oncotarget. 2015;6(25):21148–58.
Wang J, Paris PL, Chen J, Ngo V, Yao H, Frazier ML, et al. Next generation sequencing of pancreatic cyst fluid microRNAs from low grade-benign and high grade-invasive lesions. Cancer Lett. 2015;356(2):404–9.
Wang D, Zhu ZM, Tu YL, Dou CQ, Xu Y, Tan XL, et al. Identfication of key miRNAs in pancreatitis using bioinformatics analysis of microarray data. Mol Med Rep. 2016;14(6):5451–60.
Wang C, Zhang C, Liu L, A X, Chen B, Li Y, et al. Macrophage-derived mir-155-containing exosomes suppress fibroblast proliferation and promote fibroblast inflammation during cardiac injury. Mol Ther J Am Soc Gene Ther. 2017;25(1):192–204.
Wang M, Yang F, Qiu R, Zhu M, Zhang H, Xu W, et al. The role of mmu-miR-155-5p-NF-κB signaling in the education of bone marrow-derived mesenchymal stem cells by gastric cancer cells. Cancer Med. 2018a;7(3):856–68.
Wang P, Xu LJ, Qin JJ, Zhang L, Zhuang GH. MicroRNA-155 inversely correlates with esophageal cancer progression through regulating tumor-associated macrophage FGF2 expression. Biochem Biophys Res Commun. 2018b;503(2):452–8.
Wang Z, Su M, Xiang B, Zhao K, Qin B. Circular RNA PVT1 promotes metastasis via miR-145 sponging in CRC. Biochem Biophys Res Commun. 2019a;512(4):716–22.
Wang M, Qiu R, Yu S, Xu X, Li G, Gu R, et al. Paclitaxel-resistant gastric cancer MGC-803 cells promote epithelial-to-mesenchymal transition and chemoresistance in paclitaxel-sensitive cells via exosomal delivery of miR-155-5p. Int J Oncol. 2019b;54(1):326–38.
Wang H, Wei H, Wang J, Li L, Chen A, Li Z. MicroRNA-181d-5p-Containing exosomes derived from CAFs promote EMT by regulating CDX2/HOXA5 in breast cancer. Mol Ther Nucleic Acids. 2020;19:654–67.
Wang Y, Petrikova E, Gross W, Sticht C, Gretz N, Herr I, et al. Corrigendum: Sulforaphane promotes dendritic cell stimulatory capacity through modulation of regulatory molecules, JAK/STAT3- and microRNA-signaling. Front Immunol. 2022;13:975653.
Wang D, Geng W, Han L, Song R, Qu Q, Chen X, et al. Pro-carcinogenic actions of miR-155/FOXO3a in colorectal cancer development. Cell Mol Biol (Noisy-le-grand). 2023;69(10):160–5.
Washington MK, Goldberg RM, Chang GJ, Limburg P, Lam AK, Salto-Tellez M, et al. Diagnosis of digestive system tumours. Int J Cancer. 2021;148(5):1040–50.
Wawro M, Wawro K, Kochan J, Solecka A, Sowinska W, Lichawska-Cieslar A, et al. ZC3H12B/MCPIP2, a new active member of the ZC3H12 family. RNA. 2019;25(7):840–56.
Weber CE, Kothari AN, Wai PY, Li NY, Driver J, Zapf MA, et al. Osteopontin mediates an MZF1-TGF-β1-dependent transformation of mesenchymal stem cells into cancer-associated fibroblasts in breast cancer. Oncogene. 2015;34(37):4821–33.
Wilusz JE, Sharp PA. Molecular biology. A circuitous route to noncoding RNA. Science (New York, NY). 2013;340(6131):440–1.
Wolpin BM, Chan AT, Hartge P, Chanock SJ, Kraft P, Hunter DJ, et al. ABO blood group and the risk of pancreatic cancer. J Natl Cancer Inst. 2009;101(6):424–31.
Wu J, Cai H, Xiang YB, Matthews CE, Ye F, Zheng W, et al. Intra-individual variation of miRNA expression levels in human plasma samples. Biomarkers. 2018;23(4):339–46.
Wu M, Duan Q, Liu X, Zhang P, Fu Y, Zhang Z, et al. MiR-155-5p promotes oral cancer progression by targeting chromatin remodeling gene ARID2. Biomed Pharmacother. 2020;122:109696.
Wu L, Jiang F, Shen X. Helicobacter pylori CagA protein regulating the biological characteristics of gastric cancer through the miR-155–5p/SMAD2/SP1 axis. Pathogens. 2022;11(8):846.
Xiang Y, Liao XH, Yao A, Qin H, Fan LJ, Li JP, et al. MRTF-A-miR-206-WDR1 form feedback loop to regulate breast cancer cell migration. Exp Cell Res. 2017;359(2):394–404.
Xiao B, Liu Z, Li BS, Tang B, Li W, Guo G, et al. Induction of microRNA-155 during Helicobacter pylori infection and its negative regulatory role in the inflammatory response. J Infect Dis. 2009;200(6):916–25.
Xu X, Tao Y, Shan L, Chen R, Jiang H, Qian Z, et al. The Role of MicroRNAs in Hepatocellular Carcinoma. J Cancer. 2018;9(19):3557–69.
Yan XL, Jia YL, Chen L, Zeng Q, Zhou JN, Fu CJ, et al. Hepatocellular carcinoma-associated mesenchymal stem cells promote hepatocarcinoma progression: role of the S100A4-miR155-SOCS1-MMP9 axis. Hepatology (Baltimore, MD). 2013;57(6):2274–86.
Yan X, Qi M, Li P, Zhan Y, Shao H. Apigenin in cancer therapy: anti-cancer effects and mechanisms of action. Cell Biosci. 2017;7:50.
Yanaihara N, Caplen N, Bowman E, Seike M, Kumamoto K, Yi M, et al. Unique microRNA molecular profiles in lung cancer diagnosis and prognosis. Cancer Cell. 2006;9(3):189–98.
Ye J, Zou M, Li P, Liu H. MicroRNA Regulation of Energy Metabolism to Induce Chemoresistance in Cancers. Technol Cancer Res Treat. 2018;17:1533033818805997.
Yi T, Song SU. Immunomodulatory properties of mesenchymal stem cells and their therapeutic applications. Arch Pharmacal Res. 2012;35(2):213–21.
Yin L, Liu T, Li C, Yan G, Li C, Zhang J, et al. The MRTF-A/miR-155/SOX1 pathway mediates gastric cancer migration and invasion. Cancer Cell Int. 2020;20:303.
Yoon H, Belmonte KC, Kasten T, Bateman R, Kim J. Intra- and inter-individual variability of microRNA levels in human cerebrospinal fluid: critical implications for biomarker discovery. Sci Rep. 2017;7(1):12720.
Yu J, Li A, Hong SM, Hruban RH, Goggins M. MicroRNA alterations of pancreatic intraepithelial neoplasias. Clin Cancer Res. 2012;18(4):981–92.
Yu Q, Xu C, Yuan W, Wang C, Zhao P, Chen L, et al. Evaluation of plasma MicroRNAs as diagnostic and prognostic biomarkers in pancreatic adenocarcinoma: miR-196a and miR-210 could be negative and positive prognostic markers. Respect Biomed Res Int. 2017a;2017:6495867.
Yu H, Xu W, Gong F, Chi B, Chen J, Zhou L. MicroRNA-155 regulates the proliferation, cell cycle, apoptosis and migration of colon cancer cells and targets CBL. Exp Ther Med. 2017b;14(5):4053–60.
Zare A, Alipoor B, Omrani MD, Zali MR, Malekpour Alamdari N, Ghaedi H. Decreased miR-155-5p, miR-15a, and miR-186 Expression in Gastric Cancer Is Associated with Advanced Tumor Grade and Metastasis. Iran Biomed J. 2019;23(5):338–43.
Zhang H, Li W, Nan F, Ren F, Wang H, Xu Y, et al. MicroRNA expression profile of colon cancer stem-like cells in HT29 adenocarcinoma cell line. Biochem Biophys Res Commun. 2011;404(1):273–8.
Zhang M, He Y, Sun X, Li Q, Wang W, Zhao A, et al. A high M1/M2 ratio of tumor-associated macrophages is associated with extended survival in ovarian cancer patients. Journal of Ovarian Research. 2014;7:19.
Zhang J, Li S, Li L, Li M, Guo C, Yao J, et al. Exosome and exosomal microRNA: trafficking, sorting, and function. Genomics Proteomics Bioinformatics. 2015;13(1):17–24.
Zhang LF, Yu XL, Ji M, Liu SY, Wu XL, Wang YJ, et al. Resveratrol alleviates motor and cognitive deficits and neuropathology in the A53T α-synuclein mouse model of Parkinson’s disease. Food Funct. 2018a;9(12):6414–26.
Zhang LL, Zhang LF, Shi YB. Down-regulated paxillin suppresses cell proliferation and invasion by inhibiting M2 macrophage polarization in colon cancer. Biol Chem. 2018b;399(11):1285–95.
Zhang J, Guo J, He R, Li J, Du B, Zhang Y, et al. Analysis of the differential expression of serum miR-21-5p, miR-135-5p, and miR-155-5p by Bifidobacterium triplex viable capsules during the perioperative stage of colorectal cancer. Int J Colorectal Dis. 2024;39(1):48.
Zhao G, Han X, Cheng W, Ni J, Zhang Y, Lin J, et al. Apigenin inhibits proliferation and invasion, and induces apoptosis and cell cycle arrest in human melanoma cells. Oncol Rep. 2017;37(4):2277–85.
Zheng P, Chen L, Yuan X, Luo Q, Liu Y, Xie G, et al. Exosomal transfer of tumor-associated macrophage-derived miR-21 confers cisplatin resistance in gastric cancer cells. J Exp Clin Cancer Res. 2017;36(1):53.
Zheng YJ, Liang TS, Wang J, Zhao JY, Zhai SN, Yang DK, et al. MicroRNA-155 acts as a diagnostic and prognostic biomarker for oesophageal squamous cell carcinoma. Artif Cells Nanomed Biotechnol. 2020;48(1):977–82.
Zheng D, Huo M, Li B, Wang W, Piao H, Wang Y, et al. The role of exosomes and exosomal MicroRNA in cardiovascular disease. Front Cell Dev Biol. 2021;8:616161.
Zhong Y, Du Y, Yang X, Mo Y, Fan C, Xiong F, et al. Circular RNAs function as ceRNAs to regulate and control human cancer progression. Mol Cancer. 2018;17(1):79.
Zhou H, Huang X, Cui H, Luo X, Tang Y, Chen S, et al. miR-155 and its star-form partner miR-155* cooperatively regulate type I interferon production by human plasmacytoid dendritic cells. Blood. 2010;116(26):5885–94.
Zhou Q, Li M, Wang X, Li Q, Wang T, Zhu Q, et al. Immune-related microRNAs are abundant in breast milk exosomes. Int J Biol Sci. 2012;8(1):118–23.
Zhou B, Ma R, Si W, Li S, Xu Y, Tu X, et al. MicroRNA-503 targets FGF2 and VEGFA and inhibits tumor angiogenesis and growth. Cancer Lett. 2013;333(2):159–69.
Zhou D, Bai F, Zhang X, Hu M, Zhao G, Zhao Z, et al. SOX10 is a novel oncogene in hepatocellular carcinoma through Wnt/β-catenin/TCF4 cascade. Tumour Biol: J Int Soc Oncodev Biol Meds. 2014;35(10):9935–40.
Acknowledgements
Not applicable.
Funding
The Science and Technology Research Program of Chongqing Municipal Education Commission (Grant No. KJ1702021).
Author information
Authors and Affiliations
Contributions
JG, LZ and MRM contributed in the conception, design and drafting of the manuscript. All authors approved the final version for submission.
Corresponding authors
Ethics declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Guo, J., Zhong, L. & Momeni, M.R. MicroRNA-155 and its exosomal form: Small pieces in the gastrointestinal cancers puzzle. Cell Biol Toxicol 40, 77 (2024). https://doi.org/10.1007/s10565-024-09920-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10565-024-09920-2