Abstract
Introduction
Insights into real-world treatment of atopic dermatitis (AD) are relevant to clinical decision making. The aim of this analysis was to characterize patients who receive dupilumab for AD in a real-world setting.
Methods
The GLOBOSTAD registry is an ongoing, longitudinal, prospective, observational study of patients with AD who receive dupilumab according to country-specific prescribing information. We report baseline characteristics, comorbidities and treatment patterns for patients enrolled from July 11, 2019 to March 31, 2022. Analyses are descriptive; no formal statistical comparisons were performed.
Results
Nine hundred fifty-two adults and adolescents were enrolled in GLOBOSTAD. Patients had a high disease burden before starting dupilumab: (mean [standard deviation]) percent body surface area affected (44.8 [24.42]), Eczema Area and Severity Index total score (24.8 [12.95]), SCORing Atopic Dermatitis total score (60.5 [16.34]), Patient-Oriented Eczema Measure total score (19.7 [6.37]) and Dermatology Life Quality Index total score (13.7 [7.02]). Overall, 741 (77.8%) patients reported ≥ 1 type 2 inflammatory comorbidities, most frequently allergic rhinitis (492 [51.7%]), asthma (323 [33.9%]), food allergy (294 [30.9%]) or another allergy (274 [28.8%]). In the previous 12 months, 310 (32.6%) patients had received systemic non-steroidal immunosuppressants and 169 (17.8%) systemic corticosteroids; 449 (47.2%) had received topical corticosteroids, most commonly potent topical corticosteroids; 141 (14.8%) had received topical calcineurin inhibitors and 32 (3.4%) ultraviolet therapy. Most (713 [74.9%]) patients started dupilumab because of prior treatment failure.
Conclusion
Patients enrolled in GLOBOSTAD demonstrated considerable multidimensional burden of disease across AD signs, symptoms and quality of life despite previous use of systemic and non-systemic AD treatments.
Clinical Trial Registration
ClinicalTrials.gov identifier NCT03992417.
Video Abstract
Similar content being viewed by others
Avoid common mistakes on your manuscript.

GLOBOSTAD is an ongoing, international, longitudinal, prospective, observational study of patients with atopic dermatitis (AD) who receive dupilumab according to country-specific prescribing information |
Patients enrolled in GLOBOSTAD in a real-world setting, and before treatment initiation with dupilumab, have demonstrated a considerable multidimensional burden of disease despite prior treatment with systemic and/or topical AD medications |
Digital Features
This article is published with digital features, including a video abstract, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.23925021.
Introduction
Atopic dermatitis (AD) is a complex, immune-mediated, chronic type 2 inflammatory skin condition which can have a significant impact on quality of life (QoL) [1, 2]. Often starting in childhood, AD can continue into adulthood but may also begin then [3, 4]. The prevalence of AD varies considerably in different countries and regions [5]. A 2020 systematic review estimated the 1-year prevalence of physician-diagnosed AD in adults ranged from 1.2% in Asia to 17.1% in Europe and from 0.96% to 22.6% in children in Asia [5].
AD pathogenesis is driven through upregulation of type 2 immune responses mediated by interleukins (IL)-4 and -13 [6,7,8]. Patients with AD are at increased risk of developing other inflammatory diseases driven by type 2 cytokines, such as allergic rhinitis, asthma or food allergies [9]. Furthermore, increased severity of AD is associated with an increased risk for comorbid type 2 inflammatory diseases, resulting in increased disease burden [10].
Dupilumab is a fully human VelocImmune®-derived [11, 12] monoclonal antibody that blocks the shared receptor component for IL-4 and IL-13, key and central drivers of type 2 inflammation in AD and other type 2 inflammatory diseases [8]. Dupilumab is approved for the treatment of multiple type 2 inflammatory diseases, including AD, asthma, chronic rhinosinusitis with nasal polyps, eosinophilic esophagitis (EoE) and prurigo nodularis [13, 14].
While several randomized, placebo-controlled, phase 3 trials have demonstrated the efficacy and acceptable safety profile of dupilumab in patients with moderate-to-severe AD [15,16,17], long-term data on patients receiving dupilumab for AD in real-world clinical practice are limited [18]. This paucity of data led us to design the GLOBOSTAD study (NCT03992417), which aims to inform clinician treatment choices by characterizing the patients who receive dupilumab for AD in a real-world setting with respect to their medical history, sociodemographic and disease characteristics, and prior and concomitant treatments for AD.
Here, we describe the baseline demographics and clinical characteristics, including disease severity, comorbidities, treatment history and patient-reported outcomes, before treatment initiation with dupilumab, of patients with AD who are enrolled in the GLOBOSTAD registry.
Methods
Study Design
The GLOBOSTAD registry (NCT03992417) is an ongoing, 5-year, international, longitudinal, prospective, observational study of adult and adolescent patients with AD who receive dupilumab according to country-specific prescribing information. Consecutive patients with AD at each study site who received an initial prescription for dupilumab were invited to participate. Analysis includes data from all patients who were eligible and consented to participate in the study from July 11, 2019, to March 31, 2022.
GLOBOSTAD is being conducted in accordance with the Declaration of Helsinki, the International Conference on Harmonisation Good Clinical Practice guideline and applicable regulatory requirements. All subsequent amendments and the protocol were reviewed and approved by institutional review boards before patient recruitment, and all patients provided written informed consent before participating in the study.
Patients
Eligible patients were aged ≥ 12 years at the baseline visit and initiated dupilumab according to country-specific prescribing information. Participants or their parents/legally acceptable representatives provided informed consent, and patients had to be willing to participate in regular follow-up visits and to respond to requests for long-term information within the required timeframe. Exclusion criteria included any contraindication for dupilumab, any condition that in the opinion of the investigator could interfere with the patient’s ability to participate (such as short life expectancy, substance abuse, severe cognitive impairment or other comorbidities that could prevent the patient from completing the schedule of visits and assessments) and prior use of dupilumab within 6 months of the screening visit or within 6 months of the baseline visit if screening and baseline occurred on the same day. However, patients were eligible for inclusion if they had already initiated treatment with dupilumab for AD within 6 months of their enrollment in the registry, provided that all core baseline data required by the registry protocol (i.e., percent body surface area [BSA] affected, Eczema Area and Severity Index [EASI] total score, SCORing Atopic Dermatitis [SCORAD] total score, Patient-Oriented Eczema Measure [POEM] and Dermatology Life Quality Index [DLQI] total score) had been captured at the time of initiating dupilumab treatment and were available for entry in the registry database.
Assessments
Patient data for the Registry are collected at baseline (the time of treatment initiation with dupilumab, whether prior to or on/after the screening visit), month 3 (± 1 month), month 6 (± 2 months) and every 6 months (± 2 months) thereafter until the end of the total 5-year observational period. Baseline assessments are performed on the day of the screening/baseline visit and include investigator collection of sociodemographics, personal and family history of AD and selected atopic diseases and comorbidities, and AD treatments prior to baseline; concomitant medications, and reasons for initiating dupilumab. Baseline scores for physician- and patient-reported outcome measures of disease severity and burden are also collected. Physician-rated AD assessments include the EASI total score (0–72) [19], SCORAD total score (0–103) [20] and percent BSA affected. Patients complete the following patient-reported outcome (PRO) measures: POEM (0–28) [21], DLQI total score (0–30) [22] and Pruritus, Skin Pain or Soreness, Skin Feeling Hot, Skin Sensitivity to Touch and Sleep Disturbance over the previous 7 days and numeric rating scales (NRS, 0–10) for each of these measures (higher scores represent more severe disease/symptoms).
Statistical Analysis
Baseline data for all patients were analyzed using descriptive statistics (i.e., no confirmatory hypotheses were tested) including means and standard deviations (continuous variables). For categorical or ordinal data, frequencies and percentages are reported. No imputation of missing data was performed.
Results
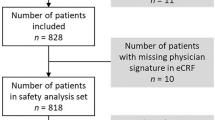
Of the 968 patients who underwent screening, 952 (98.3%) had initiated treatment with dupilumab and were included in this analysis. Among these, 725 (76.2%) had initiated dupilumab on or after screening, while 227 (23.8%) had initiated dupilumab prior to screening. Most patients were enrolled from Italy (17.2%), Japan (12.4%), Spain (11.3%) and France (9.7%) (Table 1).
Sociodemographics
The mean (standard deviation [SD]) age of patients enrolled in GLOBOSTAD was 35.5 (13.6) years, 57.8% of patients were male and 65.2% of patients were White. The mean age (SD) at AD onset was 11.1 (16.0) years and the mean duration (SD) of AD was 24.8 (14.9) years. Approximately half (50.4%) had a university/higher education and 63.6% were in full- or part-time employment (Table 1).
Clinical and Patient-Reported Burden of AD
Overall, the GLOBOSTAD population had severe AD at baseline, as reported by physician-assessed and PRO measures (Table 1). The mean (SD) percent BSA affected by AD was 44.8% (24.42), EASI total score was 24.8 (12.95) [23, 24], SCORAD total score was 60.5 (16.34), and POEM total score was 19.7 (6.37), each of which was in the severe range [23,24,25,26,27]. The mean (SD) DLQI total score was 13.7 (7.02) (i.e., a severe effect on QoL) [25, 26]. Mean (SD) NRS scores for individual skin symptoms were 6.3 (2.11) for Pruritus, 5.9 (2.69) for Skin Pain/Soreness, 5.4 (2.74) for Skin Feeling Hot and 6.2 (2.55) for Sensitivity to Touch NRS.
History of Type 2 Inflammatory and Other Comorbidities
Overall, 741 (77.8%) patients reported one or more type 2 inflammatory comorbidities, most frequently allergic rhinitis (492 [51.7%]), asthma (323 [33.9%]), food allergy (294 [30.9%]) or other allergies (274 [28.8%]). Other more commonly reported comorbidities included hypertension (82 [8.6%]), hypercholesterolemia (21 [2.2%]) and depression (26 [2.7%]) (Table 2).
Family History of AD and Selected Atopic Diseases
Overall, 364 (38.2%) patients had a family history of AD. A family history of other type 2 inflammatory conditions was prevalent, including asthma (238 [25%]), allergic rhinitis (219 [23%]), food allergies (74 [7.8%]), recurrent or chronic urticaria (31 [3.3%]), nasal polyposis (21 [2.2%]) and EoE (11 [1.2%]). Most cases of type 2 inflammatory conditions were reported in first-degree relatives (Fig. 1).
Prior Treatment for AD and Reasons for Dupilumab Initiation
Overall, 169 (17.8%) patients reported that they had used systemic corticosteroids, and 310 (32.6%) reported they had received non-steroidal systemic immunosuppressants during the 12 months prior to enrollment. The most commonly used non-steroidal systemic immunosuppressants were cyclosporine (248 [26.1%]) and methotrexate (66 [6.9%]). A few patients had received the IL-13 inhibitor tralokinumab (3 [0.3%]) and/or the Janus kinase inhibitors baricitinib (17 [1.8%]) and upadacitinib (10 [1.1%]), which have only recently become available (Table 3). The mean (SD) treatment durations for these agents were: tralokinumab 12.3 (9.1) months, baricitinib 19.2 (10.0) months and upadacitinib 15.3 (7.2) months.
In total, 449 (47.2%) patients reported that they had received topical corticosteroids, most commonly potent (393 [41.3%]) and very potent (103 [10.8%]) topical corticosteroids, and 141 (14.8%) patients had received topical calcineurin inhibitors. Only 32 (3.4%) patients had received ultraviolet/phototherapy in the 12 months prior to enrollment (Table 3).
Most patients (713 [74.9%]) were reported to have initiated dupilumab because of prior treatment failure. Other reasons provided for initiating dupilumab included disease exacerbation (153 [16.1%]) and use as maintenance treatment (84 [8.8%]) (Table 4).
Discussion
This analysis of baseline data from GLOBOSTAD reflects real-life practices in the treatment of moderate-to-severe AD according to country-specific prescribing information in 22 countries across Europe, Latin America, Asia and the Middle East.
Patients enrolling in the GLOBOSTAD registry, despite a high incidence of prior use of systemic therapies, have demonstrated significant burden of disease as evidenced by elevated baseline (pre-dupilumab) measures of AD severity and inadequate response to prior treatments. Most patients enrolled in GLOBOSTAD have severe AD, according to physician-assessed measures such as EASI total score and patient-reported measures such as POEM and Pruritus NRS. The baseline characteristics of patients enrolled in GLOBOSTAD are broadly consistent with other observational studies from North America, Europe and Japan [18, 28,29,30,31,32,33]. The ongoing PROSE registry enrolled patients with AD from the USA and Canada who were starting treatment with dupilumab according to country-specific prescribing protocols. An interim analysis of the first 15 months of the registry, which included 315 patients, reported a baseline mean EASI score in the moderate range, while POEM and DLQI leaned towards the severe range [27]. The ADDRESS-J registry enrolled Japanese patients with moderate-to-severe AD who had an Investigator’s Global Assessment (IGA) score > 3 and required treatment escalation. An interim analysis of the first 300 patients enrolled in that registry found that at baseline both physician-assessed and patient-reported measures pointed to a moderate disease burden [30]. The prospective, observational European-wide EUROSTAD registry, from ten countries, enrolled 308 patients with moderate-to-severe AD, who had either started a new systemic therapy or switched to another systemic therapy at baseline. The patient-reported burden of disease ranged from moderate to very severe, as assessed by POEM score, and > 50% of patients reported “very” or “extremely” high impairment of overall health-related QoL according to the DLQI, while physician-assessed EASI mean scores were within the “moderate” range [18]. The mean POEM and DLQI scores for patients at baseline in GLOBOSTAD were similar to those reported at baseline in the PROLEAD prospective, observational study that included 828 adult patients with moderate-to-severe AD [33].
Most (74.9%) patients in GLOBOSTAD initiated dupilumab treatment because of previous treatment failure, and 32.6% of patients had received a systemic immunosuppressant in the 12 months prior to study enrollment. The high clinical and patient-reported burden of AD in the GLOBOSTAD population, despite the use of systemic AD treatments, is consistent with findings from the EUROSTAD registry [30]. Despite receiving systemic AD treatments (patients must have initiated a new systemic AD therapy or switched to another systemic AD therapy on day 1 or within 30 days prior to enrollment), most of the EUROSTAD participants had moderate-to-severe AD, based on their baseline EASI and IGA scores [18].
The finding that most AD patients enrolled in GLOBOSTAD had concomitant type 2 inflammatory comorbidities at baseline also reflects findings from other AD registries, with most patients in the EUROSTAD, PROSE and ADDRESS-J registries reporting a history of one or more type 2 inflammatory comorbidities [18, 28, 30]. Dupilumab has been shown to confer clinical benefit across multiple type 2 comorbid conditions in patients with AD [34]. In a post hoc analysis of 2444 dupilumab-treated adults with comorbid moderate-to-severe AD, asthma and/or chronic sinonasal conditions (including allergic rhinitis/sinusitis, chronic rhinitis/sinusitis and nasal polyps), dupilumab treatment resulted in significant improvements in asthma control (Asthma Control Questionnaire-5 [ACQ-5]) and sinonasal symptoms (Sino-Nasal Outcome Test-22), in addition to AD signs and symptoms (EASI, DLQI and Peak Pruritus NRS) [34].
While most patients in the GLOBOSTAD registry reported having at least one type 2 inflammatory comorbidity (77.8%), other comorbidities were only reported by a small proportion of patients (35.5%). This finding may, in part, be attributed to the relatively young age of this patient population (mean age 35.5 years, with most patients in the 18–39 age group).
Overall, patients enrolled in GLOBOSTAD were representative of the real-world population with AD. Patients had a longstanding history of AD, with a mean 24.8 years since diagnosis. Approximately half (50.4%) had a university/higher education, and 63.6% were in full- or part-time employment.
This interim analysis of data from GLOBOSTAD expands on data from previous and ongoing studies and further characterizes patients who receive dupilumab for AD in the real-world clinical setting. The study includes adults and adolescents with AD initiating dupilumab treatment and reflects reimbursement practices according to country-specific prescribing information in 22 countries across the globe. Participating sites were selected to try to achieve a balance regarding geographic distribution, type of clinical setting (e.g., academic versus community health centers) and prescriber specialty, which could reasonably represent the larger patient and prescriber community, thereby favoring worldwide generalizability of the results. The collection of comprehensive baseline data permitted a thorough characterization of disease severity, including physician-assessed and PRO measures, type 2 comorbidities, family history of AD and AD treatment history. Future analyses of data from GLOBOSTAD will permit the longitudinal observation of the effectiveness and safety of dupilumab in adults and adolescents with AD, in the real-world setting. However, like any other prospective observational study, GLOBOSTAD may have attracted a more motivated patient population and physicians and centers that were willing to participate and provide study information (complete questionnaires, etc.). Furthermore, GLOBOSTAD patients were selected from among those who had access to dupilumab; therefore, they may not be fully representative of the wider AD population. Some countries required patients to meet certain criteria before dupilumab could be reimbursed (e.g., in Belgium, patients had to have an EASI score of > 21 or SCORAD score of > 50). Finally, some data were missing, as has been observed in many countries around the world with these types of studies and large numbers of patients.
Conclusion
Patients enrolled in GLOBOSTAD demonstrate a considerable, multidimensional burden of disease across AD signs, symptoms and QoL, despite treatment with topical and/or systemic AD medications. GLOBOSTAD will continue to follow patients for 5 years, providing a longitudinal contribution to the understanding of the course of AD and the impact of therapy on patient outcomes in the real-world setting.
Data Availability
Qualified researchers may request access to study documents (including the clinical study report, study protocol with any amendments, blank case report form, statistical analysis plan) that support the methods and findings reported in this manuscript. Individual anonymized participant data will be considered for sharing once the product and indication have been approved by major health authorities (e.g., FDA, EMA, PMDA, etc.), if there is legal authority to share the data and there is not a reasonable likelihood of participant re-identification. Submit requests to https://vivli.org/.
References
Birdi G, Cooke R, Knibb RC. Impact of atopic dermatitis on quality of life in adults: a systematic review and meta-analysis. Int J Dermatol. 2020;59(4):e75–91.
Eckert L, Gupta S, Amand C, Gadkari A, Mahajan P, Gelfand JM. Impact of atopic dermatitis on health-related quality of life and productivity in adults in the United States: An analysis using the National Health and Wellness Survey. J Am Acad Dermatol. 2017;77(2):274-9.e3.
Abuabara K, Yu AM, Okhovat JP, Allen IE, Langan SM. The prevalence of atopic dermatitis beyond childhood: A systematic review and meta-analysis of longitudinal studies. Allergy. 2018;73(3):696–704.
Garmhausen D, Hagemann T, Bieber T, et al. Characterization of different courses of atopic dermatitis in adolescent and adult patients. Allergy. 2013;68(4):498–506.
Bylund S, Kobyletzki LB, Svalstedt M, Svensson Å. Prevalence and incidence of atopic dermatitis: a systematic review. Acta Derm Venereol. 2020;100(12):adv00160.
Silverberg JI, Kantor R. The role of interleukins 4 and/or 13 in the pathophysiology and treatment of atopic dermatitis. Dermatol Clin. 2017;35(3):327–34.
Moyle M, Cevikbas F, Harden JL, Guttman-Yassky E. Understanding the immune landscape in atopic dermatitis: The era of biologics and emerging therapeutic approaches. Exp Dermatol. 2019;28(7):756–68.
Gandhi NA, Pirozzi G, Graham NMH. Commonality of the IL-4/IL-13 pathway in atopic diseases. Expert Rev Clin Immunol. 2017;13(5):425–37.
Shrestha S, Miao R, Wang L, Chao J, Yuce H, Wei W. Burden of atopic dermatitis in the United States: analysis of healthcare claims data in the commercial, Medicare, and medical databases. Adv Ther. 2017;34(8):1989–2006.
de Bruin-Weller M, Gadkari A, Auziere S, et al. The patient-reported disease burden in adults with atopic dermatitis: a cross-sectional study in Europe and Canada. J Eur Acad Dermatol Venereol. 2020;34(5):1026–36.
Macdonald LE, Karow M, Stevens S, et al. Precise and in situ genetic humanization of 6 Mb of mouse immunoglobulin genes. Proc Natl Acad Sci U S A. 2014;111(14):5147–52.
Murphy AJ, Macdonald LE, Stevens S, et al. Mice with megabase humanization of their immunoglobulin genes generate antibodies as efficiently as normal mice. Proc Natl Acad Sci U S A. 2014;111(14):5153–8.
Dupilumab Prescribing Information. https://www.regeneron.com/downloads/dupixent_fpi.pdf. Accessed 13 Nov 2022.
Dupixent Summary of Product Characteristics. https://www.ema.europa.eu/en/documents/product-information/dupixent-epar-product-information_en.pdf. Accessed 13 Nov 2022.
Blauvelt A, de Bruin-Weller M, Gooderham M, et al. Long-term management of moderate-to-severe atopic dermatitis with dupilumab and concomitant topical corticosteroids (LIBERTY AD CHRONOS): a 1-year, randomised, double-blinded, placebo-controlled, phase 3 trial. Lancet. 2017;389(10086):2287–303.
de Bruin-Weller M, Thaçi D, Smith CH, et al. Dupilumab with concomitant topical corticosteroid treatment in adults with atopic dermatitis with an inadequate response or intolerance to ciclosporin A or when this treatment is medically inadvisable: a placebo-controlled, randomized phase III clinical trial (LIBERTY AD CAFÉ). Br J Dermatol. 2018;178(5):1083–101.
Simpson EL, Bieber T, Guttman-Yassky E, et al. Two phase 3 trials of dupilumab versus placebo in atopic dermatitis. N Engl J Med. 2016;375(24):2335–48.
de Bruin-Weller M, Pink AE, Patrizi A, et al. Disease burden and treatment history among adults with atopic dermatitis receiving systemic therapy: baseline characteristics of participants on the EUROSTAD prospective observational study. J Dermatolog Treat. 2021;32(2):164–73.
Hanifin JM, Thurston M, Omoto M, Cherill R, Tofte SJ, Graeber M. The eczema area and severity index (EASI): assessment of reliability in atopic dermatitis. EASI Evaluator Group. Exp Dermatol. 2001;10(1):11–8.
Kunz B, Oranje AP, Labrèze L, Stalder JF, Ring J, Taïeb A. Clinical validation and guidelines for the SCORAD index: consensus report of the European Task Force on Atopic Dermatitis. Dermatology. 1997;195(1):10–9.
Charman CR, Venn AJ, Williams HC. The patient-oriented eczema measure: development and initial validation of a new tool for measuring atopic eczema severity from the patients’ perspective. Arch Dermatol. 2004;140(12):1513–9.
Badia X, Mascaró JM, Lozano R. Measuring health-related quality of life in patients with mild to moderate eczema and psoriasis: clinical validity, reliability and sensitivity to change of the DLQI. The Cavide Research Group. Br J Dermatol. 1999;141(4):698–702.
Chopra R, Vakharia PP, Sacotte R, et al. Severity strata for Eczema Area and Severity Index (EASI), modified EASI, Scoring Atopic Dermatitis (SCORAD), objective SCORAD, Atopic Dermatitis Severity Index and body surface area in adolescents and adults with atopic dermatitis. Br J Dermatol. 2017;177(5):1316–21.
Leshem YA, Hajar T, Hanifin JM, Simpson EL. What the Eczema Area and Severity Index score tells us about the severity of atopic dermatitis: an interpretability study. Br J Dermatol. 2015;172(5):1353–7.
Vakharia PP, Chopra R, Sacotte R, et al. Severity strata for five patient-reported outcomes in adults with atopic dermatitis. Br J Dermatol. 2018;178(4):925–30.
Silverberg JI, Gelfand JM, Margolis DJ, et al. Severity strata for POEM, PO-SCORAD, and DLQI in US adults with atopic dermatitis. Ann Allergy Asthma Immunol. 2018;121(4):464-68.e3.
Charman CR, Venn AJ, Ravenscroft JC, Williams HC. Translating Patient-Oriented Eczema Measure (POEM) scores into clinical practice by suggesting severity strata derived using anchor-based methods. Br J Dermatol. 2013;169(6):1326–32.
Bagel J, Nguyen TQ, Lima H, et al. Baseline demographics and severity and burden of atopic dermatitis in adult patients initiating dupilumab treatment in a real-world registry (PROSE). Dermatol Ther (Heidelb). 2022;12(6):1417–30.
Bosma AL, de Wijs LEM, Hof MH, et al. Long-term effectiveness and safety of treatment with dupilumab in patients with atopic dermatitis: Results of the TREAT NL (TREatment of ATopic eczema, the Netherlands) registry. J Am Acad Dermatol. 2020;83(5):1375–84.
Katoh N, Saeki H, Kataoka Y, et al. Atopic dermatitis disease registry in Japanese adult patients with moderate to severe atopic dermatitis (ADDRESS-J): Baseline characteristics, treatment history and disease burden. J Dermatol. 2019;46(4):290–300.
Siegels D, Haufe E, Heinrich L, Werfel T, Weidinger S, Schmitt J, TREATgermany Study Group. Status report on the atopic dermatitis registry TREATgermany. Allergol Select. 2021;5:274–86.
Spekhorst LS, Ariëns LFM, van der Schaft, et al. Two-year drug survival of dupilumab in a large cohort of difficult-to-treat adult atopic dermatitis patients compared to cyclosporine A and methotrexate: Results from the BioDay registry. Allergy. 2020;75(9):2376–9.
Thaçi D, Bauer A, von Kiedrowski R, et al. Dupilumab treatment of atopic dermatitis in routine clinical care: baseline characteristics of patients in the PROLEAD prospective, observational study. Dermatol Ther (Heidelb). 2022;12(9):2145–60.
Boguniewicz M, Beck LA, Sher L, et al. Dupilumab improves asthma and sinonasal outcomes in adults with moderate to severe atopic dermatitis. J Allergy Clin Immunol Pract. 2021;9(3):1212-23.e6.
Acknowledgements
The authors thank the participants of the study.
Medical Writing and Editorial Assistance.
These were provided by Amy O’Callaghan and Liselotte van Delden of Excerpta Medica, and funded by Sanofi and Regeneron Pharmaceuticals Inc., according to the Good Publication Practice guideline.
Funding
Open access funding provided by Università degli Studi di Brescia within the CRUI-CARE Agreement. This research was sponsored by Sanofi and Regeneron Pharmaceuticals Inc. ClinicalTrials.gov Identifier: NCT03992417. The study sponsors participated in the study design; collection, analysis and interpretation of the data; writing of the report; and the decision to submit the article for publication. The study sponsor funded the Rapid Service and Open Access fee.
Author information
Authors and Affiliations
Contributions
ZEO and MA contributed to the study concept and design, analysis and interpretation, provided critical feedback on the manuscript, approved the final manuscript for submission and were accountable for the accuracy and integrity of the manuscript. JW conducted the statistical analyses of the data. All other authors interpreted the data, provided critical feedback on the manuscript, approved the final manuscript for submission and were accountable for the accuracy and integrity of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Piergiacomo Calzavara-Pinton is an advisory board member for AbbVie, Almirall, Galderma, LEO Pharma, Meda and Sanofi. Jarmila Čelakovská has nothing to disclose. Hilde Lapeere is on the advisory boards of AbbVie, LEO Pharma, Eli Lilly, Pfizer and Sanofi. Gregor Holzer is an advisory board member for AbbVie, Almirall, Eli Lilly, Galderma, LEO Pharma and Sanofi. Mona Al-Ahmad is an advisory board member and speaker for AstraZeneca, GSK and Novartis. Chia-Yu Chu is an investigator for AbbVie, Dermira, Eli Lilly, Novartis, Oneness Biotech, Pfizer, Regeneron Pharmaceuticals Inc., Roche and Sanofi; a consultant for AbbVie, Eli Lilly, Novartis, Pfizer, Roche and Sanofi; a speaker for AbbVie, Eli Lilly, Mylan, Novartis, Pfizer, Roche, Sanofi and Viatris; and an advisory board member for Mylan, Pfizer, Roche and Sanofi. Silvia M. Ferrucci is an advisory board member for AbbVie, Eli Lilly and Sanofi; a Principal Investigator for Almirall, Menarini and Pfizer; and reports honoraria for lectures and research grants from Novartis. Yoko Kataoka reports lecturer honoraria from AbbVie, Pfizer and Sanofi; and research funding from AbbVie, Amgen, LEO Pharma, Lilly, Maruho, Otsuka, Pfizer, Sanofi and Taiho. Mariateresa Rossi is a speaker for AbbVie, Galderma, La Roche Posay, LEO Pharma, Pfizer and Sanofi. Daria S. Fomina reports honoraria from CSL Behring, Novartis, Sanofi and Shire. Wen-Hung Chung has nothing to disclose. Thrasyvoulos Tzellos has received honoraria from and is an advisory board member and speaker for AbbVie; and has received honoraria from and is an advisory board member for Boehringer Ingelheim and Sanofi. Anne-Claire Fougerousse is a consultant for AbbVie, Lilly and Sanofi. Jiangming Wu and Zafer E. Ozturk are employees of Sanofi and may hold stock and/or stock options in the company. Marius Ardeleanu is an employee and shareholder of Regeneron Pharmaceuticals Inc.
Ethical Approval
The GLOBOSTAD study is being conducted in accordance with the principles defined by the 18th World Medical Association General Assembly Declaration of Helsinki and all subsequent amendments. The study protocol was reviewed and approved by institutional review boards before patient recruitment. All patients provided written informed consent before any GLOBOSTAD procedures were initiated.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Calzavara-Pinton, P., Čelakovská, J., Lapeere, H. et al. Baseline Demographics, Comorbidities, Treatment Patterns and Burden of Atopic Dermatitis in Adults and Adolescents from the GLOBOSTAD Long-Term Observational Study. Adv Ther 40, 5366–5382 (2023). https://doi.org/10.1007/s12325-023-02644-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02644-5