Abstract
The treatment paradigm in myeloma is constantly changing. Upfront use of monoclonal antibodies like daratumumab along with proteasome inhibitors (PI)s, and immune modulators (IMiD)s have significantly improved survival and outcomes, but also cause unique challenges at the time of relapse. Engaging immune T cells for tumour cell kill with chimeric antigenic T-cell (CAR T-cell) therapy and bispecific antibodies have become important therapeutic options in relapsed multiple myeloma. Bispecific antibodies are dual antigen targeting constructs that engage the T cells to plasma cells through various target antigens like B-cell membrane antigen (BCMA), G-protein-coupled receptor family C group 5 member D (GPRC5D), and Fc receptor-homolog 5 (FcRH5). These agents have proven to induce deep and durable responses in heavily pre-treated myeloma patients with a predictable safety profile and the ease of off-the-shelf availability. Significant research is ongoing to overcome resistance mechanisms like T cell exhaustion, target antigen mutation or loss and high disease burden. Various trials are also studying these agents as first line options in the newly diagnosed setting. These agents play an important role in the relapsed setting, and efforts are underway to optimize their sequencing in the myeloma treatment algorithm.
Similar content being viewed by others
Introduction
The use of proteasome inhibitors (PI)s, immune modulators (IMiD)s and monoclonal antibodies (Mo-Ab) in multiple combinations as upfront therapy combined with an auto-transplant in fit and eligible patients, and as continuous therapy in transplant ineligible patients; or at relapse have substantially increased the longevity and progression free survival (PFS) of multiple myeloma (MM) patients compared to the past [1,2,3]. However, due to the emergence and evolution of treatment resistant clones, myeloma still remains an incurable disease despite these advancements. Diminishing physical performance by accumulated comorbidities, frailty and treatment related toxicities; and the decreased durability of response with successive lines of therapy, make the outcomes dismally poor in patients with multiple relapses. The outcomes are extremely poor in patients who have become refractory to CD38 Mo-Abs especially when penta-refractory, ie refractory to CD38 Mo-Ab, 2 PIs and 2 IMiDs [4]. By engaging immune T cells to lyse MM cells, bi-specific antibodies (BsAbs) are showing encouraging deep and sustained responses in heavily pre-treated patients, refractory to other available lines of therapy. Manageable and predictable side effect profile including infections and low grade cytokine release syndrome (CRS) along with the advantage of “off-the-shelf availability” have made these agents a promising add-on to the existing anti-myeloma armamentarium. Strategies to enhance their efficacy and advancement to earlier lines of the treatment paradigm are exciting avenues to improve outcomes with these agents.
In this review, we highlight the existing updated data on the various BsAbs in use and in development along with their limitations and strategies to mitigate these.
Bispecific antibodies and Bites
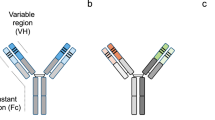
T-cell based immunotherapies have resulted in a paradigm shift in the approach to many malignancies [5,6,7]. Bispecific antibodies (BsAbs) are antibody constructs with 2 binding sites that either bind two different antigens or 2 epitopes of the same antigen. They can simultaneously bind a tumour cell (binds to the tumour specific antigen on the targeted cancer cell) and an immune effector cell (attaches to the T- cell CD3 co-receptor) [8]. BiTEs (Bispecific T cell engagers) on the other hand are engineered constructs of two single chain variable fragments (ScFv) that acts as a dual-targeting molecule [9]. This immunological synapse causes T-cell activation and degranulation, which causes MM cell wall perforation, leading to apoptosis through perforin and granzyme B [10, 11]. Furthermore, these agents also modulate T cell function by causing T cell activation, proliferation and differentiation of naïve T cells to T cells with memory phenotypes (central memory and effector memory T cells).
Tri-specific antibodies (TsAbs) go one step further and add either a co-stimulatory protein to decrease T cell anergy [12, 13] or can target an additional target antigen [14].
Viable therapeutic targets on plasma cells
To maximize efficacy and minimize toxicity, bispecific antibodies should target an antigen that is unique and specific to multiple myeloma cells, with minimal expression in other healthy tissues. Currently approved and in- trial BsAbs for MM are directed against B-cell membrane antigen (BCMA), G-protein-coupled receptor family C group 5 member D (GPRC5D), Fc receptor-homolog 5 (FcRH5), and CD38 on the plasma cells. Further tumour specific antigens like SLAMF7 and CD138 on plasma cells, as well as additional effector cell targets like CD16a, NKp30, or NKG2D are also in the therapeutic exploration phase [13, 15,16,17,18,19,20,21,22,23,24,25].
B cell maturation antigen (BCMA)
B-cell maturation antigen (BCMA) or CD269 is a type 3 transmembrane domain protein of the tumour necrosis factor receptor (TNFRSF17) superfamily that is encoded on chromosome 16p and is expressed on both normal and malignant plasma cells at high levels that makes it an ideal target antigen for myeloma therapy [26,27,28]. Along with its ligands B cell activator of the TNF family (BAFF) and a proliferation inducing ligand (APRIL), it delivers pro-survival cell signals that regulates B cell proliferation, maturation, survival as well as differentiation into plasma cells [29]. Its expression is upregulated during MM pathogenesis and evolution, from normal to MGUS to SMM to active MM [30]. Higher levels of BCMA are associated with poorer outcomes [26], indicating that BCMA is a useful biomarker of disease activity and prognosis for MM. A ubiquitous intramembranous protease called gamma secretase cleaves the membrane bound BCMA and sheds it as soluble BCMA (sBCMA) into circulation [31]. This decreases ligand density on the plasma cells and can potentially act as a “sink” with therapeutic antibodies binding to sBCMA [32]. As BCMA is expressed also on mature B and plasma cells, its function is highly integral to humoral immune responses. To date, two anti-BCMA BsAbs – teclistamab and elranatamab, have been approved by Food and Drug Administration (FDA).
G protein coupled receptor family C group 5 member D (GPRC5D)
GPRC5D is a novel target for myeloma immunotherapy identified relatively recently [33,34,35]. This orphan G protein coupled receptor is a transmembrane receptor protein, encoded by the GPRC5D gene on chromosome 12p and is highly expressed on surface of malignant plasma cells, however its functions remains unknown [36, 37]. GPRC5D expression is absent from nearly all healthy tissue with the exception of hard keratinized structures that include the hair shaft, epithelial cells of the eccrine sweat glands, nail, and filiform papillae of the tongue [38, 39]. Additionally, its expression is also high in MM cells compared to other haematological malignancies. Similar to BCMA, the high expression of GPRC5D on myeloma cells has been associated with poor prognosis [40]. Even though GPRC5D and BCMA have a similar expression on CD138+ malignant plasma cells, their expression patterns are independent of each other, thereby offering distinct clinical targets [33]. The expression of GPRC5D is also unaffected by BCMA loss, which can be seen in relapse following BCMA directed therapies. This unique advantage will not only allow the use of a GPRC5D targeting agent following failure to BCMA therapy, but will also support the strategy of combining BCMA and GPRC5D targeting agents in myeloma [34, 41]. Additionally, due to its short extracellular N-terminal domain, GPRC5D is also unlikely to be shed from target cells to serum which may reduce the risk of reduced efficacy related to target antigen shedding. There were 2 GPRC5D × CD3 BsAbs (talquetamab, forimtamig) under investigation in clinical trials. FDA granted accelerated approval to talquetamab in August 2023 following the MonumenTAL-1 study results [42], while forimtamig has been discontinued from clinical development.
Fc receptor-homolog 5 (FcRH5)
The Fc receptor-homolog 5 (FcRH5) is a surface membrane protein in the immunoglobulin superfamily that has been implicated in proliferation and isotype expression in the development of antigen-primed B cells [43,44,45]. Its expression is limited only to the B-cell lineage with expression starting in pre–B cells and increasing through its maturation to mature B cells and plasma cells [46]. FcRH5 has also been shown to be more highly expressed in malignant plasma cells than normal plasma cells [43, 46, 47]. Also known as FcRL5, its gene is expressed in the chromosomal break point in 1q21, and myeloma associated with gain of 1q21 can lead to overexpression of FcRL5 [47]. Flow cytometric analysis have shown that FcRH5 expression was more prevalent compared to GPRC5D and BCMA in bone marrow plasma cell samples from patients with multiple myeloma. However the expression was more intense and homogenous for GPRC5D than FcRH5 and the least was seen with BCMA [48]. Even though the phase1 clinical trial of a FcRH5 antibody drug conjugate was unsuccessful [49], enhanced and durable efficacy is seen in patients treated with cevostamab, a BsAb targeting FcRH5 [50].
CD38
CD38 is a type II transmembrane glycoprotein on the MM cell which was first identified as a marker of cell activation and proliferation many years ago. High expression of CD38 on the MM cell surface is closely associated with the immunocompromised tumour microenvironment (TME) [51, 52]. The acidic bone marrow microenvironment provided by the aerobic glycolysis along with the CD38 glycoprotein, promotes the generation of AMP and adenosine, which has potent immunosuppressive activity. Based on the success of daratumumab and isatuximab, studies exploring development of BsAb targeting CD38 were developed. ISB 1342 (GBR 1342) was the first CD38 × CD 3 BsAb developed to direct T cells to CD38 expressing myeloma cells on a different epitope than daratumumab [53, 54]. Preclinical studies have shown that ISB 1342 does not compete with daratumumab, induces robust MM cell lysis and overcomes resistance to anti-CD38 Mo-Abs. A phase 1 trial of ISB 1342 in RRMM patients is ongoing (NCT03309111).
Figure 1 summarizes the various tumour specific antigens on the myeloma cell and the various T cell and NK cell receptors that are engaged together by BsAbs.
Efficacy in relapsed and refractory disease as monotherapy
Efficacy data from major clinical trials using BsAbs as single agent in RRMM have been summarized in Table 1.
Teclistamab (Tecvayli- Janssen Biotech Inc), a humanized IgG Fc-anti-BCMA BsAb, was the first BsAb that was approved (EMA, Aug 2022 and US FDA, Oct 2022) for the treatment of patients with RRMM who have received at least three and four prior lines of therapy respectively, including a proteasome inhibitor, an immunomodulatory agent and an anti-CD38 monoclonal antibody. These approvals were based on the seminal MajesTEC-1 trial [55]. Following two step up doses, patients received teclistamab 1500 mcg/kg SC weekly, with the option to switch to every 2 weeks if they achieved ≥partial response after ≥4 cycles of therapy in phase 1 or ≥CR for ≥6 months in phase 2. In the long term follow up of the MajesTEC-1 trial, after a median follow up of 22 months, 43% of patients achieved a complete response (CR) or stringent CR with teclistamab monotherapy [56]. The median progression free survival (mPFS) and median overall survival (mOS) were 12.5 months and 21.9 months respectively in this heavily pre-treated cohort of 165 patients with median 5 [2,3,4,5,6,7,8,9,10,11,12,13,14] prior lines of therapy, and 77.6% being triple refractory. MRD negativity at any point was seen in 85.7% of evaluable patients. Persistent MRD negativity was seen in 56.1% for >6 months and 38.9% patients for >12 months [57]. When compared to patients who received more than 3 LOT, patients who were treated earlier had a significantly improved PFS (21.7 months, 95% CI 13.8-NR vs 9.7 months, 95% CI 6.4–13.1 months). 90% of the 49 patients who remain on the study are receiving a Q2W dose.
Data from the Asian cohort of the MajesTEC-1 study from China, among 26 patients with median 5 prior LOT and 57.7% having high risk cytogenetics and 34.6% with extramedullary disease, ORR was 76.9% with ≥VGPR in 76.9% and ≥CR in 57.7%. The median PFS and OS at 12 months were 68.0% and 83.5% [58]. Similar efficacy data was also shown in the Phase 1/ 2 Japanese MMY1002 trial (n = 26, 19.2 high risk, median 4.5 prior LOT), with ORR of 76.9%, and ≥CR in 46.1% patients [59].
Real world retrospective data from US, following the approval, on 24 patients have also shown favorable outcomes [60]. All 24 patients were triple refractory and 10 patients were exposed to BCMA directed therapy (BsAb, BCMA ADC and BCMA -CAR T) including 5 patients who had ≥2 anti-BCMA therapy. Responses were seen as early as 16 days. The ORR was 60% (9/15 evaluable patients), with ORR of 50% (5/10) in patients with prior BCMA-targeted therapy. At a short median follow up (1.3 months), this study shows that despite diminished efficacy with prior BCMA therapies, teclistamab is still effective in these heavily pre-treated patient population.
A phase 3 trial (MajesTEC-9, NCT05572515) is currently recruiting RRMM patients to compare the efficacy of single agent teclistamab to other standard of care options (pomalidomide-bortezomib-dexamethasone or carfilzomib-dexamethasone).
Elranatamab (Elrexfio, Pfizer, Inc) is a humanized anti-BCMA /CD3 bispecific IgG2 antibody [61] that was approved by FDA in August 2023 for the treatment of patients with RRMM who have received at least four prior lines of therapy, including a proteasome inhibitor, an immunomodulatory agent and an anti-CD38 monoclonal antibody. The approval was based on the efficacy demonstrated in the phase 2 MagnetisMM-3 trial [62]. Elranatamab was administered in step up doses, with a target dose of 76 mg. Patients who received QW dosing for at least six cycles and achieved a PR or better (≥PR) persisting for at least 2 months had their dosing interval changed to Q2W. Among the 123 patients enrolled in this trial, 96.7% and 42.3% of patients were triple and penta-refractory respectively with median 5 (2-22) prior lines of therapy. On long term follow up, 61% patients had overall response, with CR and above documented in 39%. MRD negativity (at threshold 10−5) was obtained in 92% (23/25) evaluable patients. Median PFS was 17.2 months and median OS was 24.6 months at 17.6 months follow up, and the respective rates at 12 months were 57.1% (95% CI, 47.2–65.9) and 62% (95% CI, 52.8–70.0) [63, 64].
Linvoseltamab, another fully humanized anti-BCMA × CD3 BsAb was studied as monotherapy in 2 doses (50 mg and 200 mg) in the Phase 2 LINKER-MM1 (REGN5458) trial that included patients who progressed on/ after ≥3 lines of therapy, including a PI, IMiD and an anti-CD38 Mo-Ab [65]. Treatment was once a week for the first 14 weeks and thereafter once every 2 weeks. The median lines of prior therapy was 5 (2-16) and 81% being triple refractory. The protocol allowed a dose escalation from 50 mg to 200 mg in patients who progressed during 4–12 weeks. This study showed better efficacy with the 200 mg, and this was seen even after progression on the 50 mg dosing. Among the 117 patients treated with the 200 mg, 39% had high risk cytogenetics and 28% were penta-refractory. At a median follow up of 14.3 months, ORR was 71% with 50% achieving ≥CR. In the 107 patients treated with the 50 mg dose, the ORR was 48%, with 21% achieving ≥CR at a median follow up of 7.4 months [66]. Based on this early promising data from the LINKER-MM1 trial, Linvoseltamab has recently received priority review by the FDA for patients who have progressed after 3 or more prior lines of therapy [67].
ABBV-383 (TNB-383B) is a next generation fully human BsAb targeting BCMA with low affinity binding to CD3 which at this time does not require step up dosing. In a phase 1 trial, with this agent, durable response were shown with manageable toxicity in patients RRMM (≥3 prior lines). The overall response rate was 68% with VGPR or better in 54% patients, and CR of 36% at doses of ≥40 mg Q3W in the dose expansion cohort [68]. Median DOR and PFS were not reached in both cohorts. The high affinity BCMA binding coupled with the low affinity to CD3 could reduce T cell activation and exhaustion with decreased inflammatory cytokine production while maintain maximal efficacy [69].
Alnuctamab (CC 93269) is a BsAb with 2 asymmetric arms carrying humanized IgG1 T-cell engagers that bind bivalently to BCMA and noncovalently to CD3 [18]. Despite a good ORR of 83.3% in the ≥6 mg cohort, in a first-in-human Phase 1 trial [70], this agent has been withdrawn from clinical development.
F182112, another anti BCMA × CD3 BsAb showed ORR of 43.8% at a median follow up of 3.1 months in a phase 1 study [71].
Pacanalotamab (AMG420) and pavurutamab (AMG701) are BCMA × CD3 BiTEs. Despite exciting early phase 1 results [72, 73], both these agents were subsequently withdrawn from further clinical development.
Talquetamab is the first in class IgG4 BsAb targeting GPCR5D on myeloma cells and CD3 on T cells [34, 36]. In the phase 2 MonumenTAL-1 trial (n = 375), talquetamab as single agent was tested as 2 doses – 0.4 mg/kg QW (n = 143, median FU – 29.8 months) and 0.8 mg/kg Q2W (n = 154, median FU = 23.4 months). Patients who had achieved at least 4 lines of prior therapy were included. At the bi-weekly dose, 73.6% (95% CI, 63.0–82.4) achieved an ORR. With a median follow up of 8.6 (0–9.5) months, 58% of patients achieved a VGPR or better, including 33% in CR or better. At the 0.4 mg QW dose, 73% (95% CI, 63.2–81.4) achieved an ORR. Fifty seven percent patients achieved a VGPR or better (including 35% CR and above at a median follow up of 14.9 (0.8–15.4) months. Responses were durable with a median duration of response not reached in the 0.8 mg/kg Q2W cohort and 9.5 months in the 0.4 mg/kg QW cohort [74, 75].
The MonumenTAL-1 trial also included 78 patients who were exposed to prior BsAb or CAR T cell therapy (94% to anti-BCMA therapy). These patients received talquetamab at 0.4 mg/kg QW. At a median follow up of 20.5 months, 67% (95% CI, 53–86) achieved an ORR, with ≥CR in 42.4%, and median duration of response among patients who achieved ≥CR was 24.2 months [75]. Following the MonumenTAL-1 data, US FDA granted accelerated approval of talquetamab in August 2023 for treatment of adult patients with RRMM who have received at least 4 prior lines, including a PI, IMiDs and an antiCD38 Mo-Ab.
Forimtamig is another GPRC5D × CD3 BsAb with 2 binding domains for GPRc5D that confers high affinity to the malignant plasma cell. Forimtamig was evaluated in a dose escalation Phase 1 study with both intravenous (IV) and subcutaneous (SC) administration in heavily pre-treated MM patients [76]. All patients were administered prophylactic steroids to mitigate CRS. Potent anti-MM effects were seen in both dose cohorts (ORR – 71.4%, ≥VGPR: 59.2% in the IV arm and 63.6% ≥VGPR: 52.8%) in the SC arm). Median duration of response was 10.8–12.5 months. In patients who were exposed to prior BCMA-directed therapy (CAR T-cell therapy, BsAb, or ADC), the ORR was 52.4%. This agent has been discontinued from clinical development.
Cevostamab is a FCRH5 × CD 3 BsAb that showed promising anti-MM activity in a phase 1 dose-finding trial that enrolled heavily pre-treated patients (n = 161, median of 6 prior lines; triple-class refractory: 84.5%) [77]. Cevostamab was administered IV every 3 weeks for a maximum of 17 cycles (approximately 1 year) with premedication to mitigate CRS (acetaminophen, antihistamine, and corticosteroid). At the higher dose levels, the overall response rate was 56.7% ( ≥ VGPR: 33.3%). Median response duration was 11.5 months in the single step-up cohorts. A subgroup analysis of 16 patients who stopped treatment after 17 cycles while in remission, showed that most responders (78%) remained in response (median follow-up 9.6 months) [78]. Also, patients who discontinued cevostamab treatment because of adverse events after a median of time on treatment of 6 months, were able to maintain their response (median duration of response after treatment discontinuation: 9.2 months). These data indicate that fixed-duration treatment may be effective in those who remain in remission at 1 year highlighting the potential for an extended treatment-free period which could soon be an emerging trend in myeloma. While it seems to be an attractive option, these data need to be validated in a larger patient cohort with longer follow-up.
Efficacy in combinations
Encouraged by the efficacy of these agents as monotherapy in RRMM, several trials have also tested these agents in combinations with other BsAb or other anti-myeloma agents. Major trials are summarized below and in Table 2.
The Phase 1b MajesTEC -2 trial tested teclistamab in various combinations in the relapsed refractory setting. In one cohort, teclistamab was tried with a combination of daratumumab and lenalidomide. Daratumumab has been shown to deplete CD38+ Tregs and promote activation and clonal expansion of cytotoxic T-cells [79]. IMiDs, including lenalidomide and pomalidomide, have been shown to potentiate T-cell responses and improved the cell killing of BsAbs in vitro [80,81,82]. Thirty two patients with median 2 (1-3) prior lines of therapy received weekly doses of Teclistamab (0.72 or 1.5 mg/kg with step up dosing) along with Daratumumab 1800 mg and Lenalidomide 25 mg at the standard dose and schedule [83]. Median time to first response was 1 (0.7–2.0) months. In the 0.72 mg/kg cohort, ORR was seen in 13/13 evaluable pts while VGPR and above was achieved in 12/13 patients at a median follow up of 8.6 months. In the 1.5 mg/kg cohort, ORR was seen in 13/16 evaluable patients at a median follow up of 4.17 months. These exciting early results will be tested in the phase 3 MajesTEC −7 study (NCT05552222) which will compare a combination of teclistamab-daratumumab- lenalidomide vs the combination of daratumumab-lenalidomide-dexamethasone in pts with NDMM ineligible or not intended for autologous stem cell transplant as initial treatment.
The TRIMM-2 trial studied the combination of SC talquetamab with daratumumab in RRMM and has shown encouraging results [84]. The median prior lines of therapy were 5 (2-16) which included 63% penta-refractory, 58% triple class refractory, including 18% with high risk cytogenetics and 25% with extramedullary disease (EMD). ORR was 75% (66% ≥VGPR, 45% ≥CR)and responses deepened over time. In patients exposed/ refractory to prior therapy, ORR was 75%/76% for anti-CD38, 74%/64% for anti BCMA, and 75%/75% for BsAb. Median time to first response was 1 (0.9–8.3) month. At 12 months, 86% of responders still maintained responses.
The Phase 1b MonumenTAL -2 trial tested the addition of pomalidomide to talquetamab. In this study, pomalidomide was added from cycle 2, after step up of talquetamab at 2 different dose levels. ORR was >80% across both dose levels of talquetamab, and response was seen as early as 1 (0.9–2.1) month showing promising efficacy of this combination [85].
The Phase 1b RedirecTT-1 trial tested a combination of teclistamab and talquetamab simultaneously targeting two MM target antigens to overcome resistance mechanisms [41]. A high 92% ORR was observed in patients with advanced RRMM with median 5 (1-11) lines of prior therapy (78% triple class refractory, 63% penta- drug exposed, 33% high risk cytogenetics, 43% extramedullary disease). At a median duration of 14.4 (0.5–21.9) months, the ORR was 84%, and CR or better was seen in 34%. At the recommended phase 2 dose (RP2D), the ORR was 92% among all evaluable patients, including 83% in patients with extramedullary disease (EMD). Despite a high ORR, the median PFS for EMD turned out to be 6.1 months (95%CI, 2.5–9.9) across all doses and 9.9 months in the RP2D arm (95% CI, 2.4-NE). This shows that dual targeting with BsAbs has still not overcome the high risk due to EMD. Part 3 of RedirecTT-1 is exclusively testing this combination in patients with RRMM and EMD (NCT04586426).
There are many ongoing and upcoming trials that are testing combinations of BsAbs alone or in combination with other agents. Some of those are listed in Table 3.
Safety profile and side effects
Despite deep and durable responses, the use of BsAb in RRMM also offers unique challenges. Common adverse events include infections, cytopenias, CRS and neurological toxicities. The various haematological and major non haematological adverse events with BsAb have been summarized in Table 4.
Deaths not due to myeloma
To date, only data from phase 1/2 trials have been presented for BsAbs, making OS difficult to interpret. Given the history of myeloma treatments like venetoclax [86], melflufen [87], and pembrolizumab [88, 89], which showed promising efficacy in early phase trials but were hampered by decreased OS in randomized trials, it is important to evaluate non-myeloma deaths in these early phase BsAb trials. Teclistamab (27/165, 16%) and Elranatamab (18/123, 15%) both demonstrated a significant number of non-myeloma deaths, primarily due to infection, and COVID-19 in particular, which will be watched closely in the larger phase 3 randomized trials. This signal was not seen with Talquetamab, while more follow-up data is needed for Cevostamab.
Infections
Infections were the most common treatment related adverse event seen with these agents, the greatest risk being in anti BCMA BsAbs due to expression of BCMA on mature B-cells and normal plasma cells and its role in generating humoral immunity. T cell exhaustion by constant stimulation of T cells by these agents also can reduce the ability of T cell mediated immune responses. Pre-clinical studies have shown that inhibition of BCMA in mouse models precludes antibody responses to a highly antigenic protein and to a pneumovax vaccine [90]. It was also reported by multiple study groups that response to COVID vaccine was blunted in RRMM patients receiving T cell directed anti-BCMA therapies including BsAbs [91,92,93,94,95]. With the longest follow up among BsAbs, the incidence of grade 3–4 infections was 55.2% in patients who received teclistamab in the MajesTEC-1 trial [57].
In a subset analysis of the MajeTEC-1 trial, teclistamab was shown to profoundly and durably suppress polyclonal immunoglobulins and B cell counts. Furthermore, response to vaccines against Streptococcus pneumoniae, Haemophilus influenzae type B, and severe acute respiratory syndrome coronavirus 2 was severely impaired in patients treated with teclistamab compared with vaccination responses observed in patients with newly diagnosed MM or relapsed/refractory MM [96]. Similarly, with the other BCMA directed BsAb also infections were seen in as high as 70% (40% grade 3 and 4) as reported with elranatamab [74] and linvoseltamab [65].
However, with GPRC5d targeting BsAbs, the incidence of infections was lower as they induce much lower B cell depletion and hence lower grades of hypogammaglobulinemia. The incidence of grade 3 and above infections was approximately 20% with talquetamab [75]. More long-term follow-up data are needed to better understand the infection profile of FcRH5-targeting cevostamab.
Primary universal prophylaxis against Herpes, Varicella and Pneumocystis is standard. The role of routine antibacterial or anti-fungal prophylaxis is not yet known and is not routinely recommended [97]. Intravenous or subcutaneous immunoglobulin prophylaxis can mitigate the defect in humoral immunity and is associated with significantly reduced rates of severe infections with anti-BCMA therapy [96, 98,99,100]. The current recommendation is to institute immunoglobulin replacement monthly if IgG is <400 mg/dL and to continue it for the total duration of immunoparesis even in the absence of infections while on BCMA BsAb [97]. Routine vaccinations against COVID-19, yearly influenza vaccination, pneumococcal vaccinations and herpes vaccinations are also strongly recommended. Rapid identification and treatment of COVID-19 is essential for patients on BCMA BsAbs given the high rate of COVID-19 deaths seen in trials to date.
Cytopenias
Cytopenias are another common adverse event seen with BsAb therapy, mostly during cycle 1 when the disease is active. Based on a pooled analysis done recently there were no significant difference between non BCMA -targeting BsAb compared to BCMA targeting BsAbs, in terms of all grade and type hematologic toxicities (combined neutropenia, anemia, lymphopenia, leukopenia and thrombocytopenia). However, combined grade 3-4 hematological toxicity was higher in anti-BCMA BsAb than others [101]. The incidence of grade 3 and above neutropenia was 65% with teclistamab [55], 48% with elranatamab [74] and 26% with ABBV-383 [68]. The rate of grade 3/4 neutropenia is very high with lenalidomide/ BCMA combinations [83]. The burden of grade 3–4 neutropenia also adds up to the increased risk of serious infections. Neutropenia related infections can be potentially life threatening, can result in treatment delays and dose reductions which in turn can affect treatment efficacy. Use of granulocyte colony stimulating factors (G-CSF) is recommended for grade 3–4 neutropenia. G-CSF should not be used during periods of active CRS as it can lead to cytokine release leading to potential worsening of CRS. Moreover, antibacterial and antifungal prophylaxis can be considered for prolonged neutropenia that fails to improve despite the use of G-CSF [97].
Cytokine release syndrome
Cytokine release syndrome (CRS) occurs as a consequence of robust cytotoxic T-cell activation and the subsequent release of inflammatory cytokines. All grade CRS has been reported in most patients (range 46.3–82.4%) across all the BsAb trials, with a very low incidence of ≥grade 3 CRS (range 0–3%) [41, 55, 62, 66, 75,76,77]. Most CRS events happened during the step up dosing or following the first full dose. Careful monitoring for CRS, step-up dosing with premedication and judicious use of tocilizumab and other supportive care can successfully mitigate this risk. In a sub cohort of the MajesTEC-1 study, prophylactic use of single dose of tocilizumab with the first dose has significantly reduced the incidence of CRS compared to the entire cohort without any additional safety signals and without any impact on treatment efficacy [102]. Another phase 1 clinical study with cevostamab, an anti FcRH5 × CD3 BsAb has shown the clinical utility of prophylactic use of tocilizumab in significantly reducing the risk of CRS without any negative effect on efficacy [103]. This strategy is an area of clinical interest and has the potential to reduce CRS risk in patients with disease profiles suitable for outpatient dosing, reducing the burden of hospitalization during step-up dosing. CRS rates may also vary by country, which may be the result of patient or treatment factors, with for example significantly higher CRS rates and severity in Japanese patients [104]. Higher CRS rates, albeit lower grades were also seen in the Chinese cohort of the MajesTEC-1 trial [58].
ICANS/neurological toxicity
Immune effector cell associated neurotoxicity syndrome (ICANS), though less common than following CAR T - cell therapy, is another well described side effect seen with BsAb. In general ICANS typically occurs relatively early in the treatment, with the step up doses and the initial full dose with a median time to onset of 2 (range 1–3) days from the most recent dose. Across all BsAbs, neurological toxicity were mostly grade 1–2 ICANS (range 1–14%), while incidence of ≥ grade 3 was low (range 0–11%) [41, 55, 62, 66, 75,76,77]. The most common manifestations were confusion and dysgraphia. Steroids are the mainstay of treatment, with tocilizumab in addition if patients also develops concurrent CRS. Most patients recover well with treatment. Another notable neurological side effect seen with elranatamab was peripheral neuropathy (17.1% with motor dysfunction and 13.8% sensory neuropathy) in the MagnetisMM-3 trial. These were mostly mild, with only 1 patient having grade 3 motor dysfunction. No patients had grade 3 sensory neuropathy, or any grade 4 or 5 events [62].
Skin, nail, and oral adverse events
Toxic side effects affecting the skin, nails and oral mucosa were common with GPRC5D targeting BsAbs due to the co-expression of these receptors in hard keratinized structures that include the hair shaft, epithelial cells of the eccrine sweat glands, nail, and filiform papillae of the tongue [38, 39]. In the phase 1 MoumenTAL -1 study, nail-related adverse events occurred in 57% of the patients who had received talquetamab at the 405-μg dose level and in 27% of those who had received it at the 800-μg dose level. Skin-related adverse events occurred in 67% of the patients at the 405-μg dose level and in 70% at the 800-μg dose level; the most common skin-related adverse events were exfoliation, pruritus, and dry skin. Grade 3 rash-related adverse events were not reported in patients who received the 405-μg dose level, but they occurred in 16% of the patients who had received it at the 800-μg dose level.
Severe grade 3 rash was sensitive to oral and topical glucocorticoid treatment and treatment was resumed in all but one patient after resolution of the rash. Oral-related adverse events were frequent, but were all of grade 1 or 2 severity, and included dysgeusia, dry mouth, and dysphagia. In an updated analysis, strategies like reducing doses or increasing the duration between doses has been shown to mitigate these side effects without compromising on clinical efficacy [105]. Skin related side effects were seen with Forimtamig, (≥ grade 3 in 11.8 and 14.8% in IV and SC arm) while no patients reported severe oral or hair and nail related adverse events [76].
Resistance mechanisms and strategies to enhance efficacy
Despite encouraging early data, loss of response to BsAb therapy has been reported. Response largely depends on the T cell immune milieu and the ability to induce durable anti-tumour responses. The key resistance mechanisms to BsAbs include high tumor burden, T-cell fitness and repertoire, and mutations and loss of target on MM cells [106]. High tumor burden, as measured by bone marrow plasma cells >60%, ISS stage 3, and extramedullary disease, has been shown to adversely impact the clinical efficacy of BsAbs in MM [55, 62, 107, 108]. Preclinical data demonstrate that a low effector : tumor ratio and high frequency of Tregs predict poor response to BsAbs in MM [109]. In vivo correlative studies of teclistamab have shown that increased Tregs and exhausted T cell phenotype at baseline predict non-response [110]. Acquired resistance mechanisms include T-cell exhaustion, antigen escape, and loss of MHC class I. In particular, there is a high rate of BCMA mutation or deletion likely due to selective pressure of continuous administration of BsAbs [111]. Novel approaches are needed to overcome these mechanisms in order to increase the proportion of patients responding to BsAbs and to create a favorable long-term immune profile. The effector T cell function is particularly compromised with multiple treatment lines and relapses compared to a newly diagnosed MM or to a precursor state [112, 113]. Many trials are currently underway looking at moving BsAbs to early phase of treatment—in the newly diagnosed setting, as post ASCT consolidation and in early relapses and these have been discussed elsewhere in this review.
Mutation or loss of BCMA expression can lead to resistance. Membrane bound BCMA is a substrate for the enzyme gamma secretase which directly sheds the BCMA from the plasma cells leading to increased levels of circulating soluble BCMA (sBCMA). This leads to decrease in the binding of APRIL and BAFF to BCMA [31] and decreased target availability for BsAbs. Levels of sBCMA increase with disease progression and correlate with adverse outcomes [114, 115]. Even though baseline sBCMA levels were highly variable and did not correlate with response in the MajesTEC trial, increased levels of sBCMA were associated with poor outcomes [116]. The addition of a gamma secretase inhibitor has been shown to in-vitro enhance BCMA BsAb induced MM cell killing with rapid clearance of sBCMA by improving antigen availability leading to enhanced tumor control and improved survival in a preclinical studies [32, 117]. This has been demonstrated by early results from one arm of the multicohort, open-label, phase 1b, MajesTEC-2 trial, which investigated the combination of teclistamab with nirogacestat across multiple dose levels and showed ORR between 57–92% [118]. However there have been safety concerns raised with this combination due to the treatment related adverse effects noted which included dose limiting grade 3 gastrointestinal bleeding, grade 3 ICANS, and death due to septic shock and cardiac arrest [118, 119].
Target antigen loss can happen due to rare events of biallelic deletions or mutations affecting the BCMA gene. This has been reported rarely in the context of BCMA CAR T-cell therapy [120, 121] and more commonly in the context of BCMA-BsAbs [122]. Biallelic deletions or single copy number variations leading to loss of GPRC5D has also been reported as important tumour intrinsic driver of relapse after anti-GPRC5D T cell directed therapy [111]. Combining agents with different targets or multiple epitopes or combining more than one BsAb simultaneously may circumvent these obstacles.
The bone marrow TME in myeloma is characterised by a complex interplay between MM cells, immune cells and the BM stromal cells (BMSCs) that impair normal immune function and facilitates proliferation and survival of MM cells leading to treatment failure and disease progression. Immunosuppressive regulatory T cells (T-regs) are increased and their effect is enhanced by MM. Myeloma cells can also directly generate functional T-regs in a contact independent manner, mediated by ICOS/ICOS-L [123]. An analysis of the MajesTEC -1 study showed that patients who had failed to respond to teclistamab had had low peripheral CD8 + T cell levels, increased T-regs and enhanced expression of markers associated with T cell exhaustion. This also correlated with poor survival in this study [116]. Combining BsAbs with therapeutic agents that augment T cell function are options to enhance efficacy. The alkylator cyclophosphamide is known to improve effector T-cell responses by depleting T-regs and promoting cytotoxic T-cell activity [124]. It also enhances expansion of memory cytotoxic T cells, required for BsAb activity by skewing T helper cells from a Th2 profile to a Th1 profile [125]. Addition of cyclophosphamide to BCMA-BsAb was found to be effective in a murine model [82] and this offers an exciting promising add-on approach to improve efficacy. Daratumumab, a highly efficient anti CD38 Mo-Ab can also reduce immunosuppressive T and B regulatory cells, and myeloid derived suppressor cells (MDSCs) and lead to clonal T cell expansion [79] especially in heavily pre-treated patients and this rationale is being tested in various combinations in the relapsed and upfront clinical settings.
T-cell exhaustion and dysfunction induced by continuous and persistent antigenic stimulation by BsAbs and other T cell directed therapies is another concern for failure of BsAb therapy [36, 110, 116, 126]. Immunomodulators (IMiDs) and Cereblon E3 ligase modulators (CELMoDs) can potentiate T cell responses. Many pre-clinical studies have shown this synergistic action. Pre-treatment of immune effector cells with lenalidomide or pomalidomide has been shown to enhance BCMA BsAb mediated MM cell kill [73]. Combining either pomalidomide, iberdomide or mezigdomide to a BCMA × CD3 BsAb Alnuctamab has shown that this combination can effectively enhance T cell activation and tumor clearance in murine models [127]. These drugs could be effective partners to BsAbs and could effectively target both T cell exhaustion and BM-driven immunosuppression, and restore T cell immunity against MM leading to better outcomes. Many clinical trials testing this combination are underway (Table 3).
Another potential option that could be explored which would allow for reversal of T cell exhaustion is fixed duration treatment with drug holidays as seen with cevostamab [78].
Check point signaling is an important immunosuppressive component of the myeloma microenvironment [128]. Induction of check point expression on B cells due to the effective T cell activation conferred by BsAb is a well-studied phenomenon [129, 130]. Due to the release of the pro-inflammatory cytokines, the expression of check point ligands and receptors like the programmed death ligand (PD-L1), and co-inhibitory receptors like T cell immunoglobulin and mucin-domain-containing-3 (TIM-3), lymphocyte activation gene -3 (LAG-3), killer cell lectin like receptor G1 (KLRG1) and T cell immunoreceptor with immunoglobulin and ITIM domain (TIGIT) are upregulated in myeloma cells [131, 132]. This in turn binds on the programmed death receptor (PD-1) on the T cells leading to T-cell anergy, T cell exhaustion, impaired cytokine production and reduced target cell kill. PD-L1 expression is also increased on MM cells compared with MGUS and healthy donor plasma cells. Preclinical studies have shown that anti-myeloma activity of FcRH5 × CD3 BsAb was limited by PD-1/PD-L1 signaling, and effective PD-L1 blockade significantly enhances myeloma cell elimination [47]. One study of interest that will throw more light on these hypotheses will be the Phase Ib study of combining cetrelimab, a PD-1 antibody to teclistamab and talquetamab (NCT05338775). The various resistance mechanisms and potential interventions to mitigate these are summarized in Fig. 2.
Moving to front line therapy
Encouraged with the promising results seen in RRMM, BsAbs are also being moved into earlier lines of therapy where T cell fitness is better compared with heavily pre-treated and relapsed-refractory disease [113, 133]. As immune dysfunction is progressive and impacted by disease features and treatment, this shift to front line therapy could potentially lead to better and sustained outcomes. Comparison of T cell repertoire in post induction leukapheresis samples and samples at relapse/progression has shown higher early memory T cells, higher CD4/CD8 T cells and a better T cell expansion in the former compared to the latter, especially if patients had received <2 lines of therapy. This suggests better T cell fitness and could predict for better outcomes when immune directed therapies are used up front in the course of the disease rather than in the relapsed setting. For example, patients in MajesTEC-1 with <3 prior lines of therapy had higher response rates than those with 3+ prior lines [55]. At the same time, it is also worth noting that moving anti-BCMA CAR-T cell therapy to earlier lines of therapy in KarMMA-3 and CARTITUDE-4 still did not produce a plateau in the PFS curves [134, 135].
There are many ongoing and upcoming clinical trials testing the combination of various BsAbs (alone or in combination) with other agents in the newly diagnosed setting as listed in Table 5. In addition to utilizing the better T cell milieu in the upfront setting, these combinations will also test the synergistic role of other agents like IMiDs, anti CD38 Mo-Ab and gamma secretase inhibitor (Nirogacestat) in mitigating various resistance mechanisms discussed earlier.
The suppression of Tregs and recovery of CD8 + T-cells leading to a low Treg/effector cell ratio following an autologous stem cell transplant (ASCT) may make the immune milieu more supportive for the action of BsAb [136]. Two phase 3 clinical trials, MajesTEC -4 (NCT05243797) and MagnetisMM -7 (NCT05317416) are recruiting patients and will respectively compare the efficacy of teclistamab with lenalidomide and elranatamab alone with standard of care lenalidomide as post ASCT consolidation/maintenance.
Additional attempts to utilize better T cell function at the precursor stages of the disease are also underway. The randomized phase 2 Immuno-PRISM study has shown significant superiority of teclistamab when compared with lenalidomide and dexamethasone in patients with high risk smoldering myeloma. Overall response rate and MRD negativity was seen in 100% of patients and this also included CR in patients with high risk FISH [137]. Another phase 2 proof of concept study, LINKER-SMM1 (NCT05955508) is also recruiting patients with high risk smoldering multiple myeloma (SMM) to test the safety, tolerability and efficacy of linvoseltamab. The phase 2 LINKER-MGUS 1 trial (NCT06140524) will soon start recruiting patients and will check the safety and efficacy of linvoseltamab in high risk monoclonal gammopathy of undetermined significance (MGUS) and non-high risk SMM.
While highly efficacious, these agents do pose certain challenges when moved to the newly diagnosed and early relapse settings. Those targeting BCMA have produced profound hypogammaglobulinemia and high rates of serious infections in the relapsed setting, including several infectious deaths [96, 98]. While acceptable in a heavily pretreated population with few available and effective treatment options, and high risk of mortality from MM itself, the level of tolerable risk will be different in a newly diagnosed patient who may be expected to live 10 years or longer. Based on early available data, from CAR T studies [138], these toxicities do appear to be lesser in earlier lines of therapy.
Comparison with other immune based therapies
Even though there are no head to head comparisons, compared to other immune based therapies like antibody drug conjugates (ADC) and chimeric antigenic receptor -T (CAR -T) cell therapies, BsAbs offer certain advantages [139]. Although CAR-T is a one-time therapy, the off-the-shelf availability of BsAbs compared to the 4–6 weeks manufacturing time for CAR- T products offer superior availability and reliability in patients who are rapidly progressing. The CAR -T products are also susceptible to 10% unpredictable manufacturing failure [140], which too makes BsAbs a more reliable option. Access to CAR-T is restricted to highly specialized centers which represents another barrier to care. Unlike CAR-T cell therapy, BsAbs does not require lymphodepletion prior to its administration. Moreover, BsAbs have a lower risk of severe immune related side effects like CRS, ICANS and delayed neurotoxicity compared to CAR -T. Phase 3 trials of CAR-T to date have shown a significant initial drop in PFS curves likely related to patients not making it to the CAR-T infusion, highlighting the importance of rapid and reliable availability of BsAbs [134, 135].
Anti-BCMA ADC like belantamab mafodotin, although being available off the shelf like BsAbs, and being effective without causing CRS/ICANS, has a lower single-agent response rate and is limited by its ocular toxicity that can significantly affect quality of life [141, 142]. This results in the need for frequent dose interruptions and delays along with the added burden of stringent ophthalmic assessment prior to each dose.
Other treatment modalities including trispecifics targeting either two myeloma antigens or an additional T-cell activator, bispecifics with structural modifications, and natural killer cell engagers are in early stages of development and have the potential to overcome some of the limitations of modern BsAbs.
Sequencing T cell directed therapies
Optimal sequencing of the various immune based treatment modalities and the different myeloma antigen targets has yet to be determined. It was shown in a sub- analysis of the KarMMa and CARTITUDE studies, that patients who were exposed to prior anti-BCMA therapies—either ADCs or BsAb, responded poorly to treatment with BCMA -CAR T products- idecabtagene vicleucel (ide-cel) and ciltacabtagene autoleucel (cilta-cel) respectively [143, 144]. On the other hand, treatment with anti BMCA BsAb after failure to anti BCMA CAR T cell therapy has shown favorable response rates, though still with short PFS [107, 145, 146]. However changing targets may prove more effective. The use of non BCMA BsAb like talquetamab and cevostamab has shown efficacy after anti BMCA therapy, though durability of responses is suboptimal [50, 84, 108, 145, 147]. Despite these exciting results many questions still remain answered. The efficacy of a different BsAb in a patient with primary refractoriness to a prior BsAb and the impact of time between T cell therapies and other intervening therapies are unclear.
Future perspectives
BsAbs have now entered routine clinical practice in multiple myeloma in the relapsed setting due to their impressive efficacy, however this only marks the beginning of a paradigm shift in myeloma treatment. Many avenues are being explored to improve upon their efficacy and safety, including moving BsAbs earlier in the patient’s treatment course, rational combinations to combat resistance mechanisms, optimizing the dose schedule including limited duration treatments, and tailoring supportive care to prevent complications. The results of ongoing and upcoming trials, as well as real-world data, will delineate the true potential of this potent new class of therapy in multiple myeloma.
Summary points
-
BsAbs have shown very high response rates and durable responses in heavily pretreated patients with multiple myeloma.
-
BsAbs are being studied in earlier lines of therapy when patients have healthier T-cell profiles.
-
Combining BsAb with other agents could mitigate resistance mechanisms and improve efficacy outcomes.
-
Infections pose a major challenge, but use of prophylactic immunoglobulins, prophylactic antimicrobials, vaccinations, and growth factors can significantly reduce the risk.
-
More data are needed on optimal sequencing of these agents with other immune-based treatment modalities.
References
Voorhees PM, Kaufman JL, Laubach J, Sborov DW, Reeves B, Rodriguez C, et al. Daratumumab, lenalidomide, bortezomib, and dexamethasone for transplant-eligible newly diagnosed multiple myeloma: the GRIFFIN trial. Blood. 2020;136:936–45.
Facon T, Kumar SK, Plesner T, Orlowski RZ, Moreau P, Bahlis N, et al. Daratumumab, lenalidomide, and dexamethasone versus lenalidomide and dexamethasone alone in newly diagnosed multiple myeloma (MAIA): overall survival results from a randomised, open-label, phase 3 trial. Lancet Oncol. 2021;22:1582–96.
Sonneveld P, Dimopoulos MA, Boccadoro M, Quach H, Ho PJ, Beksac M, et al. Phase 3 randomized study of daratumumab (DARA) + bortezomib, lenalidomide, and dexamethasone (VRd) versus Vrd alone in patients (Pts) with newly diagnosed multiple myeloma (NDMM) who are eligible for autologous stem cell transplantation (ASCT): primary results of the perseus trial. Blood. 2023;142:LBA-1-LBA.
Gandhi UH, Cornell RF, Lakshman A, Gahvari ZJ, McGehee E, Jagosky MH, et al. Outcomes of patients with multiple myeloma refractory to CD38-targeted monoclonal antibody therapy. Leukemia. 2019;33:2266–75.
Baumeister SH, Freeman GJ, Dranoff G, Sharpe AH. Coinhibitory pathways in immunotherapy for cancer. Annu Rev Immunol. 2016;34:539–73.
June CH, O’Connor RS, Kawalekar OU, Ghassemi S, Milone MC. CAR T cell immunotherapy for human cancer. Science. 2018;359:1361–5.
Goebeler ME, Bargou RC. T cell-engaging therapies - BiTEs and beyond. Nat Rev Clin Oncol. 2020;17:418–34.
Brinkmann U, Kontermann RE. Bispecific antibodies. Science. 2021;372:916–7.
Huehls AM, Coupet TA, Sentman CL. Bispecific T-cell engagers for cancer immunotherapy. Immunol Cell Biol. 2015;93:290–6.
Hosny M, Verkleij CPM, van der Schans J, Frerichs KA, Mutis T, Zweegman S, et al. Current state of the art and prospects of T cell-redirecting bispecific antibodies in multiple myeloma. J Clin Med. 2021;10:4593.
Hipp S, Tai YT, Blanset D, Deegen P, Wahl J, Thomas O, et al. A novel BCMA/CD3 bispecific T-cell engager for the treatment of multiple myeloma induces selective lysis in vitro and in vivo. Leukemia. 2017;31:1743–51.
Esensten JH, Helou YA, Chopra G, Weiss A, Bluestone JA. CD28 costimulation: from mechanism to therapy. Immunity. 2016;44:973–88.
Wu L, Seung E, Xu L, Rao E, Lord DM, Wei RR, et al. Trispecific antibodies enhance the therapeutic efficacy of tumor-directed T cells through T cell receptor co-stimulation. Nat Cancer. 2020;1:86–98.
Gantke T, Weichel M, Herbrecht C, Reusch U, Ellwanger K, Fucek I, et al. Trispecific antibodies for CD16A-directed NK cell engagement and dual-targeting of tumor cells. Protein Eng Des Sel. 2017;30:673–84.
Hoyos V, Borrello I. The immunotherapy era of myeloma: monoclonal antibodies, vaccines, and adoptive T-cell therapies. Blood. 2016;128:1679–87.
Watkins-Yoon J, Guzman W, Oliphant A, Haserlat S, Leung A, Chottin C, et al. CTX-8573, an innate-cell engager targeting BCMA, is a highly potent multispecific antibody for the treatment of multiple myeloma. Blood. 2019;134:3182.
Frerichs KA, Broekmans MEC, Marin Soto JA, van Kessel B, Heymans MW, Holthof LC, et al. Preclinical activity of JNJ-7957, a novel BCMA×CD3 bispecific antibody for the treatment of multiple myeloma, is potentiated by daratumumab. Clin Cancer Res. 2020;26:2203–15.
Seckinger A, Delgado JA, Moser S, Moreno L, Neuber B, Grab A, et al. Target expression, generation, preclinical activity, and pharmacokinetics of the BCMA-T Cell bispecific antibody EM801 for multiple myeloma treatment. Cancer Cell. 2017;31:396–410.
Gantke T, Reusch U, Kellner C, Ellwanger K, Fucek I, Weichel M, et al. AFM26 is a novel, highly potent BCMA/CD16A-directed bispecific antibody for high affinity NK-cell engagement in multiple myeloma. J Clin Oncol. 2017;35:8045.
Zou J, Chen D, Zong Y, Ye S, Tang J, Meng H, et al. Immunotherapy based on bispecific T-cell engager with hIgG1 Fc sequence as a new therapeutic strategy in multiple myeloma. Cancer Sci. 2015;106:512–21.
Chen D, Zou J, Zong Y, Meng H, An G, Yang L. Anti-human CD138 monoclonal antibodies and their bispecific formats: generation and characterization. Immunopharmacol Immunotoxicol. 2016;38:175–83.
He X, Zhang Y, Lai YW, Baguley S, Li Y, Cao X, et al. Preclinical characterization of an ANTI-CD38/CD3 T CELL-redirecting bispecific antibody. Blood. 2019;134:4463.
Kodama T, Kochi Y, Nakai W, Mizuno H, Baba T, Habu K, et al. Anti-GPRC5D/CD3 bispecific T-cell-redirecting antibody for the treatment of multiple myeloma. Mol Cancer Ther. 2019;18:1555–64.
Chan WK, Kang S, Youssef Y, Glankler EN, Barrett ER, Carter AM, et al. A CS1-NKG2D bispecific antibody collectively activates cytolytic immune cells against multiple myeloma. Cancer Immunol Res. 2018;6:776–87.
Wang Y, Li H, Xu W, Pan M, Qiao C, Cai J, et al. BCMA-targeting bispecific antibody that simultaneously stimulates NKG2D-enhanced efficacy against multiple myeloma. J Immunother. 2020;43:175–88.
Lee L, Bounds D, Paterson J, Herledan G, Sully K, Seestaller-Wehr LM, et al. Evaluation of B cell maturation antigen as a target for antibody drug conjugate mediated cytotoxicity in multiple myeloma. Br J Haematol. 2016;174:911–22.
Wei J, Han X, Bo J, Han W. Target selection for CAR-T therapy. J Hematol Oncol. 2019;12:62.
Tai YT, Anderson KC. B cell maturation antigen (BCMA)-based immunotherapy for multiple myeloma. Expert Opin Biol Ther. 2019;19:1143–56.
Coquery CM, Erickson LD. Regulatory roles of the tumor necrosis factor receptor BCMA. Crit Rev Immunol. 2012;32:287–305.
Darce JR, Arendt BK, Wu X, Jelinek DF. Regulated expression of BAFF-binding receptors during human B cell differentiation. J Immunol. 2007;179:7276–86.
Laurent SA, Hoffmann FS, Kuhn PH, Cheng Q, Chu Y, Schmidt-Supprian M, et al. γ-Secretase directly sheds the survival receptor BCMA from plasma cells. Nat Commun. 2015;6:7333.
Pont MJ, Hill T, Cole GO, Abbott JJ, Kelliher J, Salter AI, et al. γ-Secretase inhibition increases efficacy of BCMA-specific chimeric antigen receptor T cells in multiple myeloma. Blood. 2019;134:1585–97.
Smith EL, Harrington K, Staehr M, Masakayan R, Jones J, Long TJ, et al. GPRC5D is a target for the immunotherapy of multiple myeloma with rationally designed CAR T cells. Sci Transl Med. 2019;11:eaau7746.
Pillarisetti K, Edavettal S, Mendonça M, Li Y, Tornetta M, Babich A, et al. A T-cell-redirecting bispecific G-protein-coupled receptor class 5 member D x CD3 antibody to treat multiple myeloma. Blood. 2020;135:1232–43.
Rodriguez-Otero P, van de Donk N, Pillarisetti K, Cornax I, Vishwamitra D, Gray K, et al. GPRC5D as a novel target for the treatment of multiple myeloma: a narrative review. Blood Cancer J. 2024;14:24.
Verkleij CPM, Broekmans MEC, van Duin M, Frerichs KA, Kuiper R, de Jonge AV, et al. Preclinical activity and determinants of response of the GPRC5DxCD3 bispecific antibody talquetamab in multiple myeloma. Blood Adv. 2021;5:2196–215.
Consortium TU. UniProt: the Universal Protein Knowledgebase in 2023. Nucleic Acids Res. 2022;51:D523–31.
Inoue S, Nambu T, Shimomura T. The RAIG family member, GPRC5D, is associated with hard-keratinized structures. J Invest Dermatol. 2004;122:565–73.
Goldsmith R, Cornax I, Ma JY, Yao X, Peng P, Carreira V. P-095: normal human tissue expression of G-protein coupled receptor 5D (GPRC5D), a promising novel target for Multiple Myeloma, is restricted to plasma cells and hard keratinized tissues. Clin Lymphoma Myeloma Leuk. 2021;21:S91.
Atamaniuk J, Gleiss A, Porpaczy E, Kainz B, Grunt TW, Raderer M, et al. Overexpression of G protein-coupled receptor 5D in the bone marrow is associated with poor prognosis in patients with multiple myeloma. Eur J Clin Invest. 2012;42:953–60.
Cohen YC, Morillo D, Gatt ME, Sebag M, Kim K, Min C-K, et al. First results from the RedirecTT-1 study with teclistamab (tec) + talquetamab (tal) simultaneously targeting BCMA and GPRC5D in patients (pts) with relapsed/refractory multiple myeloma (RRMM). J Clin Oncol. 2023;41:8002.
US- and drug administration. FDA grants accelerated approval to talquetamab-tgvs for relapsed or refractory multiple myeloma. FDA.gov. August 10, 2023. Accessed July 24, 2024. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-talquetamab-tgvs-relapsed-or-refractory-multiple-myeloma.
Elkins K, Zheng B, Go M, Slaga D, Du C, Scales SJ, et al. FcRL5 as a target of antibody-drug conjugates for the treatment of multiple myeloma. Mol Cancer Ther. 2012;11:2222–32.
Davis RS, Ehrhardt GR, Leu CM, Hirano M, Cooper MD. An extended family of Fc receptor relatives. Eur J Immunol. 2005;35:674–80.
Dement-Brown J, Newton CS, Ise T, Damdinsuren B, Nagata S, Tolnay M. Fc receptor-like 5 promotes B cell proliferation and drives the development of cells displaying switched isotypes. J Leukoc Biol. 2012;91:59–67.
Polson AG, Zheng B, Elkins K, Chang W, Du C, Dowd P, et al. Expression pattern of the human FcRH/IRTA receptors in normal tissue and in B-chronic lymphocytic leukemia. Int Immunol. 2006;18:1363–73.
Li J, Stagg NJ, Johnston J, Harris MJ, Menzies SA, DiCara D, et al. Membrane-proximal epitope facilitates efficient T cell synapse formation by anti-FcRH5/CD3 and is a requirement for myeloma cell killing. Cancer Cell. 2017;31:383–95.
Dekhtiarenko I, Lelios I, Jacob W, Schneider M, Weisser M, Carlo-Stella C, et al. Co-expression of GPRC5D, FcRH5 and BCMA suggests that targeting more than one cell surface marker may be a viable strategy in relapsed/refractory multiple myeloma (RRMM): biomarker results from the phase I study of forimtamig, a GPRC5DxCD3 bispecific antibody. Blood. 2023;142:1948.
Stewart AK, Krishnan AY, Singhal S, Boccia RV, Patel MR, Niesvizky R, et al. Phase I study of the anti-FcRH5 antibody-drug conjugate DFRF4539A in relapsed or refractory multiple myeloma. Blood Cancer J. 2019;9:17.
Kumar S, Bachier CR, Cavo M, Corradini P, Delforge M, Janowski W, et al. CAMMA 2: A phase I/II trial evaluating the efficacy and safety of cevostamab in patients with relapsed/refractory multiple myeloma (RRMM) who have triple-class refractory disease and have received a prior anti-B-cell maturation antigen (BCMA) agent. J Clin Oncol. 2023;41:TPS8064.
Mastelic-Gavillet B, Navarro Rodrigo B, Décombaz L, Wang H, Ercolano G, Ahmed R, et al. Adenosine mediates functional and metabolic suppression of peripheral and tumor-infiltrating CD8(+) T cells. J Immunother Cancer. 2019;7:257.
Kennedy BE, Sadek M, Elnenaei MO, Reiman A, Gujar SA. Targeting NAD(+) synthesis to potentiate CD38-based immunotherapy of multiple myeloma. Trends Cancer. 2020;6:9–12.
Doucey M-A, Pouleau B, Estoppey C, Stutz C, Croset A, Laurendon A, et al. ISB 1342: a first-in-class CD38 T cell engager for the treatment of relapsed refractory multiple myeloma. J Clin Oncol. 2021;39:8044.
Pouleau B, Estoppey C, Suere P, Nallet E, Laurendon A, Monney T, et al. Preclinical characterization of ISB 1342, a CD38 × CD3 T-cell engager for relapsed/refractory multiple myeloma. Blood. 2023;142:260–73.
Moreau P, Garfall AL, van de Donk N, Nahi H, San-Miguel JF, Oriol A, et al. Teclistamab in relapsed or refractory multiple myeloma. N. Engl J Med. 2022;387:495–505.
Donk NWCJvd, Moreau P, Garfall AL, Bhutani M, Oriol A. et al. Long-term follow-up from MajesTEC-1 of teclistamab, a B-cell maturation antigen (BCMA) x CD3 bispecific antibody, in patients with relapsed/refractory multiple myeloma (RRMM). J Clin Oncol. 2023;41:8011.
Garfall AL, Nooka AK, Donk Nvd, NWCJvd, Moreau P, Bhutani M. et al. Long-term follow-up from the phase 1/2 MajesTEC-1 trial of teclistamab in patients with relapsed/refractory multiple myeloma. J Clin Oncol. 2024;42:7540.
Cai Z, Xia Z-j, He A-L, Dong Y, Wang Y, Liao A, et al. Results from the China Cohort of the Phase 1/2 MajesTEC-1 study of Teclistamab (TEC) treatment in patients (pts) with triple-class exposed relapsed/refractory multiple myeloma (RRMM). Paper presented at the 29th European Hematology Association conference, Madrid, Spain. May 14, 2024. Accessed on July, 24, 2024. https://library.ehaweb.org/eha/2024/eha2024-congress/421483/zhen.cai.results.from.the.china.cohort.of.the.phase.1.2.majestec-1.study.of.html.
Iida S, Kuroda Y, Matsue K, Komeno T, Ishiguro T, Ito T, et al. Primary results of a phase 1/2 study of Teclistamab, a B cell maturation antigen ((BCMA) X CD3 bispecific antibody, in Japanese patients with relapsed/refractory multiple myeloma (RRMM). Paper presented at the 29th European Hematology Association conference, Madrid Spain, May 14, 2024. Accessed on July 24, 2024. https://library.ehaweb.org/eha/2024/eha2024-congress/421489/shinsuke.iida.primary.results.of.a.phase.1.2.study.of.teclistamab.a.b-cell.html.
Firestone R, Shekarkhand T, Patel D, Tan CRC, Hultcrantz M, Lesokhin AM, et al. Evaluating the efficacy of commercial teclistamab in relapsed refractory multiple myeloma patients with prior exposure to anti-BCMA therapies. J Clin Oncol. 2023;41:8049.
Karwacz K, Hooper AT, Chang C-PB, Krupka H, Chou J, Lam V, et al. Abstract 4557: BCMA-CD3 bispecific antibody PF-06863135: preclinical rationale for therapeutic combinations. Cancer Res. 2020;80:4557.
Lesokhin AM, Tomasson MH, Arnulf B, Bahlis NJ, Miles Prince H, Niesvizky R, et al. Elranatamab in relapsed or refractory multiple myeloma: phase 2 MagnetisMM-3 trial results. Nat Med. 2023;29:2259–67.
Mohty M, Tomasson MH, Arnulf B, Bahlis NJ, Prince HM, Niesvizky R, et al. Elranatamab, a B-cell maturation antigen (BCMA)-CD3 bispecific antibody, for patients (pts) with relapsed/refractory multiple myeloma (RRMM): extended follow up and biweekly administration from the MagnetisMM-3 study. J Clin Oncol. 2023;41:8039.
Tomasson M, Iida S, Niesvizky R, Mohty M, Bahlis NJ, Martinez-Lopez J, et al. Long-term efficacy and safety of elranatamab monotherapy in the phase 2 magnetismm-3 trial in relapsed or refractory multiple myeloma (RRMM). Blood. 2023;142:3385.
Lee HC, Bumma N, Richter JR, Dhodapkar MV, Hoffman JE, Suvannasankha A, et al. LINKER-MM1 study: linvoseltamab (REGN5458) in patients with relapsed/refractory multiple myeloma. J Clin Oncol. 2023;41:8006.
Bumma N, Richter J, Jagannath S, Lee HC, Hoffman JE, Suvannasankha A, et al. Linvoseltamab for treatment of relapsed/refractory multiple myeloma. J Clin Oncol 2024;42:2702–2712.
Regeneron. New York. Linvoseltamab Biologics License Application for treatment of relapsed/refractory multiple myeloma accepted for FDA priority review. investor.regeneron.com. February 21, 2024. Accessed July 14, 2024. https://investor.regeneron.com/news-releases/news-release-details/linvoseltamab-bla-treatment-relapsedrefractory-multiple-myeloma.
Voorhees PM, D’Souza A, Weisel K, Hurd DD, Teipel R, Chung A, et al. A phase 1 first-in-human study of Abbv-383, a BCMA × CD3 bispecific T-cell-redirecting antibody, as monotherapy in patients with relapsed/refractory multiple myeloma. Blood. 2022;140:4401–4.
Sharon D, Robinson V, Hecquet C, Calabrese K, Cosgrove C, Mantis C, et al. Bivalent BCMA binding and low affinity CD3 T-cell engagement by abbv-383 drives sustained activation with reduced T-cell exhaustion in preclinical models of multiple myeloma. Blood. 2023;142:4666.
Costa LJ, Wong SW, Bermúdez A, de la Rubia J, Mateos M-V, Ocio EM, et al. First clinical study of the B-cell maturation antigen (BCMA) 2+1 T cell engager (TCE) CC-93269 in patients (Pts) with relapsed/refractory multiple myeloma (RRMM): interim results of a phase 1 multicenter trial. Blood. 2019;134:143.
Sun M, Qiu L, Wei Y, Jin J, Li X, Liu X, et al. Results from a first-in-human phase I study of F182112, a B-cell maturation antigen (BCMA)-CD3 bispecific antibody, in patients with relapsed/refractory multiple myeloma. J Clin Oncol. 2023;41:8038.
Topp MS, Duell J, Zugmaier G, Attal M, Moreau P, Langer C, et al. Anti-B-cell maturation antigen BiTE molecule AMG 420 induces responses in multiple myeloma. J Clin Oncol. 2020;38:775–83.
Harrison SJ, Minnema MC, Lee HC, Spencer A, Kapoor P, Madduri D, et al. A phase 1 first in human (FIH) study of AMG 701, an anti-B-cell maturation antigen (BCMA) half-life extended (HLE) BiTE® (bispecific T-cell engager) molecule, in relapsed/refractory (RR) multiple myeloma (MM). Blood. 2020;136:28–9.
Schinke, Touzeau CD, Minnema C, Donk MC, NWCJvd, Rodríguez-Otero P, et al. Pivotal phase 2 monumenTAL-1 results of talquetamab (tal), a GPRC5DxCD3 bispecific antibody (BsAb), for relapsed/refractory multiple myeloma (RRMM). J Clin Oncol. 2023;41:8036.
Rasche L, Schinke C, Trouzeau C, Minnema M, Donk NWCJV, Otero PR, et al. Long- term efficacy and safety results from the phase 1/2 MonumenTAL -1 study of Talquetamab, a GPRC5D×CD3 bispecific antibody in patients with relapsed/ refractory multiple myeloma. EHA Libr. 2024;420979:P915.
Carlo-Stella C, Mazza R, Manier S, Facon T, Yoon S-S, Koh Y, et al. RG6234, a GPRC5DxCD3 T-cell engaging bispecific antibody, is highly active in patients (pts) with relapsed/refractory multiple myeloma (RRMM): updated intravenous (IV) and first subcutaneous (SC) results from a phase I dose-escalation study. Blood. 2022;140:397–9.
Trudel S, Cohen AD, Krishnan AY, Fonseca R, Spencer A, Berdeja JG, et al. Cevostamab monotherapy continues to show clinically meaningful activity and manageable safety in patients with heavily pre-treated relapsed/refractory multiple myeloma (RRMM): updated results from an ongoing phase I study. Blood. 2021;138:157.
Lesokhin AM, Richter J, Trudel S, Cohen AD, Spencer A, Forsberg PA, et al. Enduring responses after 1-year, fixed-duration cevostamab therapy in patients with relapsed/refractory multiple myeloma: early experience from a phase I study. Blood. 2022;140:4415–7.
Krejcik J, Casneuf T, Nijhof IS, Verbist B, Bald J, Plesner T, et al. Daratumumab depletes CD38+ immune regulatory cells, promotes T-cell expansion, and skews T-cell repertoire in multiple myeloma. Blood. 2016;128:384–94.
Krämer I, Engelhardt M, Fichtner S, Neuber B, Medenhoff S, Bertsch U, et al. Lenalidomide enhances myeloma-specific T-cell responses in vivo and in vitro. Oncoimmunology. 2016;5:e1139662.
Cho SF, Lin L, Xing L, Li Y, Wen K, Yu T, et al. The immunomodulatory drugs lenalidomide and pomalidomide enhance the potency of AMG 701 in multiple myeloma preclinical models. Blood Adv. 2020;4:4195–207.
Meermeier EW, Welsh SJ, Sharik ME, Du MT, Garbitt VM, Riggs DL, et al. Tumor burden limits bispecific antibody efficacy through T cell exhaustion averted by concurrent cytotoxic therapy. Blood Cancer Discov. 2021;2:354–69.
Searle E, Quach H, Wong SW, Costa LJ, Hulin C, Janowski W, et al. Teclistamab in combination with subcutaneous daratumumab and lenalidomide in patients with multiple myeloma: results from one cohort of MajesTEC-2, a Phase1b, multicohort study. Blood. 2022;140:394–6.
Dholaria BR, Weisel K, Mateos M-V, Goldschmidt H, Martin TG, Morillo D, et al. Talquetamab (tal) + daratumumab (dara) in patients (pts) with relapsed/refractory multiple myeloma (RRMM): updated TRIMM-2 results. J Clin Oncol. 2023;41:8003.
Matous J, Biran N, Perrot A, Berdeja JG, Dorritie K, Elssen JV, et al. Talquetamab + pomalidomide in patients with relapsed/refractory multiple myeloma: safety and preliminary efficacy results from the phase 1b monumenTAL-2 study. Blood. 2023;142:1014.
Kumar SK, Harrison SJ, Cavo M, de la Rubia J, Popat R, Gasparetto C, et al. Venetoclax or placebo in combination with bortezomib and dexamethasone in patients with relapsed or refractory multiple myeloma (BELLINI): a randomised, double-blind, multicentre, phase 3 trial. Lancet Oncol. 2020;21:1630–42.
Schjesvold FH, Dimopoulos MA, Delimpasi S, Robak P, Coriu D, Legiec W, et al. Melflufen or pomalidomide plus dexamethasone for patients with multiple myeloma refractory to lenalidomide (OCEAN): a randomised, head-to-head, open-label, phase 3 study. Lancet Haematol. 2022;9:e98–110.
Mateos MV, Blacklock H, Schjesvold F, Oriol A, Simpson D, George A, et al. Pembrolizumab plus pomalidomide and dexamethasone for patients with relapsed or refractory multiple myeloma (KEYNOTE-183): a randomised, open-label, phase 3 trial. Lancet Haematol. 2019;6:e459–69.
Usmani SZ, Schjesvold F, Oriol A, Karlin L, Cavo M, Rifkin RM, et al. Pembrolizumab plus lenalidomide and dexamethasone for patients with treatment-naive multiple myeloma (KEYNOTE-185): a randomised, open-label, phase 3 trial. Lancet Haematol. 2019;6:e448–58.
Yu G, Boone T, Delaney J, Hawkins N, Kelley M, Ramakrishnan M, et al. APRIL and TALL-I and receptors BCMA and TACI: system for regulating humoral immunity. Nat Immunol. 2000;1:252–6.
Van Oekelen O, Gleason CR, Agte S, Srivastava K, Beach KF, Aleman A, et al. Highly variable SARS-CoV-2 spike antibody responses to two doses of COVID-19 RNA vaccination in patients with multiple myeloma. Cancer Cell. 2021;39:1028–30.
Terpos E, Gavriatopoulou M, Ntanasis-Stathopoulos I, Briasoulis A, Gumeni S, Malandrakis P, et al. Booster BNT162b2 optimizes SARS-CoV-2 humoral response in patients with myeloma: the negative effect of anti-BCMA therapy. Blood. 2022;139:1409–12.
Ramasamy K, Sadler R, Jeans S, Weeden P, Varghese S, Turner A, et al. Immune response to COVID-19 vaccination is attenuated by poor disease control and antimyeloma therapy with vaccine driven divergent T-cell response. Br J Haematol. 2022;197:293–301.
Abdallah AO, Mahmoudjafari Z, Atieh T, Ahmed N, Cui W, Shune L, et al. Neutralizing antibody responses against SARS-CoV-2 in patients with plasma cell disorders who are on active treatment after two doses of mRNA vaccination. Eur J Haematol. 2022;109:458–64.
Wu X, Wang L, Shen L, He L, Tang K. Immune response to vaccination against SARS-CoV-2 in hematopoietic stem cell transplantation and CAR T-cell therapy recipients. J Hematol Oncol. 2022;15:81.
Frerichs KA, Verkleij CPM, Mateos MV, Martin TG, Rodriguez C, Nooka A, et al. Teclistamab impairs humoral immunity in patients with heavily pretreated myeloma: importance of immunoglobulin supplementation. Blood Adv. 2024;8:194–206.
Raje N, Anderson K, Einsele H, Efebera Y, Gay F, Hammond SP, et al. Monitoring, prophylaxis, and treatment of infections in patients with MM receiving bispecific antibody therapy: consensus recommendations from an expert panel. Blood Cancer J. 2023;13:116.
Lancman G, Parsa K, Rodriguez C, Richter J, Cho HJ, Parekh S, et al. Infections and severe hypogammaglobulinemia in multiple myeloma patients treated with anti-BCMA bispecific antibodies. Blood. 2022;140:10073–4.
Lancman G, Parsa K, Kotlarz K, Avery L, Lurie A, Lieberman-Cribbin A, et al. IVIg use associated with ten-fold reduction of serious infections in multiple myeloma patients treated with anti-BCMA bispecific antibodies. Blood Cancer Discov. 2023;4:440–51.
Lancman G, Shyu M, Metzger M, Parsa K, Cho HJ, Parekh S, et al. Timing and nature of infections in multiple myeloma patients treated with anti-BCMA CAR-T cells. Blood. 2022;140:7198–9.
Golmohammadi M, Dima D, Albayyadhi M, Moradi A, Raza S, Jaberi-Douraki M. Pooled analysis on bispecific antibody-related toxicities in multiple myeloma. Blood. 2023;142:1953.
van de Donk N, Garfall A, Benboubker L, Uttervall K, Groen K, Rosiñol Dachs L, et al. Evaluation of prophylactic Tocilizumab (Toci) for the reduction of cytokie release syndrome (CRS) to inform the management of patients (pts) treated with Teclistamab in MajesTEC-1. Hemasphere. 2023;7:e43149cb.
Trudel S, Bahlis NJ, Spencer A, Kaedbey R, Rodriguez Otero P, Harrison SJ, et al. Pretreatment with tocilizumab prior to the CD3 bispecific cevostamab in patients with relapsed/refractory multiple myeloma (RRMM) showed a marked reduction in cytokine release syndrome incidence and severity. Blood. 2022;140:1363–5.
Iida S, Ito S, Yokoyama H, Ishida T, Nagai Y, Handa H, et al. Elranatamab in Japanese patients with relapsed/refractory multiple myeloma: results from MagnetisMM-2 and MagnetisMM-3. Jpn J Clin Oncol. 2024;24:hyae068.
Chari A, Oriol A, Krishnan A, Martinez Chamorro MDC, Costa L, Mateos MV, et al. Efficacy and safety of less frequent/lower intensity dosing of talquetamab in patients with relapsed/refractory multiple myeloma: results from the phase 1/2 monumenTAL-1 study. Blood. 2023;142:1010.
Lee H, Neri P, Bahlis NJ. BCMA- or GPRC5D-targeting bispecific antibodies in multiple myeloma: efficacy, safety, and resistance mechanisms. Blood. 2024;143:1211–7.
Bahlis NJ, Costello CL, Raje NS, Levy MY, Dholaria B, Solh M, et al. Elranatamab in relapsed or refractory multiple myeloma: the MagnetisMM-1 phase 1 trial. Nat Med. 2023;29:2570–6.
Chari A, Minnema MC, Berdeja JG, Oriol A, van de Donk N, Rodríguez-Otero P, et al. Talquetamab, a T-cell-redirecting GPRC5D bispecific antibody for multiple myeloma. N. Engl J Med. 2022;387:2232–44.
Verkleij CPM, Broekmans M, Wong A, Zweegman S, Verona R, Adams H, et al. Mechanisms of resistance and determinants of response of the GPRC5D-targeting T-cell redirecting bispecific antibody JNJ-7564 in multiple myeloma. Blood. 2020;136:8–9.
Friedrich MJ, Neri P, Kehl N, Michel J, Steiger S, Kilian M, et al. The pre-existing T cell landscape determines the response to bispecific T cell engagers in multiple myeloma patients. Cancer Cell. 2023;41:711–25.e6.
Lee H, Ahn S, Maity R, Leblay N, Ziccheddu B, Truger M, et al. Mechanisms of antigen escape from BCMA- or GPRC5D-targeted immunotherapies in multiple myeloma. Nat Med. 2023;29:2295–306.
Dhodapkar MV, Krasovsky J, Osman K, Geller MD. Vigorous premalignancy-specific effector T cell response in the bone marrow of patients with monoclonal gammopathy. J Exp Med. 2003;198:1753–7.
Garfall AL, Dancy EK, Cohen AD, Hwang WT, Fraietta JA, Davis MM, et al. T-cell phenotypes associated with effective CAR T-cell therapy in postinduction vs relapsed multiple myeloma. Blood Adv. 2019;3:2812–5.
Ghermezi M, Li M, Vardanyan S, Harutyunyan NM, Gottlieb J, Berenson A, et al. Serum B-cell maturation antigen: a novel biomarker to predict outcomes for multiple myeloma patients. Haematologica. 2017;102:785–95.
Sanchez E, Li M, Kitto A, Li J, Wang CS, Kirk DT, et al. Serum B-cell maturation antigen is elevated in multiple myeloma and correlates with disease status and survival. Br J Haematol. 2012;158:727–38.
Cortes-Selva D, Casneuf T, Vishwamitra D, Stein S, Perova T, Skerget S, et al. Teclistamab, a B-cell maturation antigen (BCMA) x CD3 bispecific antibody, in patients with relapsed/refractory multiple myeloma (RRMM): correlative analyses from MajesTEC-1. Blood. 2022;140:241–3.
Chen H, Yu T, Lin L, Xing L, Cho SF, Wen K, et al. γ-secretase inhibitors augment efficacy of BCMA-targeting bispecific antibodies against multiple myeloma cells without impairing T-cell activation and differentiation. Blood Cancer J. 2022;12:118.
Offner F, Decaux O, Hulin C, Anguille S, Sophie Michallet A, Costa L, et al. Teclistamab (tec) + Nirogacestat (niro) in relapsed/refractory multiple myeloma (RRMM): The phase 1b MajesTEC-2 study. Hemasphere. 2023;7:e1257964.
America Society of Hematology. MajesTEC-2: future of BCMA-targeted bispecific, gamma secretase inhibitor combo in question. ASH clinical news. July 2023. Accessed July 24, 2024. https://ashpublications.org/ashclinicalnews/news/7213/MajesTEC-2-Future-of-BCMA-targeted-Bispecific.
Samur MK, Fulciniti M, Aktas Samur A, Bazarbachi AH, Tai Y-T, Prabhala R, et al. Biallelic loss of BCMA as a resistance mechanism to CAR T cell therapy in a patient with multiple myeloma. Nat Commun. 2021;12:868.
Da Vià MC, Dietrich O, Truger M, Arampatzi P, Duell J, Heidemeier A, et al. Homozygous BCMA gene deletion in response to anti-BCMA CAR T cells in a patient with multiple myeloma. Nat Med. 2021;27:616–9.
Truger MS, Duell J, Zhou X, Heimeshoff L, Ruckdeschel A, John M, et al. Single- and double-hit events in genes encoding immune targets before and after T cell-engaging antibody therapy in MM. Blood Adv. 2021;5:3794–8.
Feyler S, Scott GB, Parrish C, Jarmin S, Evans P, Short M, et al. Tumour cell generation of inducible regulatory T-cells in multiple myeloma is contact-dependent and antigen-presenting cell-independent. PLoS ONE. 2012;7:e35981.
Röllinghoff M, Starzinski-Powitz A, Pfizenmaier K, Wagner H. Cyclophosphamide-sensitive T lymphocytes suppress the in vivo generation of antigen-specific cytotoxic T lymphocytes. J Exp Med. 1977;145:455–9.
Schiavoni G, Sistigu A, Valentini M, Mattei F, Sestili P, Spadaro F, et al. Cyclophosphamide synergizes with type I interferons through systemic dendritic cell reactivation and induction of immunogenic tumor apoptosis. Cancer Res. 2011;71:768–78.
Zhang Z, Liu S, Zhang B, Qiao L, Zhang Y, Zhang Y. T cell dysfunction and exhaustion in cancer. Front Cell Dev Biol. 2020;8:17.
Paiva B, Gaffney B, Burnett K, Castiglioni P, Angelo M, Pierce DW, et al. Synergistic antitumor activity of alnuctamab (ALNUC; BMS-986349; CC-93269), a BCMA 2+1 T cell engager (TCE), and celmod agents in multiple myeloma (MM) preclinical models. Blood. 2022;140:7054–5.
Görgün G, Samur MK, Cowens KB, Paula S, Bianchi G, Anderson JE, et al. Lenalidomide enhances immune checkpoint blockade-induced immune response in multiple myeloma. Clin Cancer Res. 2015;21:4607–18.
Köhnke T, Krupka C, Tischer J, Knösel T, Subklewe M. Increase of PD-L1 expressing B-precursor ALL cells in a patient resistant to the CD19/CD3-bispecific T cell engager antibody blinatumomab. J Hematol Oncol. 2015;8:111.
Feucht J, Kayser S, Gorodezki D, Hamieh M, Döring M, Blaeschke F, et al. T-cell responses against CD19+ pediatric acute lymphoblastic leukemia mediated by bispecific T-cell engager (BiTE) are regulated contrarily by PD-L1 and CD80/CD86 on leukemic blasts. Oncotarget. 2016;7:76902–19.
Swamydas M, Murphy EV, Ignatz-Hoover JJ, Malek E, Driscoll JJ. Deciphering mechanisms of immune escape to inform immunotherapeutic strategies in multiple myeloma. J Hematol Oncol. 2022;15:17.
Mishra AK, Schmidt TM, Martell EB, Chen AS, Dogru RE, Hematti P, et al. PD1(+)TIGIT(+)2B4(+)KLRG1(+) cells might underlie T cell dysfunction in patients treated with BCMA-directed chimeric antigen receptor T cell therapy. Transpl Cell Ther. 2024;30:191–202.
Danhof S, Schreder M, Knop S, Rasche L, Strifler S, Löffler C, et al. Expression of programmed death-1 on lymphocytes in myeloma patients is lowered during lenalidomide maintenance. Haematologica. 2018;103:e126–9.
Rodriguez-Otero P, Ailawadhi S, Arnulf B, Patel K, Cavo M, Nooka AK, et al. Ide-cel or standard regimens in relapsed and refractory multiple myeloma. N. Engl J Med. 2023;388:1002–14.
San-Miguel J, Dhakal B, Yong K, Spencer A, Anguille S, Mateos MV, et al. Cilta-cel or standard care in lenalidomide-refractory multiple myeloma. N. Engl J Med. 2023;389:335–47.
Chung DJ, Pronschinske KB, Shyer JA, Wu V, Hassoun H, Landau H, et al. Immune reconstitution after autologous stem cell transplantation for multiple myeloma. Biol Blood Marrow Transplant. 2014;20:S60–2.
Nadeem O, Magidson S, Midha S, O’Donnell EK, Hartley-Brown MA, Sperling AS, et al. Immuno-PRISM: a randomized phase II platform study of bispecific antibodies in high-risk smoldering myeloma. Blood. 2023;142:206.
Yong, Harrison K, Mateos SJ, Moreau M-V, Donk P, NWCJvd, et al. First phase 3 results from CARTITUDE-4: Cilta-cel versus standard of care (PVd or DPd) in lenalidomide-refractory multiple myeloma. J Clin Oncol. 2023;41:LBA106.
Subklewe M. BiTEs better than CAR T cells. Blood Adv. 2021;5:607–12.
Majzner RG, Mackall CL. Clinical lessons learned from the first leg of the CAR T cell journey. Nat Med. 2019;25:1341–55.
Lonial S, Nooka AK, Thulasi P, Badros AZ, Jeng BH, Callander NS, et al. Management of belantamab mafodotin-associated corneal events in patients with relapsed or refractory multiple myeloma (RRMM). Blood Cancer J. 2021;11:103.
Lonial S, Lee HC, Badros A, Trudel S, Nooka AK, Chari A, et al. Longer term outcomes with single-agent belantamab mafodotin in patients with relapsed or refractory multiple myeloma: 13-month follow-up from the pivotal DREAMM-2 study. Cancer. 2021;127:4198–212.
Hansen DK, Sidana S, Peres LC, Colin Leitzinger C, Shune L, Shrewsbury A, et al. Idecabtagene vicleucel for relapsed/refractory multiple myeloma: real-world experience from the myeloma CAR T consortium. J Clin Oncol. 2023;41:2087–97.
Cohen AD, Mateos MV, Cohen YC, Rodriguez-Otero P, Paiva B, van de Donk N, et al. Efficacy and safety of cilta-cel in patients with progressive multiple myeloma after exposure to other BCMA-targeting agents. Blood. 2023;141:219–30.
Van Oekelen O, Nath K, Mouhieddine TH, Farzana T, Aleman A, Melnekoff DT, et al. Interventions and outcomes of patients with multiple myeloma receiving salvage therapy after BCMA-directed CAR T therapy. Blood. 2023;141:756–65.
Touzeau C, Krishnan AY, Moreau P, Perrot A, Usmani SZ, Manier S, et al. Efficacy and safety of teclistamab (tec), a B-cell maturation antigen (BCMA) × CD3 bispecific antibody, in patients (pts) with relapsed/refractory multiple myeloma (RRMM) after exposure to other BCMA-targeted agents. J Clin Oncol. 2022;40:8013.
Jakubowiak AJ, Anguille S, Karlin L, Chari A, Schinke C, Rasche L, et al. Updated results of talquetamab, a GPRC5D × CD3 bispecific antibody, in patients with relapsed/refractory multiple myeloma with prior exposure to T-cell redirecting therapies: results of the phase 1/2 MonumenTAL-1 study. Blood. 2023;142:3377.
Author information
Authors and Affiliations
Contributions
AJD and GL conceptualized the draft. AJD wrote the original draft. AC and GL critically reviewed and edited the manuscript. All authors have read and agreed to the final version submitted for publication.
Corresponding author
Ethics declarations
Competing interests
AJD has no conflicts to declare. AC receives consultancy from Abbvie, Adaptive, Amgen, Antengene, Bristol Myers Squibb, Forus, Genetech/Roche, Glaxo Smith Klein, Janssen, Karyopharm, Millenium/Takeda, Sanofi/Genzyme; and research funding from Janssen. GL receives consultancy from Janssen and Takeda, honoraria from Janssen, Takeda, Forus, Sanofi & Pfizer.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Devasia, A.J., Chari, A. & Lancman, G. Bispecific antibodies in the treatment of multiple myeloma. Blood Cancer J. 14, 158 (2024). https://doi.org/10.1038/s41408-024-01139-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41408-024-01139-y
- Springer Nature Limited