Abstract
Healthcare systems challenged by chronic workforce shortages use task shifting and task sharing as tools to transfer certain services from providers with a high skill base to providers typically with fewer skills or qualifications. The World Health Organization’s global guidelines on task shifting advised countries to develop regulatory and implementation frameworks to expand task shifting for urgent public health issues. These frameworks direct, structure and support interventions by considering various factors that may affect their success. This paper outlines the process undertaken to develop a new implementation framework for task shifting and sharing, called the SHIFT-SHARE. We describe the framework and discuss our next steps to validate and refine it. SHIFT-SHARE draws on change management theories, particularly those of Lewin and Kotter, along with Lean Thinking and Diffusion of Innovation theory. It is further complemented by theoretical constructs of popular implementation frameworks, such as the Practical, Robust Implementation and Sustainability Model, Consolidated Framework for Implementation Research, Calderdale Framework and others. SHIFT-SHARE has six cyclical stages, namely (1) Environmental Scanning, (2) Priming, (3) Risk Signal, (4) Capacity Building, (5) Monitoring and Evaluation, and (6) Maintenance and Diffusion. Clinical safety, patient-centredness, ethical considerations and stakeholder feedback underpin every stage of SHIFT-SHARE. Following further development and refinement, our hope is that this framework can be used as a strategic planning tool to systematically redistribute tasks between different cadres of care providers, optimise resource usage, improve care access and quality, and introduce stability in service provision.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Meeting the healthcare needs and demands of populations in the context of low or stretched healthcare budgets and inadequate numbers of skilled providers is a huge challenge for countries worldwide. Projections of global deficits of human resources for healthcare (HRH) by 2035 range between 12.9 and 18 million providers (Campbell et al., 2013; Limb, 2016), with low- and middle-income countries expected to be the most impacted. While national Governments and international agencies, such as the World Health Organization (WHO) offer stewardship to strengthen systems, frontline healthcare professionals, caregivers, service managers, leaders of organisations, sponsors of healthcare programmes, and stakeholders share the overarching responsibility of building capacity and resilience, and ensuring that care is safe, of high quality, and equitable. Volume, composition, and distribution of HRH and its associated systematic planning are key to dispensing services and achieving broader healthcare goals. Proficiencies of HRH, rational skill-mixing, coordination, and collaboration between HRH are central tenets of health services delivery. Systems can maximise impact and minimise wastage through well-planned usage of available HRH, infrastructure, and financial resources (Monden, 1983). Modifying workforce organisation, sharing responsibilities or shifting tasks among cadres can provide stopgap solutions to handle system shocks, as seen during the Coronavirus disease pandemic (Das et al., 2023). These strategies can also be used to strengthen systems gradually by eliminating HRH wastage, reducing burden, and improving quality, access, and experiences, as witnessed with the human immunodeficiency virus (HIV) epidemic management in sub-Saharan Africa (Lunsford et al., 2019).
Task shifting and sharing (TS/S) are mechanisms to rationally redistribute specific services or responsibilities among HRH, particularly in low-resource settings. Often used synonymously, task shifting and task sharing entail slightly different approaches. The WHO defines task shifting as the movement of tasks, wherever appropriate, from specialised HRH to staff with lesser training or qualifications (World Health Organization, 2008). Task sharing on the other hand is not as territorial and follows a team-based approach, where care is provided by a mix of HRH rather than a single cadre, thereby allowing teams to collaborate and expand on roles (Tsui et al., 2017). Both approaches aim to expand workforce capacity, sustain and improve care access and quality, improve patient and provider experiences, relieve overburdened staff, and scale services, thereby strengthening systems overall (World Health Organization, 2008). TS/S may transfer responsibilities completely from one cadre to another, for example, shifting mental health screening from psychologists and psychiatrists to nurses and community healthcare workers (Singla et al., 2021). Conversely, TS/S may involve transferring parts of a service from one cadre to another, for example, clinical assistants/officers performing routine procedures in lieu of specialists in hospitals (Kuhlmann et al., 2021). TS/S can also move tasks from humans to digital technologies by shifting data collection, analysis, communication, and decision-making to online systems and technological aides. Thorough characterisation of tasks to be shifted or shared, identification of process enablers and barriers, and evaluation of the usefulness of TS/S are key to the overall process.
In 2008, the WHO published its landmark report titled Task shifting: Rational redistribution of tasks among health workforce teams – Global recommendations and guidelines (World Health Organization, 2008). This report produced the first authoritative guidelines on task shifting and advised countries to expand on this approach in order to improve access to HIV care and other services in contexts where workforce shortage had been rate-limiting in providing antiretroviral therapy. Evidence synthesised from commissioned research, country consultations, and stakeholder interviews in Ethiopia, Malawi, Namibia, Uganda, and other sub-Saharan countries culminated into 22 recommendations. These included suggestions on carrying out situational analyses, stakeholder consultations, and endorsements through the production of policy and implementation frameworks at national levels (World Health Organization, 2008).
Frameworks and the theories that underpin these frameworks are key to service implementation and research as they offer constructs to study underlying phenomena, predict consequences, direct decision-making and action, and make processes efficient. Terms framework, theory, and model, are often used interchangeably. While these concepts borrow principles from one another, they are distinct. A theory is a set of definitions that illuminates fundamental concepts or phenomena. Simply put, theories explain what is happening conceptually, why, and how (Nilsen, 2015). For example, theories can inform how a new intervention is adopted by one sub-group of a population and then spread across to others. Popular theories in implementation sciences include those with a focus on change management, such as Lewin’s Three-stages of change (Galli, 2018), Kotter’s Eight-step process of leading change (Kotter, 2007), principles of lean management (Monden, 1983), and theory of diffusion of innovation (Rogers et al., 2019).
Frameworks are generally more focused and specific and provide a roadmap for implementing theory- and evidence-based interventions in real-world situations. Frameworks can help evaluate needs, prime systems to change, engage stakeholders, and monitor progress. Implementation frameworks, in particular, can enable navigation through complex processes of healthcare delivery, factoring in characteristics of the intervention itself, the organisation, the workforce, process enablers and hinderers, needs, preferences, and values of stakeholders, the local context, and the broader socioeconomic and political environment (Nilsen, 2015). Implementation frameworks are generally built using multiple theories, in a manner that each may inform parts of the framework. They can be used to identify contextual barriers and facilitators for a programme or to strategise around the sustainability of a service beyond its pilot. Popular implementation frameworks include the Reach, Effectiveness–Adoption, Implementation and Maintenance (RE-AIM) (Glasgow et al., 2019), the Practical, Robust Implementation and Sustainability Model (PRISM) (Feldstein & Glasgow, 2008), the Consolidated Framework for Implementation Research (CFIR) (Damschroder et al., 2022), and the Calderdale framework (Smith & Duffy, 2010). Organisations and individual providers, including practitioners, leaders, managers, policy-makers and scholars use frameworks to ground services and policies in evidence. A systematic evidence-based approach helps increase the adoption, effectiveness and sustainability of an intervention, and ultimately benefit patients, HRH, and the broader population (Brownson et al., 2017).
The third recommendation of the WHO report on task shifting stated that, in the case of HIV services, “countries deciding to adopt the task shifting approach should define a nationally endorsed framework that can ensure harmonisation and provide stability for the HIV services that are provided throughout the public and non-state sectors. Countries should also explore a framework for the exploration of task shifting to meet other critical public health needs” (World Health Organization, 2008, p. 3). More broadly, it postulated that national frameworks specific for task shifting and by extension task sharing, have the potential to provide a systematic structure for reorganising care delivery through workforce expansion, adoption of quality assurance mechanisms, and generation of accountability. Frameworks can enhance care quality and build consistency in care standards across a system, irrespective of differences that may exist at individual organisation or provider levels, thereby making service delivery more stable. Furthermore, national-level frameworks on TS/S can catalyse the integration of public-private partnerships in service delivery, despite initial challenges of standardising practices and the resistance that can come from non-state stakeholders (World Health Organization, 2008). Indeed, frameworks help factor key constructs and variables that can affect the success of TS/S. Work by Orkin et al. (2021) on the Concepts and Opportunities to Advance Task Shifting and Task Sharing (COATS) framework, indicated implementation criteria for when to engage the approach. However, implementation-specific frameworks for how to undertake TS/S are still lacking. Therefore, we conceptualised and are in the process of piloting and refining a new implementation framework for TS/S that offers step-by-step direction on how to operationalise TS/S that we believe will address vital aspects of healthcare service management, such as evaluating needs, facilitating change, building resources and support, mitigating risks, assessing effectiveness, sustaining care, and continuous improvement.
Methodology for Developing the Framework
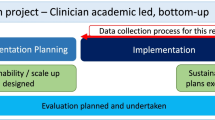
This section describes our overarching approach to developing our implementation framework for TS/S. Our approach can be broken down into the following six phases:
Defining the Scope
We began building our framework by articulating its scope and purpose (see Fig. 1). The purpose of this initial step of framework development was to offer systematic direction on how to identify the need and preparedness for TS/S. This included how to operationalise TS/S and build supporting structures, how to assess risks and impact, and how to sustain and scale TS/S in a system while focusing on workforce and resource optimisation, quality improvement, and cost-effectiveness.
Reviewing of Literature
We carried out a narrative review to identify change management theories, implementation frameworks, and tools relevant to TS/S, exploring disciplines within healthcare management, such as organisational behaviour, health policy, and operational management. We developed a query using the following terms and their variations: (change management OR implementation frameworks OR theories OR models) AND (healthcare OR health service management OR organisational behaviour OR health policy) and searched for articles across PubMed, Global Health, CINAHL, and Google Scholar in April 2023. We found 2,563 articles from this search. We screened these by examining their titles and abstracts and removed duplicates and irrelevant articles. SD performed the initial screening to identify articles that described, used, or referred to theories, frameworks, and tools relevant to task redistribution and were adaptable, measurable in terms of outcomes, and practically useful for guidance. Subsequently, LG and DW reviewed the results of this screening to ensure that the selection aligned with the scope of our implementation framework for TS/S. Ultimately, we selected five change management theories, namely Lewin’s Three-stage Model and Force Field Analysis (Galli, 2018), Kotter’s Eight-step Process of Leading Change (Kotter, 2007), Lean Management (Monden, 1983), and Diffusion of Innovation (Rogers et al., 2019); four implementation frameworks, namely the RE-AIM (Glasgow et al., 2019), PRISM (Feldstein & Glasgow, 2008), CFIR (Damschroder et al., 2022), and the Calderdale Framework (Smith & Duffy, 2010); and two quality improvement frameworks, namely the Quality Health Services Framework (World Health Organization, 2020) and the Model for Improvement (Langley et al., 2009). We also reviewed five programme assessment tools, including the National Health Service’s Health Needs Assessment (Cavanagh & Chadwick, 2005; Hooper & Longworth, 2002), Organisational Readiness for Implementing Change (Shea et al., 2014; Weiner, 2009), the Change Management Toolkit by the University of California Berkley (Sarran et al., 2011), the Risk Assessment Matrix (Rausand & Haugen, 2020), and the Cost-benefit Analysis (Harvard Business School Online, 2019).
Each of these was assessed to understand their applicability in the context of TS/S. Parameters such as clarity of terms were examined to gauge their ability to communicate concepts. Relevance was assessed to determine how well each addressed the processes of task redistribution. Flexibility was considered to examine their adaptability to different settings, especially in light of TS/S. Measurability was also a parameter, focusing on the capacity of each framework or tool to track progress and outcomes. Additionally, we examined their usefulness in practical implementation, emphasising their ability to provide actionable guidance. These parameters collectively guided our evaluation and helped us identify the strengths and weaknesses of each and inform the development of our framework. For example, we concluded that one major strength of the Calderdale Framework (Smith & Duffy, 2010) lies in its structured approach to task Analysis, which facilitates objective discussions on skills, rules and knowledge, enabling risk identification and mitigation in HRH development while ensuring cost-benefit considerations.
Characterising the Core Components of the Framework
Based on our review, we identified constructs or core components that, in our opinion, represented the essential concepts or principles fundamental to the effective implementation of TS/S. Once we identified these constructs, SD took the lead in drafting the initial framework, organising the identified components according to their intended structure and function. This draft served as a starting point, outlining how different constructs would fit together. LG and DW analysed this draft and provided feedback. Through iterative discussions within the team, we made modifications to ensure that our framework captured all constructs in a logically structured manner to meet the specific needs and challenges of TS/S. Initially conceptualised as linear, we recognised the need for continuous assessment and improvement of TS/S over time and transformed the framework into a cyclical format. We present the outcomes of this exercise in the subsequent sections of this paper as a detailed description of the framework and its components. As of March 2024, we have completed phases A through C of the framework development process and have commenced with phase D (see Fig. 1).
Engaging Stakeholders to Gather User Feedback
The subsequent steps involve engaging diverse groups of stakeholders and analysing their perspectives on our framework. This study, led by SD as part of his doctoral research, is currently underway in India and will continue until around September 2024. It involves conducting semi-structured interviews, focus group discussions, and non-participative participant observations with both public and private sector stakeholders. Using convenience sampling and snowballing techniques, we now estimate to be able to recruit over 100 participants from 20 different healthcare organisations and academic institutions across India. India was chosen due to its large population and acute workforce shortages, making it crucial for examining TS/S. Our study seeks participants from various domains of healthcare, including primary care, cardiovascular care, emergency care, newborn care, surgical services, geriatric care, mental health, health education, and other areas. This diverse participant base ensures a wide range of experiences are captured, providing a comprehensive understanding of TS/S in Indian healthcare. Participants include those onto whom tasks are shifted or shared, those from whom tasks are transferred, service managers, trainers, auditors, organisational leaders, representatives of professional associations, funders, subject matter experts, policymakers, government decision-makers, patients, and patient interest group representatives. The detailed protocol and thematic topic guides for the interviews and focus group discussions have been registered and are available to view (Das et al., 2023). The primary aim of this qualitative exercise is to test whether interventions adhere to our framework’s principles, study activities corresponding to its components and identify facilitators and barriers to implementation. To achieve this, we take a two-fold approach. Firstly, we assess the alignment between stakeholder practices and our framework through semi-structured interviews and non-participative participant observations. During these interactions, participants are kept blind to the specifics of the framework to avoid potential biases, allowing us to obtain an objective understanding of their practices. Secondly, at focus group discussions, we present our framework to stakeholders and seek specific feedback on the feasibility and applicability of its individual components based on their experiences, contexts, and workflows. This offers insights into their expectations and helps identify enablers and barriers.
Refining and Finalising the Framework
The primary data generated via the interviews, focus group discussions, and participant observations from the study underway in India will be analysed thematically using a hybrid deductive-inductive approach (Xu & Zammit, 2020) and learnings from this will help fine-tune characteristics of our framework. We will make modifications as informed by data and add resources as needed. Additionally, we will formulate a guideline document to be used while implementing the framework.
Disseminating and Implementing the Framework
The last phase of the development process will be to create a communication and dissemination strategy to promote the framework among relevant state and non-state stakeholders, including healthcare organisations, providers, policymakers, decision-makers, researchers, professional associations, and regulatory agencies. We will highlight the benefits and potential impact of adopting our framework through publications and presentations. Collaborating with key stakeholders will be crucial to foster the adoption and improvement of the framework.
Core Components of the SHIFT-SHARE
Our work so far has enabled us to conceptualise a new framework specific for TS/S. We named this the Strategic Healthcare Implementation Framework for Task Shifting, Sharing, and Resource Enhancement or SHIFT-SHARE (see Fig. 2). Our framework is structured around a cyclical sequence comprising six stages. Each stage presents an important phase in TS/S and is characterised by a set of interrelated core components. The stages and their respective constituent components are summarised below.
Environmental Scan
The first stage involves examining the environment within which TS/S is being planned. To do this and to execute other stages of SHIFT-SHARE at national, organisational, or practice levels, first, organisations must form a team that can lead through the different stages of change, as suggested by Lewin (Galli, 2018), Kotter (Kotter, 2007), and by toolkits on health needs assessment (Cavanagh & Chadwick, 2005; Hooper & Longworth, 2002) and change implementation (Sarran et al., 2011). This team can include people committed to change, familiar with the health issue of focus, and working at different hierarchies. An environmental scan consists of a complete needs assessment. This builds on the advice of the National Health Service, UK, (Hooper & Longworth, 2002) and requires that patient needs, preferences, values, workforce needs, and process needs, are all evaluated using patient and carer inputs. The team also needs to examine which services are required given the context and severity of the health issue, what support HRH needs to deliver these, and whether TS/S will enable them to do so. An assessment of whether sudden internal or external events have necessitated TS/S should be made (Damschroder et al., 2022; Feldstein & Glasgow, 2008; Glasgow et al., 2019).
The Environmental scan should include a readiness assessment, which will examine whether the organisation planning to employ TS/S has the financial and infrastructural capacity to do so and whether there is enough workforce availability, in terms of number and staff-time, to initiate TS/S; and if not, what additional capacity needs to be created. The bandwidth of available resources and situational factors, such as organisational culture and politics, are key determinants of the success of TS/S (Damschroder et al., 2022; Feldstein & Glasgow, 2008; Glasgow et al., 2019). Change Management has shown that the more a workforce values change and understands the change process, the stronger they will engage with its implementation (Weiner, 2009). Evaluating whether the workforce is open and committed to the changes that TS/S will introduce, as well as identifying whether there is enough political will (from organisational level to national levels) to support TS/S are important stages. Readiness can be assessed through surveys, as prescribed by Shea et al. (2014).
Priming
Priming is a stage of preparing the system and stakeholders for changes. This begins with task analysis, whereby the team can perform a current-state analysis to study what processes and workflows are used to deliver care presently, finalise tasks to be shifted or shared, and examine whether the HRH participating in TS/S have the required skillsets, and if not, how to identify what additional competencies are required. This approach corresponds to stages of service analysis and competency analysis of the Calderdale framework (Smith & Duffy, 2010). Concurrently, the team can initiate communication and collaboration. The stances of patients, HRH, managers, and other stakeholders on TS/S and their concerns can be carefully reviewed through stakeholder engagement and analysis (Sarran et al., 2011). Kotter (Kotter, 2007) advises that there is value in conveying a sense of urgency to employ TS/S, reasons and goals of engaging it, expected benefits, outcomes, and all anticipated changes to all stakeholders. Transparent communication will empower stakeholders and put them on the path to accept and act on changes.
Risk Signals
This stage involves two major steps – risk identification and risk mitigation. This stage aims to identify and assess potential hazards and introduce appropriate control measures to eliminate or reduce potential harm to people, the environment, and other resources (Rausand & Haugen, 2020). It is good practice to install mechanisms to identify and report risk and hazard indicators associated with TS/S and evaluate their potential impacts on patient safety, HRH safety or infrastructure. These measurements can quantify the likelihood of occurrences (or frequencies) and estimated severities. Organisations can use these indicators to prioritise the addressing of risks and develop practical response plans on how to monitor and mitigate these alongside the implementation of TS/S. It is equally crucial to periodically review the risk assessment and response plans, to ensure effective overall risk management (Rausand & Haugen, 2020).
Capacity Building
Providing focused competency-based training to all staff is critical to achieving successful change management (Galli, 2018; Kotter, 2007; Monden, 1983) and positive health outcomes (Damschroder et al., 2022; Feldstein & Glasgow, 2008; Glasgow et al., 2019; Langley et al., 2009; Smith & Duffy, 2010; World Health Organization, 2020). Proper training and mentorship can create new cadres of proficient providers, who are confident and committed to undertaking TS/S safely and efficiently. By this stage of implementation, it is necessary to have identified provider competencies essential for performing delegated tasks. Workers should now be exposed to modules designed to equip them with these skill sets. Capacity building is rarely a singular activity, thus continuous training through refresher courses and knowledge upgradation sessions are important. Cadres undertaking TS/S need to be continuously supervised and provided with constructive feedback (Smith & Duffy, 2010; World Health Organization, 2020). Cadres taking on new tasks must know their responsibilities and rights (Smith & Duffy, 2010; World Health Organization, 2020) so that there is individual accountability at provider levels.
Support systems should be in place for facilitating TS/S. Systemic changes require active leadership, as well as administrative and technological support (Damschroder et al., 2022; Feldstein & Glasgow, 2008; Glasgow et al., 2019; Smith & Duffy, 2010). Alongside revising governance structures, other supports such as administrative and technological support, medical equipment, and information systems should be made available as needed. Moreover, since TS/S involves modifications to task flows and protocols, it is important to ensure that planned TS/S does not face regulatory blocks. Local and national regulatory environments, featuring policies, practice guidelines, accreditations, financial incentives, and societal and market pressures must be reviewed (Damschroder et al., 2022; World Health Organization, 2020). Collaborations with professional bodies and academic institutions may prove beneficial, as they could give regulatory support and additionally, create funding opportunities.
Monitoring and Evaluation
This stage involves the systematic tracking and analysis of quality and safety indicators to evaluate the impact and effectiveness of TS/S. Monitoring and evaluation is a continuous process and indispensable in quality improvement (Damschroder et al., 2022; Feldstein & Glasgow, 2008; Glasgow et al., 2019; Langley et al., 2009; Monden, 1983; Smith & Duffy, 2010; World Health Organization, 2020). Those implementing TS/S should identify measurable process indicators and outcome indicators (Langley et al., 2009; World Health Organization, 2020) with respect to TS/S and regularly monitor these to determine whether TS/S is achieving intended goals. Data on indicators can be quantitative and qualitative and can be collected through routine data collection or via observations, interviews, surveys or feedback analysis (Damschroder et al., 2022; Feldstein & Glasgow, 2008; Galli, 2018; Glasgow et al., 2019; Langley et al., 2009; World Health Organization, 2020). Levels of service coverage and access, quality of care, patient satisfaction, workforce satisfaction, and cost-effectiveness are example performance indicators for TS/S. Simultaneously, it is necessary to probe whether TS/S has led to any unintended consequences in the system or in other dependent systems, directly or indirectly (Glasgow et al., 2019; Langley et al., 2009). Furthermore, the team leading the implementation may benefit from investigating instances where TS/S has been implemented and then intentionally or naturally reversed back (Feldstein & Glasgow, 2008). This will inform them of factors that can potentially cease TS/S.
Maintenance and Diffusion
When changes such as TS/S lead to successful outcomes that are reproducible, support should be given to embedding these new ways of working into practices and policies (Feldstein & Glasgow, 2008; Smith & Duffy, 2010). There will always be a risk that systems revert to pre-implementation states, especially if these were seen as having narrower, more controllable or manageable parameters. Plans to create operational and financial sustainability and scalability for TS/S should therefore be developed, alongside ways to keep cadres motivated and incentivised to carry out modified practices. It will be valuable to chart out strategies to strengthen infrastructure and generate finances to sustain TS/S (Feldstein & Glasgow, 2008; Smith & Duffy, 2010). As outlined in this framework, diffusion of TS/S knowledge and experiences from one system to another is key to scaling (see Fig. 2). Stakeholders are more likely to adopt a change such as TS/S, when its relative advantage compared to usual practice, its compatibility with the needs and values of the system, and its ability to generate tangible results are communicated to them effectively (Rogers et al., 2019). Sharing knowledge and assessing whether it alters stakeholder attitudes towards TS/S, is fundamental to driving quality improvement (Feldstein & Glasgow, 2008; World Health Organization, 2020). Diffusion will help spread TS/S to comparable contexts, where instead of reinventing the wheel, TS/S-based models of care can be contextualised and replicated.
Post completion of the sixth stage, another cycle of SHIFT-SHARE can begin. The rationale for SHIFT-SHARE to be cyclical is that it allows an implementing team to revisit aspects of implementation which can still be enhanced to improve the quality and effectiveness of TS/S (Langley et al., 2009; Monden, 1983; World Health Organization, 2020), and in the process identify other tasks or services which could be delegated.
Discussion
We are continuing to refine the SHIFT-SHARE with the goal of providing an implementation framework designed to operationalise TS/S. SHIFT-SHARE derives its philosophy and structure from several change management and implementation theories, frameworks, and tools. Once fully developed, we believe it can be adapted to settings as per specific needs and used by health system stakeholders worldwide. Once finalised, we believe SHIFT-SHARE could address the WHO’s recommendation to develop a harmonising framework for TS/S, providing beneficial support to organisations considering employing TS/S within their care models.
SHIFT-SHARE aspires to provide a practical roadmap and template for designing and executing TS/S-based interventions. The framework aims to offer a conceptual structure that will standardise processes across different settings, ensuring that those implementing TS/S adhere to best practices. Once refined and finalised, SHIFT-SHARE could be particularly beneficial for low-resource settings dealing with reduced workforces. We hope that, through successful implementation, service access will improve by maximising the available HRH skill-mixes, complemented with training, empowerment, and increased worker satisfaction. Our vision is for SHIFT-SHARE to inspire implementers to replicate or scale successful TS/S-based models to larger demographics.
The framework has the potential to become instrumental for research and development. One significant challenge that SHIFT-SHARE and its associated terminologies seek to address is the need for consistency in the language used to define goals, explain concepts and processes and report outcomes and challenges related to TS/S. We believe this could foster agreement and collaboration on TS/S beyond academia. Our goal is for SHIFT-SHARE to serve as a foundation to stimulate innovation in TS/S. For example, by enabling the establishment of baseline data and ensuring the seamless flow of this data through a change process, it could offer researchers opportunities to conceptualise studies on TS/S and investigate its impact on the quality, accessibility, or cost-effectiveness of services. It could also help identify additional tasks or services that can be shifted or shared and suggest efficient methods to do so.
We have purposefully integrated clinical safety, patient-centeredness, and ethical considerations into every stage of SHIFT-SHARE. Although TS/S can be seen as a mechanism for cost reduction and efficiency improvement, we envision that SHIFT-SHARE should only be employed when systematic evidence supports that TS/S involving less-qualified HRH leads to clinically safe outcomes. It will be important for the health issues addressed by TS/S to be relevant to the target population to ensure acceptance. Future implementations should prioritise patient participation in the planning, implementation, and evaluation of TS/S, especially in community-based care models, as their involvement will help tailor services to community needs and foster appreciation of TS/S benefits. There may be ethical concerns, such as the risk of exposing patients to lower-quality care or exploiting less-qualified HRH to meet demands (Mundeva et al., 2018). Therefore, it will be crucial to upgrade the skills of cadres involved in TS/S, respect patient rights and grievances, and ensure the welfare of HRH through fair compensation and protection against exploitation. The team adopting SHIFT-SHARE should also establish structures to collect and review feedback from patients, HRH, and other stakeholders at every stage of the cycle.
We further recognise that once fully developed, the SHIFT-SHARE framework may be too exhaustive for certain settings with very limited financial, infrastructural, or workforce capacities. In such cases, teams managing task redistributions will need to adapt the approach following thorough stakeholder consultations. They may need to prioritise and phase in specific components of SHIFT-SHARE over time as resources permit. It will be important to contextualise SHIFT-SHARE to available resources and continuously review the relevance and effectiveness of TS/S. This will help ensure better service planning and implementation in low-resource settings.
Conclusion
We are piloting and refining a new strategic framework for TS/S, called the SHIFT-SHARE, that we have based on change management theories and healthcare implementation frameworks. Upon further development and finalisation, we believe that SHIFT-SHARE will have the potential to offer step-by-step guidance on how to design and employ TS/S within existing services or while building new interventions. Each of the six stages of SHIFT-SHARE is being designed to be adaptable, facilitating the expansion of TS/S, especially in low-resource settings. We anticipate that its application will assist systems in reorganising services and reassigning tasks between different cadres of HRH to maximise workforce productivity, optimise resource usage, save costs, and improve care access and quality. By paving the way for systematic task redistribution, we aim for SHIFT-SHARE to help strengthen interprofessional collaboration and learning, empower less-qualified HRH in their professional roles, and introduce stability in service provision, especially in settings facing workforce crises. However, we acknowledge that contextual rules and regulations, interprofessional power dynamics and prevalent sociocultural norms may slow down the adoption of SHIFT-SHARE. In the subsequent phases of framework development, we are conducting qualitative interviews, focus group discussions, and participant observations to evaluate the validity, applicability and, real-world utility of SHIFT-SHARE. The evidence synthesised from these analyses will be crucial in helping us finalise the framework.
References
Brownson, R. C., Colditz, G. A., & Proctor, E. K. (2017). Dissemination and implementation research in health: Translating science to practice, second edition. In Dissemination and Implementation Research in Health: Translating Science to Practice, Second Edition. https://doi.org/10.1093/oso/9780190683214.001.0001
Campbell, J., Dussault, G., Buchan, J., Pozo-Martin, F., Guerra Arias, M., Leone, C., Siyam, A., & Cornetto, A. (2013). A universal truth: No health without a workforce. In World Health Organization. https://www.who.int/publications/m/item/hrh_universal_truth
Cavanagh, S., & Chadwick, K. (2005). Health needs assessment: A practical guide. National Institute Fo Clinical Excellence.
Damschroder, L. J., Reardon, C. M., Widerquist, M. A. O., & Lowery, J. (2022). The updated Consolidated Framework for Implementation Research based on user feedback. Implementation Science, 17(1), 75. https://doi.org/10.1186/s13012-022-01245-0
Das, S., Grant, L., & Fernandes, G. (2023a). Task shifting healthcare services in the post-COVID world: A scoping review. PLOS Global Public Health, 3(12), e0001712. https://doi.org/10.1371/journal.pgph.0001712
Das, S., Grant, L., & Weller, D. (2023b). Mixed-methods study to validate and refine the ‘Strategic Healthcare Implementation Framework for Task Shifting, Sharing and Resource Enhancement’ (SHIFT-SHARE). Protocols.Io. https://doi.org/10.17504/protocols.io.36wgq35zylk5/v1
Feldstein, A. C., & Glasgow, R. E. (2008). A practical, robust implementation and sustainability model (PRISM) for integrating research findings into practice. Joint Commission Journal on Quality and Patient Safety, 34(4). https://doi.org/10.1016/S1553-7250(08)34030-6
Galli, B. J. (2018). Change Management models: A comparative analysis and concerns. IEEE Engineering Management Review, 46(3). https://doi.org/10.1109/EMR.2018.2866860
Glasgow, R. E., Harden, S. M., Gaglio, B., Rabin, B., Smith, M. L., Porter, G. C., Ory, M. G., & Estabrooks, P. A. (2019). RE-AIM planning and evaluation framework: Adapting to new science and practice with a 20-year review. In Frontiers in Public Health (Vol. 7, Issue MAR). https://doi.org/10.3389/fpubh.2019.00064
Harvard Business School Online (2019, September 5). How to do a cost-benefit analysis & why it’s important. Business Insights. https://online.hbs.edu/blog/post/cost-benefit-analysis
Hooper, J., & Longworth, P. (2002). Health needs assessment workbook. http://healthimpactassessment.pbworks.com/f/Health+needs+assessment+workbook+-+HDA+England+-+2002.pdf
Kotter, J. P. (2007). Leading change: Why transformation efforts fail. In Harvard Business Review (Vol. 85, Issue 1). https://doi.org/10.1007/978-1-137-16511-4_7
Kuhlmann, E., Bruns, L., Hoeper, K., Richter, M., Witte, T., Ernst, D., & Jablonka, A. (2021). Work situation of rheumatologists and residents in times of COVID-19: Findings from a survey in Germany. Zeitschrift Fur Rheumatologie, 82(4), 331–341. https://doi.org/10.1007/s00393-021-01081-5
Langley, G., Nolan, K., Nolan, T., Norman, C., & Provost, L. (2009). The Improvement Guide: A practical Approach to Enhancing Organizational performance (2nd ed.). Jossey-Bass.
Limb, M. (2016). World will lack 18 million health workers by 2030 without adequate investment, warns UN. In BMJ. https://doi.org/10.1136/bmj.i5169
Lunsford, S., Broughton, E., & Fatta, K. (2019). Task Shifting/Sharing for HIV Services in 26 PEPFAR-supported Countries: A Qualitative Assessment - Research and Evaluation Report. https://pdf.usaid.gov/pdf_docs/PA00WGCS.pdf
Monden, Y. (1983). Toyota production system: practical approach to production management.
Mundeva, H., Snyder, J., Ngilangwa, D. P., & Kaida, A. (2018). Ethics of task shifting in the health workforce: Exploring the role of community health workers in HIV service delivery in low- and middle-income countries. BMC Medical Ethics, 19(1). https://doi.org/10.1186/s12910-018-0312-3
Nilsen, P. (2015). Making sense of implementation theories, models and frameworks. Implementation Science, 10(1). https://doi.org/10.1186/s13012-015-0242-0
Orkin, A. M., Rao, S., Venugopal, J., Kithulegoda, N., Wegier, P., Ritchie, S. D., VanderBurgh, D., Martiniuk, A., Salamanca-Buentello, F., & Upshur, R. (2021). Conceptual framework for task shifting and task sharing: An international Delphi study. Human Resources for Health, 19(1), 61. https://doi.org/10.1186/s12960-021-00605-z
Rausand, M., & Haugen, S. (2020). Risk assessment: Theory, methods, and applications. In Risk Assessment: Theory, Methods, and Applications. https://doi.org/10.1002/9781119377351
Rogers, E. M., Singhal, A., & Quinlan, M. M. (2019). Diffusion of innovations. In An Integrated Approach to Communication Theory and Research, Third Edition. https://doi.org/10.4324/9780203710753-35
Sarran, P., Clark, D., & Mendonca, K. (2011). Change Management Toolkit: Tips, tools, and techniques for leading a successful change initiative. https://hr.berkeley.edu/sites/default/files/change_management_toolkit.pdf
Shea, C. M., Jacobs, S. R., Esserman, D. A., Bruce, K., & Weiner, B. J. (2014). Organizational readiness for implementing change: A psychometric assessment of a new measure. Implementation Science, 9(1). https://doi.org/10.1186/1748-5908-9-7
Singla, D. R., Meltzer-Brody, S. E., Silver, R. K., Vigod, S. N., Kim, J. J., La Porte, L. M., Ravitz, P., Schiller, C. E., Schoueri-Mychasiw, N., Hollon, S. D., Kiss, A., Clark, D., Dalfen, A. K., Dimidjian, S., Gaynes, B. N., Katz, S. R., Lawson, A., Leszcz, M., Maunder, R. G., & Patel, V. (2021). Scaling up maternal Mental healthcare by increasing access to treatment (SUMMIT) through non-specialist providers and telemedicine: A study protocol for a non-inferiority randomized controlled trial. Trials, 22(1), 186. https://doi.org/10.1186/s13063-021-05075-1
Smith, R., & Duffy, J. (2010). Developing a competent and flexible workforce using the Calderdale Framework. International Journal of Therapy and Rehabilitation (Vol, 17. https://doi.org/10.12968/ijtr.2010.17.5.47844
Tsui, S., Denison, J. A., Kennedy, C. E., Chang, L. W., Koole, O., Torpey, K., Van Praag, E., Farley, J., Ford, N., Stuart, L., & Wabwire-Mangen, F. (2017). Identifying models of HIV care and treatment service delivery in Tanzania, Uganda, and Zambia using cluster analysis and Delphi survey. BMC Health Services Research, 17(1), 811. https://doi.org/10.1186/s12913-017-2772-4
Weiner, B. J. (2009). A theory of organizational readiness for change. Implementation Science, 4(1). https://doi.org/10.1186/1748-5908-4-67
World Health Organization (2020). Quality health services: a planning guide. https://www.who.int/publications/i/item/9789240011632
World Health Organization. (2008). Task Shifting: Global recommendations and guidelines. World Health Organization. https://doi.org/10.1080/17441692.2011.552067
Xu, W., & Zammit, K. (2020). Applying thematic analysis to education: A Hybrid Approach to Interpreting Data in Practitioner Research. International Journal of Qualitative Methods, 19, 1–9. https://doi.org/10.1177/1609406920918810
Author information
Authors and Affiliations
Contributions
All authors finalised the objectives for the framework together. SD performed the literature review, characterised the framework and drafted this manuscript. LG and DW advised on the methodology and reviewed the data analysis, results and this manuscript. This work is part of SD’s ongoing doctoral dissertation at the Usher Institute, University of Edinburgh, United Kingdom.
Corresponding author
Ethics declarations
Ethical Approval
This paper outlines the process being undertaken to conceptualise a new implementation framework. The initial phase of this involved review work, which did not necessitate ethics approval. Subsequent phases, aimed at validating and refining the introduced framework, have received ethics approval from the Edinburgh Medical School Research Ethics Committee at the University of Edinburgh (Reference Number: 2024-EMREC-038).
Competing Interests
The authors received no specific funding for this work. The authors have declared that no competing interests exist.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Das, S., Grant, L. & Weller, D. Conceptualisation of the SHIFT–SHARE: A New Strategic Healthcare Implementation Framework for Task Shifting, Sharing and Resource Enhancement. Glob Implement Res Appl (2024). https://doi.org/10.1007/s43477-024-00132-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s43477-024-00132-8