Abstract
Asthma exacerbations are a leading cause of emergency department (ED) visits in children. Outdoor exposures such as air pollutants and meteorological factors have been associated with risk of asthma exacerbations. We evaluated the association between ambient temperature, relative humidity, and air quality on pediatric asthma-related ED visits in Montréal, Canada. In this retrospective study, we included children ≤ 17 years presenting with asthma to two pediatric EDs between January 1, 2017 and December 31st, 2020. Temperature and relative humidity data were obtained daily for Montréal through Weather Source™ and the Air Quality Health Index (AQHI) through Environment Canada. We evaluated the association between environmental exposures and the incidence of asthma-related ED visits using a quasi-Poisson regression analysis, adjusting for seasonality. We examined 21 201 asthma-related ED visits. Increased temperature was associated with an increased number of asthma-related ED visits. Compared to the reference decile (2.8 to 7.5⁰C), the strongest association with incident ED visits was for a temperature of 15.8 to 19.3⁰C, associated with a 37% increase in the number of asthma-related ED visits (IRR = 1.37, 95% CI 1.22, 1.54). Current day relative humidity, AQHI, and changes of the exposure levels over the previous 1 to 7 days did not have an effect on asthma-related ED visits. Adjusting for seasonality, higher temperatures were associated with an increased number of asthma-related ED visits among children while humidity and air quality were not. At a population level, this can inform hospitals of upcoming trends in ED visits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Asthma exacerbation is a leading cause of emergency department (ED) visits and hospitalizations in children(Canadian Institute for Health Information 2024), with approximately 10% of Canadian children with asthma having at least one asthma-related ED visit in the previous 2 years(Guttmann et al. 2007). In addition to patient-related factors, outdoor environmental exposures such as air pollutants and meteorological factors have been associated with increased risk of asthma-related ED visits or hospitalizations (Kanchongkittiphon et al. 2015; Trasande and Thurston 2005).
Studies reported divergent association between meteorological factors (temperature, humidity, and barometric pressure changes) and asthma exacerbations. Studies from China documented that lower temperatures (Zhang et al. 2020; Zhu et al. 2022) and higher barometric pressure (Zhang et al. 2020) were associated with asthma outpatient hospital visits. Conversely, a study from Pennsylvania documented that higher temperatures from June to August were associated with asthma-related ED visits in children(Schinasi et al. 2022). In Montreal (Québec, Canada) a weak and negative correlation was found between temperature and asthma-related hospitalizations during the 2006–2008 period(Robichaud and Comtois 2019). The heterogeneity of these findings suggests that study findings may be climate- and period-specific, likely because of the contribution of other factors such as aeroallergens and air pollution. Thus, region-specific studies are needed to better understand the local public health implication of these exposures.
Increased levels of particulate matter with a diameter of ≤ 2.5 μm (PM2.5) and ozone (O3) have been associated with a higher risk of asthma ED visits and hospitalizations(Gleason et al. 2014; Goodman et al. 2017). In a recent meta-analysis of 48 studies, Zheng et al. identified a consistent positive association between O3 levels and asthma ED visits and/or hospitalizations(Zheng et al. 2021). However, there was a high degree of heterogeneity between studies, including how the exposures were assessed (e.g. over which timeframe) and the mean levels of pollutants, which was dependent on the study location. Although the effect sizes of these associations were modest, the direction of these associations remains consistent across studies. Mechanistically, there is substantial evidence that fine particles and gaseous components can produce airway inflammation through oxidative stress (Landrigan et al., 2018) and decrease the airway hyperresponsiveness threshold. Furthermore, children are particularly susceptible to the negative effects of pollutants due to their smaller and developing airways, immature and developing immune systems, higher breathing rate, among other factors (Aithal et al. 2023; Biagioni et al. 2023).
Changes in ambient exposures can lead to worsening of asthma symptoms. Specifically, changes in weather, particularly extreme weather events, is a common trigger of asthma(Global Initiative for Asthma 2023; Makrufardi et al. 2023). However, few studies have examined the effect of changes in environmental factors on the incidence of pediatric asthma exacerbations. In a single center study in Michigan, Mireku et al. found that fluctuations in humidity and temperature are associated with increased asthma-related ED visits over a period of 1 to 2 days(Mireku et al. 2009). Whether this is applicable to other regions is unknown.
In this study, we examined the association between environmental exposures and asthma-related ED visits in children 1–17 years old presenting to two pediatric EDs in Montreal, Canada from 2017 to 2020. Specifically, we examined the current day effects of temperature, humidity, and air quality and their changes over the 7 previous days on asthma-related ED visits.
Materials and methods
Study design
We conducted a retrospective study of the databases of the two urban pediatric tertiary care EDs in Montreal, Canada (Sainte-Justine Hospital University Center (CHUSJ) and the Montreal Children’s Hospital (MCH), which have 60 000 to 80 000 annual visits each. We retrieved data from January 1, 2017 until December 31st, 2020. This study was approved by the research ethics boards of both institutions (project number MP-21-2023-4372, approved on May 17, 2021). Subject consent was deemed not necessary because of the retrospective design using only medical records. This report follows the Strengthening the Reporting of Observational Studies in Epidemiology Statement (STROBE)(STROBE 2024).
Participants
We included all children aged 1 to 17 years inclusively with an asthma-related ED visit, defined as an ED visit with a primary discharge diagnosis of asthma or bronchospasm or with an ICD-10-CA code J45 or ICD-9 code 493.XX. These ICD codes have been validated and widely used in other asthma studies and both the principal diagnosis and ICD codes have been validated for identifying acute asthma exacerbations using administrative data (Sundaresan et al. 2018). We excluded children who left the ED before being assessed by a physician as they did not have a discharge diagnosis. Given that we had environmental data for a large geographical around Montreal and that this area represents the catchment area of the two hospitals, we did not exclude subjects based on residential postal code.
Measurement of the outcome
The outcome of interest was the daily number of asthma-related ED visits during the study period. Data was retrieved from the electronic databases of the two participating EDs. Missing information (n < 150 entries) was retrieved manually from the patients’ electronic medical records by a member of the research team.
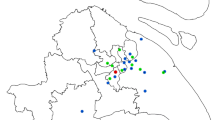
Measurement of exposures
Historical daily data for temperature (in degrees Celsius) and relative humidity were obtained from Weather Source(Weathersource 2024), which generates local data based on 203 virtual weather station by pulling in weather sensing inputs such as radar, satellite, and airport observation station data. For each exposure measure, the daily average was calculated over the 203 Weather Source OnPoint Grid Points in the Greater Montréal area, which encompasses the catchment area for the two pediatric hospitals in this study (Fig. 1). Missing temperature and humidity data were observed for < 1% (1 day). The Air Quality Health Index (AQHI) for Montréal, Québec, Canada during the study period (available from April 1st, 2017 onward) was obtained from Environment Canada(Government of Canada 2022). Specifically, for Montréal, the AQHI data is sourced from Quebec’s Info-Smog program(Government of Canada 2018). The AQHI is calculated using 3 pollutants (NO2, O3, and PM2.5) and presented on a 10 + point scale. This composite parameter is a standard measure used locally to represent air quality and serves as a guide to the health risk presented by common air pollutants, with the higher number associated with a greater health risk (1–3: low risk; 4–6: moderate risk; 7–10: high risk; >10: very high risk).
Statistical analyses
We performed a descriptive analysis of the patient characteristics, the monthly number of asthma-related ED visits, and environmental exposures. Given the non-normal distribution of the exposures, we normalized each exposure into deciles for analytic purposes. For each exposure, the reference decile was the one that contained the mean value of that exposure over the study period. We conducted a quasi-Poisson time series regression analysis to analyze the association between the exposure and asthma-related ED visits with adjustment for seasonality and long-term patterns by utilizing flexible spline functions. This adjustment accounts for the seasonal variability and trends in asthma-related ED visits, thus allowing the analyses to better evaluate the underlying relationship between environmental exposures on the outcome. Specifically, the quasi-Poisson family was employed to address overdispersion and the spline specification involved the implementation of a cubic B-spline with a total of 28 degrees of freedom (7 per calendar year). The B-spline basis functions were generated using the function “bs” from the package “splines”. Analyses were performed in R (version 4.2.3).
Given that asthma exacerbations can be triggered by changes in exposures, we also analysed the effect of a change in the exposure variable over the 1 to 7 days prior to the day when asthma-related ED visits were assessed. Specifically, we calculated the difference between the current day’s mean level of exposure and the previous days’ mean level of exposure and assessed the impact of this difference on the current day’s number of asthma-related ED visits, and this, for the entire study period.
Results
Description of the study population and exposures
From January 1st, 2017 to December 31st, 2020, there were a total of 21 201 asthma-related ED visits at the two hospitals. The median age of these children was 2.7 years (interquartile range (IQR) 1.7, 5.0) and the majority were boys (13 279, 62.6%) (Table 1). As shown in Fig. 2, asthma-related ED visits demonstrated seasonal variations, consistent with the well-described biannual peak of asthma exacerbations in the fall and spring. An exception occurred during the COVID-19 pandemic, when there were fewer exacerbations, especially at the beginning of the pandemic (April to June 2020).
During the study period, the daily median (IQR) temperature was 7.5⁰C (-1.6, 17.6) with a range of -23.5⁰C to 28.8⁰C. Notably, the first decile for temperature ranged from −23.5⁰C to -9.0⁰C and the last decile ranged from 22.0⁰C to 28.8⁰C. This suggests that there were no extreme cold (not accounting for windchill) or extreme heat weather for extended periods. The median (IQR) relative humidity was 73.0% (65.0, 81.0) with a range of 27.0 to 98.0%. The median (IQR) AQHI was 2.3 (1.9, 2.7), which was in the low risk level, with a range of 1.1 to 5.2 (up to a moderate health risk).
Association between environmental exposures and asthma-related ED visits
Adjusting for seasonality and long-term trends, increased temperature was associated with an increased number of asthma-related ED visits. In general, higher temperature deciles were associated with higher incidence rate ratios of ED visits (Fig. 3a). For example, with the decile from 2.8 to 7.5 ⁰C as a reference, a temperature of 15.8 to 19.3⁰C was associated with a 37% increase in the number of asthma-related ED visits (IRR = 1.37, 95% CI 1.22, 1.54). Changes in temperatures over the previous 1 to 7 days did not have a statistically significant effect on asthma-related ED visits (Supplemental Fig. 1a).
Relative humidity and changes in relative humidity over the previous 1 to 7 days were generally not associated with asthma-related ED visits (Fig. 3b and Supplemental Fig. 1b). Compared to the decile from 70.3 to 73.1% relative humidity, a relative humidity of 73.1 to 76.3% was associated with a 10% increase in asthma-related ED visits (IRR = 1.10, 95% CI 1.02, 1.18). However, higher humidity deciles (i.e. over 76.3%) were not associated with increased ED visits. Similarly, AQHI and changes in AQHI over the previous 1 to 7 days were not statistically significantly associated with asthma-related ED visits (Fig. 3c and Supplemental Fig. 1c).
Discussion
Using data on over 21 000 asthma-related ED visits over a period of 4 years from Montreal, Canada, we found that while adjusting for seasonality and long-term trends, increasing temperature was associated with increased numbers of asthma-related ED visits. While the effect sizes are small, they are consistent with studies on the impact of environmental factors on health and may still have a large impact from a population perspective(Verbeek et al. 2021). Current day relative humidity and air quality did not have an effect on asthma-related ED visits. Additionally, the changes of these exposure levels over the previous 1 to 7 days did not have an effect on asthma-related ED visits.
While temperature and humidity are well documented triggers for asthma exacerbations at the individual level, the threshold at which they can trigger asthma symptoms varies from one patient to another. Some individuals are sensitive to high heat and humidity while others are more sensitive to cold and dry air. These ambient factors can induce bronchoconstriction through the cholinergic reflex pathway and thermosensitive sensory nerves in the airways(Hayes et al. 2012). At a population level, previous studies have reported conflicting findings on the association between ambient temperature and asthma-related ED visits in children, with some studies reporting a positive association (Mireku et al. 2009) while others reported a negative association(Zhang et al. 2020). Corroborating with our findings, a study in Michigan, United States, documented that a 10⁰F increase in temperature over 24 h was associated with 1.8 additional asthma-related ED visits in children over a mean of 35 asthma-related visits per day (Mireku et al. 2009). We found one comparable study examining these exposures in Montreal, Canada. This study, performed over the 2006–2008 period, found that warm fronts were associated with higher asthma-related hospitalisations (Robichaud and Comtois 2019). However, when isolating the effect of temperature on asthma-related hospitalisations, the authors found a weak but statistically significant, negative correlation between the two variables (Pearson’s coefficient of -0.12). The seemingly discrepant results with our findings may be due to differing methodology, as their study was restricted to the spring season and included both adult and pediatric asthma-related hospitalisations in limited numbers (total n = 609). Interestingly, in our study, the positive association was seen even with temperatures that are not considered extreme heat events. In the face of climate change, increasing global temperatures, among other changes in exposures, could translate into increasing numbers of childhood asthma exacerbations. While we adjusted for seasonality in our model, it is possible that the temperatures affect pollen load, which may in turn disproportionately affect some children with environmental allergies. We attempted to mitigate this issue by adjusting for seasonality as we did not have data on personal allergies.
Our findings may seem unintuitive as there are normally more asthma-related ED visits during winter, when temperatures are colder. However, it is important to note that by adjusting for seasonality and long-term trends, we examined only the association between temperature and asthma-related ED visits. Thus, it is likely that during winter, other factors (e.g. increased incidence and transmission of respiratory infections) contribute to the higher incidence of asthma-related ED visits, with temperature having a smaller effect.
Studies have examined the effect of different lag times in temperature on asthma-related events. Mireku et al. found that the change in temperature over the 24 h preceding was associated with asthma-related ED visits, but not further lags in time. Zhang et al. documented the lag effects of exposures for up to 10 days prior to the asthma exacerbation and found significant lag effects for temperature (lag day 5), wind speed (lag day 5), humidity (lag day 9), and air quality index (lag day 2)(Zhang et al. 2020). However, the relative risk remained very small (RR < 1.05).
Outdoor pollution can be a trigger for asthma exacerbations in children(Global Initiative for Asthma 2023). Air pollutants can promote oxidative stress and induce inflammatory responses in the airways, leading to asthma symptoms (Dondi et al. 2023). Children may be particularly vulnerable given their developing lungs, higher breathing and metabolic rates, and spend more time outdoors(Committee on Environmental Health 2004). In Quebec, using population-based data, specific air pollutants (PM2.5, NO2, and SO2) have been associated with small but significant increases in childhood asthma onset rates(Liu et al. 2023). We did not find a statistically significant association between the AQHI and asthma-related ED visits. However, a trend for a weak but positive association can be observed in Fig. 3c. The lack of association in our study may be due to the relatively unpolluted air in Montreal overall and the lack of large variations in air quality. Specifically, the median AQHI was 2.3 (IQR 1.9, 2.7) over our study period, which is in the low risk zone. The maximum AQHI was 5.2, which represents a moderate health risk. Studies that have documented a positive association between air quality and asthma-related events were performed in locations with generally poorer air quality(Rosser et al. 2022; Zhang et al. 2020). In 2023, Montreal and the province of Quebec experienced periods of very poor air quality due to landscape fires, when the AQHI was 10+. Future studies could focus on these periods to evaluate the impact of unhealthy air quality indices associated with such extreme events.
Some limitations are noteworthy in our study. First, we did not capture all asthma-related ED visits in the greater Montreal area as we did not have access to smaller, non-pediatric-focused hospitals. However, given the pediatric oriented care, it is likely that the majority of patients in the study catchment area would have presented to one of the two pediatric EDs in Montreal. Furthermore, few walk-in clinics in Montreal offer acute management of asthma, particularly for children. This is reflected in the high number of asthma-related ED visits in our sample (average of 5300 asthma-related ED visits per study year). Second, we did not exclude patients based on their residential postal codes (who would not have been exposed to the environmental factors in Montreal), although this would have a been a small minority of patients. Third, we used the composite measure of AQHI to measure air quality, which is derived from O3, PM2.5/PM10, and NO2(Government of Canada 2022) and which was considered the same for the Montreal region. However, the air quality and specific pollutants can vary between neighborhoods within Montreal. Additionally, children may be more or less susceptible to environmental factors based on their comorbidities (e.g. environmental allergies). Such comorbidities are not routinely documented during acute ED visits and thus we did not have access to this data. Future studies should evaluate the association between neighborhood-specific exposures and personal comorbidities, and how these relate to risks of asthma exacerbations.
Conclusion
We found that in Montreal, Canada, higher temperatures were associated with an increased number of asthma-related ED visits among children while humidity and air quality were not, after adjusting for seasonality. At a population level, this can inform hospitals of increasing ED visits during the warmer seasons. Whether this is a significant trigger at the individual will depend on other personal factors, which should be further studied.
Data availability
The datasets analyzed during the current study are not publicly available due to individual privacy but are available from the corresponding author on reasonable request and with the participating sites’ institutional research ethics board’s approval.
References
Aithal SS, Sachdeva I, Kurmi OP (2023) Air quality and respiratory health in children. Breathe (Sheff) 19:230040. https://doi.org/10.1183/20734735.0040-2023
Biagioni B, Cecchi L, D’Amato G, Annesi-Maesano I (2023) Environmental influences on childhood asthma: climate change. Pediatr Allergy Immunol 34:e13961. https://doi.org/10.1111/pai.13961
Canadian Institute for Health Information (2024) Asthma hospital stays by children and youth
Committee on Environmental Health (2004) Ambient Air Pollution: Health hazards to Children. Pediatrics 114:1699–1707. https://doi.org/10.1542/peds.2004-2166
Dondi A, Carbone C, Manieri E, Zama D, Del Bono C, Betti L, Biagi C, Lanari M (2023) Outdoor Air Pollution and Childhood Respiratory Disease: the role of oxidative stress. Int J Mol Sci 24:4345. https://doi.org/10.3390/ijms24054345
Gleason JA, Bielory L, Fagliano JA (2014) Associations between ozone, PM2.5, and four pollen types on emergency department pediatric asthma events during the warm season in New Jersey: a case-crossover study. Environ Res 132:421–429. https://doi.org/10.1016/j.envres.2014.03.035
Global Initiative for Asthma (2023) 2023 GINA Main Report [WWW Document]. Global Initiative for Asthma - GINA. URL https://ginasthma.org/2023-gina-main-report/ (accessed 7.21.23).
Goodman JE, Loftus CT, Liu X, Zu K (2017) Impact of respiratory infections, outdoor pollen, and socioeconomic status on associations between air pollutants and pediatric asthma hospital admissions. PLoS ONE 12:e0180522. https://doi.org/10.1371/journal.pone.0180522
Government of Canada (2018) Info-Smog
Government of Canada (2022) Air Quality Health Index
Guttmann A, Zagorski B, Austin PC, Schull M, Razzaq A, To T, Anderson G (2007) Effectiveness of emergency department asthma management strategies on return visits in children: a population-based study. Pediatrics 120:e1402–1410. https://doi.org/10.1542/peds.2007-0168
Hayes D, Collins PB, Khosravi M, Lin R-L, Lee L-Y (2012) Bronchoconstriction triggered by Breathing Hot Humid Air in patients with asthma. Am J Respir Crit Care Med 185:1190–1196. https://doi.org/10.1164/rccm.201201-0088OC
Kanchongkittiphon W, Mendell MJ, Gaffin JM, Wang G, Phipatanakul W (2015) Indoor environmental exposures and exacerbation of asthma: an update to the 2000 review by the Institute of Medicine. Environ Health Perspect 123:6–20. https://doi.org/10.1289/ehp.1307922
Landrigan PJ, Fuller R, Acosta NJR, Adeyi O, Arnold R, Basu N (Nil), Baldé AB, Bertollini R, Bose-O’Reilly S, Boufford JI, Breysse PN, Chiles T, Mahidol C, Coll-Seck AM, Cropper ML, Fobil J, Fuster V, Greenstone M, Haines A, Hanrahan D, Hunter D, Khare M, Krupnick A, Lanphear B, Lohani B, Martin K, Mathiasen KV, McTeer MA, Murray CJL, Ndahimananjara JD, Perera F, Potočnik J, Preker AS, Ramesh J, Rockström J, Salinas C, Samson LD, Sandilya K, Sly PD, Smith KR, Steiner A, Stewart RB, Suk WA, van Schayck OCP, Yadama GN, Yumkella K, Zhong M (eds) (2018) The Lancet Commission on pollution and health. The Lancet 391, 462–512. https://doi.org/10.1016/S0140-6736(17)32345-0
Liu Y, Geng X, Smargiassi A, Fournier M, Gamage SM, Zalzal J, Yamanouchi S, Torbatian S, Minet L, Hatzopoulou M, Buteau S, Laouan-Sidi E-A, Liu L (2023) Changes in industrial air pollution and the onset of childhood asthma in Quebec, Canada. Environ Res 117831. https://doi.org/10.1016/j.envres.2023.117831
Makrufardi F, Manullang A, Rusmawatiningtyas D, Chung KF, Lin S-C, Chuang H-C (2023) Extreme weather and asthma: a systematic review and meta-analysis. Eur Respir Rev 32:230019. https://doi.org/10.1183/16000617.0019-2023
Mireku N, Wang Y, Ager J, Reddy RC, Baptist AP (2009) Changes in weather and the effects on pediatric asthma exacerbations. Ann Allergy Asthma Immunol 103:220–224. https://doi.org/10.1016/S1081-1206(10)60185-8
Robichaud A, Comtois P (2019) Environmental factors and asthma hospitalization in Montreal, Canada, during spring 2006–2008: a synergy perspective. Air Qual Atmos Health 12:1495–1509. https://doi.org/10.1007/s11869-019-00744-2
Rosser F, Han Y-Y, Rothenberger SD, Forno E, Mair C, Celedón JC (2022) Air Quality Index and Emergency Department Visits and hospitalizations for Childhood Asthma. Annals ATS 19:1139–1148. https://doi.org/10.1513/AnnalsATS.202105-539OC
Schinasi LH, Kenyon CC, Hubbard RA, Zhao Y, Maltenfort M, Melly SJ, Moore K, Forrest CB, Roux D, de Roos AV, A.J (2022) Associations between high ambient temperatures and asthma exacerbation among children in Philadelphia, PA: a time series analysis. Occup Environ Med 79:326–332. https://doi.org/10.1136/oemed-2021-107823
STROBE (2024) STROBE: strengthening the reporting of observational studies in epidemiology. [WWW Document]. STROBE. URL https://www.strobe-statement.org/ (accessed 1.16.24)
Sundaresan AS, Schneider G, Reynolds J, Kirchner HL (2018) Appl Clin Inf 9:528–540. https://doi.org/10.1055/s-0038-1666994. Identifying Asthma Exacerbation-Related Emergency Department Visit Using Electronic Medical Record and Claims Data
Trasande L, Thurston GD (2005) The role of air pollution in asthma and other pediatric morbidities. J Allergy Clin Immunol 115:689–699. https://doi.org/10.1016/j.jaci.2005.01.056
Verbeek J, Hoving J, Boschman J, Chong L-Y, Livingstone-Banks J, Bero L (2021) Systematic reviews should consider effects from both the Population and the individual perspective. Am J Public Health 111:820–825. https://doi.org/10.2105/AJPH.2020.306147
Weathersource (2024) OnPoint® API
Zhang H, Liu S, Chen Z, Zu B, Zhao Y (2020) Effects of variations in meteorological factors on daily hospital visits for asthma: a time-series study. Environ Res 182:109115. https://doi.org/10.1016/j.envres.2020.109115
Zheng X-Y, Orellano P, Lin H-L, Jiang M, Guan W-J (2021) Short-term exposure to ozone, nitrogen dioxide, and sulphur dioxide and emergency department visits and hospital admissions due to asthma: a systematic review and meta-analysis. Environ Int 150:106435. https://doi.org/10.1016/j.envint.2021.106435
Zhu Y, Yang T, Huang S, Li H, Lei L, Xue X, Gao Y, Jiang Y, Liu C, Kan H, Chen C (2022) Cold temperature and sudden temperature drop as novel risk factors of asthma exacerbation: a longitudinal study in 18 Chinese cities. The Science of the total environment 814 https://doi.org/10.1016/j.scitotenv.2021.151959
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Sze Man Tse: Conceptualization, methodology, supervision, writing (original draft), visualization, project administration. Sadio Sambahke: Data curation, formal analysis, writing (review and editing). Masoumeh Sajedi: Formal analysis, Jocelyn Gravel: Conceptualization, methodology, writing (review and editing). Esli Osmanlliu: Conceptualization, methodology, writing (review and editing).
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the research ethics boards of the Centre Hospitalier Universitaire Sainte-Justine and Montreal Children’s Hospital (project number MP-21-2023-4372, approved on May 17, 2021).
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tse, S.M., Sambahke, S., Sajedi, M. et al. Higher temperatures are associated with increased asthma-related emergency department visits among children: a time series analysis of environmental exposures in Montreal, Canada. Air Qual Atmos Health (2024). https://doi.org/10.1007/s11869-024-01610-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11869-024-01610-6