Abstract
Background
Non-small cell lung cancer (NSCLC) is a highly aggressive type of lung cancer with poor responses to traditional therapies such as surgery, radiotherapy, and chemotherapy. While immunotherapy has become an effective approach for treating multiple types of cancer, solid tumors frequently exhibit immune escape through various mechanisms, including downregulation of MHC I expression. However, whether the upregulation of MHC I expression can improve the immunotherapeutic effect on NSCLC remains unexplored. Suberoylanilide hydroxamic acid (SAHA) is a potent histone deacetylase (HDAC) inhibitor that has been applied clinically to treat lymphoma, but a high dose of SAHA kills tumor cells and normal cells without preference. Here, we report that low-dose SAHA enhances CD8+ T cell-mediated antitumor immunity by upregulating MHC I expression in NSCLC cells.
Methods
Flow cytometric analysis, quantitative real-time PCR and western blot were used to analyze the expression of MHC I, STAT1 and Smad2/3 in both human and mouse NSCLC cell lines after SAHA treatment. The nuclear translocation of phosphorylated STAT1 and Smad2/3 was investigated by western blot and immunofluorescence staining. The mechanisms underlying STAT1 and Smad2/3 upregulation were analyzed through database searches and chromatin immunoprecipitation-qPCR. Finally, we assessed the antitumor effect of specific CD8+ T cells with SAHA treatment in vivo and in vitro.
Results
We showed that low-dose SAHA upregulated the expression of MHC I in NSCLC cell lines without affecting cell viability. We also provided evidence that high levels of MHC I induced by SAHA promoted the activation, proliferation, and cytotoxicity of specific CD8+ T cells in mouse models. Mechanistically, low-dose SAHA increased the levels of H3K9ac and H3K27ac in the promoters of the STAT1, Smad2 and Smad3 genes in NSCLC cells by inhibiting HDAC activity, resulting in elevated expression levels of STAT1, Smad2 and Smad3. The nuclear translocation of phosphorylated STAT1 and Smad2/3 markedly upregulated the expression of MHC I in NSCLC cells.
Conclusions
Low-dose SAHA enhances CD8+ T cell-mediated antitumor immunity by boosting MHC I expression in NSCLC cells. Thus, we revealed a key mechanism of SAHA-mediated enhanced antitumor immunity, providing insights into a novel immunotherapy strategy for NSCLC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Background
Lung cancer continues to be a major health problem associated with high morbidity and mortality [1]. More than 85% of lung cancers are non-small cell lung cancers (NSCLCs) [2]. The traditional treatments for NSCLC include surgery, radiotherapy, and chemotherapy, which have limited curative effects and obvious side effects [3]. Although traditional lung cancer treatment has reached a bottleneck, immunotherapy has gained considerable attention [4, 5]. Importantly, enhancing antitumor immunity by targeting the immune system is the key treatment strategy [6]. However, several studies have demonstrated that tumor cells play important roles in regulating host immune responses and have various ways to escape immune surveillance and attacks [7, 8]. During the tumor immune response, major histocompatibility complex class I (MHC I) combined with antigen peptides is indispensable for specific CD8+ T cell activation and proliferation [9]. Nevertheless, one of the principal mechanisms of immune escape by solid tumors is the downregulation of MHC I, resulting in a weakened antitumor effect [10, 11]. Thus, increasing the expression of MHC I on the surface of tumor cells is one of the most critical aspects for improving the immunotherapeutic effect for NSCLC.
Suberoylanilide hydroxamic acid (SAHA) is a classic chemotherapeutic drug and a potent histone deacetylase (HDAC) inhibitor. According to previous studies, HDAC inhibitors can enhance T cell-mediated antitumor immunity and exert multiple cytotoxic effects on cancer cells, including inhibiting tumor proliferation, invasion, metastasis, and differentiation [12, 13]. To take advantage of these biological effects, SAHA has been reported to be clinically applied to treat lymphoma that continues to deteriorate or relapse [14]. Despite the common use of SAHA to kill tumor cells, SAHA has been demonstrated to participate in immune regulation, such as promoting MHC I expression [15]. Although there have been several clinical studies on SAHA combined with other anticancer drugs for NSCLC treatment [16, 17], the immunotherapeutic effect of SAHA in NSCLC remains elusive.
Upon stimulation by extracellular signals, STAT1 in the cytoplasm can be phosphorylated and form heterodimers, and the translocation of p-STAT1 from the cytoplasm to the nucleus is considered a key regulator of tumor immune surveillance [18, 19]. In addition, upon stimulation, STAT1, Smad2 and Smad3 can be phosphorylated and translocated into the nucleus to control the transcription of immune regulatory genes [20, 21]. However, the molecular mechanism by which low-dose SAHA exerts antitumor effects on NSCLC is poorly understood, and whether STAT1 and Smad2/3 are involved in SAHA-mediated immune regulation is unclear.
In the present study, we demonstrated that low-dose SAHA can upregulate the expression of MHC I on the surface of NSCLC cells, thereby enhancing specific CD8+ T cell activation and proliferation. Moreover, we provide evidence that SAHA can activate the STAT1 and Smad2/3 signaling pathways to achieve strong immunotherapeutic outcomes in NSCLC.
2 Methods
2.1 Chemicals and reagents
Suberoylanilide hydroxamic acid (SAHA) and carboxyfluorescein succinimidyl ester (CFSE) were purchased from Sigma‒Aldrich. Lipofectamine 2000 was purchased from Invitrogen. siRNAs targeting human STAT1, Smad2, and Smad3 were purchased from GenePharma (Shanghai, China), and siRNAs targeting mouse STAT1, Smad2, and Smad3 were purchased from Gene Biosystems (Anhui, China). For western blot analysis, antibodies against human and mouse p-STAT1, p-Smad2/3, and STAT1 were purchased from Cell Signaling Technology; antibodies against human and mouse Smad2, Smad3, β-actin, GAPDH, and mouse MHC I were purchased from Proteintech (Wuhan, China); and antibodies against human MHC I were obtained from Huaan (Hangzhou, China). All the antibodies used for flow cytometry were purchased from BioLegend. All the antibodies used for chromatin immunoprecipitation were purchased from Cell Signaling Technology. For the antibodies used for immunofluorescence staining, anti-STAT1 and anti-Smad2 were purchased from Proteintech (Wuhan, China), and anti-Smad3 was purchased from ImmunoWay Biotechnology. The STAT1 and Smad2/3 inhibitors nifuroxazide and ITD-1 were purchased from Selleck. The purified anti-mouse PD-1 antibody was purchased from Biolegend. Anti-CD3/CD28 beads were purchased from Invitrogen. The CD8+ T cell isolation kit was purchased from Miltenyi Biotec. IFN-γ and TNF-α ELISA kits were purchased from Dakewe (Beijing, China). An apoptosis detection kit was purchased from BD Biosciences. The HDAC Activity Direct Assay Kit was purchased from Epigentek.
2.2 Animals and cell lines
Male C57BL/6 mice (6–8 weeks old) were purchased from the Shanghai SLAC Laboratory Animal Center (Shanghai, China), and male BALB/C nude mice (6–8 weeks old) were purchased from Vital River with a health certificate. All the mice had acclimatization periods of 1 week after arrival. All animal experiments were conducted at the Animal Experiment Center of the First Affiliated Hospital of USTC and approved by the Ethics Committee of the First Affiliated Hospital of USTC. A549, NCI-H520, NCI-H460, NCI-H157, NCI-H1975 and NCI-H1703 human NSCLC cell lines; the human normal lung epithelial cell line BEAS-2B; and the mouse Lewis lung carcinoma cell line were obtained from the Chinese Academy of Sciences Cell Bank (Shanghai, China). A549 and Lewis lung carcinoma cells were cultured in DMEM, and the other cells were cultured in RPMI 1640 culture medium. All the cell lines were cultured in an incubator at 37 °C in a humidified atmosphere with 5% CO2.
2.3 Western blot analysis
Proteins from tumor cells were extracted with RIPA buffer, and the concentrations of the lysates were determined using a BCA protein assay kit (Thermo Scientific). The samples were loaded and separated on a 10% gel by SDS‒PAGE and transferred onto PVDF membranes. The membranes were blocked in 5% bovine serum albumin (BSA) and probed with specific primary antibodies at 4 °C overnight. Then, the membranes were incubated with peroxidase-conjugated secondary antibodies at room temperature for 1 h. Finally, the protein bands were detected using an enhanced chemiluminescence (ECL) western blot detection kit.
2.4 Quantitative real-time PCR (qPCR)
Total RNA was extracted using TRIzol reagent (Invitrogen) according to the manufacturer’s protocol. qPCR was performed using SYBR Master Mix (Takara Bio) on an ABI 7500 system. The mRNA levels were normalized to those of GAPDH. The primer sequences are listed in Supplemental Table S1.
2.5 Chromatin immunoprecipitation-qPCR
Chromatin immunoprecipitation was conducted according to the manufacturer’s protocols (Cell Signaling Technology). Briefly, the tumor cells were crosslinked, and the chromatin was sheared and extracted. Immunoprecipitation was performed with anti-p-Smad2, anti-H3K9ac and anti-H3K27ac antibodies. The sequences of the primers used for ChIP‒qPCR are listed in Supplemental Table S2.
2.6 Gene silencing experiments
siRNAs targeting human or mouse STAT1, Smad2, and Smad3 were transfected into tumor cells via Lipofectamine 2000 according to the manufacturer’s protocol. The expression of the indicated genes was verified via qPCR. The siRNA sequences are listed in Supplemental Table S3.
2.7 Flow cytometric analysis
The following surface-staining antibodies were used: anti-human HLA-A, -B, and -C (W6/32), anti-human CD80 (2D10), anti-human CD86 (IT2.2), anti-mouse H-2Kb/H-2Db (28-8-6), anti-mouse CD80 (16-10A1), anti-mouse CD86 (GL-1), anti-mouse CD8a (53-6.7), and anti-mouse PD-1 (29 F.1A12). For intracellular cytokine staining, tumor-infiltrating lymphocytes were isolated and cultured for 4 h in the presence of a cell stimulation cocktail with brefeldin A (BioLegend). The lymphocytes were treated with anti-mouse IFN-γ (XMG1.2) following the cytoplasmic protein staining protocol (BioLegend), and flow cytometric analysis was performed with a flow cytometer (BD Calibur).
2.8 Immunofluorescence staining
Tumor cells seeded in confocal dishes were fixed with 15% formaldehyde for 15 min at room temperature and then permeabilized with 0.2% Triton X-100 for 10 min. After being blocked with 5% BSA for 1 h, the cells were incubated with primary antibodies overnight at 4 °C, followed by incubation with fluorescent secondary antibodies for 1 h at room temperature. Finally, the nuclei were stained with DAPI (1 µg/ml). The fluorescent cells were observed by confocal microscopy (ZEISS LSM880).
2.9 Mouse immunization
Lewis lung carcinoma cells were subjected to three cycles of rapid freezing at -80 °C and thawing at 37 °C to prepare tumor cell lysates, followed by centrifugation at 2000×g for 10 min to remove cellular debris. Emulsions containing equal volumes of Lewis cell lysate and complete Freund’s adjuvant (CFA, Sigma‒Aldrich) or incomplete Freund’s adjuvant (IFA, Sigma‒Aldrich) were prepared by vortexing the suspensions for 30 min until a stable oil‒water emulsion was achieved. The mice were immunized as described previously [22, 23]. Briefly, C57BL/6 mice were immunized by subcutaneous injection of 100 µg of Lewis cell lysate in CFA on day 0 and boosted with 100 µg of Lewis cell lysate in IFA on days 7 and 14. Splenic CD8+ T cell were isolated by magnetic sorting (Miltenyi Biotec) and cocultured with SAHA-pretreated Lewis lung carcinoma cells. The proliferation of CFSE-labeled T cells and the apoptosis of Lewis lung carcinoma cells were detected.
2.10 In vivo animal experiments
For the Lewis tumor model, C57BL/6 mice or nude mice were challenged subcutaneously with 5 × 105 Lewis lung carcinoma cells. Five days after tumor cell inoculation, the mice were treated intratumorally with SAHA or intraperitoneally with nifuroxazide and ITD-1 every other day. The palpable tumors were measured with calipers, and the tumor volume was calculated according to the following formula: volume = (length×width²)/2, where length and width are measured in millimeters. The maximal tumor size permitted by the Ethics Committee of the First Affiliated Hospital of USTC was 2.0 cm3, and the maximal tumor size in our experiments was not exceeded.
2.11 Isolation of tumor-infiltrating lymphocytes (TILs)
Lewis cell-derived tumor tissues were removed, digested with collagenase IV (10 mg/mL), hyaluronidase (100 µg/mL), and DNA enzyme (20 µg/mL) for 2 h at 37 °C, and homogenized with frosted slides. After the red blood cells were lysed, the lymphocytes were separated by a mouse lymphocyte separation solution (Dakewe, China).
2.12 Database search
The CISTROME DB database (http://cistrome.org/db) was used to determine the binding abundance of H3K9ac and H3K27ac in the promoter regions of STAT1, Smad2 and Smad3, and the data were visualized in the UCSC database (http://genome.ucsc.edu). We used the JASPAR database to predict the binding sites of Smad2 to the promoter regions of the HLA-A, HLA-B, and HLA-C genes.
2.13 Statistical analysis
Unpaired t tests or one-way ANOVA were performed to evaluate the differences between the groups, and the Shapiro‒Wilk normality test was used to assess the normality of the data. The data are expressed as the mean ± SD of three independent experiments. GraphPad Prism software 9.3 was used to analyze the data. Differences were considered statistically significant when p < 0.05.
3 Results
3.1 Low-dose SAHA upregulates the expression of MHC I in NSCLC cell lines
HDACIs have been reported to be associated with the repression of MHC I in various tumors [24, 25]. Therefore, we postulated that SAHA, a classic HDAC inhibitor, might upregulate the expression of MHC I in NSCLC. First, we analyzed MHC I expression in a series of NSCLC cell lines and normal lung epithelial cells. It was observed that the expression level of MHC I in NSCLC cells was significantly lower than that in normal lung epithelial cells, and the lowest expression was detected in A549 and NCI-H520 (hereafter, H520) cells (Fig. S1A). Therefore, we selected these two NSCLC cell lines for subsequent experiments. Next, a CCK-8 assay was employed to determine the cytotoxicity of SAHA in A549 and H520 cells. We found that cell viability was inhibited in a dose-dependent manner, especially at relatively high concentrations of SAHA, which significantly decreased the survival rates of A549 and H520 cells (Fig. S1B). To determine the immunoregulatory effect of SAHA on NSCLC cells, when the cell viability was approximately 85%, 3 µM SAHA was added to A549 and H520 cells (Fig. S1B). Surprisingly, the qPCR results showed that the expression levels of HLA-A, HLA-B, and HLA-C were clearly elevated after 24 h (Fig. 1A and B). In parallel, the protein levels of MHC I in SAHA-treated A549 and H520 cells also increased, as determined by western blotting and flow cytometry at 24 h and 48 h (Fig. 1C–F). The same results were also observed in Lewis lung carcinoma cells, a typical mouse NSCLC cell line (Fig. 1G and H). Moreover, 3 µM SAHA inhibited the activity of total HDAC (Fig. S1C). Based on these results, SAHA was used at a concentration of 3 µM in subsequent experiments. In addition to HLA-A, HLA-B, and HLA-C, the gene encoding MHC I molecules (Β2m) was upregulated in SAHA-treated cells, as were genes directing peptide transporters (Tap1 and Tap2) (Fig. 1I–K). Moreover, the expression of costimulatory molecules such as CD80 and CD86 increased dramatically with SAHA treatment (Fig. S2A–C). Taken together, the above results suggest that low-dose SAHA upregulates the expression of both MHC I and related molecules, such as peptide transporters and costimulatory molecules, in NSCLC cell lines without affecting cell viability, thereby indicating the potential of SAHA in immune regulation.
Low-dose SAHA upregulates the expression of MHC I in NSCLC cell lines. A–F A549 and H520 cells were cultured with 3 µM SAHA for 24 h and 48 h. The expression of HLA-A, HLA-B, and HLA-C at 24 h was measured by qPCR (A, B). The protein levels of MHC I at 24 h and 48 h were detected by western blotting (C, D), and the surface expression of MHC I was assessed by flow cytometry (E, F). G, H The expression of MHC I in Lewis lung carcinoma cells treated with 3 µM SAHA for 24–48 h was measured by western blotting (G) and flow cytometry (H). I–K The expression of B2m, Tap1 and Tap2 in Lewis (I), A549 (J) and H520 (K) cells treated with 3 µM SAHA for 48 h was measured by qPCR. The error bars represent the mean ± SD; *p < 0.05; **p < 0.01; SAHA-treated group compared with the control group. All the experiments were repeated three times
3.2 SAHA promotes STAT1 and Smad2/3 phosphorylation and nuclear translocation to increase MHC I expression in NSCLC cell lines
Next, we investigated the molecular mechanism by which SAHA upregulated MHC I expression. According to previous studies, STAT1 is a key regulator of MHC I and MHC II expression [26, 27], and HDACI treatment can activate Smad2/3 to enter the nucleus and regulate the expression of downstream genes [28]. Here, we treated both human and mouse NSCLC cells with SAHA for 24 h and 48 h. As expected, the total protein levels of STAT1, Smad2 and Smad3 increased significantly (Fig. 2A, B and Fig. S3A). Since the activation of STAT1 and Smad2/3 is characterized by phosphorylation, H520, A549 and Lewis lung carcinoma cells were treated with SAHA at different time points. As shown in Fig. 2C, D and Fig. S3B, SAHA rapidly induced STAT1 and Smad2/3 phosphorylation at 10 min in H520 and A549 cells and at 60 min in Lewis lung carcinoma cells. To further study whether SAHA promoted the translocation of cytoplasmic p-STAT1 and p-Smad2/3 to the nucleus, cell fractionation experiments and western blotting were performed to analyze SAHA-treated NSCLC cells. The addition of SAHA led to an increase in the expression of p-STAT1 and p-Smad2/3 in the nuclei of H520, A549 and Lewis lung carcinoma cells (Fig. 3A, B and Fig. S3C). Moreover, immunofluorescence analysis further confirmed the nuclear accumulation of STAT1, Smad2 and Smad3 after SAHA treatment for 24 h and 48 h (Fig. 3C–F). These findings imply that SAHA activates NSCLC cells via STAT1 and Smad2/3 phosphorylation and their nuclear translocation.
Next, we wondered whether phosphorylated STAT1 and Smad2/3 could influence MHC I expression after nuclear translocation. Previous studies have demonstrated that STAT1 can act as a transcription factor that targets the promoter regions of MHC I genes to regulate their expression [29]. In the case of Smad2/3, the JASPAR website revealed multiple binding sites for Smad2 at the promoter regions of the HLA-A, HLA-B, and HLA-C genes. Therefore, chromatin immunoprecipitation (ChIP)-qPCR was conducted and further confirmed that p-Smad2 indeed bound to the promoters of HLA-A, HLA-B, and HLA-C and that the binding of p-Smad2 could be promoted significantly by SAHA (Fig. 3G and H). Smad2 and Smad3 translocate into the nucleus together once activated [30], and our above data demonstrate that p-Smad2 is the binding site of activated Smad2/3. Taken together, our results indicate that the activation of STAT1 and Smad2/3 by SAHA can increase MHC I expression by binding to the promoters of the HLA-A, B, and C genes.
SAHA promotes STAT1 and Smad2/3 phosphorylation in NSCLC cell lines. A, B H520 and Lewis lung carcinoma cells were cultured with 3 µM SAHA for 24–48 h, and the total STAT1, Smad2 and Smad3 protein levels were evaluated by western blotting. The error bars represent the mean ± SD; *p < 0.05; **p < 0.01; 24 h and 48 h groups compared with the 0 h group. C, D H520 and Lewis lung carcinoma cells were treated with 3 µM SAHA at different time points, and the expression levels of p-STAT1, p-Smad2/3 and total STAT1, Smad2 and Smad3 were tested by western blotting. Error bars represent the mean ± SD; *p < 0.05; **p < 0.01; ***p < 0.001; 10 min to 120 min groups or 60 min to 180 min groups compared with the 0 min group. All the experiments were repeated three times
SAHA promotes the nuclear translocation of p-STAT1 and p-Smad2/3 in NSCLC cell lines. A, B H520 and Lewis lung carcinoma cells were treated with 3 µM SAHA for 24 h, the expression levels of p-STAT1 and p-Smad2/3 in the cytosol and nucleus were detected by western blotting, and the nuclear/cytosolic ratio (Nuc/Cyt) was calculated relative to that in the control group. The error bars represent the mean ± SD; **p < 0.01; ***p < 0.001; SAHA-treated group compared with the control group. C–F H520 and Lewis lung carcinoma cells treated with 3 µM SAHA for 24–48 h were subjected to immunofluorescence staining for STAT1, Smad2 and Smad3. Scale bars, 20 μm. The data are representative of three independent experiments. The percentages of colocalization were calculated by ImageJ software. The error bars represent the mean ± SD; *p < 0.05; **p < 0.01. G, H A549 and H520 cells were treated with 3 µM SAHA for 48 h, and ChIP‒qPCR analysis was performed with p-Smad2 antibody and HLA-A, -B, and -C promoter-specific primers. The error bars represent the mean ± SD; *p < 0.05; ***p < 0.001; SAHA-treated group compared with the control group. All the experiments were repeated three times
3.3 SAHA-induced MHC I upregulation is blocked by STAT1 and Smad2/3 knockdown
To confirm the role of STAT1 and Smad2/3 in SAHA-induced MHC I upregulation, the expression of STAT1, Smad2 and Smad3 in H520 and A549 cells was silenced by siRNA. The protein levels of MHC I obviously decreased upon STAT1, Smad2 and Smad3 knockdown, even after the cells were treated with SAHA for 48 h (Fig. 4A–C and Fig. S4A–C). Consistent with these results, the silencing of STAT1, Smad2 and Smad3 in Lewis lung carcinoma cells was performed (Fig. S4D–F) and markedly reduced SAHA-mediated MHC I upregulation, as shown by both western blotting and flow cytometry (Fig. 4D–I). In summary, the above data revealed that SAHA upregulates the expression of MHC I in NSCLC cells by activating the STAT1 and Smad2/3 pathways.
SAHA-induced MHC I upregulation is blocked by STAT1 and Smad2/3 knockdown. A–I H520 and Lewis lung carcinoma cells were transfected with STAT1, Smad2 and Smad3 siRNAs prior to treatment with SAHA for 48 h. The protein levels of MHC I, STAT1, Smad2 and Smad3 in H520 (A–C) and Lewis (D–F) cells were detected by western blotting, and the surface expression of MHC I in Lewis lung carcinoma cells was evaluated by flow cytometry (G–I). Error bars represent the mean ± SD; *p < 0.05; **p < 0.01; the siRNA group compared with the NC group. All the experiments were repeated three times
3.4 SAHA drastically increases the acetylation of the promoter regions of STAT1, Smad2 and Smad3
The above data revealed that the expression of STAT1, Smad2 and Smad3 in NSCLC cells increased after SAHA treatment, which prompted us to investigate how SAHA influences these signaling molecules. It has been reported that HDACIs can increase the expression of targeted molecules by promoting the acetylation of genes [31]. Interestingly, we discovered H3K9ac and H3K27ac modifications in the promoter regions of STAT1, Smad2 and Smad3 in A549 cells via analysis of the CISTROME DB and UCSC databases (Fig. 5A). To verify this finding, ChIP‒qPCR was carried out to test histone acetylation. As expected, H3K9 and H3K27 were acetylated in the promoter regions of STAT1, Smad2 and Smad3 in H520 cells and Lewis lung carcinoma cells (Fig. 5B–G). More importantly, the degree of acetylation was dramatically increased by SAHA treatment in both NSCLC cell lines, except for H3K9ac on STAT1 in Lewis lung carcinoma cells (Fig. 5B–G). Collectively, these observations indicate that SAHA triggers the upregulation of STAT1, Smad2 and Smad3 by increasing the acetylation of the promoter regions of the corresponding genes.
SAHA drastically increases the acetylation of the promoter regions of STAT1, Smad2 and Smad3. A H3K9ac and H3K27ac modifications in the promoter regions of STAT1, Smad2 and Smad3 in A549 cells were analyzed via the CISTROME DB and UCSC databases. B–G H520 and Lewis lung carcinoma cells were treated with 3 µM SAHA for 24 h, and ChIP‒qPCR analysis was performed with H3K9ac and H3K27ac antibodies and STAT1, Smad2 and Smad3 promoter-specific primers. Error bars represent the mean ± SD; *p < 0.05; **p < 0.01; ***p < 0.001; SAHA-treated group compared with the control group. All the experiments were repeated three times
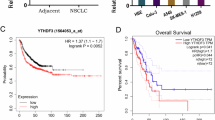
3.5 SAHA remarkably enhances antitumor immunity in a mouse model
Next, we sought to validate the therapeutic effect of SAHA in tumor-bearing mice. To this end, C57BL/6 mice were inoculated subcutaneously with Lewis lung carcinoma cells, followed by intratumoral SAHA injection every other day. As shown in Fig. 6A, compared with the control group, SAHA significantly inhibited tumor growth, indicating that SAHA could generate an antitumor effect. In addition, the same experiment was conducted in T cell-deficient nude mice, and we found that SAHA failed to exert an antitumor effect (Fig. 6B), suggesting that SAHA may elicit potent antitumor T cell immunity. To further clarify the immunomodulatory effect of SAHA on T cells, tumor-infiltrating lymphocytes (TILs) were isolated from Lewis cell-derived tumors after five consecutive days of intratumoral SAHA injection. Flow cytometric analysis revealed that the percentage of CD8+ T cells among the TILs was increased significantly (Fig. 6C). More importantly, SAHA induced a high frequency of IFN-γ+ CD8+ T cells among the TILs (Fig. 6D). In addition, IFN-γ levels were strikingly increased, whereas TNF-α levels were moderately increased in TILs, as demonstrated by ELISA (Fig. S5A and B). These results revealed the activation and proliferation of tumor-infiltrating CD8+ T cells in the presence of SAHA in vivo. To further evaluate the influence of SAHA on Lewis-specific CD8+ T cells in vitro, splenic CD8+ T cells purified from mice immunized with Lewis lung carcinoma cell lysates emulsified in Freund’s adjuvant were cocultured with Lewis lung carcinoma cells pretreated with SAHA for 48 h. As a result, SAHA-treated Lewis lung carcinoma cells had a greater ability to stimulate T cell proliferation (Fig. 6E) and a greater rate of early and late apoptosis (Fig. 6F). In addition, we found that the dosage of SAHA we used had less side-effect on CD8+ T cell proliferation (Fig. S5C), so we tried to evaluate whether SAHA could improve the immunotherapy sensitivity of NSCLC when SAHA was combined with an anti-PD-1 antibody. As expected, SAHA had little effect on the expression of PD-1 on CD8+ T cells (Fig. 6G), and tumor growth was dramatically inhibited in the SAHA and anti-PD-1 antibody combination group compared with the anti-PD-1 antibody alone group (Fig. 6H). Together, the above data indicate that SAHA can markedly enhance CD8+ T cell-mediated antitumor immunity by upregulating MHC I expression in Lewis lung carcinoma cells and improve the efficacy of anti-PD-1 antibodies in cancer immunotherapy for NSCLC.
SAHA remarkably enhances antitumor immunity in a mouse model. A, B C57BL/6 mice (A) or nude mice (B) were challenged subcutaneously with 5 × 105 Lewis lung carcinoma cells. Five days after tumor cell inoculation, the mice were treated intratumorally with SAHA (100 mg/kg) or DMSO as a control every other day (n = 6 per group). The tumor volumes were measured and calculated. The error bars represent the mean ± SD; ***p < 0.001; SAHA-treated group compared with the control group. C, D TILs were isolated after intratumoral injection of 100 mg/kg SAHA in Lewis cell-derived tumor-bearing mice for five consecutive days, and the percentages of CD8+ T cells (C) and IFN-γ+ CD8+ T cells (D) were detected by flow cytometry after culturing for an additional 4 h in the presence of the Cell Stimulation Cocktail with Brefeldin A. Error bars represent the mean ± SD; **p < 0.01; SAHA-treated group compared with the control group. E, F C57BL/6 mice were immunized by subcutaneous injection of 100 µg of Lewis cell lysate in CFA on day 0 and boosted with 100 µg of Lewis cell lysate in IFA on days 7 and 14. Splenic CD8+ T cells were isolated by magnetic sorting and subsequently cocultured with SAHA-pretreated Lewis lung carcinoma cells for 24 h and 48 h. The proliferation of 5 µM CFSE-labeled CD8+ T cells at 48 h (E) and the apoptosis of Lewis lung carcinoma cells at 24 h and 48 h (F) were evaluated by flow cytometry. The error bars represent the mean ± SD; **p < 0.01; SAHA-treated group compared with the control group. G Splenic CD8+ T cells isolated from C57BL/6 mice activated with anti-CD3/CD28 beads were cultured with 3 µM SAHA, and the expression of PD-1 at 48 h and 72 h was measured by flow cytometry. The error bars represent the mean ± SD. H C57BL/6 mice were challenged subcutaneously with 6 × 105 Lewis lung carcinoma cells. Five days after tumor inoculation, the mice were treated intratumorally with DMSO as a control or SAHA (100 mg/kg) or intraperitoneally with an anti-PD1 antibody (200 µg) every other day (n = 6 per group). The tumor volumes were measured and calculated. The error bars represent the mean ± SD; ***p < 0.001, anti-PD-1 antibody-treated group compared with the control group or the SAHA and anti-PD-1 antibody combination group compared with the anti-PD-1 antibody-treated group. All the experiments were repeated three times
3.6 Inhibition of STAT1 and Smad2/3 represses SAHA-mediated antitumor immunity
We then investigated the potential significance of STAT1 and Smad2/3 blockade in SAHA-mediated antitumor immunity. Here, STAT1 and Smad2/3 inhibitors (nifuroxazide and ITD-1) were used to block the signaling pathway in SAHA-treated mice. As shown in Fig. 7A, SAHA failed to exert a therapeutic effect on Lewis cell-derived tumors when STAT1 and Smad2/3 inhibitors were injected intraperitoneally. Notably, the increase in the percentage of CD8+ T cells and IFN-γ-secreting CD8+ T cells in Lewis cell-derived tumor-infiltrating lymphocytes was also blocked by the inhibitors (Fig. 7B and C), revealing that STAT1 and Smad2/3 are involved in the immunomodulatory effect of SAHA. Moreover, the ability of SAHA-treated Lewis lung carcinoma cells to stimulate T cell proliferation was strikingly repressed by silencing STAT1, Smad2, and Smad3 (Fig. 7D). Consistently, when STAT1, Smad2, and Smad3 were knocked down, coculture of specific CD8+ T cells and SAHA-treated Lewis lung carcinoma cells did not lead to an increase in the rate of apoptosis (Fig. S5D). Taken together, these results suggest that SAHA-mediated antitumor immunity is regulated through the STAT1 and Smad2/3 pathways.
Inhibition of STAT1 and Smad2/3 represses SAHA-mediated antitumor immunity. A C57BL/6 mice were challenged subcutaneously with 5 × 105 Lewis lung carcinoma cells. Five days after tumor inoculation, the mice were treated intratumorally with DMSO as a control or SAHA (100 mg/kg) or intraperitoneally with nifuroxazide (Nif, 25 mg/kg) and ITD-1 (ITD, 5 mg/kg) every other day (n = 6 per group). The tumor volumes were measured and calculated. The error bars represent the mean ± SD; ***p < 0.001, the SAHA-treated group compared with the control group; NS, the Nif + ITD + SAHA-treated group compared with the Nif + ITD-treated group. B, C TILs were isolated after the intratumoral injection of SAHA (100 mg/kg) or the intraperitoneal injection of nifuroxazide (Nif, 25 mg/kg) or ITD-1 (ITD, 5 mg/kg) in Lewis cell-derived tumor-bearing mice for five consecutive days, and the percentages of CD8+ T cells (B) and IFN-γ+ CD8+ T cells (C) were detected by flow cytometry. The error bars represent the mean ± SD; *p < 0.05. D C57BL/6 mice were immunized by subcutaneous injection of 100 µg of Lewis lung carcinoma cell lysate in CFA on day 0 and boosted with 100 µg of Lewis lung carcinoma cell lysate in IFA on days 7 and 14. Splenic CD8+ T cells were isolated by magnetic sorting and subsequently cocultured with SAHA-pretreated Lewis lung carcinoma cells with STAT1, Smad2, and Smad3 knockdown. The proliferation of 5 µM CFSE-labeled CD8+ T cells was tested by flow cytometry. The error bars represent the mean ± SD; **p < 0.01. All the experiments were repeated three times
4 Discussion
In recent years, HDAC inhibitors have been increasingly applied as therapeutic agents in the treatment of a variety of cancers and other diseases [32, 33]. SAHA, a potent HDAC inhibitor, has shown remarkable performance in the treatment of cutaneous T-cell lymphomas since its introduction to the market [34], but its effect on immunotherapy in NSCLC is not clear. In the present study, SAHA was applied at low doses to treat NSCLC cells without affecting cell viability. We discovered that SAHA increased the levels of H3K9ac and H3K27ac in the promoters of the STAT1, Smad2 and Smad3 genes in NSCLC cells by inhibiting HDAC activity, thereby driving an increase in their expression levels. Upon SAHA stimulation, phosphorylated STAT1 and Smad2/3 are subsequently translocated from the cytosol to the nucleus, resulting in a marked increase in the expression of MHC I on the surface of both human and mouse NSCLC cells. More importantly, we provided evidence that high levels of MHC I induced by SAHA promoted the activation, proliferation, and cytotoxicity of specific CD8+ T cells, thereby enhancing the antitumor immunotherapeutic effect of low-dose SAHA (Fig. 8). To our knowledge, this is the first report to reveal the specific mechanism of the immunotherapeutic effect of SAHA on NSCLC.
Schematic representation of the study. SAHA increases the levels of H3K9ac and H3K27ac in the promoters of the STAT1, Smad2 and Smad3 genes in NSCLC cells by inhibiting HDAC activity, thereby increasing their expression levels. Upon SAHA stimulation, STAT1 and Smad2/3 are phosphorylated and translocated from the cytosol to the nucleus, resulting in a marked increase in the expression of MHC I on the surface of both human and mouse NSCLC cells. High levels of MHC I promote the activation, proliferation, and cytotoxicity of specific CD8+ T cells, thereby enhancing the antitumor immunotherapeutic effect of SAHA
Lung cancer is one of the malignant tumors with the fastest increase in morbidity and mortality and is therefore a great threat to the health and quality of life of the population [35]. Approximately 85% of lung cancers are NSCLC, most of which are already in advanced stages at the time of diagnosis [36]. Surgery, radiotherapy, and chemotherapy constitute traditional clinical treatments for NSCLC, which have great limitations and impact patients’ quality of life. In addition, due to immune deficiency or damage caused by radiotherapy and chemotherapy, residual tumor cells develop further, which is characterized by proliferation, invasion, and metastasis. Thus, it is necessary to explore effective therapeutic approaches with fewer side effects for treating NSCLC to meet critical medical needs. In recent years, tumor immune escape has attracted much attention, and treatments targeting the immune system are being developed. In previous clinical studies, SAHA was used to treat NSCLC in combination with erlotinib or bortezomib, but the treatment effect was not satisfactory [16, 17]. The negative clinical data could be explained by the following reasons: (1) the scale of these studies was too small, (2) the drug exposure was limited by oral administration, and (3) the mechanism of other anticancer drugs antagonized the therapeutic effect of SAHA. Here, we investigated the immunomodulatory effect of low-dose SAHA, but the optimal route for drug administration remains to be explored, and additional clinical trials are needed.
Tumor immune escape is an important strategy for tumor survival and involves a variety of mechanisms. Nevertheless, one of the principal mechanisms is the downregulation of MHC I, which has been observed in approximately 40–90% of human tumors and is usually associated with poor prognosis [37]. More importantly, the MHC I-antigen peptide complex plays a pivotal role in stimulating CD8+ T cell immunity [38], whereas costimulatory molecules such as CD80 and CD86 provide the second signal for T cell activation. In general, the downregulation of MHC I in tumor cells is often accompanied by low levels of CD80 and CD86, so tumor-specific CD8+ T cells cannot be activated completely [39]. Therefore, increasing the expression of MHC I and costimulatory molecules in NSCLC cells will improve the antitumor immune response to some extent. In this study, we compared MHC I expression in a series of human NSCLC cell lines verified by short tandem repeat (STR) analyses and HLA gene sequencing at the Chinese Academy of Sciences Cell Bank. Under the premise of ensuring that the HLA gene was not mutant, A549 and H520 cell lines with relatively low MHC I expression were selected for all experiments to ensure the reliability of the experimental results.
The significant finding of this study is that low-dose SAHA can kill NSCLC cells through immune regulation rather than through direct induction of tumor cell death. Previous studies have confirmed that activated STAT1 enters the nucleus to regulate the expression of human MHC genes [40], and the translocation of phosphorylated Smad2/3 into the nucleus is associated with the process of immune regulation [41]. On this basis, we found that in NSCLC cells, MHC I upregulation and the proliferation and killing ability of specific CD8+ T cells could be repressed by STAT1 and Smad2/3 blockade, suggesting the synergistic effects of STAT1 and Smad2/3 in SAHA-induced immune regulation. In our study, the protein levels of STAT1 and Smad2/3 were increased at 24–48 h after SAHA treatment, and the phosphorylation of STAT1 and Smad2/3 occurred within 1 h. Because phosphorylation and gene expression are two distinct processes [42, 43], we hypothesize that STAT1 and Smad2/3 could be phosphorylated in a short time by rapid signal transduction from some unknown SAHA receptors on the cell membrane or in the cytoplasm, but gene acetylation and upregulated expression may take longer. To further clarify the relationships among SAHA, histone acetylation, p-STAT1/Smad2/Smad3, STAT1/Smad2/Smad3 and MHC I, we can paraphrase the process as follows: SAHA-induced phosphorylation of STAT1 and Smad2/3 in a short period of time, but the small amount of phosphorylated STAT1 and Smad2/3 entering the nucleus may not be enough to regulate MHC I expression; under the continued influence of SAHA, the enhanced acetylation-mediated increases in STAT1 and Smad2/3 levels resulted in elevated levels of phosphorylated STAT1 and Smad2/3 entering the nucleus to upregulate MHC I expression. However, the current study did not explore the mechanism of phosphorylation of STAT1 and Smad2/3 triggered by SAHA, nor did it explore the specific mechanism by which STAT1 and Smad2/3 regulate MHC I gene transcription, which is a limitation of this study. In addition, we observed that H3K9ac and H3K27ac in the promoter regions of STAT1, Smad2 and Smad3 in NSCLC cells were dramatically increased by SAHA treatment, which explains why SAHA upregulated the expression of STAT1, Smad2 and Smad3. Notably, for STAT1 in Lewis lung carcinoma cells, only H3K27ac was enhanced by SAHA, while both H3K9ac and H3K27ac on STAT1 were increased in H520 cells. These results reveal that human and mouse NSCLC cells are heterogeneous and that increased acetylation of H3K9 and H3K27 is not required simultaneously for STAT1 upregulation.
In summary, the data presented in this study clearly show that MHC I expression in NSCLC cells can be upregulated by low-dose SAHA, revealing a key mechanism of SAHA-mediated enhanced antitumor immunity and opening the door to a novel immunotherapeutic strategy for NSCLC with potential applications.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- NSCLCs:
-
Non-small cell lung cancers
- SAHA:
-
Suberoylanilide hydroxamic acid
- HDAC:
-
Histone deacetylase
- MHC I:
-
Major histocompatibility complex class I
- CFSE:
-
Carboxyfluorescein succinimidyl ester
- BSA:
-
Bovine serum albumin
- ECL:
-
Enhanced chemiluminescence
- ChIP:
-
Chromatin immunoprecipitation
- H520:
-
NCI-H520
- TILs:
-
Tumor-infiltrating lymphocytes
- DMSO:
-
Dimethyl sulfoxide
References
M. Oudkerk, S. Liu, M.A. Heuvelmans, J.E. Walter, J.K. Field, Lung cancer LDCT screening and mortality reduction - evidence, pitfalls and future perspectives. Nat. Rev. Clin. Oncol. 18(3), 135–151 (2021)
R.S. Herbst, D. Morgensztern, C. Boshoff, The biology and management of non-small cell lung cancer. Nature. 553(7689), 446–454 (2018)
De D. Ruysscher, C. Faivre-Finn, K. Nackaerts, K. Jordan, J. Arends, J.Y. Douillard et al., Recommendation for supportive care in patients receiving concurrent chemotherapy and radiotherapy for lung cancer. Ann. Oncol. 31(1), 41–49 (2020)
S. Billan, O. Kaidar-Person, Z. Gil, Treatment after progression in the era of immunotherapy. Lancet Oncol. 21(10), e463–e476 (2020)
M. Massafra, M.I. Passalacqua, V. Gebbia, P. Macrì, C. Lazzari, V. Gregorc et al., Immunotherapeutic advances for NSCLC. Biologics. 15, 399–417 (2021)
G. Cannone, G.M. Comacchio, G. Pasello, E. Faccioli, M. Schiavon, A. Dell’Amore et al., Precision surgery in NSCLC. Cancers (Basel). 15(5), 1571 (2023)
M.L. Burr, C.E. Sparbier, K.L. Chan, Y.C. Chan, A. Kersbergen, E.Y.N. Lam et al., An evolutionarily conserved function of polycomb silences the MHC Class I Antigen Presentation Pathway and enables Immune Evasion in Cancer. Cancer Cell. 36(4), 385–401e8 (2019)
N. McGranahan, R. Rosenthal, C.T. Hiley, A.J. Rowan, T.B.K. Watkins, G.A. Wilson et al., Allele-specific HLA loss and Immune escape in Lung Cancer Evolution. Cell. 171(6), 1259–1271e11 (2017)
D. Dersh, J. Hollý, J.W. Yewdell, A few good peptides: MHC class I-based cancer immunosurveillance and immunoevasion. Nat. Rev. Immunol. 21(2), 116–128 (2021)
G. Sari, K.L. Rock, Tumor immune evasion through loss of MHC class-I antigen presentation. Curr. Opin. Immunol. 83, 102329 (2023)
M.L.M. Jongsma, J. Neefjes, R.M. Spaapen, Playing hide and seek: tumor cells in control of MHC class I antigen presentation. Mol. Immunol. 136, 36–44 (2021)
K. Qu, L.C. Zaba, A.T. Satpathy, P.G. Giresi, R. Li, Y. Jin et al., Chromatin Accessibility Landscape of cutaneous T cell lymphoma and dynamic response to HDAC inhibitors. Cancer Cell. 32(1), 27–41e4 (2017)
J. Wang, F. Hasan, A.C. Frey, H.S. Li, J. Park, K. Pan et al., Histone deacetylase inhibitors and IL21 cooperate to Reprogram Human Effector CD8 + T cells to memory T cells. Cancer Immunol. Res. 8(6), 794–805 (2020)
B.S. Mann, J.R. Johnson, M.H. Cohen, R. Justice, R. Pazdur, FDA approval summary: vorinostat for treatment of advanced primary cutaneous T-cell lymphoma. Oncologist. 12(10), 1247–1252 (2007)
W. Yang, Y. Li, R. Gao, Z. Xiu, T. Sun, MHC class I dysfunction of glioma stem cells escapes from CTL-mediated immune response via activation of Wnt/β-catenin signaling pathway. Oncogene. 39(5), 1098–1111 (2020)
N. Reguart, R. Rosell, F. Cardenal, A.F. Cardona, D. Isla, R. Palmero et al., Phase I/II trial of vorinostat (SAHA) and erlotinib for non-small cell lung cancer (NSCLC) patients with epidermal growth factor receptor (EGFR) mutations after erlotinib progression. Lung Cancer. 84(2), 161–167 (2014)
T. Hoang, T.C. Campbell, C. Zhang, K. Kim, J.M. Kolesar, K.R. Oettel et al., Vorinostat and bortezomib as third-line therapy in patients with advanced non-small cell lung cancer: a Wisconsin Oncology Network Phase II study. Invest. New. Drugs. 32(1), 195–199 (2014)
K. Meissl, N. Simonović, L. Amenitsch, A. Witalisz-Siepracka, K. Klein, C. Lassnig et al., STAT1 isoforms differentially regulate NK Cell Maturation and Anti-tumor Activity. Front. Immunol. 11, 2189 (2020)
X. Li, K. Pan, M. Vieth, M. Gerhard, W. Li, R. Mejías-Luque, JAK-STAT1 signaling pathway is an early response to Helicobacter pylori Infection and contributes to Immune escape and gastric carcinogenesis. Int. J. Mol. Sci. 23(8), 4147 (2022)
B.V. Park, Z.T. Freeman, A. Ghasemzadeh, M.A. Chattergoon, A. Rutebemberwa, J. Steigner et al., TGFβ1-Mediated SMAD3 enhances PD-1 expression on Antigen-Specific T cells in Cancer. Cancer Discov. 6(12), 1366–1381 (2016)
I. Kashiwagi, R. Morita, T. Schichita, K. Komai, K. Saeki, M. Matsumoto et al., Smad2 and Smad3 inversely regulate TGF-β autoinduction in Clostridium butyricum-activated dendritic cells. Immunity. 43(1), 65–79 (2015)
Y. Liu, L. Xu, Y. Jiang, J. Sun, X. He, Phenotypic and functional analysis of LCMV gp33-41-specific CD8 T cells elicited by multiple peptide immunization in mice revealed the up-regulation of PD-1 expression on antigen-specific CD8 T cells. Cell. Mol. Immunol. 4(6), 431–437 (2007)
A.A. Mehrizi, N. Rezvani, S. Zakeri, A. Gholami, L. Babaeekhou, Poly(I:C) adjuvant strongly enhances parasite-inhibitory antibodies and Th1 response against Plasmodium Falciparum merozoite surface protein-1 (42-kDa fragment) in BALB/c mice. Med. Microbiol. Immunol. 207(2), 151–166 (2018)
A.M. Cornel, E. Dunnebach, D.A. Hofman, S. Das, S. Sengupta, van den F. Ham et al., Epigenetic modulation of neuroblastoma enhances T cell and NK cell immunogenicity by inducing a tumor-cell lineage switch. J. Immunother Cancer. 10(12), e005002 (2022)
X. Wu, T. Li, R. Jiang, X. Yang, H. Guo, R. Yang, Targeting MHC-I molecules for cancer: function, mechanism, and therapeutic prospects. Mol. Cancer. 22(1), 194 (2023)
H. Jiang, Y. Li, M. Shen, Y. Liang, Y. Qian, H. Dai et al., Interferon-α promotes MHC I antigen presentation of islet β cells through STAT1-IRF7 pathway in type 1 diabetes. Immunology. 166(2), 210–221 (2022)
J. Tur, C. Farrera, E. Sánchez-Tilló, T. Vico, P. Guerrero-Gonzalez, A. Fernandez-Elorduy et al., Induction of CIITA by IFN-γ in macrophages involves STAT1 activation by JAK and JNK. Immunobiology. 226(5), 152114 (2021)
C. Schelker, P. Nowak-Sliwinska, G. Borchard, HDACIs and TKIs combinations and their liposomal delivery for cancer treatment. J. Control Release. 358, 59–77 (2023)
J.E. Jr Darnell, I.M. Kerr, G.R. Stark, Jak-STAT pathways and transcriptional activation in response to IFNs and other extracellular signaling proteins. Science. 264, 1415–1421 (1994)
E.H. Ervin, R. French, C.H. Chang, S. Pauklin, Inside the stemness engine: mechanistic links between deregulated transcription factors and stemness in cancer. Semin Cancer Biol. 87, 48–83 (2022)
T. Liang, F. Wang, R.M. Elhassan, Y. Cheng, X. Tang, W. Chen et al., Targeting histone deacetylases for cancer therapy: Trends and challenges. Acta Pharm. Sin B 13(6), 2425–2463 (2023)
X.S. Xiang, P.C. Li, W.Q. Wang, L. Liu, Histone deacetylases: a novel class of therapeutic targets for pancreatic cancer. Biochim. Biophys. Acta Rev. Cancer. 1877(1), 188676 (2022)
J. Pedro Ferreira, B. Pitt, F. Zannad, Histone deacetylase inhibitors for cardiovascular conditions and healthy longevity. Lancet Healthy Longev. 2(6), e371–e379 (2021)
P.A. Marks, R. Breslow, Dimethyl sulfoxide to vorinostat: development of this histone deacetylase inhibitor as an anticancer drug. Nat. Biotechnol. 25(1), 84–90 (2007)
A.K. Ganti, A.B. Klein, I. Cotarla, B. Seal, E. Chou, Update of incidence, prevalence, survival, and initial treatment in patients with Non-small Cell Lung Cancer in the US. JAMA Oncol. 7(12), 1824–1832 (2021)
K.C. Arbour, G.J. Riely, Systemic therapy for locally Advanced and Metastatic Non-small Cell Lung Cancer: a review. JAMA 322(8), 764–774 (2019)
S. Gettinger, J. Choi, K. Hastings, A. Truini, I. Datar, R. Sowell et al., Impaired HLA Class I Antigen Processing and Presentation as a mechanism of Acquired Resistance to Immune checkpoint inhibitors in Lung Cancer. Cancer Discov. 7(12), 1420–1435 (2017)
K. Dhatchinamoorthy, J.D. Colbert, K.L. Rock, Cancer Immune Evasion through loss of MHC Class I Antigen Presentation. Front. Immunol. 12, 636568 (2021)
R.G. Majzner, C.L. Mackall, Tumor Antigen escape from CAR T-cell therapy. Cancer Discov. 8(10), 1219–1226 (2018)
J.A. Simpson, A. Al-Attar, N.F. Watson, J.H. Scholefield, M. Ilyas, L.G. Durrant, Intratumoral T cell infiltration, MHC class I and STAT1 as biomarkers of good prognosis in colorectal cancer. Gut. 59(7), 926–933 (2010)
W. Xu, H. Liu, Z.G. Liu, H.S. Wang, F. Zhang, H. Wang et al., Histone deacetylase inhibitors upregulate snail via Smad2/3 phosphorylation and stabilization of snail to promote metastasis of hepatoma cells. Cancer Lett. 420, 1–13 (2018)
E.L. Huttlin, M.P. Jedrychowski, J.E. Elias, T. Goswami, R. Rad, S.A. Beausoleil et al., A tissue-specific atlas of mouse protein phosphorylation and expression. Cell. 143(7), 1174–1189 (2010)
R. Vosooghi, A. Motavalizadehkakhky, A. Mansouri, J. Mehrzad, M. Homayouni, Investigating the effect of hesperetin on estrogen receptor alpha (ERα) expression, phosphorylation and activity in MCF-7 cells. Gene. 911, 148357 (2024)
Acknowledgements
We are grateful to Jie Wang for language polishing.
Funding
This research study was supported by the National Natural Science Foundation of China (81972006) to Baolong Wang. This work was also supported by the National Natural Science Foundation of China (82103307), the Natural Science Foundation of Anhui Province (2108085QH350), the University Natural Science Research Project of Anhui Province (2022AH051254) and the Fundamental Research Funds for the Central Universities (WK9110000074) to Wenqian Dong.
Author information
Authors and Affiliations
Contributions
BW: conception and design. WD: conception and design, animal experiments, data analysis and interpretation, and manuscript writing. HW: conception and design, data analysis and interpretation. BH, YC, RY, SZ, YK and DL: performed the experiments. XZ, YH and MZ: analyzed and interpreted the data. CW, SY and DC: completed critical revisions and proofread the manuscript. All the authors reviewed the manuscript and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval
All the animal experiments were approved by the Ethics Committee of the First Affiliated Hospital of University of Science and Technology of China, and the approval number was 2023-N(A)-73.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Dong, W., He, B., Cao, Y. et al. Low-dose SAHA enhances CD8+ T cell-mediated antitumor immunity by boosting MHC I expression in non-small cell lung cancer. Cell Oncol. (2024). https://doi.org/10.1007/s13402-024-00989-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s13402-024-00989-9