Abstract
Background
Disability is typically correlated with lower quality of life and decreased capacity for self-care. It has been demonstrated that multimorbidity is closely linked to a variety of unfavorable events, such as disability. Researchers are still figuring out how and to what extent co-morbidities impact disability, though. In order to fill up this gap, this study examines the prevalence and contributing variables of disability in older patients who have multimorbidity.
Methods
We conducted a systematic search of Pubmed, Cochrane Library, Web of Science, Embase, and CINAL databases for articles from their inception until September 2023. We selected co-morbid older adults aged > 60 years and used the ADL scale or any scale that assesses disability as an assessment tool. We excluded literature that did not meet the criteria, and literature that could not be included in the data we needed. We extracted data from the included literature and calculated synthetic prevalence rates, ORs, and 95% confidence intervals.
Results
A total of 32 papers (71,135 older adults) were included in the study. The prevalence of disability among older patients with multimorbidity was around 34.9% (95% CI = 25.8-43.9%). Subgroup analysis showed higher rates of disability among comorbidities who were older, female, unmarried, and long-term users of health services. And the incidence of disability increased each year. Meanwhile, the regions of the United States, China, and Spain showed higher rates of disability.
Conclusions
Disability rates in older patients with multimorbidity are higher, thus it’s critical to focus on risk factors while fully accounting for regional variances.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multimorbidity, also known as multiple chronic diseases(MCC), refers to the simultaneous presence of two or more chronic diseases in an individual [1, 2]. Due to improvements in global healthcare, a rise in the average lifespan, and demographic shifts, multimorbidity is becoming more common. The prevalence of multimorbidity is approximately 30% in the young and middle-aged population [3], it can reach up to 55−93% in the population aged 60 and over [4]. Moreover, the prevalence and number of chronic diseases also appear to increase significantly with age, and multimorbidity is more common than any single chronic disease, with prevalence rates of more than 80% of the elderly population aged 80 and over [5].
Multimorbidity makes maintaining the health of older persons more challenging, especially the disabilities that accompany multimorbidity. Disability is a complicated multifactorial state that arises from the interplay of the individual with their whole environment. Disability means a reduction in the person’s autonomy and independence as well as their general capacity to adapt to their social and living environment. According to the World Health Organization’s (WHO) International Classification of Functioning, Disability, and Health (ICF) criteria, disability is often considered an impairment, activity restrictions, and participation limitation in general [6].
Multimorbidity and disability are strongly related, as has been shown in earlier research [7]. Physical functionality may be a good indicator of the cumulative combined impact of chronic illnesses on health. For each additional disease, the patient’s risk of dysfunction increases by 16%, life expectancy decreases by 1.8 years, and the risk of needing the assistance of a healthcare professional increases by 20% [8, 9]. These relationships are typically nonlinear, multimorbidity accelerating the weakening of bodily functions and leading to a rapid deterioration of an individual’s metabolic mechanisms, and given the physiological vulnerabilities associated with aging, older adults are more likely to experience functional disability. The healthcare system is put under an additional burden because of the relationship between disabilities and adverse outcomes including falls and depression, a considerable increase in mortality, frailty, and Emergency Department visits, and a higher likelihood that patients may face social and economic squalor in later life [10,11,12,13]. In order to effectively address the disability of patients, minimize eventual healthcare expenses, and enhance health, determining the disability rate of patients with multimorbidity as well as the risk factors has thus become especially crucial.
Currently, only one systematic review [14] from 2015 explored the correlation between multimorbidity and functional decline. However, the study had a large age span (> 18 years) and did not focus on older adults who were most affected by comorbidity; On the other hand, the study did not calculate the combined rate of disability, and explored and analyzed the influencing factors. Moreover, the study has a long history, and it needs to be discussed in newer literature.Therefore, this study explores and explains this part of the content, and provides a basis for future intervention to delay and control the progress of disability.
Methods
Materials and methods
This study has been registered with the International Prospective Register of Systematic Reviews (Prospero) under the registration number CRD42023425740. This article is reported according to Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA).This study was based on the Cochrane Handbook of Systematic Literature Reviews.
Search strategy
Two researchers searched the literature from the PubMed, Cochrane Library, EMBASE, CINAL, and Web of Science databases with an English-only search language from the library until September 2023. We used Medical Subject Headings (MeSH) keywords to search by title and abstract, using AND, OR to concatenate the following text: older adults (older population, aged, elderly, geriatric) AND multimorbidity (multiple chronic conditions) AND disability (activities of daily living, disabled, ADL, BADL, IADL ). Additional articles were then incorporated by way of hand-searched references.
Eligibility criteria
Inclusion criteria: (1) age 60 and above; (2) multimorbidity: refers to the simultaneous presence of two or more chronic diseases in an individual; (3) studies reporting clinical outcomes including disability. Activities of Daily Living Scale (ADL) are the most common indicator of disability and includes the Basic Activities of Daily Living Scale (BADL) and Instrumental Activities of Daily Living Scale (IADL). The most common scales for BADL include the Katz Independence Index and the Barthel Index, with 6 or 10 items. Including dressing, eating, bathing, dressing, etc. while the IADL has 8 items, including shopping, cooking, etc. In addition, any literature that could define an indicator of disability was also included. (4) study design: Observational studies, including cross-sectional and cohort studies; (5) using disability as a dichotomous outcome indicator, data from the literature provided corrected ORs and 95% CI or sufficient data to calculate prevalence.
The following papers are excluded: duplicates, unrelated to the topic, documents lacking the whole text, and documents from which the necessary data cannot be retrieved.
Risk of bias assessment
Two investigators evaluated the quality of the included literature. The Agency for Healthcare Research and Quality (AHRQ) scale was utilized in the cross-sectional study [15], which has 11 entries with a yes or no answer, yes scoring 1 and no scoring 0, respectively. The final score was 0–3 for low quality literature, 4–7 for moderate quality literature, and 8–11 for high quality literature. The Newcastle Ottawa Scale (NOS) were utilized in the cohort study [16], which has 8 entries, with 0–3 being low quality literature, 4–6 being moderate quality literature, and ≥ 7 being high quality literature, with higher scores indicating better quality literature.
Data extraction
Two researchers were responsible for including, screening and extracting literature according to the criteria. When there was disagreement, we consulted a third researcher. The extracted data was as follows: (a) basic characteristics: authors, year, country, age, gender, number of events, total population, and incidence rate; and (b) study design, research instrument, sample source, sample size, and marital status.
Quality of evidence
In this study, the quality of evidence was evaluated using GRADE (Grading of Recommendations, Assessments, Development, and Evaluation), which consists of 5 evaluations: (a) risk of bias; (b) inconsistency; (c) indirectness; (d) imprecision; and (e) publication bias. The presence of one item was downgraded to a medium quality level; the presence of two items was downgraded to a low quality level; and the presence of three items was a very low quality level.
Statistical analysis
The two researchers independently extracted the data into EXCEL and then analyzed the prevalence rate and 95% confidence interval by STATA17.0 software. The magnitude of heterogeneity was assessed using I 2 and Q tests [17, 18]. When P < 0.05 or I2 > 50%, it was considered that there was significant heterogeneity in the study, which was analyzed by the random-effects model (SMD); When P ≥ 0.5 or I2 ≤ 50%, it was considered that there was no significant heterogeneity, which was analyzed by the fixed-effects model (MD)The articles differed in nadir criteria, study design, and disability criteria, so there was significant heterogeneity between studies (I2 = 99.94%). Therefore, a random effects model was used to calculate the combined effect size. When studies had high heterogeneity, the source of heterogeneity was analyzed subgroups. The publication year (-2015, 2015–2020, 2020-), sample size (<500, > 500), study design (cross-sectional study, cohort study), data source (community, hospitals), gender (male > 50%, female > 50%), marital status (married, unmarried), and country were all taken into consideration. A sensitivity analysis was performed to assess the stability of the findings by excluding individual papers. Funnel plots were generated by Begg-Mazumdar’s and Egger’s tests to determine publication bias. Statistical significance was defined as P < 0.05, and 95% confidence intervals were calculated.
Results
Study selection
In this study, 2823 documents were retrieved from Pubmed, Cochrane Library, Web of Science, EMBASE, and CINAL, and 3 documents were searched manually, totaling 2826 documents included, and 1112 documents remained after deduplication. 1010 literatures were eliminated by reading titles and abstracts. Reading the remaining 102 literature, 73 of them were excluded because they did not meet the inclusion criteria. See Fig. 1.
Study characteristics
32 studies with a total of 71,135 individuals were included in this study, with years from 2006 to 2023, covering countries such as Brazil (n = 1), China (n = 7), the United States (n = 5), Poland (n = 1), Sweden (n = 2), Spain (n = 4), Norway (n = 2), Belgium (n = 1), India (n = 1), Singapore (n = 1), South Korea (n = 1), Netherlands (n = 1), Canada (n = 1), Europe (n = 1), Iceland (n = 1), Nigeria (n = 1), Global (n = 1). See Table 1.
Quality assessment for methodology
A total of 32 papers was included in this study, including 17 cross-sectional [19, 21,22,23, 25, 28, 30,31,32,33, 35,36,37,38, 42, 44, 47] and 15 cohort studies [20, 24, 26, 27, 29, 34, 39,40,41, 43, 45, 46, 48,49,50] with a total of 71,135 individuals. Of the cross-sectional studies, 11 [19, 21,22,23, 31, 33, 35,36,37,38, 42, 44] (45.0%) had high-quality ratings and 6 [25, 28, 30, 32, 33, 47] (25.0%) had moderate quality ratings; of the cohort studies, 9 [24, 27, 29, 34, 39, 40, 43, 46, 47] (20.0%) and 6 [20, 26, 41, 45, 49, 50] (10.0%) of the literature rated as moderate in quality, indicating that the overall quality of the included literature was good. Nine [27, 28, 31, 36, 38,39,40,41, 44] literature explained the sampling method, seven [27, 31, 38,39,40,41, 44] used random sampling, one [28] used systematic random sampling, one [26] used multi-stage cluster random sampling, and the rest of the literature did not elaborate on the sampling method; 15 [19, 23, 26, 27, 29, 31, 35, 37, 39,40,41,42,43, 46, 49] articles described in detail the screening of the included population and the response rate; most of the studies did not have a follow-up, and only 8 [20, 26, 27, 29, 34, 39, 40, 46] articles had a follow-up of 1.5–10 years and described the shedding. See Table 1.
Meta-analysis results
The prevalence of disability among multimorbid elderly individuals
This meta-analysis comprised 32 [19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50] studies, of which 29 [19,20,21,22,23, 25,26,27,28,29,30,31, 34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50] employed ADL scales, such as BADL scales, and IADL scales, and 10 [28, 29, 31, 34, 36, 37, 39, 42, 49, 50] publications used two ADL scales. And 3 [24, 32, 33] publications utilized different measures for assessing disabilities. See Fig. 2. The studies were evaluated using a random effects model due to the studies’ significant heterogeneity (P<0.001, I2>99.9%). In older adults with multimorbidity, the prevalence of disability was 34.9% (95% CI = 25.8−43.9%).
Subgroups analysis
This study has a high heterogeneity, and subgroup analysis is used to examine the origins of heterogeneity. Divided by year of publication: pre−2015, the disability rate among co-morbid patients was 27.9% [95% CI (13.7%, 42.1%)], from 2015 to 2019 the disability rate was 34.7% [95% CI (17.9%, 51.4%)], and after 2020 the disability rate was 37.2% [95% CI (23.3%, 51.0%)]. By country of investigation, the disability rate for co-morbid patients was 40.7% [95% CI (17.5%, 63.9%)] in China, 44.8% [95% CI (36.7%, 53.0%)] in the United States, 18.4% [95% CI (13.9%, 22.9%)] in Sweden, and 38.1% [95% CI (24.1%,52.0%)] in Spain, and 10.4% [95% CI (2.0%,18.8%)] in Norway. By sample size, the disability rate was 37.1% [95% CI (23.5%,51.1%)] for < 500 and 33.6% [95% CI (22.2%,45.0%)] for > 500. By gender, the rate of disability was 33.0% [95% CI (17.4%,48.6%)] for females > 50% and 22.7% [95% CI (17.9%,25.5%)] for males < 50%. By study instrument, the disability rate was 30.1% [95% CI (16.3%,44.0%)] using the ADL scale, 40.7% [95% CI (21.5%,59.9%)] using the IADL scale, 37.6% [95% CI (26.1%,49.0%)] using the BADL, and 43.9% [95% CI (26.1%,49.0%)] using the other scales. By age, the disability rate was 10.3% [95% CI (0.7%,19.49)] for 60–69 years, 21.7% [95% CI (16.2%,27.2%)] for 70–79 years, and 45.9% for ≥ 80 years. By study site, the disability rate was 21.3% [95% CI (15.8%,26.9%)] in the community and 46.7% [95% CI (24.6%,68.8%)] in hospitals. Divided by marital status, the disability rate was 16.8% [95% CI (11.5%,22.0%)] for married and 39.5% [95% CI (25.8%,53.2%)] for unmarried. When categorized by study quality, the disability rate was 39.5% [95% CI (25.8%,53.2%)] for high-quality studies and 30.8% [95% CI (17.0%,44.6%)] for moderate-quality studies. See Table 2.
Sensitivity analysis
To ascertain if the study findings were consistent and dependable, the included literature was eliminated one at a time. The omission of a single piece of literature did not significantly alter the disability rate, according to the results of the sensitivity analysis.
Bias analysis
The results of the funnel plot showed that the graphical distribution was symmetrical, with a low likelihood of risk of bias. See Fig. 3. p = 0.03 < 0.05 in the Begg-Mazumdar’s and Egger’s tests, suggesting the possibility of publication bias.We evaluated the effect of publication bias on the results by trim and filling analysis. The results of trim and filling analysis (PR = 1.093, 95%CI = 0.988 to 1.208) did not affect the results of this study.
Quality of evidence
We evaluated the quality of evidence for the results of the meta-analysis, which showed that the incidence of disability was of low quality.See Table 3.
Conclusion
Findings of summary
This is the first meta-analysis to evaluate the rate of disability in elderly patients with multimorbidity. In all, 32 studies with moderate or high quality literature and dependable results were included in this analysis. The meta-analysis’s findings demonstrated that older patients with multimorbidity had a disability rate of 34.9% (95% CI = 25.8−43.9%)). The results were higher than those of middle-aged and elderly patients in Canada (27.4%) [51] and higher than the senior disability rate globally, which is 10.2% across 194 nations and territories [52]. multimorbidity may be a significant predictor of functional decline in the elderly [15, 53].
We performed subgroup analyses to determine sources of heterogeneity. The results of the subgroup analyses showed that:
-
(1)
Year of Publication: The disability rate rose with the year of publication, we suspect it has to do with the aging trend. The elderly population currently makes up 9.3% of the world’s population [54], reach 41.1% in some countries by 2050, and age is an important indication of disability [55]. On the other hand, the baseline population with disabilities rises due to better medical care, longer life expectancy, and an expanding population with multimorbidity [56]. To lessen and postpone the likelihood of disability, our response strategies to the aging trend and co-morbidity trend should be suggested earlier.
-
(2)
Demographic factors: advanced age, females, and unmarried are more likely to have disabilities. Older people are less able to successfully protect themselves against a range of hostile influences, according to prior studies [55], their physiological functions weaken, their resistance declines, and their compensating systems worsen. The functional independence of the elderly is gravely challenged by the synergistic and cumulative effects of many chronic disorders [57]. Women had a higher likelihood of being disabled, which was in line with Yau’s findings [58]. In addition to biological disparities, Zhu [59] claims that due to cultural and familial obligations, women commonly face difficulties while seeking to receive healthcare treatments. Therefore, while having a greater life expectancy than men, women may have worse health outcomes. To compensate for the differences caused by aging and gender, which are objective factors that cannot be changed, the researchers suggest that social and medical resources can be appropriately tilted, and appropriate medical assistance and financial subsidies can be provided. According to Pang’s study [60], the probability of disability is higher for people who are alone or unmarried. Based on the marital resource hypothesis, marriage has a health-protective effect that delays health deterioration, and the feeling of duty and responsibility it imparts promotes positive behaviors in old age and has an influence on health status [60]. We believe that having healthy interpersonal interactions and participating in social activities as appropriate may help to lessen the disability of celibacy people [61, 62].
-
(3)
Sample source: Compared to those in the community, hospital patients are more likely to be disabled. This is simple to understand. People with major health problems and a high risk of becoming disabled are those who frequently get primary healthcare or live in long-term care facilities. Elderly residents of the community are more physically and mentally well, have more energy for social contact, and are less prone to suffer negative outcomes. Consequently, the management of multiple medications, remote monitoring of their physical condition, diet and exercise advice, and standardized rehabilitation training are helpful assistance for people who have used healthcare services for a long time [63, 64, 76]. For community residents, we support the involvement of formal and informal caregivers in assisting patients to maintain their functional independence [65].
-
(4)
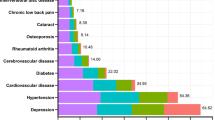
Nation: We find that the disability rate in the US, China, and Spain is around 40% higher than in Norway and Sweden. A serious issue with population aging also exists in China. Due to a mismatch in the availability and demand for healthcare services, China, the world’s largest developing country, has seen a steady increase in the burden of disabilities [66]. Spain also has one of the fastest aging populations in the world [55]. Despite being one of the best countries in the world in terms of economic strength and access to healthcare, the United States has a high rate of disability. There is a clear socioeconomic hierarchy, and those from lower socioeconomic classes have a harder time accessing better healthcare and are more likely to have health status inequalities while coping with serious sickness, according to prior research [67]. The high level of economic development, high level of education, comprehensive social security system, and a substantial proportion of public health spending may all be contributing factors to the low disability rate in places like Norway and Sweden [68].
There was high heterogeneity in this study. The researchers believe that it is related to the inconsistent standards of disability. The most commonly used is the ADL scale, while EQ−5D and Specific disability measures (24 items) have also been studied. Even articles that also use ADL have different criteria for determining disability: The first is any difficulty in basic or using tools can be defined as a disability, and the second recognizes moderate or severe dependence as a disability. In addition, the physical condition of the population, the duration of multiple diseases, and the severity of the disease can all affect the course of disability. People with two or three or more chronic diseases are more likely to become disabled than those with a single chronic disease [69]. This may be related to the deterioration of organ and tissue function exacerbated by multiple diseases. Certain patterns of comorbidities may accelerate and promote negative events. For example, psychosomatic comorbidities are more predictive of disability than other somatic comorbidities and have a higher degree of disability in the former [70,71,72]. Unfortunately, a similar analysis could not be performed in this study.
In recent years, the study of disability-free survival has come to be recognized as a crucial issue in the field of gerontological research [73]. With the prevalence of multimorbidity, the previous single chronic disease management model is no longer adapted to the status quo of multimorbidity. Considering the synergistic and cumulative effects of multimorbidity, countries like the United Kingdom have developed multimorbidity clinical guidelines that emphasize patient-centered healthcare services to enhance health-related quality of life [75]. A multidisciplinary integrated team treatment approach, which may offer the best diagnostic and treatment plan for patients with multimorbidity and lessen the side effects of many drugs [75, 76], has received attention from academics. Additionally, nutritional schedules, exercise recommendations, and other strategies for encouraging healthy living are thought to be effective approaches to prevent or postpone the onset of chronic illnesses and disabilities [74, 76]. Since chronic diseases require long-term care, it is envisioned that community-based staff would be incorporated as a part of the primary healthcare system to establish long-term, stable, and continuous services with the co-patient population. We urge patients to monitor their own health. Additionally, In order to effectively accompany and psychologically assist co-morbid patients, boost their adherence to rehabilitation, and decrease despair and loneliness, we expect that caregivers will be acknowledged as a crucial component of social support.
Strengths and limitations
The strength of this meta-analysis is that it synthesizes disability rates in older adults with multimorbidity, understands the influencing factors that exist, is the first of its kind to the best of our knowledge, and can inform the development of subsequent clinical guidelines. The study’s shortcomings are visible. First, the non-English literature was left out of this study due to language restrictions; second, some studies were not included in the meta-analysis because it was not feasible to extract data from the literature, potentially introducing bias; third, there was a sizable amount of heterogeneity in this study, but it was not brought on by the subgroups.
Conclusion
In conclusion, around 34.9% of older co-morbid patients have varying degrees of disability. Advanced age, female gender, unmarried status, and long-term utilization of healthcare services are all likely significant factors contributing to disability. Through exercise regimens, nutritional advice, and other pharmacological management techniques, we may manage disability. The number and types of co-morbidities, and other factors could not be meta-analyzed due to the limited literature included, and it is anticipated that more high-quality, large-sample, multi-center studies will be carried out in the future to support the theory and serve as a foundation for the clinical development of an integrated, comprehensive, and personalized disease wellness program.
Data availability
No datasets were generated or analysed during the current study.
References
Reyes-Ortiz CA, Lee T, Campo-Arias A et al (2023) Racial discrimination and Multimorbidity among older adults in Colombia: a National Data Analysis. Prev Chronic Dis 20:E34. https://doi.org/10.5888/pcd20.220360
Johnston MC, Crilly M, Black C et al (2019) Defining and measuring multimorbidity: a systematic review of systematic reviews. Eur J Public Health 29(1):182–189. https://doi.org/10.1093/eurpub/cky098
Vetrano DL, Palmer K, Marengoni A et al (2019) Frailty and Multimorbidity: a systematic review and Meta-analysis. J Gerontol Biol Sci Med Sci 74(5):659–666. https://doi.org/10.1093/gerona/gly110
Xue B, Xue Y, Dong F et al (2022) The impact of socioeconomic status and sleep quality on the prevalence of multimorbidity in older adults. Front Public Health 10:959700. https://doi.org/10.3389/fpubh.2022.959700
Forman DE, Maurer MS, Boyd C et al (2018) Multimorbidity in older adults with Cardiovascular Disease. J Am Coll Cardiol 71(19):2149–2161. https://doi.org/10.1016/j.jacc.2018.03.022
World Health Organization (2001) International classification of Functioning. ICF. WHO; Geneva, Switzerland, Disability and Health
Aubert CE, Kabeto M, Kumar N et al (2022) Multimorbidity and long-term disability and physical functioning decline in middle-aged and older americans: an observational study. BMC Geriatr 22(1):910. https://doi.org/10.1186/s12877-022-03548-9
Davies LE, Mercer SW, Brittain K et al (2022) The association between multimorbidity and mobility disability-free life expectancy in adults aged 85 years and over: a modelling study in the Newcastle 85 + cohort. PLoS Med 19(11):e1004130. https://doi.org/10.1371/journal.pmed.1004130
Rizzuto D, Melis RJF, Angleman S et al (2017) Effect of chronic diseases and Multimorbidity on Survival and Functioning in Elderly adults. J Am Geriatr Soc 65(5):1056–1060. https://doi.org/10.1111/jgs.14868
Ballesteros SM, Moreno-Montoya J, Grooten WJA et al (2021) Socioeconomic variation of multimorbidity in Colombian older adults. Sci Rep 11(1):22738. https://doi.org/10.1038/s41598-021-02219-w
Ho HE, Yeh CJ, Cheng-Chung Wei J et al (2023) Association between multimorbidity patterns and incident depression among older adults in Taiwan: the role of social participation. BMC Geriatr 23(1):177. https://doi.org/10.1186/s12877-023-03868-4
Vetrano DL, Roso-Llorach A, Fernández S et al (2020) Twelve-year clinical trajectories of multimorbidity in a population of older adults. Nat Commun 11(1):3223. https://doi.org/10.1038/s41467-020-16780-x
He K, Zhang W, Hu X et al (2021) Relationship between multimorbidity, disease cluster and all-cause mortality among older adults: a retrospective cohort analysis. BMC Public Health 21(1):1080. https://doi.org/10.1186/s12889-021-11108-w
Ryan A, Wallace E, O’Hara P et al (2015) Multimorbidity and functional decline in community-dwelling adults: a systematic review. Health Qual Life Outcomes 13:168. https://doi.org/10.1186/s12955-015-0355-9
Zeng X, Liu H, Chen X et al (2012) Meta analysis series IV: quality evaluation tool for observational research. Chin J Evidence-Bases Cardiovasc Med 4(4):297–299
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605. https://doi.org/10.1007/s10654-010-9491-z
Higgins J, Thomas J, Chandler J et al (2021) Cochrane Handbook for Systematic Reviews of Interventions version 6.2. The Cochrane Collaboration. www.training.cochrane.org/handbook
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558. https://doi.org/10.1002/sim.1186
Pivetta NRS, Marincolo JCS, Neri AL et al (2020) Multimorbidity, frailty and functional disability in octogenarians: a structural equation analysis of relationship. Arch Gerontol Geriatr 86:103931. https://doi.org/10.1016/j.archger.2019.103931
Woo J, Leung J (2014) Multi-morbidity, dependency, and frailty singly or in combination have different impact on health outcomes. Age (Dordr) 36(2):923–931. https://doi.org/10.1007/s11357-013-9590-3
Chamberlain AM, Rutten LJF, Jacobson DJ et al (2019) Multimorbidity, functional limitations, and outcomes: interactions in a population-based cohort of older adults. J Comorb 9:2235042X19873486. https://doi.org/10.1177/2235042X19873486
Liu LH, Kao CC, Wang RH et al (2021) Impacts of multi-morbidity, hemoglobin levels, and frailty on functional disability of older adult residents of long-term care facilities: a structural equation analysis. 21(6):532–537. https://doi.org/10.1111/ggi.14177
Shirazi D, Haudenschild C, Lynch DH et al (2023) Obesity, multiple chronic conditions, and the relationship with physical function: data from the national health and aging trends survey. Arch Gerontol Geriatr 107:104913. https://doi.org/10.1016/j.archger.2022.104913
Bagai A, Ali FM, Gregson J et al (2022) Multimorbidity, functional impairment, and mortality in older patients stable after prior acute myocardial infarction: insights from the TIGRIS registry. Clin Cardiol 45(12):1277–1286. https://doi.org/10.1002/clc.23915
Jędrzejczyk M, Foryś W, Czapla M et al (2022) Relationship between Multimorbidity and Disability in Elderly patients with coexisting Frailty Syndrome. Int J Environ Res Public Health 19(6):3461. https://doi.org/10.3390/ijerph19063461
Marengoni A, von Strauss E, Rizzuto D et al (2009) The impact of chronic multimorbidity and disability on functional decline and survival in elderly persons. A community-based, longitudinal study. J Intern Med 265(2):288–295. https://doi.org/10.1111/j.1365-2796.2008.02017.x
Abizanda P, Romero L, Sánchez-Jurado PM et al (2014) Age, frailty, disability, institutionalization, multimorbidity or comorbidity. Which are the main targets in older adults? J Nutr Health Aging 18(6):622–627. https://doi.org/10.1007/s12603-014-0033-3
Kshatri JS, Palo SK, Bhoi T et al (2020) Associations of multimorbidity on frailty and dependence among an elderly rural population: findings from the AHSETS study. Mech Ageing Dev 192:111384. https://doi.org/10.1016/j.mad.2020.111384
Marengoni A, Akugizibwe R, Vetrano DL et al (2021) Patterns of multimorbidity and risk of disability in community-dwelling older persons. Aging Clin Exp Res 33(2):457–462. https://doi.org/10.1007/s40520-020-01773-z
Schmidt AE, Ilinca S, Schulmann K et al (2016) Fit for caring: factors associated with informal care provision by older caregivers with and without multimorbidity. Eur J Ageing 13(2):103–113. https://doi.org/10.1007/s10433-016-0373-4
Peng X, Bao X, Xie Y et al (2020) The mediating effect of pain on the association between multimorbidity and disability and impaired physical performance among community-dwelling older adults in southern China. Aging Clin Exp Res 32(7):1327–1334. https://doi.org/10.1007/s40520-019-01324-1
Forjaz MJ, Rodriguez-Blazquez C, Ayala A et al (2015) Chronic conditions, disability, and quality of life in older adults with multimorbidity in Spain. Eur J Intern Med 26(3):176–181. https://doi.org/10.1016/j.ejim.2015.02.016
Lee WJ, Peng LN, Lin CH et al (2018) The synergic effects of frailty on disability associated with urbanization, multimorbidity, and mental health. Implications Public Health Med care 8(1):14125. https://doi.org/10.1038/s41598-018-32537-5
Lee Y, Cho CC et al (2021) Examining the effects of multiple chronic conditions on cognitive decline and potential moderators among older koreans: findings from the Korean Longitudinal Study of Ageing 2006–2016. Arch Gerontol Geriatr 95:104424. https://doi.org/10.1016/j.archger.2021.104424
Laan W, Bleijenberg N, Drubbel I et al (2013) Factors associated with increasing functional decline in multimorbid independently living older people. Maturitas 75(3):276–281. https://doi.org/10.1016/j.maturitas.2013.04.005
Wang Z, Peng W, Li M et al (2021) Association between multimorbidity patterns and disability among older people covered by long-term care insurance in Shanghai, China. BMC Public Health 21(1):418. https://doi.org/10.1186/s12889-021-10463-y
Quah JHM, Wang P, Ng RRG et al (2017) Health-related quality of life of older Asian patients with multimorbidity in primary care in a developed nation. Geriatr Gerontol Int 17(10):1429–1437. https://doi.org/10.1111/ggi.12881
Zhang L, Ma L, Sun F et al (2020) A Multicenter Study of Multimorbidity in older adult inpatients in China. J Nutr Health Aging 24(3):269–276. https://doi.org/10.1007/s12603-020-1311-x
Martín Lesende I, Mendibil Crespo LI, Castaño Manzanares S et al (2018) Functional decline and associated factors in patients with multimorbidity at 8 months of follow-up in primary care: the functionality in pluripathological patients (FUNCIPLUR) longitudinal descriptive study. BMJ Open 8(7):e022377. https://doi.org/10.1136/bmjopen-2018-022377
Martin Lesende I, Mendibil Crespo LI, Garaizar, Bilbao et al (2019) Functional decline, mortality and institutionalization after 18 months in multimorbid older persons living in the community: the FUNCIPLUR longitudinal study. Eur Geriatr Med 10(3):523–528. https://doi.org/10.1007/s41999-019-00193-1
Wong CH, Weiss D, Sourial N et al (2010) Frailty and its association with disability and comorbidity in a community-dwelling sample of seniors in Montreal: a cross-sectional study. Aging Clin Exp Res 22(1):54–62. https://doi.org/10.1007/BF03324816
Lynch DH, Petersen CL, Fanous MM et al (2022) The relationship between multimorbidity, obesity and functional impairment in older adults. J Am Geriatr Soc 70(5):1442–1449. https://doi.org/10.1111/jgs.17683
Aarts S, Patel KV, Garcia ME et al (2015) Co-presence of Multimorbidity and disability with Frailty: an examination of heterogeneity in the Frail Older Population. J Frailty Aging 4(3):131–138. https://doi.org/10.14283/jfa.2015.45
Abdulazeez ZU, Grema BA, Michael GC et al (2021) Multimorbidity and Functional Status of the Elderly in a primary care setting of Northern Nigeria: a cross-sectional study. West Afr J Med 38(7):620–628
Li C, Zhou R, Yao N et al (2020) Health Care utilization and unmet needs in Chinese older adults with multimorbidity and functional impairment. J Am Med Dir Assoc 21(6):806–810. https://doi.org/10.1016/j.jamda.2020.02.010
Storeng SH, Vinjerui KH, Sund ER et al (2020) Associations between complex multimorbidity, activities of daily living and mortality among older norwegians. A prospective cohort study: the HUNT Study, Norway. BMC Geriatr 20(1):21. https://doi.org/10.1186/s12877-020-1425-3
Koroukian SM, Murray P, Madigan E (2006) Comorbidity, disability, and geriatric syndromes in elderly cancer patients receiving home health care. J Clin Oncol 24(15):2304–2310. https://doi.org/10.1200/JCO.2005.03.1567
Boeckxstaens P, Vaes B, Legrand D et al (2015) The relationship of multimorbidity with disability and frailty in the oldest patients: a cross-sectional analysis of three measures of multimorbidity in the BELFRAIL cohort. Eur J Gen Pract 21(1):39–44. https://doi.org/10.3109/13814788.2014.914167
Collins DM, Downer B, Kumar A et al (2018) Impact of multiple chronic conditions on Activity limitations among older Mexican-American Care recipients. Prev Chronic Dis 15:E51. https://doi.org/10.5888/pcd15.170358
Grov EK, Fosså SD, Dahl AA (2017) A controlled study of the influence of comorbidity on activities of daily living in elderly cancer survivors (the HUNT-3 survey). J Geriatr Oncol 8(5):328–335. https://doi.org/10.1016/j.jgo.2017.05.007
Yokota RT, Van der Heyden J, Nusselder WJ et al (2016) Impact of chronic conditions and multimorbidity on the disability Burden in the older Population in Belgium. J Gerontol Biol Sci Med Sci 71(7):903–909. https://doi.org/10.1093/gerona/glv234
Zheng PP, Guo ZL, Du XJ et al (2022) Prevalence of disability among the Chinese older Population: a systematic review and Meta-analysis. Int J Environ Res Public Health 19(3):1656. https://doi.org/10.3390/ijerph19031656
Castellanos-Perilla N, Borda MG, Fernández-Quilez Á et al (2020) Factors associated with functional loss among community-dwelling Mexican older adults. Biomedica 40(3):546–556. https://doi.org/10.7705/biomedica.5380
Gu D, Andreev K, Dupre ME (2021) Major trends in Population Growth around the World. China CDC Wkly 3(28):604–613. https://doi.org/10.46234/ccdcw2021.160
Carmona-Torres JM, Rodríguez-Borrego MA, Laredo-Aguilera JA et al (2019) Disability for basic and instrumental activities of daily living in older individuals. PLoS ONE 14(7):e0220157. https://doi.org/10.1371/journal.pone.0220157
Hao L, Xu X, Dupre ME et al (2020) Adequate access to healthcare and added life expectancy among older adults in China. BMC Geriatr 20(1):129. https://doi.org/10.1186/s12877-020-01524-9
Sinclair AJ, Abdelhafiz AH (2022) Multimorbidity, Frailty and Diabetes in Older people-identifying interrelationships and outcomes. J Pers Med 12(11):1911. https://doi.org/10.3390/jpm12111911
Yau PN, Foo CJE, Cheah NLJ et al (2022) The prevalence of functional disability and its impact on older adults in the ASEAN region: a systematic review and meta-analysis. Epidemiol Health 44:e2022058. https://doi.org/10.4178/epih.e2022058
ZHU X, ZHANG Y, LIU H( (2019) Prevalence and influencing factors of disability among the elderly in China. Chin J Public Health 35(7):917–920
Pang J, Xu S, Wu Y (2023) Effect of widowhood on the risk of disability among the elderly in China. Front Psychiatry 14:1169952. https://doi.org/10.3389/fpsyt.2023.1169952
Abdi S, Spann A, Borilovic J et al (2019) Understanding the care and support needs of older people: a scoping review and categorisation using the WHO international classification of functioning, disability and health framework (ICF). BMC Geriatr 19(1):195. https://doi.org/10.1186/s12877-019-1189-9
Jiao D, Watanabe K, Sawada Y et al (2021) Multimorbidity and functional limitation: the role of social relationships. Arch Gerontol Geriatr 92:104249. https://doi.org/10.1016/j.archger.2020.104249
Friedrich B, Elgert L, Eckhoff D et al (2023) A system for monitoring the functional status of older adults in daily life. Sci Rep 13(1):12396. https://doi.org/10.1038/s41598-023-39483-x
Mugica-Errazquin I, Zarrazquin I, Seco-Calvo J et al (2021) The nutritional status of long-term institutionalized older adults is Associated with Functional Status, physical performance and activity, and Frailty. Nutrients 13(11):3716. https://doi.org/10.3390/nu13113716
Falck RS, Percival AG, Tai D et al (2022) International depiction of the cost of functional independence limitations among older adults living in the community: a systematic review and cost-of-impairment study. BMC Geriatr 22(1):815. https://doi.org/10.1186/s12877-022-03466-w
Guo Y, Wang T, Ge T et al (2022) Prevalence of self-care disability among older adults in China. BMC Geriatr 22(1):775. https://doi.org/10.1186/s12877-022-03412-w
Zaninotto P, Batty GD, Stenholm S et al (2020) Socioeconomic inequalities in disability-free life expectancy in older people from England and the United States: a cross-national Population-based study. J Gerontol Biol Sci Med Sci 75(5):906–913. https://doi.org/10.1093/gerona/glz266
Clarsen B, Nylenna M, Klitkou ST et al (2022) Changes in life expectancy and disease burden in Norway, 1990–2019: an analysis of the global burden of Disease Study 2019. Lancet Public Health 7(7):e593–e605. https://doi.org/10.1016/S2468-2667(22)00092-5
Quiñones AR, Markwardt S, Botoseneanu A (2016) Multimorbidity combinations and disability in older adults. J Gerontol Biol Sci Med Sci 71(6):823–830. https://doi.org/10.1093/gerona/glw035
Jacob ME, Ni P, Driver J et al (2020) Burden and patterns of Multimorbidity: impact on disablement in older adults. Am J Phys Med Rehabil 99(5):359–365. https://doi.org/10.1097/PHM.0000000000001388
Wang XX, Lin WQ, Chen XJ et al (2017) Multimorbidity associated with functional independence among community-dwelling older people: a cross-sectional study in Southern China. Health Qual Life Outcomes 15(1):73. https://doi.org/10.1186/s12955-017-0635-7
Shi Z, Zhang Z, Shi K et al (2022) Association between multimorbidity trajectories and incident disability among mid to older age adults: China Health and Retirement Longitudinal Study. BMC Geriatr 22(1):741. https://doi.org/10.1186/s12877-022-03421-9
Neumann JT, Thao LTP, Murray AM et al (2022) Prediction of disability-free survival in healthy older people. Geroscience 44(3):1641–1655. https://doi.org/10.1007/s11357-022-00547-x
Pan C, Cao N, Kelifa MO et al (2023) Age and cohort trends in disability among Chinese older adults. Front Public Health 11:998948. https://doi.org/10.3389/fpubh.2023.998948
Salisbury C, Man MS, Bower P et al (2018) Management of multimorbidity using a patient-centred care model: a pragmatic cluster-randomised trial of the 3D approach. Lancet. 2018;392(10141):41–50. https://doi.org/10.1016/S0140-6736(18)31308-4
Huang Y, Zhang L, Huang X et al (2020) Potentially inappropriate medications in Chinese community-dwelling older adults. Int J Clin Pharm 42(2):598–603. https://doi.org/10.1007/s11096-020-00980-y
Funding
Our study was supported by a Fund from the Sichuan Provincial Science and Technology Department (2023YFS0068).
Author information
Authors and Affiliations
Contributions
Study Design: Jin Zhang, Yan Sun. Data extraction and Collection: Jin Zhang, AiYing Li. Data Analysis and Interpretation: Jin Zhang, Yan Sun. Manuscript Writing: Jin Zhang.The first draft of the manuscript was written by Jin Zhang and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Informed consent
Not applicable.
Competing interests
We claim that there is no conflict of interest in this paper that would affect the results of the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, J., Sun, Y. & Li, A. The prevalence of disability in older adults with multimorbidity: a meta-analysis. Aging Clin Exp Res 36, 186 (2024). https://doi.org/10.1007/s40520-024-02835-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40520-024-02835-2