Abstract
Introduction
The number of elderly patients who require surgery as their primary treatment has increased rapidly in recent years. Among 300 million people globally who underwent surgery every year, patients aged 65 years and over accounted for more than 30% of cases. Despite medical advances, older patients remain at higher risk of postoperative complications. Early diagnosis and effective prediction are essential requirements for preventing serious postoperative complications. In this study, we aim to provide new biomarker combinations to predict the incidence of postoperative intensive care unit (ICU) admissions > 24 h in elderly patients.
Methods
This investigation was conducted as a nested case–control study, incorporating 413 participants aged ≥ 65 years who underwent non-cardiac, non-urological elective surgeries. These individuals underwent a 30-day postoperative follow-up. Before surgery, peripheral venous blood was collected for analyzing serum creatinine (Scr), procalcitonin (PCT), C-reactive protein (CRP), and high-sensitivity CRP (hsCRP). The efficacy of these biomarkers in predicting postoperative complications was evaluated using receiver operating characteristic (ROC) curve analysis and area under the curve (AUC) values.
Results
Postoperatively, 10 patients (2.42%) required ICU admission. Regarding ICU admissions, the AUCs with 95% confidence intervals (CIs) for the biomarker combinations of Scr × PCT and Scr × CRP were 0.750 (0.655–0.845, P = 0.007) and 0.724 (0.567–0.882, P = 0.015), respectively. Furthermore, cardiovascular events were observed in 14 patients (3.39%). The AUC with a 95% CI for the combination of Scr × CRP in predicting cardiovascular events was 0.688 (0.560–0.817, P = 0.017).
Conclusion
The innovative combinations of biomarkers (Scr × PCT and Scr × CRP) demonstrated efficacy as predictors for postoperative ICU admissions in elderly patients. Additionally, the Scr × CRP also had a moderate predictive value for postoperative cardiovascular events.
Trial Registration
China Clinical Trial Registry, ChiCTR1900026223.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
As a result of an aging population, more and more elderly people need to undergo surgical treatment. Among the 300 million people who undergo surgery worldwide each year, over 30% are elderly people aged 65 and above. |
Compared to young people, these elderly individuals have a significantly higher risk of postoperative complications and even admission to the intensive care unit (ICU). Early identification and effective prediction are crucial for preventing serious postoperative complications. |
This study aims to provide new biomarker combinations to predict the incidence of postoperative ICU admissions in elderly patients. |
What was learned from the study? |
The novel biomarker combinations (Scr × PCT and Scr × CRP) exhibited acceptable performance in predicting the postoperative ICU admissions in elderly patients. |
Scr × CRP also had a moderate predictive value for postoperative cardiovascular events. |
For complications ≥ CDC grade 3, Scr × PCT, Scr × CRP, and Scr × hsCRP were moderate predictors. |
Introduction
Over the past three decades, improvements in the quality of healthcare have led to an increase in life expectancy. In 2019, there were about 703 million people aged 65 years and over worldwide, and the number is expected to reach 1.5 billion by 2050 [1]. The growing numbers of elderly people who are more susceptible to health problems poses new challenges for perioperative medicine. Aging is a common risk factor for diseases such as malignancies and fractures [2,3,4], which often require surgical treatment. The number of elderly patients who require surgery as their primary treatment has increased rapidly in recent years. Among 300 million people globally who underwent surgery every year, patients aged 65 years and over accounted for more than 30% of cases [5]. Despite continuous advances in medicine, these elderly patients have an increased risk of postoperative complications and even the need for postoperative admission to an intensive care unit (ICU), because of their decreased physiological reserve, increased comorbidity, and a chronic inflammatory background [6,7,8,9].
Early diagnosis and effective prediction are essential requirements for preventing serious postoperative complications [10]. As a result of tissue specificity and reproducible measurements, some biomarkers play a key role in the timely prediction and early identification of the risk for disease, risk stratification, and patient management [11]. However, the use of a single biomarker has a number limitations in predicting and evaluating postoperative complications because of the complexity of the underlying disease processes, especially for elderly patients with multiple complications. In recent years, an increasing number of studies have focused on identifying the optimal combination of biomarkers to predict or identify patients’ outcomes [10,11,12,13].
Serum creatinine (Scr) is usually used to estimate the glomerular filtration rate under stable renal function, and its elevation usually indicates acute kidney injury (AKI) or chronic kidney disease [14]. In addition, Scr has been used as a surrogate of muscle mass measurements at a steady state and as an indicator of protein energy expenditure to predict the prognosis of the patients admitted to ICU [15, 16]. As a result of physiological degeneration and multiple comorbidities, elderly patients usually present with a chronic inflammatory background [8], with perioperative inflammatory responses being associated with multiple postoperative complications [17,18,19]. These may be due to imbalanced cytokines that cause systemic inflammatory responses or immunosuppression, leading to postoperative tissue/organ dysfunction [20]. Procalcitonin (PCT), C-reactive protein (CRP), and high-sensitivity CRP (hsCRP) are non-specific proteins which indicate the degree of systemic inflammation and can assist in the identification of an infection and characterization of disease severity [21]. In addition, CRP and hsCRP, as indicators of cardiac and vascular aging, have been widely used for cardiovascular risk prediction [22, 23].
The aim of this study was to combine the Scr concentration and inflammatory levels of the biomarkers (e.g., PCT, CRP, hsCRP) to provide a novel biomarker combination to predict the occurrence of postoperative complications in elderly patients.
Methods
Study Setting
This was a single-center, nested case–control study from a prospective observational cohort, strictly conducted according to STROBE guidelines, carried out from June 1, 2020 to January 19, 2021. The trial was prospectively registered with the China Clinical Trial Registry (ChiCTR1900026223, https://www.chictr.org.cn).
Ethical Approval
The study was performed in accordance with the Helsinki Declaration. The study protocols were approved (No. 199, 2020) by the ethical committees of West China Hospital of Sichuan University, Chengdu, (Chairperson Prof Shaolin Deng) on May 25, 2020. All study participants have signed informed consent to participate in the study, and they were free to withdraw from the study at any time for any reason. There was no any identifying information of participants included in the manuscript.
Patients
In this study, a cohort of patients who were scheduled for surgery under general anesthesia were systematically enrolled on the basis of specific inclusion criteria. These criteria included being 65 years or older, irrespective of sex, undergoing elective non-cardiac and non-urological surgery set to start before 10:00 a.m., having an American Society of Anesthesiologists (ASA) physical status ranging from I to IV, and providing signed informed consent. Exclusion criteria for the study encompassed patients with major preoperative comorbidities such as acute kidney injury (AKI), acute coronary syndrome, stroke, pneumonia, delirium, etc., those already in the ICU prior to surgery, individuals with blood disorders or immune deficiencies, patients with mental health conditions or those unable to give written informed consent or participate in the study, and anyone with a known allergy to anesthetics. Participants were notified about the collection and analysis of peripheral blood samples for the study, with the assurance that they could opt out at any point without any specific reason.
Anesthesia Procedure
Every patient received routine preoperative evaluations, encompassing medical history review, physical checks, blood laboratory tests, chest radiography, and a 12-lead electrocardiogram. Additional examinations were conducted as deemed necessary by the medical team. On the day preceding the surgery, the assigned anesthesiologist assessed each patient to establish the appropriate anesthesia plan.
Upon entering the operating room, each patient was monitored using standard methods: electrocardiography, non-invasive blood pressure, pulse oximetry, and the bispectral index (BIS). Central venous pressure and invasive blood pressure monitoring were implemented when necessary. Continuous monitoring of end-tidal CO2 partial pressure (PETCO2) and airway pressure began following endotracheal intubation. For general anesthesia induction, a combination of 1.5–2.5 mg kg−1 propofol, 0.3 μg kg−1 sufentanil, and 0.1–0.2 mg kg−1 cisatracurium or 0.08–0.1 mg kg−1 vecuronium bromide was administered intravenously. Post intubation, the ventilation was regulated with a 6–8 mL kg−1 tidal volume and a respiratory rate of 10–16 beats min−1 to maintain PETCO2 between 35 and 45 mmHg. Anesthesia maintenance involved opioids (remifentanil and sufentanil), muscle relaxants (cisatracurium or vecuronium bromide), inhalation anesthetics (sevoflurane or desflurane), and propofol, aiming for a BIS range of 40–60. Anesthetic administration ceased upon completion of the surgery. The patient was then transferred to the post-anesthesia care unit or directly to the ICU on the basis of the anesthesiologist’s decision.
Scr, PCT, CRP, and hsCRP Measurements
Venous blood samples were obtained from all patients 24 h prior to surgery, using ethylenediaminetetraacetic acid-evacuated tubes which were immediately centrifuged. Scr concentrations were determined through preoperative blood biochemistry, with a normal reference range of 49–88 μmol L−1. Measurements of plasma PCT, CRP, and hsCRP levels were conducted using a Finecare 3 FS-205 Plus immunofluorescence automatic analyzer (Guangzhou Wanfu Biotechnology Co., Ltd, Guangzhou, China). The minimum detectable levels for PCT, CRP, and hsCRP were 0.05 ng mL−1, 2.5 mg L−1, and 0.25 mg L−1, respectively. For values below these thresholds, the recorded concentration was the minimum detectable limit. When measuring hsCRP levels using the analyzer, if blood sample concentrations exceeded 5 mg L−1, which is the device’s maximum detection limit, the recorded value was set at 5 mg L−1. For PCT, CRP, and hsCRP, the established normal reference ranges were 0–0.5 ng mL−1, 0–10 mg L−1, and 0–1 mg L−1, respectively.
Data Collection
After obtaining their signed consent forms, patients were assigned unique identification codes for anonymity. Different trained professionals conducted the pre-surgery data collection and the post-surgery follow-up, with each group not having access to each other’s information.
Patient information, such as demographic, clinical, and laboratory data, was gathered from the hospital electronic medical record system. This encompassed details like age, gender, body weight, stature, body mass index, and whether they smoked. Clinical information covered existing health conditions, frailty, ASA physical status, the New York Heart Association (NYHA) cardiac function classification, motion equivalence, surgical procedure type, surgery and anesthesia time. Preoperative blood tests provided Scr. Frailty was assessed with reference to the previous study using Clinical Frailty Scale [24].
Trained researchers monitored postoperative complications through interviews while the patients were in the hospital and via phone calls after their discharge. These follow-ups occurred at 24 h, 72 h, 7 days, and 30 days post-surgery. In cases of serious adverse events, daily follow-ups were conducted during the patient’s hospitalization. The severity of complications was assessed using a modified version of the Clavien–Dindo Classification (CDC) scheme [25]. Complications rated as CDC grade 3 or higher were considered moderate to severe. Major complications encompassed death related to the disease or surgery within 30 days post surgery, admissions to the ICU, cardiovascular incidents, acute kidney injury (AKI), postoperative delirium (POD), and infections. The patients admitted to ICU in this study required further life monitoring and treatment; however, the individuals who were only temporarily transferred and quickly discharged within less than 24 h were excluded from the study [26, 27]. AKI was defined by the 2012 Kidney Disease Improving Global Outcomes (KDIGO) criteria [28]. Cardiovascular events covered newly developed or worsened congestive heart failure, acute myocardial infarction, or arrhythmias [29]. The diagnosis of POD was based on the confusion assessment method [30].
Outcomes
The primary outcomes of the study were the efficacy of preoperative concentrations of Scr, PCT, CRP, and hsCPR for predicating the risk of ICU admissions. The secondary outcomes were the predictive effectiveness of preoperative concentrations of Scr, PCT, CRP, and hsCPR for other complications, including cardiovascular events, complications ≥ CDC grade 3, major complications, AKI, POD, and infection.
Statistical Analysis
The determination of the sample size was grounded on the assessment of the area under the curve (AUC) of the receiver operating characteristic (ROC) curves, utilizing MedCalc software (version 19). Drawing on data from a prior study and anticipating a 3% incidence of ICU admissions, along with an AUC of 0.75 for Scr, PCT, CRP, and hsCRP levels, with a two-sided alpha of 0.05, it was calculated that 380 patients would provide a 90% statistical power to discern significant differences in AUC values. Considering the possibility of a 10% dropout rate due to patients lost to follow-up, the study ultimately included 418 patients.
Statistical analyses were executed using SPSS software (version 15). Data were tested for normal distribution and variance homogeneity using Kolmogorov–Smirnov and Brown–Forsythe tests. For comparisons between two groups, the Wilcoxon test was employed. The ROC curve analysis and the corresponding AUC results were utilized to assess the predictive accuracy of preoperative Scr, PCT, CRP, and hsCRP levels for postoperative complications. Diagnostic test accuracy is considered poor if the AUC is between 0.5 and 0.6, moderate if it is between 0.6 and 0.7, acceptable with an AUC ranging from 0.7 to 0.8, very good for an AUC between 0.8 and 0.9, and excellent when the AUC exceeds 0.9 [31]. The cutoff points were determined using the Youden index. The relative risk (RR) and 95% confidence intervals (CIs) were calculated using chi-squared tests. Statistical analyses in this study were conducted using two-sided tests, with a P value of less than 0.05 being considered indicative of a significant result.
Results
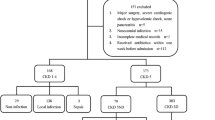
A total of 450 patients were in principle eligible for inclusion, but 21 were excluded because they had preoperative kidney dysfunction (n = 7), a history of hematological diseases (n = 2) or mental diseases (n = 3), were in the ICU before surgery (n = 11), and data missing (n = 9). Five patients were lost to follow-up, and a total of 413 completed the 30-day follow-up (Fig. 1). The demographics, surgery, and clinical features of the patients are shown in Table 1.
The incidence of various complications within 30 days of surgery is shown in Supplementary Table 1, with 22 (5.33%) patients with complications ≥ CDC grade 3 after surgery. Comparing the demographics, surgery, and clinical features of CDC grade 3 positive and negative patients, we found that the positive patients had a higher prevalence of COPD preoperatively, and more patients underwent thoracic and pancreatic surgeries (Supplementary Table 2). The incidence of ICU admissions was 5.33% (Supplementary Table 1). As listed in Table 2, the patients admitted to ICU had higher Scr × PCT (P = 0.007) and Scr × CRP (P = 0.015) values than the negative patients. Fourteen (3.39%) patients exhibited significant cardiovascular events. The value of Scr × CRP in these patients was higher than those of negative patients (P = 0.016, Table 2). The values of hsCRP, Scr × PCT, Scr × CRP, and Scr × hsCRP in patients with complications ≥ CDC grade 3, major complications, or with infections were higher than those in negative patients (Table 2). However, no statistically significant differences were found in the indicators between AKI and POD positive and negative patients (Supplementary Table 3). In addition, we also analyzed these indicators of elderly people aged 75 years and above, and found that the positive patients admitted to ICU had higher Scr (P = 0.020) and Scr × CRP (P = 0.006) than negative patients (Supplementary Table 4).
The ROC analysis revealed a predictive value of preoperative concentrations of Scr, PCT, CRP, and hsCRP for 30-day complications after surgery. For ICU admissions, the AUCs (95% CI) of Scr × PCT and Scr × CRP were 0.750 (0.655–0.845) (P = 0.007) and 0.724 (0.567–0.882) (P = 0.015), respectively (Table 3, Fig. 2a). The cutoff values were 3.875 and 216.250, respectively, which had the best combined sensitivities and specificities (Table 3). RR values were also calculated to identify the risk of different values of Scr × PCT and Scr × CRP for ICU admissions (Table 4). The AUC (95% CI) of Scr × CRP for cardiovascular events was 0.688 (0.560–0.817) (P = 0.017), with a cutoff value of 203.750 (Table 3, Fig. 2b). The AUCs (95% CI) and the cutoff values of complications ≥ CDC grade 3, major complications, and infection are given in Table 3 and Fig. 2c–e.
Results of ROC analysis for preoperative PCT, CRP, hsCRP, and Scr for predicting ICU admission (a), cardiovascular events (b), complications ≥ CDC grade 3 (c), major complications (d), and infection (e) within 30 days after surgery. CDC Clavien–Dindo Classification, CRP C-reactive protein, hsCRP high-sensitivity C-reactive protein, ICU intensive care unit, PCT procalcitonin, ROC receiver operating characteristic, Scr serum creatinine
Discussion
This study demonstrated that combinations of Scr and PCT or CRP are acceptable predictors of postoperative ICU admissions in elderly patients. Furthermore, combinations of Scr and CRP can effectively predict cardiovascular events in elderly patients within 30 days of surgery. For complications ≥ CDC grade 3, Scr × PCT, Scr × CRP, and Scr × hsCRP were valuable predictors. Scr × hsCRP also has predictive value for major complications and postoperative infections.
The elderly patients had a higher ICU admissions rate compared to younger patients as a result of the various comorbidities. Elderly people over 65 years old account for 45.7% of the total ICU population [32]. Among the patients admitted to ICU > 65 years old, 39.2% were admitted because of trauma or for surgical reasons [32]. There was no significant correlation between ICU admission and advanced age, admission mainly being determined by the severity of comorbidities [32]. The elderly patients included in this study did not have serious complications before surgery, and their ASA status was II to III in all cases. This may be a reason for the low incidence of postoperative ICU admissions reported among the patients in this study. With advanced age, trauma and infectious etiologies increased [32]. Elderly patients are often in a chronic inflammatory state, which likely increases their susceptibility to inflammatory damage and hospital infections, especially those who are critically ill [33]. PCT, CRP, and hsCRP are easily measurable laboratory biomarkers, which are recommended as promising candidate predictors for ICU admission, and can provide a different prognostic classification for clinicians according to different stratifications [34,35,36].
In the present study, no statistically significant differences were found between PCT, CRP, and hsCRP in positive and negative ICU admission patients before surgery, but when CRP or PCT was combined with Scr, these biomarker combinations exhibited acceptable predictive efficacy for ICU admissions. We speculate that the upper limit of the hsCRP concentration detected by the analyzer was 5 mg L−1, which limited the true expression in positive patients and thus reduced the predictive effect of Scr × hsCRP.
Inflammation characterizes all stages of atherosclerotic thrombosis [37], and therefore various inflammatory factors may be useful clinical markers for predicting cardiovascular events. Among them, hsCRP is considered to be the most powerful single factor in predicting cardiovascular events [23]. While in our study, there were no statistically significant differences in PCT, CRP, or hsCRP concentrations in patients with or without postoperative cardiovascular events. However, we found that Scr combined with CRP had a moderate predictive effect for the occurrence of postoperative cardiovascular events. We look forward to the completion of a multicenter study with a larger sample size to demonstrate the predictive efficacy of this combination of biomarkers for cardiovascular events.
PCT and CRP concentrations are commonly used indicators to assist in the diagnosis of infection [21]. As previous studies reported, PCT and CRP concentrations 1–2 days after surgery can predict the occurrence of infection, while preoperative PCT and CRP concentrations cannot [38,39,40]. This is consistent with the results of our study. Although there were significant differences in the values of their combination with Scr in patients with infection positive and negative diagnoses, their predictive effect is not sufficiently useful, and further explorations of more valuable biomarker combinations are needed.
AKI is a common clinical condition encountered in the ICU. Approximately 50% of the patients admitted to ICU will develop AKI and over 20% of critically ill patients will develop severe AKI at stage 2 or 3 [41]. Usually, AKI is unpredictable. For most patients, AKI develops without obvious warning or symptoms until a sudden drop in renal function occurs [42]. The change in Scr concentration is the cornerstone of the current diagnostic approach, but it has been shown to be a clinically lacking biomarker [41]. We found there was no statistic difference in Scr concentrations between AKI positive and negative patients, which was consistent with the findings of previous studies. Inflammation is an important component of AKI, playing a considerable role in its pathophysiology [43]. Some studies have found that the changes in perioperative PCT and CRP are good indicators for predicting AKI after cardiac surgery [44, 45]. In contrast, few studies reported on the predictive effect of preoperative inflammatory indicators on postoperative AKI. Kurtul and colleagues found the concentration of PCT measured on admission was a significant independent predictor for contrast-induced AKI [46]. However, in the study no statistically significant differences were found in PCT, CRP, and hsCRP concentrations in postoperative AKI negative and positive patients. Therefore, preoperatively, Scr and inflammatory biomarkers cannot accurately predict the likely occurrence of AKI after surgery, and more research is still needed to explore this predictor.
This study used AUC to assess the predictive efficacy of biomarkers for postoperative complications. Multifactor analysis is also a common prognostic method in clinical practice. Multifactor analysis might be more accurate and cost-effective but can vary between individuals, like the ASA physical status, affecting stability [47]. The biomarkers we selected are commonly used clinical indicators. The advantages of applying molecular markers are good stability, sensitivity, and repeatability, which are convenient for continuous monitoring and dynamic risk assessment, and may have better generalization ability. If molecular indicators and clinical indicators are jointly applied, it may be possible to combine the advantages of both sides to improve the accuracy and scope of evaluation and prediction, which will be the focus of further exploration.
There were a number of limitations to the present study. First, the effects of the time of surgery on the incidence of postoperative complications remains controversial. We only recruited patients who started surgery before 10 a.m., so the reported incidence of postoperative complications may have been influenced by the time of surgery. Second, this was a single-center study, and the results need to be validated by larger multicenter cohort trials. Finally, we analyzed the AUC and corresponding P values of multiple secondary outcomes, but the values were between 0.5 and 0.7, which were not satisfactory. Thus, the prediction for ICU admissions is relatively clear, but the predictive values of secondary outcomes were only suggestive.
Conclusions
The novel biomarker combinations (Scr × PCT and Scr × CRP) exhibited acceptable performance in predicting the postoperative ICU admissions in elderly patients. Scr × CRP also has a moderate clinical predictive effect for the occurrence of postoperative cardiovascular events.
Data Availability
Data are available upon reasonable request. The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Vogel A, Guinemer C, Fürstenau D. Patients’ and healthcare professionals’ perceived facilitators and barriers for shared decision-making for frail and elderly patients in perioperative care: a scoping review. BMC Health Serv Res. 2023;23(1):197.
Montagu A, Speirs A, Baldock J, Corbett J, Gosney M. A review of vertebroplasty for osteoporotic and malignant vertebral compression fractures. Age Ageing. 2012;41(4):450–5.
Liu Y, Wang Z, Xiao W. Risk factors for mortality in elderly patients with hip fractures: a meta-analysis of 18 studies. Aging Clin Exp Res. 2018;30(4):323–30.
Soerjomataram I, Bray F. Planning for tomorrow: global cancer incidence and the role of prevention 2020–2070. Nat Rev Clin Oncol. 2021;18(10):663–72.
Nepogodiev D, Martin J, Biccard B, Makupe A, Bhangu A. Global burden of postoperative death. Lancet. 2019;393(10170):401.
Partridge JS, Harari D, Dhesi JK. Frailty in the older surgical patient: a review. Age Ageing. 2012;41(2):142–7.
Santhirapala R, Partridge J, MacEwen CJ. The older surgical patient – to operate or not? A state of the art review. Anaesthesia. 2020;75(Suppl 1):e46–53.
Colloca G, Santoro M, Gambassi G. Age-related physiologic changes and perioperative management of elderly patients. Surg Oncol. 2010;19(3):124–30.
Xin Q, Xie T, Chen R, et al. Construction and validation of an early warning model for predicting the acute kidney injury in elderly patients with sepsis. Aging Clin Exp Res. 2022;34(12):2993–3004.
Parnetti L, Gaetani L, Eusebi P, et al. CSF and blood biomarkers for Parkinson’s disease. Lancet Neurol. 2019;18(6):573–86.
Barichello T, Generoso JS, Singer M, Dal-Pizzol F. Biomarkers for sepsis: more than just fever and leukocytosis—a narrative review. Crit Care. 2022;26(1):14.
Xie Y, Ankawi G, Yang B, et al. Tissue inhibitor metalloproteinase-2 (TIMP-2) • IGF-binding protein-7 (IGFBP7) levels are associated with adverse outcomes in patients in the intensive care unit with acute kidney injury. Kidney Int. 2019;95(6):1486–93.
Müller D, Győrffy B. DNA methylation-based diagnostic, prognostic, and predictive biomarkers in colorectal cancer. Biochim Biophys Acta. 2022;1877(3):188722.
Prowle JR, Kolic I, Purdell-Lewis J, Taylor R, Pearse RM, Kirwan CJ. Serum creatinine changes associated with critical illness and detection of persistent renal dysfunction after AKI. Clin J Am Soc Nephrol. 2014;9(6):1015–23.
Park J, Mehrotra R, Rhee CM, et al. Serum creatinine level, a surrogate of muscle mass, predicts mortality in peritoneal dialysis patients. Nephrol Dial Transplant. 2013;28(8):2146–55.
Thongprayoon C, Cheungpasitporn W, Kashani K. Serum creatinine level, a surrogate of muscle mass, predicts mortality in critically ill patients. J Thorac Dis. 2016;8(5):E305-311.
Riedel B, Browne K, Silbert B. Cerebral protection: inflammation, endothelial dysfunction, and postoperative cognitive dysfunction. Curr Opin Anaesthesiol. 2014;27(1):89–97.
Boehm O, Baumgarten G, Hoeft A. Epidemiology of the high-risk population: perioperative risk and mortality after surgery. Curr Opin Crit Care. 2015;21(4):322–7.
Romagnoli S, Ricci Z. Postoperative acute kidney injury. Minerva Anestesiol. 2015;81(6):684–96.
Lin E, Calvano SE, Lowry SF. Inflammatory cytokines and cell response in surgery. Surgery. 2000;127(2):117–26.
Pierrakos C, Velissaris D, Bisdorff M, Marshall JC, Vincent JL. Biomarkers of sepsis: time for a reappraisal. Crit Care. 2020;24(1):287.
Bao H, Cao J, Chen M, et al. Biomarkers of aging. Sci China Life Sci. 2023;66(5):893–1066.
Lawler PR, Bhatt DL, Godoy LC, et al. Targeting cardiovascular inflammation: next steps in clinical translation. Eur Heart J. 2021;42(1):113–31.
Yamato Y, Kamiya K, Hamazaki N, et al. Utility of the fatigue, resistance, ambulation, illness, and loss of weight scale in older patients with cardiovascular disease. J Am Med Dir Assoc. 2022;23(12):1971–1976.e2.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Chan DXH, Sim YE, Chan YH, Poopalalingam R, Abdullah HR. Development of the Combined Assessment of Risk Encountered in Surgery (CARES) surgical risk calculator for prediction of postsurgical mortality and need for intensive care unit admission risk: a single-center retrospective study. BMJ Open. 2018;8(3):e019427.
Chiew CJ, Liu N, Wong TH, Sim YE, Abdullah HR. Utilizing machine learning methods for preoperative prediction of postsurgical mortality and intensive care unit admission. Ann Surg. 2020;272(6):1133–39.
Gumbert SD, Kork F, Jackson ML, et al. Perioperative acute kidney injury. Anesthesiology. 2020;132(1):180–204.
Zhao Y, Hao X, Zhu Y, Chen M, Ou M, Zhu T. A combination of N-terminal proB-type natriuretic peptide and myoglobin can predict severe complications after major non-cardiac surgery in elderly patients: a prospective observational cohort study. Front Med. 2021;8:679260.
Shin HJ, Woo Nam S, Kim H, et al. Postoperative delirium after dexmedetomidine versus propofol sedation in healthy older adults undergoing orthopedic lower limb surgery with spinal anesthesia: a randomized controlled trial. Anesthesiology. 2023;138(2):164–71.
Šimundić AM. Measures of diagnostic accuracy: basic definitions. EJIFCC. 2009;19(4):203–11.
Fuchs L, Chronaki CE, Park S, et al. ICU admission characteristics and mortality rates among elderly and very elderly patients. Intensive Care Med. 2012;38(10):1654–61.
Muscedere J, Waters B, Varambally A, et al. The impact of frailty on intensive care unit outcomes: a systematic review and meta-analysis. Intensive Care Med. 2017;43(8):1105–22.
Liu JX, Zhang Q, Bai JS, et al. Procalcitonin (PCT) improves the accuracy and sensitivity of CURB-65 score in predicting CAP patients admission to ICU. Clin Lab. 2023. https://doi.org/10.7754/Clin.Lab.2022.220342.
Chen Y, Li LIQ, Ge YL, et al. Procalcitonin (PCT) improves the accuracy and sensitivity of Dyspnea, Eosinopenia, Consolidation, Acidemia and Atrial Fibrillation (DECAF) score in predicting AECOPD patients admission to ICU. Clin Lab. 2020. https://doi.org/10.7754/Clin.Lab.2019.190612.
Li WQ, Chen Y, Liu TJ, et al. Serum procalcitonin, white blood cell and hypersensitive C-reactive protein combined with age established a new prediction model in predicting ICU admission in adult community-acquired pneumonia (CAP) patients. Clin Lab. 2020. https://doi.org/10.7754/Clin.Lab.2019.191008.
Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation. 2002;105(9):1135–43.
Liu H, Luo Z, Liu L, et al. Early kinetics of procalcitonin in predicting surgical outcomes in type A aortic dissection patients. Chin Med J. 2017;130(10):1175–81.
Zhao D, Zhou J, Haraguchi G, Arai H, Mitaka C. Procalcitonin for the differential diagnosis of infectious and non-infectious systemic inflammatory response syndrome after cardiac surgery. J Intensive Care. 2014;2:35.
Cananzi FCM, Biondi A, Agnes A, et al. Optimal predictors of postoperative complications after gastrectomy: results from the procalcitonin and C-reactive protein for the early diagnosis of anastomotic leakage in esophagogastric surgery (PEDALES) study. J Gastrointest Surg. 2023;27(3):478–88.
Ronco C, Bellomo R, Kellum JA. Acute kidney injury. Lancet. 2019;394(10212):1949–64.
Uettwiller-Geiger DL, Vijayendran R, Kellum JA, Fitzgerald RL. Analytical characteristics of a biomarker-based risk assessment test for acute kidney injury (AKI). Clin Chim Acta. 2016;455:93–8.
Akcay A, Nguyen Q, Edelstein CL. Mediators of inflammation in acute kidney injury. Mediators Inflamm. 2009;2009:137072.
Brocca A, Virzì GM, de Cal M, Giavarina D, Carta M, Ronco C. Elevated levels of procalcitonin and interleukin-6 are linked with postoperative complications in cardiac surgery. Scand J Surg. 2017;106(4):318–24.
Chen X, Zhou J, Fang M, et al. Procalcitonin, interleukin-6 and C-reactive protein levels predict renal adverse outcomes and mortality in patients with acute type A aortic dissection. Front Surg. 2022;9:902108.
Kurtul A, Murat SN, Yarlioglues M, et al. Procalcitonin as an early predictor of contrast-induced acute kidney injury in patients with acute coronary syndromes who underwent percutaneous coronary intervention. Angiology. 2015;66(10):957–63.
Mayhew D, Mendonca V, Murthy BVS. A review of ASA physical status—historical perspectives and modern developments. Anaesthesia. 2019;74(3):373–9.
Acknowledgements
We thank the participants of the study.
Funding
This work was supported by Sichuan Natural Science Foundation project (2023NSFSC1647), 1·3·5 project for disciplines of excellence, West China Hospital, Sichuan University (ZYJC21008), and CAMS Innovation Fund for Medical Sciences (2019-I2M-5-011, 2022-I2M-C&T-B-099). The journal’s Rapid Service Fee was funded by the authors.
Author information
Authors and Affiliations
Contributions
Conceptualization: Mengchan Ou, Xuechao Hao; Methodology: Yali Chen, Yi Teng, Xiran Peng, Xuechao Hao; Formal analysis and investigation: Yali Chen, Yi Teng, Juan Liu; Writing—original draft preparation: Yali Chen; Writing—review and editing: Mengchan Ou, Xuechao Hao; Funding acquisition: Xuechao Hao; Resources: Tao Zhu, Mengchan Ou, Xuechao Hao; Supervision: Tao Zhu, Mengchan Ou, Xuechao Hao.
Corresponding authors
Ethics declarations
Conflict of Interest
Yali Chen, Yi Teng, Xiran Peng, Tao Zhu, Juan Liu, Mengchan Ou and Xuechao Hao have nothing to disclose.
Ethical Approval
The study was performed in accordance with the Helsinki Declaration. The study protocols were approved (No. 199, 2020) by the ethical committees of West China Hospital of Sichuan University, Chengdu, (Chairperson Prof Shaolin Deng) on May 25, 2020. All study participants have signed informed consent to participate in the study, and they were free to withdraw from the study at any time for any reason. There was no any identifying information of participants included in the manuscript.
Additional information
Prior Presentation: The abstract was presented in part at the 18th World Congress of Anaesthesiologists in Singapore on March 6, 2024.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Chen, Y., Teng, Y., Peng, X. et al. Combination of Creatinine with Inflammatory Biomarkers (PCT, CRP, hsCRP) for Predicting Postoperative ICU Admissions for Elderly Patients. Adv Ther 41, 2776–2790 (2024). https://doi.org/10.1007/s12325-024-02874-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-024-02874-1