Abstract
Purpose
Computer-navigated (CN) total hip arthroplasty (THA) offers improved acetabular component placement and radiographic outcomes, but inconsistent assessment methods of its learning curves render the evaluation of adopting a novel platform challenging. Therefore, we conducted a systematic review to assess the learning curve associated with CN-THA, both tracking a surgeon's performance across initial cases and comparing their performance to manual THA (M-THA).
Methods
A search was conducted using PubMed, MEDLINE, EBSCOhost, and Google Scholar on June 16, 2023 to find research articles published after January 1, 2000 (PROSPERO registration: CRD4202339403) that investigated the learning curve associated with CN-THA. 655 distinct articles were retrieved and subsequently screened for eligibility. In the final analysis, nine publications totaling 847 THAs were evaluated. The Methodological Index for Nonrandomized Studies (MINORS) tool was utilized to evaluate the potential for bias, with the mean MINORS score of 21.3 ± 1.2.
Results
CN-THA showed early advantages to M-THA for component placement accuracy and radiographic outcomes but longer operative times (+ 3− 20 min). There was a learning curve required to achieve peak proficiency in these metrics, though mixed methodologies made the required caseload unclear.
Conclusions
CN-THA offers immediate advantages to M-THA for component placement accuracy and radiographic outcomes, though CN-THA’s advantages become more pronounced with experience. Surgeons should anticipate longer operative times during the learning curve for CN-THA, which lessen following a modest caseload. A more thorough evaluation of novel computer-navigated technologies would be enhanced by adopting a more uniform method of defining learning curves for outcomes of interest.
Registration PROSPERO registration of the study protocol: CRD42023394031, 27 June 2023.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Accurate placement of the acetabular component is crucial for favorable outcomes after total hip arthroplasty (THA), as malposition of the implant is a prominent cause of complications and revision [1,2,3,4]. Traditionally, surgeons rely on intraoperative landmarks to guide placement, a challenging feat that has become increasingly difficult with the popularity of minimally invasive procedures [5]. Therefore, manual techniques for attaining consistent and accurate component placement and restoration of leg length and offset are challenging. This has created a growing demand for surgical technologies, such as computer-navigated (CN) THA platforms, which have demonstrated improved placement of the acetabular component and radiographic outcomes compared to manual THA (M-THA) [6,7,8,9]. However, much like the acquisition of any other surgical skill, surgeons face a learning curve upon adoption of surgical technologies [10,11,12,13].
Surgical learning curves have received growing interest in recent years, as studies continue to indicate substantial implications related to cost-effectiveness, clinical outcomes, and patient safety [14,15,16,17,18,19]. The surgical learning curve was initially described by Luft et al. [20] as having four stages: (1) at the onset of training, a sharp uprise in the measured outcome; (2) period of diminishing returns with slight improvements in the outcome; (3) plateau exhibiting no further improvements; and (4) age-related regression. The point in time or case number in which the outcome of interest begins to stabilize, or plateau, is the inflection point, which delineates the transition from the learning to the proficiency phase [20]. With the continued introduction of novel CN-THA platforms, authors have explored the learning curve associated with their use, and evaluated how patient outcomes are influenced as surgeons gain familiarity with these technologies [21,22,23,24,25]. While insightful, these studies have been inconsistent in the methodologies used to assess the learning curve, making the interpretation of their collective findings unclear. As surgeons will continue to face decisions regarding the implementation of surgical technologies into practice, clarity regarding the early challenges that may be incurred with the use of novel computer navigation platform will be valuable.
Therefore, to comprehensively evaluate the learning curve for adopting CN-THA, a systematic review of current literature was conducted. We aimed to answer: (1) What case load must a surgeon achieve to become proficient in respect to operative time, component placement accuracy, and radiographic outcomes for CN-THA? and (2) How does a surgeon’s initial performance with CN-THA compare to other techniques, such as M-THA?
Methods
Search strategy
On June 16, 2023, a search was conducted using PubMed, MEDLINE, EBSCOhost, and Google Scholar to find studies that assessed the learning curve for RA- and CN-THA that were published between January 1, 2000, and June 16, 2023. The Boolean operators “AND” or “OR” were combined with the following keywords and Medical Subject Headings (Mesh): (“Arthroplasty, Replacement, Hip”[Mesh] OR “Arthroplasty, Replacement”[Mesh] OR “total hip arthroplasty” OR “THA”) AND (“Robotics”[Mesh] OR “robotic*” OR “Surgery, Computer-Assisted”[Mesh] OR “Robotic Surgical Procedures”[Mesh] OR “robotic arm” OR “computer navigated”) AND (“Learning Curve”[Mesh] OR “learning” OR “curve” OR “train*” OR “skill*” OR “development” OR “education” OR “proficiency”).
Eligibility criteria
Eligible articles included studies that had (1) full-text manuscripts in English and (2) evaluated the learning curve in adopting CN-THA. The following articles were excluded from the analysis: (1) case reports, (2) reviews, (3) duplicate articles, (4) gray literature (preprint server articles, posters, and abstracts), and (5) articles not written in English.
Study selection
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed in conducting this review (PROSPERO registration: CRD42023394031, June 27, 2023). After deleting duplicates, 655 articles were returned by the query. Each unique article retrieved via the search term was evaluated for eligibility by two independent reviewers (PAS, JRP). To reach consensus, any differences were consulted with a third reviewer (CJH). Forty-eight papers were eligible for a full-text evaluation after title and abstract screening, with nine meeting all criteria for inclusion in the present analysis. No further studies were found when the reference lists for each article were reviewed (Fig. 1).
Risk of bias in individual studies
Using the MINORS tool, two independent reviewers (PAS, JRP) evaluated the bias risk [26]. Using 12 criteria regarding the rigor of the study design, outcomes assessed, and follow-up, this verified grading method assigns comparative studies a score between 0 and 24, with higher scores denoting higher quality research. Grading disagreements were settled by reaching a consensus with a third reviewer (CJH). The average MINORS score was 21.3 ± 1.2.
Outcome measures
Two methods were used to evaluate the learning curve: (1) temporally evaluating a surgeon’s performance over their initial versus later CN-THA cases and (2) comparatively comparing initial CN-THA case outcomes versus outcomes achieved via other THA approaches (namely M-THA). Outcomes of interest included operative time, accuracy of acetabular component placement, radiographic accuracy (LLD and offset), functional outcomes, radiation exposure, and postoperative adverse events. No studies included in the review compared complication profiles during the learning curve. The accuracy of acetabular component placement was assessed with anteversion and inclination (i.e., average values, target value deviations, and safe zone outliers). As the included studies had substantial methodologic heterogeneity, a meta-analysis was not conducted; rather, we conducted a narrative synthesis by presenting and synthesizing key findings. When available, we reported quantitative data for positive findings and qualitative data for negative findings. Likewise, due to substantial heterogeneity in the comparison cohorts among studies, we were unable to visually represent the acetabular component placement accuracy metrics via Bland-Altman plots for both the temporal and comparative assessments of the CN-THA learning curve.
Study characteristics
Included in the final analysis were a total of nine studies assessing 847 THAs [21,22,23,24,25, 27,28,29,30] (Table 1). Six studies assessed the learning curve temporally [21, 23, 25, 27,28,29] and six assessed the curve comparatively [22,23,24, 28,29,30]. Patient characteristics, follow-up timeframes, THA approach, type of acetabular implant, and computer-navigated platform utilized varied among articles (Table 1).
Results
Temporal assessment of the CN-THA learning curve
Of the six studies that assessed the learning curve of CN-THA temporally, five divided the surgeon’s initial cases into cohorts and compared early cases to later [21, 25, 27,28,29] (Table 2). Two of these studies compared the first 20 procedures to a group of later ones [21, 28], with one showing marked improvements in cup medialization accuracy after 20 cases, but no difference in deviation from planned cup height, anteversion, or inclination, or mean LLD [21]. However, the other study showed marked improvement in anteversion and inclination accuracy, as more components were placed within the target zone after 20 cases (44% vs 87%) [28]. Another study compared the surgeon’s initial 49 cases to 47 cases thereafter, showing a decrease in deviation from planned anteversion (1.04° vs 0.85°) and inclination (0.88° to 0.69°), though no change in operative time [29]. Thorey et al. [25] demonstrated marked differences between intraoperative and radiographic anteversion (15.1° vs 20.9°) and inclination (43.7° vs 47.3°) in cases 1–30, but found no difference in intraoperative versus measured values in cases 31–60. Additionally, navigation time was lessened after 30 cases (13.2 vs 4.8 min). Meanwhile, a remaining study reported a marked decrease in operative time after five cases, though no change in deviation from planned cup inclination or anteversion with experience [27].
Comparative assessment of the CN-THA learning curve
Of the six studies that assessed the learning curve of CN-THA comparatively, three compared a surgeon's initial navigated procedures to past conventional procedures they had performed, with one showing marked increases in cups placed within the surgeon’s combined target zone with navigation (30% vs 6%) [28] and another showing fewer ≥ 10° outliers in anteversion (14% vs 21%) and inclination (4% vs 13%) [29] (Table 3). Additionally, one of these studies showed increased operative time for CN-THA (+ 20 min), with little improvement when comparing the early navigated cases (cases 1–49: 128 min), to the later cases (cases 50–96: 124 min) [29]; though another study showed only a modest increase in operative time for CN-THA compared to M-THA (+ 3 min)[24]. Another study compared a surgeon’s initial CN-THA procedures to fluoroscopically guided procedures they had performed, with handheld navigation demonstrating lower deviation from planned inclination (2.9° vs 3.4°) and a longer operative time (92 vs 72 min) over the first 30 cases [23]. After 35 cases, handheld navigation demonstrated lower deviation from planned anteversion (2.0° vs 5.8°) and inclination (1.3° vs 5.4°), lower LLD (1.0 vs 3.4 mm) and offset (1.4 vs 6.1 mm), fewer ≥ 10° outliers for version (0% vs 20%) and inclination (0% vs 15%), and reduced radiation time and dose (dose: 0.6 vs 2.1 mGy; time: 5.3 vs 19.1 s) compared to fluoroscopically guided THA.
Discussion
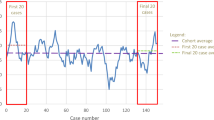
Given the variety of CN-THA platforms available and the differing approaches used to evaluate learning curves in the literature, this review aimed to identify patterns in characterizing and evaluating the learning curve. Our analysis of CN-THA demonstrated increased operative times compared to M-THA (3–20 min), though several studies showed improvements could me made over the initial caseload. Additionally, several studies demonstrated a learning curve for component placement accuracy and radiographic outcomes for CN-THA; however, mixed methodologies to analyzing the curve made the exact case number to achieve proficiency unclear. These findings underscore the value of a rigorous, standardized approach to the analysis of surgical learning curves, such as CUSUM analysis, and mitigate concerns for compromised patient outcomes in adopting CN-THA.
Temporal assessment of the CN-THA learning curve
Several studies investigating the learning curve for CN-THA similarly chose to track the progress of the surgeon over their initial series of navigated procedures. However, CUSUM analysis was not utilized, which may reflect the CN-THA studies having been conducted before CUSUM was popularized. Most studies instead employed a predetermined case number in the series to compare early cases to later ones. The case number chosen to delineate early from later cases was left to the authors’ discretion and varied greatly, between 20 and 50 cases. There were mixed findings regarding the case number required to achieve peak component placement accuracy, which may be a reflection of the limited accuracy of the approach used to analyze the curve as well the fact that different navigation platforms were used. While these studies aimed at estimating an inflection, CUSUM analysis was able to provide an exact case number based on the metric analyzed. Thus, a more standardized approach to the analysis of surgical learning curves in future investigations may allow for more accurate information on the learning process involved with THA technologies and enable direct comparison of available platforms.
Comparative assessment of the CN-THA learning curve
The use of CN-THA also demonstrated immediate advantages in acetabular component placement accuracy but came with an increased operative time as compared to M-THA. Kolodychuk et al. [23] compared CN-THA to fluoroscopically guided THA and demonstrated that while handheld navigation offered immediate advantages in component inclination accuracy, operative time was initially longer. However, after 35 cases, there was no difference in operative time between approaches and CN-THA began to demonstrate additional advantages, including markedly lower LLD, offset, and radiation time and dose, as well as further improvements in component placement accuracy. Therefore, while CN-THA provides immediate advantages in component placement accuracy and radiographic outcomes, these advantages become more pronounced as experience is acquired. While CUSUM has typically been used to analyze operative time as the outcome of interest, future analyses using alternative outcomes, such as placement accuracy, LLD, offset, and functional outcomes, can provide a clearer understanding of the learning curve required to achieve peak proficiency in CN-THA.
Limitations
This study had its limitations, many of which resulted from heterogeneity between studies, including the methodologies used to assess the learning curve, navigation platforms, implants, and surgical approaches used, and the statistical analysis of outcomes. As a quantitative synthesis of the evidence was infeasible, and the authors conducted a narrative analysis instead. Additionally, this heterogeneity also prevented direct comparisons between the CN-THA platforms assessed. Furthermore, as the analysis was compromised of observational cohort studies, there is a greater risk of bias in the included studies. Similarly, the intrinsic mean error of each CN-THA platform differs and impacts the overall final placement accuracy of the system, therefore influencing results. Also, none of the included studies assessed complications during the learning curve of CN-THA compared to M-THA, which is a key factor to consider when deciding whether to adopt CN-THA.
Conclusion
Compared to M-THA, CN-THA offers immediate advantages for implant placement accuracy, and LLD and offset radiographic outcomes. To attain the full extent of these advantages, there is a modest learning curve to achieve peak placement accuracy and radiographic outcomes with CN-THA. Surgeons should expect to experience increased operative times, though marked improvements can be made over a modest caseload. A standardized approach to reporting learning curves, such as CUSUM analysis, can allow for more robust assessment of learning curves associated with various platforms and outcomes of interest. Additional investigation into the complication profile associated with the learning curve of CN-THA is merited to evaluate both the benefits and potential drawbacks of utilizing these intraoperative technologies more fully.
Data availability
No datasets were generated or analysed during the current study.
References
Del Schutte H Jr, LipmanBannar AJSM, Livermore JT, Ilstrup D, Morrey BF (1998) Effects of acetabular abduction on cup wear rates in total hip arthroplasty. J Arthroplast 13:621–626. https://doi.org/10.1016/S0883-5403(98)80003-X
Jolles BM, Zangger P, Leyvraz PF (2002) Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. J Arthroplast 17:282–288. https://doi.org/10.1054/arth.2002.30286
D’Lima DD, Urquhart AG, Buehler KO, Walker RH, Colwell CW Jr (2000) The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios. J Bone Joint Surg Am 82:315–321. https://doi.org/10.2106/00004623-200003000-00003
Lu Y, Xiao H, Xue F (2019) Causes of and treatment options for dislocation following total hip arthroplasty. Exp Ther Med 18:1715. https://doi.org/10.3892/ETM.2019.7733
Sarin VK, Pratt WR, Bradley GW (2005) Accurate femur repositioning is critical during intraoperative total hip arthroplasty length and offset assessment. J Arthroplast 20:887–891. https://doi.org/10.1016/J.ARTH.2004.07.001
Guo XZ, Dou BX, Liu Q, Huang Y, Zhou Y (2007) Comparison of the acetabular orientation after minimally-invasive total hip arthroplasty with and without computer-navigation: a clinical report of 106 hip in 87 patients. Nat Med J Chin 87:2489–2493. https://doi.org/10.3760/j.issn:0376-2491.2007.35.011
Leenders T, Vandevelde D, Mahieu G, Nuyts R (2002) Reduction in variability of acetabular cup abduction using computer assisted surgery: a prospective and randomized study. Comput Aided Surg 7:99–106. https://doi.org/10.1002/IGS.10033
Sharma AK, Cizmic Z, Carroll KM, Jerabek SA, Paprosky WG, Sculco PK, Gonzalez Della Valle A, Schwarzkopf R, Mayman DJ, Vigdorchik JM (2022) Computer navigation for revision total hip arthroplasty reduces dislocation rates. Ind J Orthop 56:1061–1065. https://doi.org/10.1007/s43465-022-00606-7
Digioia AM 3rd, Jaramaz B, Plakseychuk AY, Moody JE Jr, Nikou C, Labarca RS, Levison TJ, Picard F (2002) Comparison of a mechanical acetabular alignment guide with computer placement of the socket. J Arthroplast 17:359–364. https://doi.org/10.1054/arth.2002.30411
Kolodychuk N, Su E, Alexiades MM, Ren R, Ojard C, Waddell BS (2021) Can robotic technology mitigate the learning curve of total hip arthroplasty? Bone Jt Open 2:365–370. https://doi.org/10.1302/2633-1462.26.BJO-2021-0042.R1
Kamara E, Robinson J, Bas MA, Rodriguez JA, Hepinstall MS (2017) Adoption of robotic vs fluoroscopic guidance in total hip arthroplasty: is acetabular positioning improved in the learning curve? J Arthroplast 32:125–130. https://doi.org/10.1016/j.arth.2016.06.039
Buchan GBJ, Hecht CJ 2nd, Lawrie CM, Sculco PK, Kamath AF (2023) The learning curve for a novel, fluoroscopy-based robotic-assisted total hip arthroplasty system. Int J Med Robot 19:e2518. https://doi.org/10.1002/RCS.2518
Kayani B, Konan S, Huq SS, Ibrahim MS, Ayuob A, Haddad FS (2021) The learning curve of robotic-arm assisted acetabular cup positioning during total hip arthroplasty. Hip Int 31:311–319. https://doi.org/10.1177/1120700019889334
Pernar LIM, Robertson FC, Tavakkoli A, Sheu EG, Brooks DC, Smink DS (2017) An appraisal of the learning curve in robotic general surgery. Surg Endosc 31:4583–4596. https://doi.org/10.1007/s00464-017-5520-2
Soomro NA, Hashimoto DA, Porteous AJ, Ridley CJA, Marsh WJ, Ditto R, Roy S (2020) Systematic review of learning curves in robot-assisted surgery. BJS Open 4:27–44. https://doi.org/10.1002/BJS5.50235
Mazzon G, Sridhar A, Busuttil G, Thompson J, Nathan S, Briggs T, Kelly J, Shaw G (2017) Learning curves for robotic surgery: a review of the recent literature. Curr Urol Rep. https://doi.org/10.1007/s11934-017-0738-z
Arora KS, Khan N, Abboudi H, Khan MS, Dasgupta P, Ahmed K (2015) Learning curves for cardiothoracic and vascular surgical procedures—a systematic review. Postgrad Med 127:202–214. https://doi.org/10.1080/00325481.2014.996113
Khan N, Abboudi H, Khan MS, Dasgupta P, Ahmed K (2014) Measuring the surgical “learning curve”: methods, variables and competency. BJU Int 113:504–508. https://doi.org/10.1111/BJU.12197
Shlobin NA, Huang J, Wu C (2022) Learning curves in robotic neurosurgery: a systematic review. Neurosurg Rev 46:14. https://doi.org/10.1007/S10143-022-01908-Y
Luft HS, Bunker JP, Enthoven AC (1979) Should operations be regionalized? the empirical relation between surgical volume and mortality. N Engl J Med 301:1364–1369. https://doi.org/10.1056/NEJM197912203012503
Inori F, Ohashi H, Yo H, Okajima Y, Matsui Y, Shintani K (2012) Accuracy of cup height and medialization in THA for dysplastic hip osteoarthritis using an imageless navigation system. Orthopedics 35:7–12. https://doi.org/10.3928/01477447-20120919-50
Gofton W, Dubrowski A, Tabloie F, Backstein D (2007) The effect of computer navigation on trainee learning of surgical skills. J Bone Joint Surg Am 89:2819–2827. https://doi.org/10.2106/JBJS.F.01502
Kolodychuk NL, Raszewski JA, Gladnick BP, Kitziger KJ, Peters PC, Waddell BS (2022) Handheld navigation improves accuracy in direct anterior total hip replacement. Arthroplast Today 17:58–65. https://doi.org/10.1016/J.ARTD.2022.06.016
Christ A, Ponzio D, Pitta M, Carroll K, Muir JM, Sculco PK (2018) Minimal increase in total hip arthroplasty surgical procedural time with the use of a novel surgical navigation tool. Open Orthop J 12:389–395. https://doi.org/10.2174/1874325001812010389
Thorey F, Klages P, Lerch M, Floerkemeier T, Windhagen H, von Lewinski G (2009) Cup positioning in primary total hip arthroplasty using an imageless navigation device: is there a learning curve? Orthopedics 32:14–17. https://doi.org/10.3928/01477447-20090915-52
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73:712–716. https://doi.org/10.1046/J.1445-2197.2003.02748.X
Kamenaga T, Hayashi S, Hashimoto S, Matsumoto T, Takayama K, Fujishiro T, Hiranaka T, Niikura T, Kuroda R (2019) Accuracy of cup orientation and learning curve of the accelerometer-based portable navigation system for total hip arthroplasty in the supine position. J Orthop Surg 27:2. https://doi.org/10.1177/2309499019848871
Wixson RL, MacDonald MA (2005) Total hip arthroplasty through a minimal posterior approach using imageless computer-assisted hip navigation. J Arthroplast 20:51–56. https://doi.org/10.1016/J.ARTH.2005.04.024
Najarian BC, Kilgore JE, Markel DC (2009) Evaluation of component positioning in primary total hip arthroplasty using an imageless navigation device compared with traditional methods. J Arthroplast 24:15–21. https://doi.org/10.1016/J.ARTH.2008.01.004
Suhardi VJ, Chiu fen Y, Sculco PK, Gonzalez Della Valle A (2021) Accuracy of acetabular cup placement positively correlates with level of training. Int Orthop 45:2797–2804. https://doi.org/10.1007/S00264-021-05165-4
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
CJH, JRP, and PAS were involved in conceptualization, methodology, formal analysis, visualization, writing original draft, and writing review and editing. YH, PKS, and AFK were involved in conceptualization, methodology, project administration, formal analysis, visualization, writing original draft, writing review and editing, and supervision.
Corresponding author
Ethics declarations
Competing interests
A.F.K. reports the following disclosures: paid presenter or speaker (Zimmer Biomet), paid consultant (Zimmer Biomet, BodyCad, Ortho Development, United Ortho), stock or stock options (Zimmer Biomet, Johnson & Johnson, and Procter & Gamble), IP royalties (Innomed), and board or committee member (AAOS, AAHKS, and Anterior Hip Foundation). Y.H. reports the following disclosures: paid presenter or speaker (Zimmer Biomet Japan, B.Braun Aesculap, Smith and Nephew), paid consultant (Zimmer Biomet Japan, Kyocera, and Teijin Nakashima Medical). P.K.S. reports the following disclosures: research support (Intelijoint Surgical), paid presenter of speaker (Intelijoint Surgical, DePuy, EOS Imaging), paid consultant (Intelijoint Surgical, Zimmer Biomet, DePuy, EOS Imaging, Lima Corporate), and stock or stock options (Intelijoint Surgical, Parvizi Surgical Innovation). CJH, JRP, and PAS have no disclosures.
Ethical approval
This study was deemed exempt from review by the Cleveland Clinic Foundation ethical review board due to all included data being publicly available and the lacking any protected health information.
Conflict of interest
A.F.K. reports the following disclosures: paid presenter or speaker (Zimmer Biomet), paid consultant (Zimmer Biomet, BodyCad, Ortho Development, United Ortho), stock or stock options (Zimmer Biomet, Johnson & Johnson, and Procter & Gamble), IP royalties (Innomed), and board or committee member (AAOS, AAHKS, and Anterior Hip Foundation). Y.H. reports the following disclosures: paid presenter or speaker (Zimmer Biomet Japan, B.Braun Aesculap, Smith and Nephew), paid consultant (Zimmer Biomet Japan, Kyocera, and Teijin Nakashima Medical). P.K.S. reports the following disclosures: research support (Intellijoint Surgical), paid presenter of speaker (Intellijoint Surgical, DePuy, EOS Imaging), paid consultant (Intellijoint Surgical, Zimmer Biomet, DePuy, EOS Imaging, Lima Corporate), and stock or stock options (Intellijoint Surgical, Parvizi Surgical Innovation). CJH, JRP, and PAS have no disclosures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hecht II, C.J., Porto, J.R., Sanghvi, P.A. et al. Navigating the learning curve: assessing caseload and comparing outcomes before and after the learning curve of computer-navigated total hip arthroplasty. J Robotic Surg 18, 104 (2024). https://doi.org/10.1007/s11701-024-01855-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11701-024-01855-4