Abstract
Chronic respiratory diseases’ (CRDs) impact on re-intubation rate remains unclear. We investigated the association between these factors in mechanically ventilated patients. Data were extracted from the freely available online Medical Information Mart for Intensive Care III database. CRDs were defined according to ICD-9 codes. Generalised linear regression and propensity score matching were performed. Of 13,132 patients, 7.9% required re-intubation. Patients with chronic obstructive pulmonary disease (COPD) had higher re-intubation (OR 2.48, 95% CI 1.83–3.33) and mortality rates (OR 1.64, 95% CI 1.15–2.34) than those without. Patients with asthma had a lower mortality rate (OR 0.63, 95% CI 0.43–0.92) but a similar re-intubation rate to those of patients without. These findings remained stable after propensity score matching and bootstrapping analysis. The association of COPD with re-intubation was significantly stronger in patients with high oxygen-partial pressure (PaO2) or mild disease severity but was independent of carbon dioxide partial pressure. Corticosteroid use was associated with increased re-intubation rates in subgroups without CRDs (OR 1.77–1.99, p < 0.001) but not in subgroups with CRDs. COPD patients with high post-extubation PaO2 or mild disease severity should be carefully monitored as they have higher re-intubation and mortality rates.
Similar content being viewed by others
Introduction
Mechanical ventilation (MV) is a common respiratory support method in the intensive care unit (ICU). Millions of patients receive invasive MV in the United States each year1,2. Successful extubation is important for these patients, as extubation failure is associated with poor outcomes, including high mortality rates ranging from 25 to 50%3,4,5. However, despite multiple weaning protocols, such as the spontaneous breathing trial6, the overall re-intubation rate remains high at 10%3,7, and even exceeds 20% in high-risk patients8. Thus, identifying patients with a high re-intubation risk may be important for clinicians.
Chronic respiratory diseases (CRDs) such as chronic obstructive pulmonary disease (COPD), asthma, and bronchiectasis are common comorbidities in patients in ICUs. Impaired respiratory strength is common in patients with CRDs and often leads to poor efficiency in ventilation9,10,11, even in patients who are stable. Evidence indicates that altered inspiratory and expiratory strength often leads to an increased risk of extubation failure12,13, and studies have reported re-intubation rates as high as 20–30% in patients with CRDs14,15,16.
One cohort study5 has reported that chronic cardiac or respiratory disease may be a risk factor for extubation failure in patients aged > 65 years. However, the heterogeneous effect of different CRDs on re-intubation rate among ICU patients on MV has not been well established.
This study aimed to investigate the associations between different CRDs and re-intubation rate and evaluate the impact of corticosteroids on re-intubation rate. We hypothesised that different CRDs may have differing effects on the prognosis of patients in ICUs.
Results
Baseline characteristics
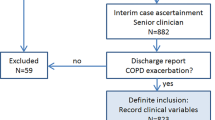
A total of 13,132 patients were included in this analysis (Supplementary Fig. S1). The re-intubation rate was 7.9% (Table 1). The duration of the first intubation and the total ICU length of stay were significantly longer in the re-intubation group than in the successful extubation group. Overall, the proportion of patients with CRDs was 9.5% (1250/13,132) in this cohort. Compared to that in the successful extubation group, the proportion of patients with COPD was significantly higher in the re-intubation group (61/1042 vs. 255/12,090, p < 0.001), whereas the proportion of patients with asthma was comparable in both groups (75/1042 vs. 800/12,090, p = 0.471). Patients in the re-intubation group were more likely to receive corticosteroids after extubation. The detailed comparisons of baseline characteristics are presented in Table 1.
Re-intubation rate within different CRDs
Crude comparisons
The crude re-intubation rate and the duration of the first intubation were significantly lower in patients without CRDs than in those with CRDs (899/11,882 patients vs. 143/1250 patients, p < 0.001, and 14 [range 5–44] hours vs. 17 [range 6–61] hours, p < 0.001, respectively; Table 2). Likewise, in the comparison between patients without and with COPD, the re-intubation rate (981/11,835 [8.2%] vs. 61/316 [19.3%], respectively; p < 0.001) and the duration of the first intubation (14 [range 5–44] hours vs. 29 [range 9–78] hours, respectively; p < 0.001) were significantly lower in patients without COPD. However, the re-intubation rate and the duration of the first intubation were not significantly different between the asthma and no-asthma groups.
Adjusted outcomes
Potential confounders were adjusted in the multivariable logistic models (Table 3). The odds ratio (OR) for re-intubation was significant in patients with CRDs (OR 1.51, 95% CI 1.24–1.83, p < 0.001) and in those with COPD (OR 2.48, 95% CI 1.83–3.33, p < 0.001). However, for asthma, the OR for re-intubation was non-significant. All results were found to be stable in the logistic models after applying bootstrap techniques with 1000 resamples.
Outcomes after PSM
The comparison of re-intubation rate was also verified using PSM. A total of 316 patients from the COPD group and 1147 patients from the no-COPD group were well matched using a 1:4 matching algorithm (Table 4). The overall quality of the matched sample was assessed by graphically inspecting the propensity scores between the groups (Supplementary Fig. S2), and the mean standardised difference was < 10% in all covariates, which demonstrated substantial improvement in covariate balance across the treatment groups. Among the matched cases, re-intubation was significantly higher in the COPD group (61/316 vs. 90/1147, p < 0.001), and patients with COPD were more likely to have a longer intubation duration and ICU stay. However, in matched patients with and without asthma, the re-intubation rates were comparable between these two groups.
Interaction between COPD and clinical parameters
A significant interaction was detected between COPD and post-extubation oxygen partial pressure (PaO2, p = 0.008; Fig. 1). The association between COPD and re-intubation rate was considerably stronger in patients with high PaO2 (≥ 120 mmHg, OR 4.30, 95% CI 2.41–5.97, p < 0.001) than in those with low PaO2 (< 120 mmHg, OR 1.70, 95% CI 1.14–2.53, p = 0.009). A significant interaction was also found between COPD and Sequential Organ Failure Assessment (SOFA) scores (both the initial and maximum scores), and the association between COPD and the re-intubation rate was considerably stronger in patients with mild disease severity, than the association in those with severe disease severity. No significant interaction was found between COPD and carbon dioxide partial pressure (PaCO2) in the current study.
Factors influencing the impact of COPD on re-intubation rate. The impact of COPD on re-intubation rate was found to be affected by post-extubation PaO2 and SOFA but not by PaCO2. SOFA sequential organ failure assessment, COPD chronic obstructive pulmonary disease, PaCO2 carbon dioxide partial pressure.
Impact of corticosteroids on re-intubation
The association between post-extubation corticosteroid use and re-intubation rate was investigated in different subgroups. After adjusting for covariates, corticosteroid use was found to be consistently associated with an increased re-intubation rate in the subgroups without respiratory diseases (ORs 1.77–1.99, p < 0.001; Fig. 2), but its association was non-significant in the subgroups with respiratory diseases (CRDs: OR 1.33, p = 0.142; COPD: OR 1.15, p = 0.660; asthma: OR 0.9, p = 0.748).
Association between post-extubation corticosteroid use and re-intubation rate in patients with different respiratory diseases. The p for interaction is 0.199, 0.155, and 0.029 in groups with/without CRDs, COPD, and asthma, respectively. COPD chronic obstructive pulmonary disease, CRDs chronic respiratory diseases.
In-hospital mortality rates in terms of different CRDs
Crude comparisons
The crude in-hospital mortality rate was higher in the COPD group than in the no-COPD group (40/316 vs. 678/11,835, p < 0.001; Table 2), while the in-hospital mortality rate was lower in the asthma group than in the no-asthma group (30/875 vs. 688/12,257, respectively; p = 0.006).
Adjusted outcomes
After adjusting for confounders in the multivariable logistic models (Table 3), COPD was associated with an increased risk of in-hospital mortality (OR 1.64, 95% CI 1.15–2.34, p = 0.007). However, asthma appeared to be a protective factor for in-hospital mortality (OR 0.63, 95% CI 0.43–0.92, p = 0.019). The overall OR for in-hospital mortality concerning CRDs was not significant.
Outcomes after PSM
Among matched patients with and without COPD, the in-hospital mortality rate was significantly higher in the COPD patient group (40/316 vs. 89/1147, p = 0.007). In matched patients with and without asthma, a decreased in-hospital mortality rate was found in the asthma group (30/875 vs. 156/2865, p = 0.016).
Discussion
There were three major findings in this study. First, CRDs were present in 9.5% of critically ill patients on MV, and different CRDs had different impacts on the prognosis of these patients. Second, the re-intubation rate was significantly higher in patients with COPD, and this association was even stronger in patients with mild disease severity or high post-extubation PaO2, but was independent of post-extubation PaCO2. In patients with asthma, the association with re-intubation rate was non-significant. Third, post-extubation corticosteroid use was significantly associated with an increased re-intubation rate in patients without CRDs, but was non-significant in patients with CRDs. These findings remained stable after adjusting for covariates and PSM.
Successful extubation plays an essential role in critical care as both prolonged MV and extubation failure have been found to be associated with a poor prognosis3,17. However, current re-intubation rates remain as high as 10–20%. Strategies to identify patients at high risk for extubation failure are essential to improve the management of weaning and extubation. Many risk factors, such as age, disease severity, and intubation duration, have been reported for extubation failure18. However, studies assessing the effect of different CRDs on the re-intubation rate remain scarce.
One cohort study5 investigated the extubation failure rate in medical ICU patients and found that mixed chronic cardiac or respiratory disease may be a risk factor for extubation failure in patients aged > 65 years (34% vs. 9%, p < 0.01). However, owing to that study’s limited sample size, chronic respiratory and cardiac diseases were classified as one group and the adjusted impact of different CRDs was not investigated. Chu et al.19 assessed factors associated with re-intubation within 14 days after weaning from the ventilator and found that the primary reasons for intubation, including COPD, were also significant risks for re-intubation. Different from our study, the overall re-intubation rate was significantly low in Chu et al.’s study (2.8% vs 7.9%), suggesting possible heterogeneity between the two cohorts. In addition, only acute exacerbation of COPD was analysed and the impact of stable COPD or other CRDs remained undetermined.
In this study, we found that different CRDs had different impacts on re-intubation rate. A significant association between COPD and re-intubation rate was confirmed in the multivariable logistic model and PSM. This finding was not unexpected, as a prolonged high workload of the respiratory muscles makes respiratory muscle fatigue common in these patients20,21,22. Moreover, we noted that this association interacted with PaO2 but was independent of PaCO2. The possible mechanisms cannot be inferred due to the retrospective design of our study. However, several studies have indicated that in patients with COPD receiving oxygen therapy23, the respiratory response to CO2 could be blunted due to high PaO2, which leads to hypoventilation after extubation. Furthermore, it has been reported that hyperoxia is associated with lung oxidant/antioxidant imbalance24,25. Whether these mechanisms contribute to an increased re-intubation risk in patients with high PaO2 requires further investigation.
In clinical practice, an elevated but stable PaCO2 is often permitted in patients with COPD requiring extubation. However, whether this mild hypercapnia may lead to a higher extubation failure in patients with COPD has not been investigated. Contou et al.26 reported that in patients with severe cardiogenic pulmonary oedema, hypercapnia did not increase the rate of intubation or prolong non-invasive ventilation. However, no confounder correction or interaction analysis was performed due to the small sample size. In this study, we found the association between COPD and re-intubation rate was not affected by post-extubation PaCO2, after adjusting for confounders. However, we also noted that 95% of the patients in our study had a post-extubation PaCO2 of < 55 mmHg. Therefore, whether a higher PaCO2 would have resulted in a different interaction with COPD should be investigated in future studies.
Furthermore, we found that the association between COPD and re-intubation rate was even stronger in the patient subgroup with mild disease severity, than the association in those with severe disease severity. In patients with severe disease severity, many factors may lead to extubation failure, such as low PaO2/FiO227, a rapid shallow breathing index28, and ICU-related weakness and respiratory muscle insufficiency12,13,29,30,31. Therefore, it is possible that the association between COPD and re-intubation may be weakened or even undetectable in patients with severe condition.
We also noted that the association between asthma and re-intubation was not significant. In contrast to patients with COPD, patients with asthma may have had relatively normal respiratory function, which could explain this result. We also observed that asthma was significantly associated with decreased mortality. This finding has not previously been reported concerning patients in ICUs. However, similar findings have been reported in patients with influenza. In a multicentre retrospective analysis involving 1520 patients with influenza, Myles et al.32 found that patients with asthma were less likely to require intensive care or die compared with those without asthma. Similarly, two other studies33,34 have also reported that patients with a history of asthma had a lower in-hospital mortality rate than that of patients without asthma. Several reasons have been proposed for these findings32,33,34, such as early admission, mild disease severity, and rapid response to treatment. In our study, we noted that patients with asthma were significantly younger that those without asthma. However, our findings remained stable after adjusting for this factor. More studies are required to further investigate possible relevant mechanisms.
Finally, we found that corticosteroid use was associated with an increased re-intubation rate in subgroups without CRDs, but not in subgroups with CRDs. Concerning patients post-extubation, corticosteroids are more commonly prescribed for patients with extubation failure risk factors, such as hypoxemia and lung infiltration. Therefore, there is a risk that the true efficacy of corticosteroid use may be offset by its close relationship with extubation failure factors, due to its selective use in clinical practice35. However, this finding still indicates that the efficacy of corticosteroids may vary in relation to CRDs, and this needs to be further investigated in future studies.
This study had several limitations. First, the MIMIC III recorded data from 2001 to 2012, during which time there were major changes to extubation guidelines. Therapeutic bias should be considered when interpreting the findings. Second, due to our study’s retrospective design, specific reasons for ICU admission or MV could not be ascertained and, therefore, were not included in the analysis. Moreover, although we included as many potential confounders as possible, there remains a risk that some potential confounding factors, such as non-invasive ventilation application, COPD severity, or pulmonary function status, were not accounted for. Third, only COPD and asthma were analysed in the current study, and due to the limited number of patients, other types of CRDs such as bronchiectasis were not evaluated. Furthermore, re-intubation was defined as all re-intubation events occurring during the entire hospital stay. Whether our findings would vary if we used different re-intubation definitions remains unclear. Finally, this was a single-centre study, and the applicability of the conclusions remains uncertain. Nevertheless, our study findings may provide a solid foundation for further research.
In conclusion, this study showed that different CRDs may impact patients on MV differently. The association between COPD and re-intubation rate was influenced by disease severity and PaO2. More attention should be paid to patients with COPD after extubation, especially to those with mild disease severity. Titrating oxygen saturation to avoid hyperoxia may be beneficial. More studies are required to investigate the underlying mechanisms in relation to our observations and to further validate our findings.
Methods
Data sources
Data were extracted from the Medical Information Mart for Intensive Care III (MIMIC III)36 database, which is an online database containing detailed information concerning > 40,000 patients in ICUs of Beth Israel Deaconess Medical Centre. Patient information was anonymised for privacy. The Institutional Review Board of Massachusetts Institute of Technology for Publications approved publication of the database information and of this study and waived the requirement for informed patient consent. Researchers who passed an online training test and were authorized to access this database. Y.S. was responsible for data extraction (certification NO. 1564657). The study protocol was performed in accordance with the relevant guidelines.
Patient selection
All patients who had intubation records were initially screened, and those with the following conditions were excluded: records indicating tracheotomy status, no record of extubation, age < 18 years, length of ICU stay < 24 h, and a diagnosis indicating intracranial haemorrhage. If one patient was found to have had multiple admissions or re-intubation records, only data from their first admission or first re-intubation were used.
Data extraction
Data concerning patient demographics and comorbidities were extracted. As the current study aimed to determine the potential risk for re-intubation, other information such as biochemical and drug records was also recorded within the period between extubation and re-intubation. Re-intubation was the primary endpoint, which was defined as all re-intubation events that occurred throughout a hospital stay. In-hospital mortality was the secondary endpoint.
Definition of CRDs
COPD, asthma, bronchiectasis, and pulmonary or pleural tuberculosis were defined as CRDs. Three diagnostic codes indicating COPD were identified in the MIMIC III database. Diagnostic codes referring to any form of asthma (for example, extrinsic asthma, intrinsic asthma, acute asthma exacerbation, cough variant asthma) were considered as indicative of asthma. The detailed ICD-9 codes for these diseases are listed in the Supplementary file 1.
Definition of corticosteroid use
Details on the systemic use (enteral or intravenous) of different types of corticosteroids (for example, dexamethasone, methylprednisolone, prednisone, hydrocortisone) were extracted from this database. Inhalatory corticosteroid use was excluded. Patients with records indicating corticosteroid use within the extubation and re-intubation periods were designated as a corticosteroid use group.
Missing data management
Most continuous variables in the current study had < 5% missing values, which were replaced with their mean or median values. Variables with > 20% missing values were not filled. For dichotomous variables, a missing value was replaced with a default value (zero).
Statistical analysis
Continuous variables were presented as mean (± standard deviation) or median (interquartile range). A student’s t-test or Wilcoxon rank-sum test was used as appropriate. Categorical data were compared using a chi-square test and expressed as proportions. To adjust for the potential impact of possible confounders, variables with a p-value < 0.2 in the univariable comparison were included in the initial model. A stepwise approach method was used to build the final logistic model. Multicollinearity was tested using the variance inflation factor (VIF) method, with a VIF ≥ 5 indicating multicollinearity. To test the stability of these logistic models, bootstrap techniques using 1000 resamples were performed. Subgroup analysis was performed in patients with COPD or asthma. Propensity score matching (PSM) was used to minimise the effect of confounding factors such as biochemical indices and disease severity, which could have led to biased outcomes. The propensity score was estimated using a logistic regression model. A one-to-four nearest-neighbour-matching algorithm was applied with a calliper of 0.05. Age, sex, hypertension, diabetes, renal replacement therapy, maximum SOFA score during ICU stay, duration of intubation, vasopressor use within the first 24 h, serum creatinine level, haemoglobin level, potassium level, and sodium level were selected to generate the propensity score. A bias in the mean (or proportion) of the covariates between the two groups was examined using the standardised difference before and after PSM37,38. To test for bias due to imbalance in unmeasured covariates in the PSM, sensitivity analyses were performed to quantify the degree of hidden bias needed to invalidate the main conclusions. A two-tailed test was performed, and a p-value < 0.05 was considered statistically significant. All statistical analyses were performed using STATA version 14.0 (College Station, TX, USA) software.
References
Wunsch, H. et al. The epidemiology of mechanical ventilation use in the United States. Crit. Care Med. 38, 1947–1953. https://doi.org/10.1097/CCM.0b013e3181ef4460 (2010).
Adhikari, N. K., Fowler, R. A., Bhagwanjee, S. & Rubenfeld, G. D. Critical care and the global burden of critical illness in adults. Lancet 376, 1339–1346. https://doi.org/10.1016/S0140-6736(10)60446-1 (2010).
Thille, A. W., Richard, J. C. & Brochard, L. The decision to extubate in the intensive care unit. Am. J. Respir. Crit. Care Med. 187, 1294–1302. https://doi.org/10.1164/rccm.201208-1523CI (2013).
Epstein, S. K., Ciubotaru, R. L. & Wong, J. B. Effect of failed extubation on the outcome of mechanical ventilation. Chest 112, 186–192. https://doi.org/10.1378/chest.112.1.186 (1997).
Thille, A. W., Harrois, A., Schortgen, F., Brun-Buisson, C. & Brochard, L. Outcomes of extubation failure in medical intensive care unit patients. Crit. Care Med. 39, 2612–2618. https://doi.org/10.1097/CCM.0b013e3182282a5a (2011).
Ouellette, D. R. et al. Liberation from mechanical ventilation in critically ill adults: An official American College of Chest Physicians/American Thoracic Society Clinical Practice Guideline: Inspiratory pressure augmentation during spontaneous breathing trials, protocols minimizing sedation, and noninvasive ventilation immediately after extubation. Chest 151, 166–180. https://doi.org/10.1016/j.chest.2016.10.036 (2017).
Thille, A. W., Cortes-Puch, I. & Esteban, A. Weaning from the ventilator and extubation in ICU. Curr. Opin. Crit. Care 19, 57–64. https://doi.org/10.1097/MCC.0b013e32835c5095 (2013).
Esteban, A. et al. Evolution of mortality over time in patients receiving mechanical ventilation. Am. J. Respir. Crit. Care Med. 188, 220–230. https://doi.org/10.1164/rccm.201212-2169OC (2013).
Templeman, L. & Roberts, F. Effectiveness of expiratory muscle strength training on expiratory strength, pulmonary function and cough in the adult population: A systematic review. Physiotherapy 106, 43–51. https://doi.org/10.1016/j.physio.2019.06.002 (2020).
Chiu, K. L. et al. Exercise training increases respiratory muscle strength and exercise capacity in patients with chronic obstructive pulmonary disease and respiratory muscle weakness. Heart Lung https://doi.org/10.1016/j.hrtlng.2020.03.005 (2020).
Geltser, B. I., Kurpatov, I. G., Dej, A. A. & Kozhanov, A. G. Respiratory muscles dysfunction and respiratory diseases. Ter. Arkh. 91, 93–100. https://doi.org/10.26442/00403660.2019.03.000108 (2019).
Hermans, G. & Van den Berghe, G. Clinical review: Intensive care unit acquired weakness. Crit. Care 19, 274. https://doi.org/10.1186/s13054-015-0993-7 (2015).
Latronico, N. & Bolton, C. F. Critical illness polyneuropathy and myopathy: A major cause of muscle weakness and paralysis. Lancet Neurol. 10, 931–941. https://doi.org/10.1016/S1474-4422(11)70178-8 (2011).
Vargas, F. et al. Intermittent noninvasive ventilation after extubation in patients with chronic respiratory disorders: A multicenter randomized controlled trial (VHYPER). Intensive Care Med. 43, 1626–1636. https://doi.org/10.1007/s00134-017-4785-1 (2017).
Girault, C. et al. Noninvasive ventilation and weaning in patients with chronic hypercapnic respiratory failure: A randomized multicenter trial. Am. J. Respir. Crit. Care Med. 184, 672–679. https://doi.org/10.1164/rccm.201101-0035OC (2011).
Ferrer, M. et al. Early noninvasive ventilation averts extubation failure in patients at risk: A randomized trial. Am. J. Respir. Crit. Care Med. 173, 164–170. https://doi.org/10.1164/rccm.200505-718OC (2006).
Mancebo, J. Weaning from mechanical ventilation. Eur. Respir. J. 9, 1923–1931. https://doi.org/10.1183/09031936.96.09091923 (1996).
Penuelas, O. et al. Characteristics and outcomes of ventilated patients according to time to liberation from mechanical ventilation. Am. J. Respir. Crit. Care Med. 184, 430–437. https://doi.org/10.1164/rccm.201011-1887OC (2011).
Chu, C. C. et al. Factors associated with re-intubation within 14 days after ventilator liberation. Respir. Care 62, 1557–1564. https://doi.org/10.4187/respcare.05649 (2017).
da Fonseca, J. D. M., Resqueti, V. R., Benicio, K., Fregonezi, G. & Aliverti, A. Acute effects of inspiratory loads and interfaces on breathing pattern and activity of respiratory muscles in healthy subjects. Front. Physiol. 10, 993. https://doi.org/10.3389/fphys.2019.00993 (2019).
Smith, J. A. et al. Chest wall dynamics during voluntary and induced cough in healthy volunteers. J. Physiol. 590, 563–574. https://doi.org/10.1113/jphysiol.2011.213157 (2012).
McCool, F. D. Global physiology and pathophysiology of cough: ACCP evidence-based clinical practice guidelines. Chest 129, 48S-53S. https://doi.org/10.1378/chest.129.1_suppl.48S (2006).
Chiang, L. L. et al. Respiratory response to carbon dioxide stimulation during low flow supplemental oxygen therapy in chronic obstructive pulmonary disease. J. Formos Med. Assoc. 101, 607–615 (2002).
Foschino Barbaro, M. P. et al. Oxygen therapy at low flow causes oxidative stress in chronic obstructive pulmonary disease: Prevention by N-acetyl cysteine. Free Radic. Res. 39, 1111–1118. https://doi.org/10.1080/10715760500250257 (2005).
Arkovitz, M. S., Szabo, C., Garcia, V. F., Wong, H. R. & Wispe, J. R. Differential effects of hyperoxia on the inducible and constitutive isoforms of nitric oxide synthase in the lung. Shock 7, 345–350. https://doi.org/10.1097/00024382-199705000-00006 (1997).
Contou, D. et al. Severe but not mild hypercapnia affects the outcome in patients with severe cardiogenic pulmonary edema treated by non-invasive ventilation. Ann. Intensive Care 5, 55. https://doi.org/10.1186/s13613-015-0055-y (2015).
Khamiees, M., Raju, P., DeGirolamo, A., Amoateng-Adjepong, Y. & Manthous, C. A. Predictors of extubation outcome in patients who have successfully completed a spontaneous breathing trial. Chest 120, 1262–1270. https://doi.org/10.1378/chest.120.4.1262 (2001).
Yang, K. L. & Tobin, M. J. A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation. N. Engl. J. Med. 324, 1445–1450. https://doi.org/10.1056/NEJM199105233242101 (1991).
Schroder, J. B. et al. Intubation, tracheostomy, and decannulation in patients with Guillain–Barre-syndrome-does dysphagia matter?. Muscle Nerve 59, 194–200. https://doi.org/10.1002/mus.26377 (2019).
Garnacho-Montero, J., Amaya-Villar, R., Garcia-Garmendia, J. L., Madrazo-Osuna, J. & Ortiz-Leyba, C. Effect of critical illness polyneuropathy on the withdrawal from mechanical ventilation and the length of stay in septic patients. Crit. Care Med. 33, 349–354. https://doi.org/10.1097/01.ccm.0000153521.41848.7e (2005).
Jeong, B. H. et al. Impact of limb weakness on extubation failure after planned extubation in medical patients. Respirology https://doi.org/10.1111/resp.13305 (2018).
Myles, P. et al. Differences between asthmatics and nonasthmatics hospitalised with influenza A infection. Eur. Respir. J. 41, 824–831. https://doi.org/10.1183/09031936.00015512 (2013).
Morales-Suarez-Varela, M. et al. Asthma in older people hospitalized with influenza in Spain: A case-control study. Allergy Asthma Proc. 38, 277–285. https://doi.org/10.2500/aap.2017.38.4060 (2017).
Louie, J. K. et al. A novel risk factor for a novel virus: Obesity and 2009 pandemic influenza A (H1N1). Clin. Infect. Dis. 52, 301–312. https://doi.org/10.1093/cid/ciq152 (2011).
Shen, Y., Cai, G. & Zhu, S. Inconsistent evidence of corticosteroid use in different respiratory disorders. Clin. Infect. Dis. https://doi.org/10.1093/cid/ciaa1439 (2020).
Johnson, A. E. et al. MIMIC-III, a freely accessible critical care database. Sci. Data 3, 160035. https://doi.org/10.1038/sdata.2016.35 (2016).
D’Agostino, R. B. Jr. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat. Med. 17, 2265–2281. https://doi.org/10.1002/(sici)1097-0258(19981015)17:19%3c2265::aid-sim918%3e3.0.co;2-b (1998).
Normand, S. T. et al. Validating recommendations for coronary angiography following acute myocardial infarction in the elderly: A matched analysis using propensity scores. J. Clin. Epidemiol. 54, 387–398. https://doi.org/10.1016/s0895-4356(00)00321-8 (2001).
Funding
Yanfei Shen received funding from the Zhejiang Medical and Health Science and Technology project (NO. 2021KY001).
Author information
Authors and Affiliations
Contributions
Y.S. and W.R. designed the project. X.H. and G.C. analysed the data and prepared the figures. S.C., Z.Y., and J.Y. drafted the manuscript. All the authors have revised the manuscript critically, approved the version submitted for publication, and have agreed to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shen, Y., Ru, W., Huang, X. et al. Impact of chronic respiratory diseases on re-intubation rate in critically ill patients: a cohort study. Sci Rep 11, 8663 (2021). https://doi.org/10.1038/s41598-021-88007-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-88007-y
- Springer Nature Limited