Abstract
Prostaglandin E2 (PGE2) is a major contributor to inflammatory pain hyperalgesia, however, the extent to which it modulates the activity of nociceptive axons is incompletely understood. We developed and characterized a microfluidic cell culture model to investigate sensitisation of the axons of dorsal root ganglia neurons. We show that application of PGE2 to fluidically isolated axons leads to sensitisation of their responses to depolarising stimuli. Interestingly the application of PGE2 to the DRG axons elicited a direct and persistent spiking activity propagated to the soma. Both the persistent activity and the membrane depolarisation in the axons are abolished by the EP4 receptor inhibitor and a blocker of cAMP synthesis. Further investigated into the mechanisms of the spiking activity showed that the PGE2 evoked depolarisation was inhibited by Nav1.8 sodium channel blockers but was refractory to the application of TTX or zatebradine. Interestingly, the depolarisation of axons was blocked by blocking ANO1 channels with T16Ainh-A01. We further show that PGE2-elicited axonal responses are altered by the changes in chloride gradient within the axons following treatment with bumetanide a Na-K-2Cl cotransporter NKCC1 inhibitor, but not by VU01240551 an inhibitor of potassium-chloride transporter KCC2. Our data demonstrate a novel role for PGE2/EP4/cAMP pathway which culminates in a sustained depolarisation of sensory axons mediated by a chloride current through ANO1 channels. Therefore, using a microfluidic culture model, we provide evidence for a potential dual function of PGE2 in inflammatory pain: it sensitises depolarisation-evoked responses in nociceptive axons and directly triggers action potentials by activating ANO1 and Nav1.8 channels.
Similar content being viewed by others
Introduction
Despite the recent advances, but primarily due to the complexity of the pain pathways, clinical management of pain remains an area of significant unmet need1. PGE2 is involved in the regulation of a number of processes in the nervous system and plays a central role in both inflammatory and neuropathic pain (see2 and3 for review). It belongs to a class of abundantly expressed eicosanoids, produced by enzymatic catalysis of arachidonic acid. Cyclooxygenases COX-1 and COX-2 produce the prostaglandin precursors PGG2 and PGH2 which are in turn converted by prostaglandin synthases into the active prostaglandins E2 (PGE2), D2 and F2A, prostacyclin (PGI2) and thromboxane (see4 for review). The COX inhibitors, which belong to a class of non-steroidal anti-inflammatory drugs (NSAIDS), are extensively used as analgesic compounds. However, the adverse effects, such as peptic ulcers and increased cardiovascular risks, associated with these inhibitors have made the development of new anti-inflammatory analgesics an area of urgent need5.
PGE2 has been shown to bind to EP receptor subtypes (EP1-4), which are G-protein coupled receptors expressed in many tissues including the sensory neurons6. The high affinity receptor for PGE2, EP4, forms a Gs complex, and activates adenylate cyclase which in turn increases cyclin AMP (cAMP) production7,8. The PGE2/EP4 pathway has been shown to play an important role in osteoarthritis and rheumatoid arthritis (e.g. Ref9). In other animal models with CFA and carrageenan treatment, pharmacological antagonism of EP4, the high-affinity binding receptor for PGE2, was efficacious in attenuating the associated inflammatory hyperalgesia10,11.
The pronociceptive effects of PGE2 and its role in peripheral sensitisation have been established in animal models and are supported by studies that show the sensitisation of the nociceptive nerve endings in the skin and membrane targets by PGE2/EP4 pathway (see2 and3 for review). Although sensitisation of sensory stimuli by PGE2 is well established, whether PGE2 can directly excite the nociceptive fibers remains incompletely understood. For instance, initial studies had suggested the excitation of nociceptors by prostaglandins12, whereas others have reported that PGE2 fails to evoke spike discharge in visceral afferents and skin-saphenous nerve preparations (e.g.13,14). Studies using conventional cell cultures have also been inconclusive. Some reports have shown that PGE2 evoked Ca2+ influx in dissociated rat DRG neurons (e.g.15), whereas others have reported that exogenous application of the same concentration of PGE2 did not elicit an increase in intracellular Ca2+ levels in DRG cell bodies (e.g.16).
We have previously reported the development of a microfluidic culture platform17 to investigate the function of sensory axons in isolation from the soma, as a cell culture model of nociceptive endings. We further have shown that the DRG neurites in microfluidic cultures recapitulate key features of mature axons and hence are ideal for studying the functional changes in nociceptive axons in response to mediators such as NGF 17,18. In the present study we investigate the modulation of axonal excitation in response to PGE2 utilizing the microfluidic culture platform. We demonstrate that local treatment of axons with PGE2 in microfluidic cultures leads to sensitisation of the responses to depolarising stimuli, but also induces a persistent activity in many nociceptive axons by causing a direct depolarisation of the axons in the absence any other stimuli. We provide evidence for the ionic mechanism of PGE2-evoked excitation of nociceptive axons and show that the sodium channel Nav1.8 and the calcium-activated chloride channel Anoctamin 1 (ANO1) are indispensable for the depolarization and the concomitant persistent activity in sensory axons.
Results
PGE2 sensitises axonal responses to KCl in the microfluidic cultures
To investigate PGE2 modulation of axonal function, we employed a microfluidic culture platform. We had previously shown the versatility of this culture platform for examining axonal responses to various stimuli17. As demonstrated by Tsantoulas et al.17, chemical or electrical stimulation of fluidically isolated DRG axons results in a local depolarisation and generation of action potentials that propagate to the cell soma. This triggers the opening of voltage-dependent calcium channels, resulting in an increase in intracellular Ca2+ at the soma17,18.
We examined the modulation of axonal responses to 20 mM KCl by PGE2 using the microfluidic platform (Fig. 1A) where the somal compartment is fluidically isolated from the axonal compartment17. The magnitude of the responses in the fluidically isolated DRG axons were evaluated by measuring the changes in intracellular Ca2+ at the soma as a readout for axonal function17. Only DiI positive cell bodies, indicative of axonal crossings (see “Materials and methods”), were selected for further analysis (Fig. S1). Administration of KCl to axons led to a robust increase in Ca2+ concentration measured at the soma (Figs. 1B and S2).
PGE2-mediated sensitisation of response to KCl stimulation of axonal compartment in microfluidic cultures. (A) Schematic of the experimental setup using microfluidic cultures. Somal side is separated from the axonal side by 150 µm microgrooves. Each drug application was followed by a washout (not shown). (B) Representative Fura-2 traces recorded from the somal compartment while stimulating the axonal compartment with 20 mM KCl and a 2-min treatment with PGE2. (C) Summary of the changes in peak responses to KCl stimulation after treatment with imaging buffer (control) or PGE2 and the effect of zatebradine. The potentiation of KCl-evoked axonal responses was abolished by inclusion of 10 mM zatebradine (****p < 0.0001,Oneway ANOVA followed by Tukey’s t-test, ns p = 0.2061, n = 21–45 from 5 cultures).
PGE2 treatment of the axons led to a potentiation of the responses to KCl administered to the axons (Fig. 1B and C). This potentiation was also observed using a cocktail of inflammatory mediators (Fig. S3).
The magnitude of Ca2+ responses displayed a 2.7-fold increase, from 0.88 ± 0.03 to 2.38 ± 0.12, to KCl stimulation following application of PGE2 (Fig. 1C). HCN channels have been shown to play a crucial role in PGE2 mediated pain sensitisation in mice19,20. We investigated the effect of zatebradine, a blocker that is selective for HCN channels but does not discriminate amongst the isoforms HCN1-4, on the PGE2 mediated enhancement of axonal responses. We found that pretreatment of axons with zatebradine completely abolished the PGE2 mediated enhancement of KCl responses (Fig. 1D). Our results demonstrate that PGE2 sensitises axonal responses to depolarising stimuli, and further, consistent with in vivo data, this enhancement is dependent on HCN channels.
PGE2 evokes persistent firing activity in sensory axons
We had observed that the application of PGE2 after KCl stimulation of fluidically isolated sensory axons induced short, repetitive bursts of intracellular Ca2+ detected at the soma (Fig. 1B). We sought to determine whether PGE2 on its own could evoke firing activity in these sensory axons. We employed a three-compartment microfluidic device configuration where sensory axons from the neurons plated in the somal compartment, traversed the middle and distal compartments (Fig. 2A). A 2-min application of PGE2 to the distal compartment produced a persistent axonal activity in the form of calcium transients detected at the soma compartment that were observed for at least 30 min following application of PGE2 (Fig. 2B). We found that the ongoing activity continued following washout of PGE2. This persistent activity in the form of calcium transients was quantified as the total number of transients observed over 3 min following PGE2 application (Fig. 2E). PGE2 application to the distal axonal compartment produced transients at a rate of 6.12 ± 0.63/3 min after application, compared to no transients observed in the absence of PGE2.
PGE2 evokes a persistent axonal activity which is abolished by lidocaine. (A) Schematic of experimental set up used for data shown in panel (B), three-compartment MFC is depicted with the somal compartment (blue), middle (white) and distal axonal compartments (green). (B) Representative trace showing the Ca2+ transients recorded at the soma. Perfusion of 10 μM PGE2 for 2 min resulted in axonal activity detected at the soma, which persisted after washout of PGE2. (C) Schematic of the experimental set up used for data shown in (D) and (E), using the three-compartment microfluidic configuration. KCl was applied to the distal axon compartment as control, followed by PGE2. 5 mM lidocaine was then applied to the middle axonal compartment. (D) Representative Fratio trace showing the calcium transients evoked by the application of PGE2 and blocked by the perfusion of 5 mM lidocaine in the middle axonal compartment. (E) Summary of the number of transients observed during a 3 min window following stimulus application. An increase in the number of transients after application of PGE2 compared to baseline and a significant reduction in the number of transients after application of lidocaine was observed. (Kruskal–Wallis test with Dunn’s multiple comparisons test, ****p < 0.0001, n = 9 from 4 cultures).
To localize the site of activation of the persistent activity, we examined the effect of the application of the anesthetic lidocaine, a non-selective sodium and calcium channel blocker, to the central compartment (Fig. 2C). Pretreatment of the middle compartment with lidocaine (5 mM) completely blocked the PGE2 evoked persistent responses detected at the soma (Fig. 2D and E). This experiment demonstrates that the persistent responses elicited by PGE2 originate in the distal axons.
We next examined whether cAMP-dependent signaling downstream of PGE2 receptor activation is required for the persistent activity observed in the axons. A 3-min application of Rp-cAMPS, a membrane permeant inhibitor of cAMP-dependent protein kinases, reversibly and completely blocked the PGE2-evoked persistent activity in the axons (Fig. 3A–C). Taken together, these data establish that the inflammatory mediator PGE2 evokes a local persistent activity in the DRG axons, and that this persistent activity requires the generation of cAMP and activation of PKA.
The PGE2-evoked persistent axonal firing is dependent on the cAMP/PKA signaling pathway. (A) Schematic of the experimental protocol. Stimulation of the axonal side (green) with PGE2 was followed by a wash and application of Rp-cAMPS. Ca imaging was performed from the somal compartment. (B) Scatter plot quantifying the frequency of the Ca2+ transients observed. Rp-cAMP blocked PGE2-induced transients. The activity partially recovered following washout of Rp-cAMPS. (C) Representative trace showing repetitive firing activity recorded at the soma in response to 1-min axonal stimulation with PGE2. The activity is blocked with the application of 20 µM Rp-cAMPS for 3 min. (One-way ANOVA with Tukey’s multiple comparisons test, *p < 0.05, ****p < 0.0001 n = 11 from 3 cultures).
PGE2-evoked persistent activity in sensory axons requires Nav1.8 but not TTX-S channels
Given the observed silencing of PGE2-evoked axonal activity by the application of lidocaine to the middle chamber, which suggested a likely block of the propagation of the generated action potentials to the soma, we next considered the role of voltage-gated sodium channels in the generation of the persistent activity evoked by PGE2 in the axons. We found that application of 500 nM TTX did not attenuate the PGE2 evoked persistent activity in the axons (Fig. 4A–C), suggesting that TTX-sensitive (TTX-S) sodium channels are not involved in the generation or propagation of this persistent activity. Nav1.8 channels on the other hand have been shown to be modulated by PGE221. We next considered the role of Nav1.8 channel in the PGE2-induced persistent activity. Using the three-compartment microfluidic configuration (Fig. 5A), we found that application of Nav1.8 blocker PF-01247324 (2uM) significantly attenuated the PGE2-evoked activity in the sensory axons (Fig. 4D–F).
The PGE2-evoked persistent activity in the axons is dependent on Nav1.8 but not TTX-sensitive sodium channels. (A) Schematic of the experimental protocol for data shown in (B) and (C). Stimulation of the axonal side with PGE2 was followed by a washout and application of 500 nM TTX while recording from the somal compartment. (B) Representative trace showing repetitive firing activity recorded from the soma in response to a 1-min application of PGE2 to the axonal compartment, which is maintained in the presence of 500 nM TTX. (C) Summary of the TTX effect on the number of transients observed after application of each stimulus. No significant change in the number of PGE2-induced transients after application of 500 nM TTX was observed. (p = 0.1261, One-way ANOVA with Tukey’s multiple comparisons test, n = 15 from 3 cultures). (D) Schematic of the experimental set up for data shown in (E) and (F). Stimulation of the axonal side with PGE2 was followed by a washout and application of PF-01247324 while recording from the somal compartment. (E) Representative trace showing repetitive persistent activity recorded from the soma in response to axonal stimulation with PGE2. Application of 2 µM PF-01247324 largely attenuated the response. (F) Summary of the data showing the effect of PF-05089771 on number of PGE2-evoked transients. A threefold decrease in the number of PGE2-induced transients after application of PF-01247324 was observed (**p < 0.01, Wilcoxon matched-pairs signed rank test, n = 10 devices from 3 cultures).
Application of PGE2 to the axons depolarises the membrane potential. (A) Schematic of experimental set up for data shown in (B–G) A two-compartment microfluidic configuration was used, where PGE2 or KCl were applied in the axonal side. FluoVolt fluorescence intensity was measured in the axonal compartment as a measure of membrane potential (Vm). (B) Bright field image showing a representative field of view (FoV) from the axonal compartment of a microfluidic culture. (C) Background subtracted image (ΔF/F) of the FoV shown in (B), prior to PGE2 or KCl application. No change in brightness intensity occurs prior to PGE2 application. (D) Background subtracted image (ΔF/F) of the FoV shown in (B), after PGE2 application. Changes in FluoVolt brightness intensity upon PGE2 stimulation are highlight with arrows. (E and F) Representative traces of FluoVolt brightness intensity from the axonal compartment showing increased intensity with 30 mM of KCl (E) or 10 μM PGE2 (F). The KCl trace returns to baseline after washout whereas the PGE2 trace remains elevated. (G) Summary of the data describing peak KCl and PGE2 evoked changes in FluoVolt fluorescence. Application of 10 μM PGE2 to the axonal compartment elicited a 5.89% ± 0.09% increase in fluorescent intensity comparable to the 5.18% ± 0.11% increase evoked by 30 mM KCl. (Student’s t-test, p < 0.354, nROIs = 925 on 20 devices from 18 cultures for PGE2 and nROIs = 135 on 4 devices from 3 cultures for KCl).
PGE2 application directly depolarises axonal membrane in the absence of other stimuli
We hypothesized that the observed persistent activity, initiated locally at axonal endings and propagating to the soma is due to the depolarisation of the axonal membrane in response to PGE2. Using the voltage-sensitive dye Fluovolt22,23, we measured the changes in axonal membrane potential in the axonal compartment (Fig. 5A–D). Application of KCl (30 mM) for 90 s produced a change in fluorescent intensity of 5.18% ± 0.11% which returned to baseline immediately after wash with buffer (Fig. 5D). Similarly, an application of PGE2 (10 μM) produced a robust 5.89% ± 0.09% increase in the FluoVolt fluorescence intensity (Fig. 5E–G). However, the PGE2 evoked depolarisation exhibited slow activation kinetics and a sustained plateau following the wash (Fig. 5E), supporting the activation of a second messenger pathway that may be inducing this persistent depolarisation. Altogether these data demonstrate a direct and local depolarization of the axonal membrane in response to PGE2.
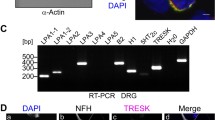
PGE2-induced depolarisation is mediated by EP4 receptors
To further explore the mechanism of PGE2 evoked activation of sensory axons, we examined the role of the high-affinity prostaglandin receptor, EP4, in initiating the depolarisation of the axonal membrane. We found that EP4 receptors are colocalized with Nav1.8 channels on DRG axons in microfluidic cultures (Fig. 6A–E). We observed a co-expression pattern of EP4 and the Nav1.8 channel along the adult DRG axons and EP4 staining was evident in a subset of Nav1.8 positive neurons (Fig. 6E). Next, we performed voltage imaging experiments on axons following a 20-min incubation with the EP4 inhibitor L-161,982 (10 nM). As shown in Fig. 6F, the EP4 receptor inhibitor completely abolished PGE2-evoked axonal membrane depolarisations. The total axonal area activated by PGE2-stimulation in the presence of the EP4 inhibitor was 5.92 ± 1.92% of the total axonal area, as compared to 47.94% ± 4.39% of total axonal area that was activated by PGE2 alone. We also found a significant attenuation of the change in the amplitude of FluoVolt fluorescence, to 3.49 ± 0.085% by PGE2 in the responding axonal areas (Fig. 6G and H). Therefore, this data supports the sole dependence of PGE2 on the high-affinity EP4 receptor for the generation of the persistent activity observed in the DRG axons.
EP4 receptors colocalize with Nav1.8 channels in the axons and inhibition of EP4 receptors abolishes PGE2-evoked axonal depolarisation. Representative images of adult DRG axons taken at day 5 in culture. (A and B) Expression of EP4 in DRG axons in the MFC axonal compartment B) Nav1.8 staining in same FoV as A. (C and D) Control for the secondary antibodies. (E) An expanded view of an overlay image of EP4 (red) and Nav1.8 (green) staining from A and B. Arrows mark representative areas of co-localisation of EP4 receptors and Nav1.8 channels. Scale bars, 100 μm. (F) Representative FluoVolt intensity trace from an axonal area following a 1-min stimulation with 10 µM PGE2 in the presence of 10 nM L-161,982. PGE2 failed to evoked a change in membrane potential in the presence of the EP4 inhibitor. (G) Summary of the changes in total PGE2 activated axonal area in the presence of L-161,982. L-161,982 significantly reduced mean total PGE2 activated axonal area (****p < 0.0001, Brown-Forsythe and Welch ANOVA tests, n = 10 devices from10 for PGE2 and n = 7 devices from 4 cultures for PGE2 + L-161,982). (H) Summary data describing the changes in the peak brightness intensity in the activated areas for PGE2-treated and PGE2 + L-161,982 treated axons. Application of PGE2 in the presence of the selective EP4 inhibitor significantly attenuated the mean amplitudes (****p < 0.0001, Student’s t-test, nROIs = 925on 20 devices from18 cultures for PGE2 and nROIs = 141 on 7 devices from 4 cultures for PGE2 + L-161,982).
PGE2-evoked depolarisation of sensory axons is attenuated by Nav1.8 and Nav1.7 channel blockers
We next examined the contribution of Nav1.8 and Nav1.7 sodium channels to the PGE2-mediated depolarisation of the axons. We stimulated sensory axons with PGE2 for 90 s in the presence or absence of a selective Nav1.7 channel blocker P-05089771 at 8 nM and monitored the changes in axonal membrane potential using FluoVolt (Fig. 7A–D). We assessed the effect of the Nav1.7 blocker on membrane potential in two ways. We quantified the proportion of axonal area where the FluoVolt signal was increased by PGE2 stimulation (see “Materials and methods”) either alone or in the presence of Nav1.7 blockers. We observed no significant change in the proportion of axonal membrane that exhibited a change in membrane potential, in response to PGE2 in the presence or absence of the Nav1.7 blocker (Fig. 7C). There was, however, a slight decrease in the average axonal depolarisation in the presence of the Nav1.7 blocker (Fig. 5D) suggesting a potential contribution from Nav1.7 channels to the observed PGE2 evoked depolarisation.
PGE2-evoked depolarisation of axons is predominantly mediated by Nav1.8 sodium channels. (A and B) Representative traces of FluoVolt brightness intensity in the axons showing the increase following stimulation with 10 µM PGE2 (D) and 10uM of PGE2 followed by application of 8 nM the Nav1.7 blocker PF-05089771. (C) Summary of the data in A and B. Application of PGE2 + Nav1.7 blocker decreased the average peak brightness intensity by 5.47 ± 0.03% (****p < 0.0001, Student’s t-test, nROIs = 925 on 20 devices from18 cultures for PGE2, and nROIs = 1202 on6 devices from 4 cultures for PGE2 + PF-05089771). (D) PGE2 application elicits activation of 47.94 ± 4.39% of the total axonal area, and addition of PF-05089771 with PGE2 did not significantly change the total activated area (44.03 ± 5.53%, p < 0.5975 Student’s t-test, n = 10 devices from 10 cultures for PGE2, and n = 6 devices from 4 cultures for PGE2 + PF-05089771). (E–G) Representative traces of FluoVolt intensity showing changes following treatment of the axonal compartment with PGE2, PGE2 with 2 uM PF-01247324, and PGE2 in the presence of 10 nM A-803467. Nav1.8 blockers attenuate the amplitude of the membrane depolarisation evoked by PGE2. (H) Summary of the changes in the brightness intensity evoked by PGE2. Application of PGE2 in the presence of the Nav1.8 blockers significantly reduces the average amplitudes of responses to nearly half (4.40 ± 0.035% for PF-01257324 and 3.46 ± 0.31% SEM for A-803467, ****p < 0.0001, Brown-Forsythe and Welch ANOVA tests, nROIs = 518on 3 devices from 3 cultures for PGE2 + PF-01247324, and nROIs = 53 on 5 devices from 5 cultures for PGE2 + A-803467). I) Summary of the changes in total PGE2-evoked activated axonal area in the presence of Nav1.8 blockers. PGE2 application depolarises 47.94 ± 4.39% of the total axonal area while Nav1.8 blockers significantly reduce the activated area to 7.53 ± 4.25% for PF-01257324 and 7.60 ± 0.73% for A-803467, ***p < 0.0006 and ****p < 0.0001 respectively, Brown-Forsythe and Welch ANOVA tests, n = 3 devices from 3 cultures for PGE2 + PF-01247324 and n = 5 devices from 5 cultures for PGE2 + A-803467 blocker.
Using the two-compartment microfluidic configuration we then examined the effects of two Nav1.8-selective channel blockers, PF-01247324 and A-803467 (Fig. 7E–I). While PGE2 evoked a 5.89 ± 0.09% increase in the average FluoVolt fluorescence intensity in the axons, co-application of either PF-01247324 or A-803467 led to a statistically significant reduction in the observed fluorescence to 4.40 ± 0.035% and 3.46 ± 0.31%, respectively (Fig. 7H and I). Interestingly, in the presence of the Nav1.8 blockers there was a stark reduction in the axonal area activated by PGE2 stimulation. We observed an almost complete abolishment (85% reduction) of PGE2-evoked axonal depolarisation by the Nav1.8 blockers (Fig. 7I). Overall, these data suggest an important contribution of Nav1.8 channels to PGE2-evoked depolarisation of sensory axons.
Given the involvement of HCN channels in PGE2-mediated sensitisation of sensory axons, we next considered if zatebradine, a non-selective HCN channel blocker, can also affect the PGE2-evoked axonal depolarisation. Zatebradine, at 10 μM and 50 μM, however, did not reduce the amplitude of PGE2-evoked depolarisation of axons (Fig. S5E–G), nor produced a change in the total activated axonal area (Fig. S5H), suggesting that HCN channel activation is not a requirement for the PGE2-evoked depolarisation of axons.
PGE2-evoked axonal depolarisation is mediated by ANO1 channels
Given the established role of Nav1.8 channels in the upstroke of action potentials in TTX-resistant (TTX-R) DRG neurons24 we hypothesized that a localized activation of another channel or channel complex leads the depolarisation of axonal membrane and the subsequent activation of Nav1.8 channels. We therefore further investigated other candidate ion channels that might initiate the PGE2-evoked depolarisation of the axons. We examined ANO1, a calcium activated chloride channel expressed in Nav1.8 expressing DRG neurons and known to be involved in inflammatory pain25. We found that application of the selective ANO1 blocker T16inh-A01 at concentrations of 20 μM and 100 μM significantly inhibited the PGE2-evoked axonal depolarisation by 4.7 ± 0.12% and 53 ± 0.73% respectively (Fig. 8A–C). ANO1 blockade did not reduce the total area of PGE2-activated axons (Fig. 8D). This data indicates that ANO1 is activated in response to PGE2 application and initiates the depolarisation of the axonal membrane. To further confirm that PGE2-evoked axonal depolarisation is dependent on the Cl− gradient, we used bumetanide, a selective inhibitor of the chloride transporter NKCC1. NKCC1 has been shown to be highly expressed in mature DRG neurons and functions to increase the intracellular Cl− concentration which could make chloride channel activation excitatory in these neurons26,27. We found that bumetanide, in a similar fashion to T16inh-A01, significantly attenuated the amplitude of PGE2-evoked responses (Fig. 8G) and did not alter the total activated axonal area. Furthermore, treatment with bumetanide eliminated the PGE2-induced enhancement of KCl-evoked responses at the axons (Fig. S6), indicating the involvement of chloride gradients in PGE2 sensitisation.
PGE2-induced axonal depolarisation amplitude is attenuated by ANO1 but not HCN channel blockade. (A,B) Representative trace indicating changes in fluorescence expressed as Fluovolt Fluorescence (ΔF/F), of an axonal region of interest in response to application of PGE2 in the presence of a selective ANO1 blocker (T16inh-A01) at 20 µM and 100 µM respectively. (C) Summary of the changes in the brightness intensity evoked by PGE2. Application of PGE2 in the presence of the ANO1 blocker significantly attenuates the average amplitudes of responses (from 5.92 ± 0.098% for PGE2 (10 µM) to 5.64 ± 0.11% for PGE2 + T16inh-A01 (20 µM) and 2.78 ± 0.17% SEM for PGE2 + T16inh-A01 (100 µM), ****p < 0.0001 and ****p < 0.0001 respectively, Brown-Forsythe and Welch ANOVA tests, nROIs = 943 on 23 devices from 21 cultures for PGE2, nROIs = 317 on 4 devices from 4 cultures for PGE2 + T16inh-A01 (20 µM) and nROIs = 68 on 3 devices from 3 cultures for PGE2 + T16inh-A01 (100 µM). (D) Summary of the changes in total PGE2-evoked activated axonal area in the presence of ANO1 blockade. The ANO1 blockade at both 20 µM and 100 µM did not produce significant reduction of total axonal area activated. Brown-Forsythe and Welch ANOVA tests, 13 devices from 13 cultures for PGE2 (10 µM) 4 devices from 4 cultures for PGE2 + T16inh-A01 (20 µM) and 3 devices from 3 cultures for PGE2 + T16inh-A01 (100 µM). (E,F) Representative trace indicating changes in fluorescence expressed as Fluovolt Fluorescence (ΔF/F), of an axonal region of interest in response to application of PGE2 (10 µM) and of PGE2 in concomitance with the NKCC1 inhibitor bumetanide (10 µM). (G) Summary of the changes in the brightness intensity evoked by PGE2. Application of PGE2 in the presence of the NKCC1 blocker ameliorates the average amplitudes of responses (from 14.81 ± 1.069% for PGE2 (10 µM) to 7.90 ± 0.40% for PGE2 + Bumetanide (10 µM). In the presence of KCC2 inhibitor VU0240551 (2 µM), we observed no significant change (17.83 ± 1.63% ****p < 0.0001 and p > 0.223 respectively, Brown-Forsythe and Welch ANOVA tests, nROIs = 62 on 3 devices from 4 cultures for PGE2, nROIs = 151 on 5 devices from 4 cultures for PGE2 + Bumetanide (10 µM) and nROIs = 68 on 4 devices from 4 cultures for PGE2 + VU0240551 (2 µM). (H) Summary of the changes in total PGE2-evoked activated axonal area in the presence of chloride transporter inhibition. Both the NKCC1 and KCC2 inhibitors failed to appreciably alter the activation of axonal areas in comparison to PGE2. Brown-Forsythe and Welch ANOVA tests (3 devices from 4 cultures for PGE2, 5 devices from 4 cultures for PGE2 + Bumetanide (10 µM) and 4 devices from 4 cultures for PGE2 + VU0240551 (2 µM).
We also employed VU01240551, a chloride transporter inhibitor of KCC2 which functions to decrease Cl− concentration in the neurons leading to hyperpolarizing responses in the neurons26,28. KCC2 and NKCC1 maintain the Cl-homeostasis in the central neurons, however, the expression of KCC2 in mature DRG is very low26,28. KCC2 inhibitor did not potentiate the PGE2-evoked axonal amplitude or the area of axonal depolarisation (Fig. 8E–H), concordant with its minimal expression in mature DRG neurons. Taken together, these data indicate that the localized depolarisation of DRG axons evoked by PGE2 is dependent on the axonal Cl− concentration gradient and is due to the opening of ANO1 channels.
Discussion
Taking advantage of microfluidic cultures, we present a model of peripheral sensitisation to investigate the modulation of nociceptive axons downstream of PGE2/EP4 pathway. We and others have characterized the utility of the microfluidic culture platform for studying axonal physiology17,18,29,30,31,32. While most in vitro studies using conventional cell cultures have focused on events occurring at the cell bodies of DRG neurons, it is the nerve endings at the site of inflammation that are the first targets of inflammatory mediators. The fluidic isolation of axons in microfluidic cultures provides a more precise anatomical recapitulation of the peripheral neurons, and in addition the axons represent a closer physiological model of the nerve endings than the cell soma17.
Using the microfluidic culture platform, we demonstrate that acute treatment of fluidically isolated DRG axons with PGE2 leads to a robust enhancement of the local responses to depolarisation by KCl. Prostaglandins have been shown to target many channels in the membrane leading to enhancement of their responses. Previous studies for instance have shown the PGE2 mediated sensitisation of ion channels such as TRPV1 in DRG cell bodies in culture33. Nevertheless, stimulation by heat, mechanical or chemical stimuli ultimately leads to membrane depolarisation and firing of action potentials in nerve endings, hence sensitisation of the axonal responses to depolarization described here could represent a common feature of inflammatory modulation independent of the processes that mediated enhancement of the local transducer channels such as TRPV1. We found that pharmacological blockade of HCN channels abolished the sensitisation of KCl-evoked responses in the axons. HCN channels play an important role in regulating the firing frequency of DRG neurons and have been shown to be involved in neuropathic and inflammatory pain states19,34,35. We found that blocking HCN channels with zatebradine led to a complete inhibition of PGE2-mediated sensitisation of axonal responses to depolarisation in our microfluidic model. This is consistent with the lack of PGE2-induced thermal hyperalgesia observed in mice with the HCN2 gene deleted from Nav1.8 expressing DRG neurons36. Taken together, the microfluidic culture model presented here closely reproduces the features of in vivo sensitisation and extends our understanding of the axonal mechanism of pain sensitisation.
Intriguingly, we observed that PGE2 directly activated a subset of sensory axons leading to generation of persistent Ca signals recorded at the soma. We found that local activation of PGE2/EP4/cAMP pathway in the adult mouse DRG axons consistently induces a membrane depolarisation that results in the generation of action potentials propagating to the cell soma. Whilst the excitatory effects of bradykinin have been extensively characterized37,38,39, whether PGE2 can induce excitation of nociceptive nerve terminals remains unclear. Previous studies have been inconclusive with some reporting that PGE2 failed to evoke spike discharge in primary visceral afferents and skin-saphenous nerve preparations13,14,40,41, but that PGE2 can induce spike discharge in joint afferents42. Species differences may account for some of the inconsistency in the in vivo observations, but technical limitations inherent to in vivo recordings17 including conduction failure can confound the results from the in vivo studies. Studies on the excitatory action of PGE2 on sensory neurons in culture have primarily focused on the cell soma. For instance, application of PGE2 has been reported to evoke Ca2+ influx in dissociated rat DRG neurons15, whereas, others have reported that exogenous application of the same concentration of PGE2 did not elicit any increase in the intracellular Ca2+ levels in DRG cell bodies (e.g.16). We show however that PGE2-evoked axonal responses are downstream of EP4/cAMP activation in DRG axons. Several studies have examined the spatiotemporal dynamics of cAMP in the peripheral structures and have found a concentration gradient with the highest concentration of cAMP generated in the axons and the lowest in the soma during signaling43,44,45,46. The differences in cAMP concentration reached in axons can potentially explain the previous inconsistencies in the responses of neurons to PGE2 in culture. Here using the microfluidic cultures, we demonstrate an unambiguous, localized, and sustained activation of sensory axons in response to PGE2.
We hypothesized that the PGE2-evoked activity seen in the axons was the result of a depolarisation of the axonal membrane. Using voltage imaging in the axonal compartment, we show that activation of EP4 receptor by PGE2, and the subsequent accumulation of cAMP lead to a localized depolarization in DRG axons. We focused on voltage-gated sodium channels, which possess a central role in pain sensation. PGE2 and cAMP have been shown to potentiate the TTX-R but not TTX-S currents in DRG neurons47,48,49. We found that TTX-sensitive sodium channels do not contribute to the PGE2-evoked axonal activation, and a specific Nav1.7 blocker had only a marginal effect on the ensuing depolarisation, which are in keeping with the in vivo findings that deletion or block of Nav1.7 channels do not abolish peripheral sensitisation induced by PGE236,50. Blockers of Nav1.8 channel on the other hand significantly attenuated the PGE2-evoked axonal depolarisation. It has been reported that acute administration of PGE2 can potentiate Nav1.8 current amplitudes as well as causing a hyperpolarizing shift in the current–voltage relationship49. We show co-localization of Nav1.8 and EP4 receptors on nociceptive axons, supporting the role of Nav1.8 in PGE2-evoked depolarisation of these axons. However, it remains unclear how the changes in the magnitude of depolarisation evoked currents or the small shifts observed in the current–voltage relationship could give rise to the large depolarization observed in the DRG axons. It is possible that other channels are involved, mediating subthreshold depolarization which is then amplified by Nav1.8 activation in the axons. For instance, potentiation of the heat sensor TRPV1 by PGE2 has been suggested to cause its activation by body temperature leading spontaneous or ongoing heat pain3.
We sought to further delineate the molecular mechanisms of PGE2-evoked depolarisation. cAMP mediated depolarization of the membrane has been shown to occur through several mechanisms, including the closing of potassium channels, or opening of calcium activated chloride channels51. ANO1 expressed on small diameter sensory neurons is activated by calcium and heat to induce depolarisation of the DRG nociceptive neurons25. We show here that the pharmacological blockade of ANO1 inhibits the observed PGE2-evoked depolarisation of the DRG axons. To our knowledge this the first time a link between ANO1 activation and PGE2/EP4 pathway has been demonstrated. Depolarisation of axons by PGE2 through the activation of ANO1 and subsequently Nav1.8 has important implications for advancing our understanding of the mechanisms underlying inflammatory spontaneous pain.
Intracellular Cl− concentration is an important determinant of whether activation of Cl− channels would lead to the depolarisation or hyperpolarization of the cell membrane52. Unlike central neurons, there is a consistently high intracellular Cl− concentration in mature sensory neurons maintained by the expression of sodium potassium chloride co-transporter NKCC153. We confirmed the dependence of PGE2-evoked depolarisation on intracellular Cl− concentration through the application of bumetanide, an inhibitor of the NKCC1, which significantly reduced the amplitude of the PGE2-evoked depolarisation of sensory axons. Application of bumetanide has been shown to alleviate thermal and mechanical hyperalgesia associated with sciatic nerve injury54. In contrast NKCC1, KCC2 works to extrude intracellular Cl− reducing it concentration, however, the expression of KCC2 in mature DRG neurons has been subject to controversy26,28. Inhibition of KCC2 would be predicted to increase intracellular Cl− concentration and potentiate the excitatory effects of opening Cl− channels. However, we found that inhibition of KCC2 had no effect on depolarisation of sensory axons by PGE2, which is consistent with previous results of the lack of KCC2 mRNA expression in mature DRG neurons55. Taken together, these data demonstrate the requirement of a high intracellular Cl− concentration maintained by NKCC1 for PGE2-evoked responses in sensory axons.
In the present study we show a potential dual role of PGE2/EP4 pathway, serving as both an initiator and a sensitiser of pain signals in DRG sensory neurons. The ANO1-mediated activation of nociceptive axons and the concomitant HCN-dependent enhancement of axonal responses to depolarising stimuli by PGE2 potentially provide a general explanation for both acute and chronic manifestations of ongoing pain following tissue injury.
Materials and methods
All methods were performed in accordance with the relevant guidelines and regulations.
Animals
Adult male C57BL/6 mice were purchased from Charles-River UK. All animals were maintained in a designated facility according to the UK Home Office Code of Practice for the Housing and Care of Animals Used in Scientific Procedures. Mice were sacrificed through CO2-anaesthetization followed by cervical dislocation in full compliance with UK Home Office Regulations and procedures under Schedule 1 of Animals (Scientific Procedures) Act 1986. All procedures were approved by the Animal Welfare and Ethical Review Body at King’s College London (PPL U136). The reporting of the animals used in the experiments complies with ARRIVE guidelines.
Preparation of microfluidic devices
The protocol used is a modification of the protocol described by Tsantoulas et al.45. Microfluidic devices (Xona Microfluidics) with either 2 compartments (150 μm microgroove length) or 3 compartments (500 μm microgroove) were prepared according to published protocols (Vysokov 2016) Glass bottom dishes (WillCo Wells) were cleaned by sonication and sterilized with 70% ethanol. The dishes were previously coated with 0.5 mg/ml poly-l-lysine (Sigma). Microfluidic devices were non-plasma bonded onto the glass. The assembled devices were coated after assembly with 40 µg/ml laminin (Sigma) dissolved in Neurobasal-A medium (Thermo Fisher).
DRG cultures
Preparation of dissociated primary neuron cultures was performed through aseptic excision of the spinal column. Cervical, thoracic, lumbar and sacral DRG-containing cavities were exposed and DRG were collected. The ganglia were digested with enzyme mixture containing 0.125 mg/ml collagenase (Sigma) and 10 mg/ml dispase (Thermo Fisher Scientific) for 40 min in a 37 °C and 5% CO2 humidified incubator.
Following mechanical trituration, the dissociated neurons were centrifuged on a 10% bovine serum albumin cushion in HBSS. The cell pellet was washed twice and resuspended in complete medium containing Neurobasal-A (ThermoFisher), 1% B27 supplement (Invitrogen) and 1% Glutamax (Gibco), 100 units/ml penicillin and 100 μg/ml streptomycin.
The cells were loaded into prepared microfluidic devices and left to adhere for 60 min before being flooded with 200 μl containing 150 ng/ml NGF (Gibco) on the somal side and 130 μl containing 200 ng/ml NGF on the axonal side.
DiI tracing
The lipophilic trace dye DiI was used to mark cell bodies with axons crossing the microgrooves to the axonal side of the microfluidic devices. 24–48 h prior to the recording, the axonal compartments were incubated with the DiI solution (1:200 in complete medium medium) for 1 h at 37 °C. Care was taken to ensure microfluidic isolation remained intact. After washing with Neurobasal-A medium, and replacing with complete medium, the devices were placed in 37 °C incubator until use. The stained cell bodies were visualized (Fig. S1) immediately prior to live imaging on a Nikon TE200 microscope using a TRITC fluorescence filter set.
Reagents
PGE2 stock (Sigma Aldrich) was dissolved in DMSO at 10 mM. Histamine dihydrochloride, Bradykinin and Serotonin (Tocris) stock solutions were prepared in DMSO. Tetrodotoxin (TTX) stock solution (Alomone Labs) was prepared in deionized H2O at 1 mM; Nav1.8 blockers PF-01247324, Nav1.7 blocker PF-05089771 (Tocris) were prepared in DMSO at 1 mM; the non-selective sodium channel blocker lidocaine, the cAMP antagonist cAMPS-Rp, Nav1.8 blocker A-803467, EP4 inhibitor L-161,982, ANO1 blocker T16Ainh-A01, and the non-selective HCN channel blocker zatebradine hydrochloride (all purchased from Tocris) were dissolved in DMSO. All stock solutions were kept at − 20 °C until use.
Drug perfusion
A bespoke perfusion system has been built for controlled pharmacological administration and avoidance of movement artefacts. The system is comprised of an 8-channel pen with a 360 μm removable tip (Automate Scientific) and regulated by a VC-8 Valve Controller (Warner Instruments) to allow 50 μl of solution every 5 s upon turning on.
Calcium imaging
After 4 days of culturing, both somal and axonal compartments were incubated with 2 μM of the calcium indicator dye Fura-2-AM (Invitrogen) in imaging buffer consisting of HBSS [Ca2+ and Mg2+-free] supplemented with 10 mM HEPES (ThermoFischer), 2 mM CaCl2 (Sigma), 1 mM MgCl2, 2 mM probenecid (Sigma), pH 7.4 with NaOH. Axonal and somal MFC compartments were washed twice with imaging buffer prior to recording. The devices were mounted on an inverted fluorescent microscope (Nikon Eclipse TE200) equipped with 20X Plan Fluor 0.5 NA objective and an EasyRatioPro imaging unit (Horiba Scientific). Images were acquired using ORCA 4.2 sCMOS camera (Hamamatsu). Bright field and DiI staining were visualized first and only neurons with staining in the soma (indicative of axonal crossing) were used for the analysis. The regions of interest (ROIs) were drawn around each corresponding soma and fluorescent images were acquired at 510 nm at 6 Hz using 340 and 380 nm excitation wavelengths. Drugs were applied to the axonal compartment manually or using a perfusion system while recording from the somal compartment. Care was taken to keep the fluid level higher in the somal compartment to maintain fluidic isolation intact while performing the experiments.
Voltage imaging
For recording changes of in axonal membrane potential, a voltage sensitive probe, Fluovolt (Life Technologies) was employed. Cells were loaded with Fluo|Volt according to the manufactures recommended protocols (Life Technologies). Briefly, the axonal compartment was treated with 1:1000 dissolved Fluovolt in imaging buffer for 20 min at 37 °C. After loading the axons were washed, and the devices were mounted on stage of the imaging microscope connected to EasyRatioPro. The excitation wavelength produced by the monochromator for fluorescent images is at 388 nm with an emission from the axonal compartment was recorded at 535 nm at 6.3 Hz. Following stimulation by 30 mM KCl or 10 μM PGE2, axonal responses were recorded. Care was taken to preserve the fluidic isolation between somal and axonal compartments by maintaining the fluid level in the compartments.
Image analysis
For calcium imaging experiments, the F340/F380 ratios (Fratio) were determined for designated regions of interest (ROIs) using EasyRatioPro software and the Fratio traces were analysed using Clampfit 9.0 (Molecular Devices). The responses to stimulation were visually verified and confirmed if the maximum increase in Fratio was at least three times greater than the standard deviations of the baseline calculated from at least 50 s prior to drug application (Fig. S2). The peak response (ΔFratio) was calculated as the maximum increase in fluorescence intensity above the baseline. In some experiments, 60 mM KCl was applied to the somal compartment to determine the number of neuronal responders. For PGE2 induced activity, each transient event was defined as increase in Fratio with a peak that was at least three times greater the standard deviation of the baseline. Baselines were calculated from at least 10 s prior to application of stimulus. All events were visually inspected and confirmed as a response.
The detection of FluoVolt fluorescence intensity changes was defined as the (ΔF/F) between baseline responses taken at least 10 s prior to application of stimulus where no fluorescence activity was reported and ΔF maximum peaks within the timespan of application.
For voltage imaging experiments, frame by frame TIFF files were transferred from EasyRatio Pro to FIJI, where axonal ROIs were selected according to brightness intensity changes. We quantified the changes in axonal membrane potential in microfluidic cultures by determining the average peak change in fluorescent intensity across all axonal regions in the field of view (FoV). The average peak change in fluorescence intensity was calculated by first determining a mean baseline image from 50 frames prior to drug application and subtracting the mean baseline image from all image stacks to create a ΔF image stack. The ΔF images were thresholded to demarcate the activated regions of in the axons. Particle Analysis in FIJI was used to assign the ROIs. The average peak in FluoVolt fluorescence intensity for each axonal ROI was calculated using the formula: 100 (Mean Peak Response- Mean Baseline Response) / Mean Baseline Response).
We also determined the proportion of the total axonal area that showed a change in FluoVolt fluorescence signal intensity in the FoV. As the limitations of FluoVolt did not allow longer recording times needed to determine the responses in the same FoV to the application of the inhibitors, we used the proportion of axonal area that showed an increase in FluoVolt signal to avoid any bias caused by the heterogeneity of the axonal responses between the experiments. The quantification of axonal areas that exhibited a change in membrane potential was represented as a percentage of the total axonal area that showed a change in FluoVolt fluorescence following drug application. Total axonal areas in each image, expressed as total number of pixels, were determined prior to drug application by thresholding the images in Fiji and selecting the entire axonal regions over the background. The activated axonal areas were determined from background subtracted images that were thresholded to highlight the areas that showed a change in intensity following drug application. The percentage ratio of the activated area to the total axonal area was taken as a measure of the activated area.
Statistics
All data are reported as mean ± SEM unless otherwise stated. Statistical analysis has been performed using GraphPad Prism 9. Statistical significance was set at p < 0.05. Student t-test (unpaired, equal variance) was used to compare groups in calcium imaging analysis. One Way ANOVA with Tukey’s multiple comparison test was used for comparisons between three or more independent groups in calcium imaging analysis. Brown-Forsythe and Welch ANOVA tests were used to determine significance between groups of equal and different variance respectively on voltage imaging analysis. All data were normally distributed based on the Shapiro–Wilk normality test. For the analysis of the number of calcium transients per 3-min interval a Wilcoxon matched-pairs signed rank test was used.
Data availability
All data is provided within the manuscript or supplementary information file. All queries should be directed to Dr Ramin Raouf at ramin.raouf@kcl.ac.uk.
References
Roberts, N. L. S., Mountjoy-Venning, W. C., Anjomshoa, M., Banoub, J. A. M. & Yasin, Y. J. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study (vol 392, pg 1789, 2018). Lancet 393, E44–E44 (2019).
Jang, Y., Kim, M. & Hwang, S. W. Molecular mechanisms underlying the actions of arachidonic acid-derived prostaglandins on peripheral nociception. J. Neuroinflammation 17, 30. https://doi.org/10.1186/s12974-020-1703-1 (2020).
Petho, G. & Reeh, P. W. Sensory and signaling mechanisms of bradykinin, eicosanoids, platelet-activating factor, and nitric oxide in peripheral nociceptors. Physiol. Rev. 92, 1699–1775. https://doi.org/10.1152/physrev.00048.2010 (2012).
Smith, W. L., Dewitt, D. L. & Garavito, R. M. CYCLOOXYGENASES: Structural, cellular, and molecular biology. Annu. Rev. Biochem. 69, 145–182 (2000).
McCarberg, B. & Gibofsky, A. Need to develop new nonsteroidal anti-inflammatory drug formulations. Clin. Ther. 34, 1954–1963. https://doi.org/10.1016/j.clinthera.2012.08.005 (2012).
Oida, H. et al. In situ hybridization studies of prostacyclin receptor mRNA expression in various mouse organs. Br. J. Pharmacol. 116, 2828–2837. https://doi.org/10.1111/j.1476-5381.1995.tb15933.x (1995).
Regan, J. W. EP2 and EP4 prostanoid receptor signaling. Life Sci. 74, 143–153. https://doi.org/10.1016/j.lfs.2003.09.031 (2003).
Fujino, H., Salvi, S. & Regan, J. W. Differential regulation of phosphorylation of the cAMP response element-binding protein after activation of EP2 and EP4 prostanoid receptors by prostaglandin E2. Mol. Pharmacol. 68, 251–259. https://doi.org/10.1124/mol.105.011833 (2005).
Clark, A. L. Osteoarthritis: What we have been missing in the patellofemoral joint. Exerc. Sport Sci. Rev. 36, 30–37. https://doi.org/10.1097/jes.0b013e31815e4217 (2008).
Murase, A., Nakao, K. & Takada, J. Characterization of binding affinity of CJ-023,423 for human prostanoid EP4 receptor. Pharmacology 82, 10–14. https://doi.org/10.1159/000125674 (2008).
McCoy, J. M., Wicks, J. R. & Audoly, L. P. The role of prostaglandin E2 receptors in the pathogenesis of rheumatoid arthritis. J. Clin. Investig. 110, 651–658. https://doi.org/10.1172/JCI15528 (2002).
Coleridge, H. M. et al. Stimulation of “irritant” receptors and afferent C-fibres in the lungs by prostaglandins. Nature 264, 451–453. https://doi.org/10.1038/264451a0 (1976).
Mizumura, K., Minagawa, M., Tsujii, Y. & Kumazawa, T. Prostaglandin E2-induced sensitization of the heat response of canine visceral polymodal receptors in vitro. Neurosci. Lett. 161, 117–119. https://doi.org/10.1016/0304-3940(93)90154-d (1993).
Brunsden, A. M. & Grundy, D. Sensitization of visceral afferents to bradykinin in rat jejunum in vitro. J. Physiol. 521(Pt 2), 517–527. https://doi.org/10.1111/j.1469-7793.1999.00517.x (1999).
Linhart, O., Obreja, O. & Kress, M. The inflammatory mediators serotonin, prostaglandin E2 and bradykinin evoke calcium influx in rat sensory neurons. Neuroscience 118, 69–74. https://doi.org/10.1016/s0306-4522(02)00960-0 (2003).
Nicolson, T. A., Foster, A. F., Bevan, S. & Richards, C. D. Prostaglandin E2 sensitizes primary sensory neurons to histamine. Neuroscience 150, 22–30. https://doi.org/10.1016/j.neuroscience.2007.09.003 (2007).
Tsantoulas, C. et al. Probing functional properties of nociceptive axons using a microfluidic culture system. PLoS ONE https://doi.org/10.1371/journal.pone.0080722 (2013).
Vysokov, N., McMahon, S. B. & Raouf, R. The role of NaV channels in synaptic transmission after axotomy in a microfluidic culture platform. Sci. Rep. https://doi.org/10.1038/s41598-019-49214-w (2019).
Emery, E. C., Young, G. T., Berrocoso, E. M., Chen, L. & McNaughton, P. A. HCN2 ion channels play a central role in inflammatory and neuropathic pain. Science 333, 1462–1466. https://doi.org/10.1126/science.1206243 (2011).
Momin, A., Cadiou, H., Mason, A. & McNaughton, P. A. Role of the hyperpolarization-activated current Ih in somatosensory neurons. J. Physiol. 586, 5911–5929. https://doi.org/10.1113/jphysiol.2008.163154 (2008).
Gold, M. S., Levine, J. D. & Correa, A. M. Modulation of TTX-R INa by PKC and PKA and their role in PGE2-induced sensitization of rat sensory neurons in vitro. J. Neurosci. 18, 10345–10355 (1998).
Ceriani, F. & Mammano, F. A rapid and sensitive assay of intercellular coupling by voltage imaging of gap junction networks. Cell Commun. Signal. https://doi.org/10.1186/1478-811X-11-78 (2013).
Miller, E. W. et al. Optically monitoring voltage in neurons by photoinduced electron transfer through molecular wires. Proc. Natl. Acad. Sci. USA 109, 2114–2119. https://doi.org/10.1073/pnas.1120694109 (2012).
Renganathan, M., Cummins, T. R. & Waxman, S. G. Contribution of Na(v)1.8 sodium channels to action potential electrogenesis in DRG neurons. J. Neurophysiol. 86, 629–640. https://doi.org/10.1152/jn.2001.86.2.629 (2001).
Cho, H. et al. The calcium-activated chloride channel anoctamin 1 acts as a heat sensor in nociceptive neurons. Nat. Neurosci. 15, 1015–1021. https://doi.org/10.1038/nn.3111 (2012).
Rivera, C. et al. The K+/Cl− co-transporter KCC2 renders GABA hyperpolarizing during neuronal maturation. Nature 397, 251–255. https://doi.org/10.1038/16697 (1999).
Sung, K. W., Kirby, M., McDonald, M. P., Lovinger, D. M. & Delpire, E. Abnormal GABAA receptor-mediated currents in dorsal root ganglion neurons isolated from Na-K-2Cl cotransporter null mice. J. Neurosci. 20, 7531–7538. https://doi.org/10.1523/JNEUROSCI.20-20-07531.2000 (2000).
Lu, J., Karadsheh, M. & Delpire, E. Developmental regulation of the neuronal-specific isoform of K-Cl cotransporter KCC2 in postnatal rat brains. J. Neurobiol. 39, 558–568 (1999).
Park, J., Koito, H., Li, J. & Han, A. Microfluidic compartmentalized co-culture platform for CNS axon myelination research. Biomed. Microdevices 11, 1145–1153. https://doi.org/10.1007/s10544-009-9331-7 (2009).
Taylor, A. M. et al. A microfluidic culture platform for CNS axonal injury, regeneration and transport. Nat. Methods 2, 599–605. https://doi.org/10.1038/nmeth777 (2005).
Vitzthum, L. et al. Study of Na+/H+ exchange-mediated pHi regulations in neuronal soma and neurites in compartmentalized microfluidic devices. Integr. Biol. 2, 58–64. https://doi.org/10.1039/b918440f (2010).
Yang, I. H., Siddique, R., Hosmane, S., Thakor, N. & Hoke, A. Compartmentalized microfluidic culture platform to study mechanism of paclitaxel-induced axonal degeneration. Exp. Neurol. 218, 124–128. https://doi.org/10.1016/j.expneurol.2009.04.017 (2009).
Pitchford, S. & Levine, J. D. Prostaglandins sensitize nociceptors in cell culture. Neurosci. Lett. 132, 105–108 (1991).
Dubin, A. E. & Patapoutian, A. Nociceptors: The sensors of the pain pathway. J. Clin. Investig. 120, 3760–3772 (2010).
Young, G. T., Emery, E. C., Mooney, E. R., Tsantoulas, C. & McNaughton, P. A. Inflammatory and neuropathic pain are rapidly suppressed by peripheral block of hyperpolarisation-activated cyclic nucleotide-gated ion channels. Pain 155, 1708–1719. https://doi.org/10.1016/j.pain.2014.05.021 (2014).
Emery, E. C. et al. In vivo characterization of distinct modality-specific subsets of somatosensory neurons using GCaMP. Sci. Adv. 2, e1600990. https://doi.org/10.1126/sciadv.1600990 (2016).
Koda, H. & Mizumura, K. Sensitization to mechanical stimulation by inflammatory mediators and by mild burn in canine visceral nociceptors in vitro. J. Neurophysiol. 87, 2043–2051. https://doi.org/10.1152/jn.00593.2001 (2002).
Banik, R. K., Kozaki, Y., Sato, J., Gera, L. & Mizumura, K. B2 receptor-mediated enhanced bradykinin sensitivity of rat cutaneous C-fiber nociceptors during persistent inflammation. J. Neurophysiol. 86, 2727–2735. https://doi.org/10.1152/jn.2001.86.6.2727 (2001).
Pettinger, L., Gigout, S., Linley, J. E. & Gamper, N. Bradykinin controls pool size of sensory neurons expressing functional delta-opioid receptors. J. Neurosci. 33, 10762–10771. https://doi.org/10.1523/JNEUROSCI.0123-13.2013 (2013).
Mizumura, K., Sato, J. & Kumazawa, T. Effects of prostaglandins and other putative chemical intermediaries on the activity of canine testicular polymodal receptors studied in vitro. Pflügers Archiv. 408, 565–572. https://doi.org/10.1007/bf00581157 (1987).
Lang, E., Novak, A., Reeh, P. W. & Handwerker, H. O. Chemosensitivity of fine afferents from rat skin in vitro. J. Neurophysiol. 63, 887–901. https://doi.org/10.1152/jn.1990.63.4.887 (1990).
Schaible, H. G. & Schmidt, R. F. Excitation and sensitization of fine articular afferents from cat’s knee joint by prostaglandin E2. J. Physiol. 403, 91–104 (1988).
Nikolaev, V. O., Bunemann, M., Hein, L., Hannawacker, A. & Lohse, M. J. Novel single chain cAMP sensors for receptor-induced signal propagation. J. Biol. Chem. 279, 37215–37218. https://doi.org/10.1074/jbc.C400302200 (2004).
Gervasi, N. et al. Dynamics of protein kinase A signaling at the membrane, in the cytosol, and in the nucleus of neurons in mouse brain slices. J. Neurosci. 27, 2744–2750. https://doi.org/10.1523/JNEUROSCI.5352-06.2007 (2007).
Dunn, T. A. & Feller, M. B. Imaging second messenger dynamics in developing neural circuits. Dev. Neurobiol. 68, 835–844. https://doi.org/10.1002/dneu.20619 (2008).
Calebiro, D. & Maiellaro, I. cAMP signaling microdomains and their observation by optical methods. Front. Cell Neurosci. 8, 350. https://doi.org/10.3389/fncel.2014.00350 (2014).
England, S., Bevan, S. & Docherty, R. J. PGE2 modulates the tetrodotoxin-resistant sodium current in neonatal rat dorsal root ganglion neurones via the cyclic AMP-protein kinase A cascade. J. Physiol. 495(Pt 2), 429–440. https://doi.org/10.1113/jphysiol.1996.sp021604 (1996).
Baker, M. D. Protein kinase C mediates up-regulation of tetrodotoxin-resistant, persistent Na+ current in rat and mouse sensory neurones. J. Physiol. 567, 851–867. https://doi.org/10.1113/jphysiol.2005.089771 (2005).
Gold, M. S., Reichling, D. B., Shuster, M. J. & Levine, J. D. Hyperalgesic agents increase a tetrodotoxin-resistant Na+ current in nociceptors. Proc. Natl. Acad. Sci. USA 93, 1108–1112. https://doi.org/10.1073/pnas.93.3.1108 (1996).
MacDonald, D. I. et al. A central mechanism of analgesia in mice and humans lacking the sodium channel NaV1.7. Neuron 109, 1497-1512.e1496. https://doi.org/10.1016/j.neuron.2021.03.012 (2021).
Vaughn, A. H. & Gold, M. S. Ionic mechanisms underlying inflammatory mediator-induced sensitization of dural afferents. J. Neurosci. 30, 7878–7888. https://doi.org/10.1523/JNEUROSCI.6053-09.2010 (2010).
Kaila, K., Price, T. J., Payne, J. A., Puskarjov, M. & Voipio, J. Cation-chloride cotransporters in neuronal development, plasticity and disease. Nat. Rev. Neurosci. 15, 637–654. https://doi.org/10.1038/nrn3819 (2014).
Price, T. J., Cervero, F., Gold, M. S., Hammond, D. L. & Prescott, S. A. Chloride regulation in the pain pathway. Brain Res. Rev. 60, 149–170. https://doi.org/10.1016/j.brainresrev.2008.12.015 (2009).
Modol, L., Cobianchi, S. & Navarro, X. Prevention of NKCC1 phosphorylation avoids downregulation of KCC2 in central sensory pathways and reduces neuropathic pain after peripheral nerve injury. Pain 155, 1577–1590. https://doi.org/10.1016/j.pain.2014.05.004 (2014).
Lucas, O., Hilaire, C., Delpire, E. & Scamps, F. KCC3-dependent chloride extrusion in adult sensory neurons. Mol. Cell Neurosci. 50, 211–220. https://doi.org/10.1016/j.mcn.2012.05.005 (2012).
Acknowledgements
We would like to thank M. Malcangio and S.B. McMahon for their insightful comments on the project. We also thank N. Vysokov for helpful discussions and technical assistance. The authors acknowledge kind support from the following: G.K. is supported by the Foundation for Education and European Culture (Founders Nicos & Lydia Tricha) N.R. was supported by KMRT Joint Research Committee PhD Studentship to R.R. and P.A.M.
Funding
The authors acknowledge kind support from the following: G.K. is supported by the Foundation for Education and European Culture (Founders Nicos & Lydia Tricha) N.R. was supported by KMRT Joint Research Committee PhD Studentship to R.R. and P.A.M.
Author information
Authors and Affiliations
Contributions
G.K., N.R., P.A.M and R.R. designed the experiments. G.K., N.R., B.J.J., S.J., and R.R. carried out data collection and analysis. P.A.M and R.R. supervised the study.
Corresponding author
Ethics declarations
Competing interests
R.R. is involved in a research collaboration with Grünenthal GmbH to develop microfluidic culture models based on human iPSCs for pain research. P.A.M. is involved in a drug discovery program in collaboration with Merck & Co, Inc, to develop HCN2-selective molecules as novel analgesics. G.K., N.R., B.J.J., and S.J. declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kimourtzis, G., Rangwani, N., Jenkins, B.J. et al. Prostaglandin E2 depolarises sensory axons in vitro in an ANO1 and Nav1.8 dependent manner. Sci Rep 14, 17360 (2024). https://doi.org/10.1038/s41598-024-67793-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-67793-1
- Springer Nature Limited