Abstract
Keeping up to date with the latest clinical advances in prostate cancer can be challenging. We investigated the impact of guideline use on quality of treatment decisions as well as the impact of a novel, CE-certified clinical decision support tool (Siemens AIPC software) on the amount of time clinicians spend on decision-making in a multicenter setting. Ten urologists assessed ten clinical cases (screening and localized prostate cancer) in three settings: without support, using a digital version of the EAU guidelines, and with the AIPC tool, resulting in 300 clinical decisions. Comparison involved time spent, decision correct- and completeness. Using AIPC compared to digital guidelines led to a significant reduction of expenditure of time at a per case level (3.57 min and 0:14 min, p < 0.01) and for overall time per urologist (39.45 min and 02:20 min, p < 0.01). Decision options without guidelines support, online guideline usage and usage of AIPC were complete in 61%, 80% and 100%, respectively (p < 0.01). Decision making without guidelines support, online guideline usage and usage of AIPC was correct including all options in 28%, 66% and 100%, respectively (p < 0.01).
Clinical decision support systems have the potential to reduces decision-making time and to enhance decision quality.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Prostate cancer, with approximately 1.4 million newly diagnosed cases worldwide, ranks as the second most common cancer in men. Given its diverse stages and the wide range of diagnostic and treatment options available, it represents a heterogeneous disease with a rapidly evolving diagnostic and therapeutic landscape1. For clinicians, staying up-to-date in such an interdisciplinary medical field can be a demanding challenge, both in terms of time and mental effort, amidst their routine work. The EAU Guidelines serve as a widely accepted compilation of evidence-based urologic care2. To ensure optimal oncological care experts for different specialties must cooperate and the patient's opinion must be taken into consideration. The vast amount of data generated during this process is often spread within different platforms specialized for each discipline3.
This scattered and overwhelming data can pose challenges during clinical practice, as clinicians spend a significant portion of their time gathering and processing medical information4. Ideally, the clinical data required for a comprehensive overview should be easily accessible in a standardized and clearly structured format, facilitating the continuous and efficient exchange of relevant information. This ensures that healthcare professionals can access and interpret the necessary information without undue difficulty.
In recent years, advancements in data technology and artificial intelligence have led to the development of clinical decision support systems (CDSSs) for a wide range of diseases. In the field of oncology, CDSS has emerged as a transformative tool, revolutionizing the diagnosis, treatment, and management of cancer patients. By leveraging its capability to analyze vast amounts of medical data and provide evidence-based recommendations, CDSS holds tremendous potential for enhancing clinical decision-making and ultimately improving patient outcomes5,6,7,8.
To address the challenges mentioned above, our clinic implemented AI-Pathway Companion, a CE-certified clinical decision support software, specifically designed for patients with prostate cancer since 20209. Previous publications have highlighted the time-saving benefits of AIPC and similar software, allowing clinicians to efficiently access and interpret relevant clinical data for prostate cancer patients9,10. However, research on its advanced functionalities, particularly its ability to generate treatment recommendations in line with established guidelines, remains limited. Therefore, this study aims to bridge this research gap by adopting a preliminary approach using fictional patient cases.
Methods
All methods were carried out in accordance with relevant guidelines and regulations. The Ethikkommission Nordwest- und Zentralschweiz (EKNZ) provided an exempt from ethical committee approval due to its design and study category.
The patients examined in the study were purely virtual, not real individuals, therefore no specific informed consent was necessary.
Clinical decision support software (CDSS)
We utilized the clinical decision support software AI-Pathway Companion Prostate Cancer VA10B (Siemens Healthcare GmbH, Erlangen, Germany) for this study. This software effectively consolidates, correlates, and presents pertinent clinical information along the disease-specific pathway in user-friendly dashboards, as previously described8. Furthermore, it offers support and recommendations regarding diagnostic and therapeutic options for prostate cancer by incorporating evidence from clinical guidelines (such as the current EAU guidelines, as applied in this study) and aligning them with the patients' present disease condition.
Study participants
Ten urology residents from two distinct Swiss departments, namely Kantonsspital Baselland Liestal and Universitätsspital Basel, participated in this study. The residents had varying professional experience, ranging from 1 to 6 years. Prior to the actual investigation, all participants underwent a brief training on the usage of the AIPC software.
Patients’ characteristics
Ten prostate cancer cases comprising the patient pathway from screening to treatment of localized prostate cancer had to be solved (Table 1).
Study design
We evaluated the utility of the software for clinical decision making in prostate care. Ten urologists solved ten prostate cancer cases in three distinguished test settings (as described below) resulting in a total of 300 decisions.
The spectrum of clinical cases ranged from screening to newly diagnosed prostate cancer with different EAU risk groups and the task was to propose the most appropriate consecutive diagnostic or therapeutic step. To reduce possible confounds due to case variations, each reader had to accomplish the same ten cases. Expenditure of time, correctness, and completeness of the decision for therapeutic or diagnostic options were assessed.
Settings
In the first setting participants solved the cases solely based on their knowledge with the use of literature, guidelines etc. being excluded. For the assessment of the cases, participants were presented with a comprehensive table containing the available clinical information.
In the second setting participants were instructed to use a digital version of the EAU prostate cancer guideline to support the clinical decision making and had to find the according guideline recommendation based on a comprehensive table containing the available clinical information. Decisions solely reliant on the knowledge of participants were not deemed valid.
In a third setting participants were supported by the use of the AIPC guideline service providing decision options including a link to the relevant section of the EAU guideline to optimize the decision-making process. The AIPC software provided the available clinical information.
To reduce bias, a wash-out period of two weeks was instantiated between the sessions. All cases were first compiled in the first setting afterwards using the guidelines and finally using the AIPC in order to avoid previous opinion bias.
Evaluation
Time for clinical decision with and without EAU Guideline verification was measured. Correctness of the clinical decision was graded in complete, incomplete and wrong by a team of two board certified urologists. The current EAU Guideline recommendations were used as the standard for definitive management.
Statistical analysis
The Wilcoxon signed-rank test was used to compare case preparation time for the traditional method and the software. p < 0.05 was considered statistically significant. Analysis was conducted in R (R Core Team, 2014) and figures were produced using the package ggplot2.
Results
Time expenditure
Time expenditure overall, per urologist and per patient are summarized in Table 2.
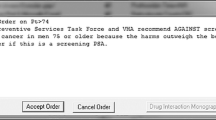
The usage of AIPC significantly reduced the time spent per patient, per urologist as well as the overall time as compared to decision making without guidelines and usage of written guidelines (Fig. 1).
The bars show the mean time to complete all 10 tasks overall (1) and per urologist (2) with (a) without guideline use and (b) support of written guidelines and (c) AI-Pathway Companion; ***p < 0.00001; The last bar chart shows the percentage of (I) wrong (II) incomplete and (III) complete decision with all 3 settings used.
Decision completeness and correctness
With a mean of 35 s per patient, the first setting without any decision support was fast. However, it only led to complete answers in 28% and to correct answers in 66% of cases.
The usage of written guidelines improved the correctness of decisions and completeness of options to 80% and 66%, respectively (Fig. 1). AIPC support led to 100% correct and complete answers. However, using the guideline to verify decision making was associated with a significantly longer time for decision making (35 s vs. 597 s; + 1700% per patient).
Discussion
Guidelines are statements that include recommendations intended to optimize patient care that are informed by a systematic review of evidence and an assessment of the benefits and harms of alternative care options11. Whether in discussions with colleagues during multidisciplinary team meetings or conducting one-on-one consultations with patients, physicians are expected to implement this data driven best practice. This challenge becomes even more pronounced in the context of low-volume centers, rare cancer entities, and in trainees who oncologic knowledge may be incomplete. Written guidelines play a central role in this process, but disease stage specific information is often spread in hundreds of pages of text and time is a limiting factor to check every decision for its guideline adherence.
On average, physicians can only spend 4.6 h a week to acquire the most recent information, leading to an increasing gap between clinically applied treatment and actually available evidence-based recommendations12,13,14.
Given the excessive amount of data generated during the treatment of prostate cancer patients, a CDSS is a valuable tool for extracting and presenting relevant information in a time-efficient manner9. Automated AI supported data interpretation and decision-making are next milestones in AI-assisted patient care.
Prior applications have focused on early detection and treatment specific automated calculation and processing. Even the advanced approach with IBM`s Watson for Oncology focused mainly on therapeutic options while AIPC not only suggests therapeutic but also diagnostic options6,13.
This study represents the initial exploration of APIC's advanced feature aimed at providing automated guideline-conforming recommendations for clinical decision-making in patients with prostate cancer. Within the protected framework of fictional patients our study is a first step on this journey.
The result of this study demonstrate that the use of guidelines is very time consuming. Prior studies already demonstrated that the application of the AIPC software has resulted in a noteworthy impact on time expenditure for case preparation9.
The application of the decisions support tool led to a highly significant reduction of overall time (-94%) required for the entire clinical decision-making process as compared to conventional approach with the usage of written guidelines. This time saving effect is of particular value as it enables the treating physicians to allocate their precious and already limited time in clinical practice not to searching processes but to focusing more on the patient’s individual treatment.
Here, we also demonstrate the potential of CDSS to improve the quality of decision making. By using the software, the rate of incomplete and wrong decisions significantly decreased from 33 to 0% and incomplete decisions decreased from 39 to 0% as compared to the first setting using no guidelines.
These results highlight the potential of CDSS to augment our adherence to established clinical guidelines, ensuring that our medical interventions align with the latest evidence-based practices. By doing so, it not only contributes to better patient outcomes but also underscores our commitment to providing the highest quality of care while optimizing resource allocation15,16,17. Especially out of the patient’s perspective establishing extra safety barriers in order to prevent medical errors is of prime interest18,19.
The utilization of the software enables clinicians to operate automatically at the cutting edge of oncologic knowledge including yearly updates.
As a result, modifications in guideline recommendations could become more promptly evident, given its integration into clinical routines. This fosters a continuous educational effect, particularly through the software's capability to link specific recommendations with corresponding text passages in the EAU Guidelines document.
Despite the multicenter setting and the overall analysis of 300 cases, this study is associated with limitations. First, “only” 10 resident urologists solved “only” 10 clinical cases each, thus limiting the diversity of settings. Secondly, these clinical cases were preconstructed but nonetheless reflect routine cases present in everyday clinical practice. Lastly, since the clinical experience of our participants ranges between 1 and 6 years, the generalization to the full spectrum of urologists is limited Nonetheless, even among experienced clinicians, non-adherence to oncologic guidelines continues to be a persistent challenge and AI-supported tools may offer a valuable solution8,20,21.
Prostate cancer as a highly variable medical condition, demands clinicians to carefully weigh clinical advantages, patient life expectancy, concurrent health issues, and potential treatment-related complications when making decisions. Therefore, a software might support but not replace a human made clinical decision to fully implement all important individual factors.
Importantly, AIPC also allows for individualized options and therapy interruptions, ensuring that the user is not coerced into a specific decision but instead maintains flexibility.
Overall, the utilization of AIPC resulted in a noteworthy reduction in the time required for making verified clinical decisions, indicating increased efficiency. Moreover, the software demonstrated a significantly stronger adherence to clinical guidelines and improved quality of decision-making.
As a future outlook, the application of CDSS has wide implications20,21 not only for prostate cancer treatment but multiple tumor entities as well as benign conditions and can help to streamline and optimize the patient pathway and treatment quality. Especially in cases involving more advanced tumor stages, where treatment options become increasingly complex, software-based support, such as AIPC, hold promising potential.
Conclusion
Implementing advanced clinical decision support systems, such as AIPC, not only significantly reduces decision-making time but also enhances decision quality, underscoring their transformative potential for efficient, high-quality patient care.
Future studies are necessary to assess the effect of AIPC in real life patients and their oncologic heterogeneity.
Data availability
The data that support the findings of this study are available from corresponding authors but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Siemens Healthineers.
References
De Santis, M., Mottet, N., Cornford, P. & Gillessen, S. Precision oncology for metastatic prostate cancer: Translation into practice. Eur. Urol. Switzerland 78, 771–4 (2020).
N.Mottet, P.Cornford, Bergh RCN va. den, al EB et. EAU - EANM - ESTRO - ESUR - ISUP - SIOG Guidelines on Prostate Cancer 2023. EAU Guidelines. p.
Melzer, G., Maiwald, T., Prokosch, H. U. & Ganslandt, T. Leveraging real-world data for the selection of relevant eligibility criteria for the implementation of electronic recruitment support in clinical trials. Appl. Clin. Inform. 12(01), 17–26. https://doi.org/10.1055/s-0040-1721010 (2021).
Henkel, M. & Stieltjes, B. Structured data acquisition in oncology. Oncology. 98, 423–9 (2020).
Suwanvecho, S. et al. Comparison of an oncology clinical decision-support system’s recommendations with actual treatment decisions. J. Am. Med. Inform. Assoc. 28, 832–8 (2021).
Jie, Z., Zhiying, Z. & Li, L. A meta-analysis of Watson for oncology in clinical application. Sci. Rep. 11, 5792 (2021).
Kann, B. H., Hosny, A. & Aerts, H. J. W. L. Artificial intelligence for clinical oncology. Cancer Cell 39(7), 916–927 (2021).
Voigt, W. & Trautwein, M. Improved guideline adherence in oncology through clinical decision-support systems: Still hindered by current health IT infrastructures?. Curr. Opin. Oncol. 35(1), 68 (2023).
Henkel, M. et al. Initial experience with AI pathway companion: Evaluation of dashboard-enhanced clinical decision making in prostate cancer screening. PloS One. 17, e0271183 (2022).
Henkel, M. et al. Toward a platform for structured data acquisition in oncology: A pilot study on prostate cancer screening. Oncology. 99(12), 802–812 (2021).
Graham R, Mancher M, Wolman DM, Greenfield S, Steinberg E. Clinical Practice Guidelines We Can Trust. Graham R, Mancher M, Wolman DM, Greenfield S, Steinberg E, editors. Washington, D.C.: National Academies Press; (2011)
Woolhandler, S. & Himmelstein, D. U. Administrative work consumes one-sixth of U.S. Physicians’ working hours and lowers their career satisfaction. Int. J. Heal. Serv. 44(4), 635–42. https://doi.org/10.2190/HS.44.4.a (2014).
Lee, K. & Lee, S. H. Artificial intelligence-driven oncology clinical decision support system for multidisciplinary teams. Sens. (Basel). 20(17), 4693 (2020).
Cornford, P. et al. IMAGINE-IMpact assessment of guidelines implementation and education: The next frontier for harmonising urological practice across europe by improving adherence to guidelines. Eur. Urol. 79(2), 173–176 (2021).
Kozikowski, M., Malewski, W., Michalak, W. & Dobruch, J. Clinical utility of MRI in the decision-making process before radical prostatectomy: Systematic review and meta-analysis. PLoS One. 14(1), e0210194–e0210194 (2019).
Mazo, C., Kearns, C., Mooney, C. & Gallagher, W. M. Clinical decision support systems in breast cancer: A systematic review. Cancers (Basel). 12(2), 369 (2020).
Nafees, A. et al. Evaluation of clinical decision support systems in oncology: An updated systematic review. Crit. Rev. Oncol. Hematol. 192, 104143 (2023).
Lipczak, H., Dørflinger, L., Enevoldsen, C., Vinter, M. M. & Knudsen, J. L. Cancer patients’ experiences of error and consequences during diagnosis and treatment. Patient Exp. J. 2, 102–10 (2015).
Carey, M. et al. The patient perspective on errors in cancer care: Results of a cross-sectional survey. J. Patient Saf. 15(4), 322–327 (2019).
Khilfeh, I. et al. Real world US community urology adherence to prostate cancer guidelines. JCO Oncol. Pract. 19(11suppl), 449. https://doi.org/10.1200/OP.2023.19.11_suppl.449 (2023).
MacLennan, S. et al. Improving guideline adherence in urology. Eur. Urol. Focus. 8(5), 1545–52 (2022).
Author information
Authors and Affiliations
Contributions
Conceptualization: Christian Wetterauer, Philip Cornford, Bram Stieltjes, Aurelien Stalder Data curation: Christian Engesser, Saskia Fassbind, Viktor Alargkof, Joelle Studer, Johannes Engesser, Manuel Walter, Carmen Eckert, Sarah Gina Dugas, Sarah Ursula Sutter, Anas Elyan, Trotsenko Pawel, Seifert Helge Supervision: Christian Wetterauer Writing – original draft: Christian Engesser, Maurice Henkel, Christian Wetterauer. Writing – review & editing: Maurice Henkel, Christian Wetterauer.
Corresponding author
Ethics declarations
Competing interests
No competing interest: Alargkof V., Fassbind S., Studer J., Engesser J., Walter M., Elyan A., Dugas S., Trotsenko P., Sutter S., Eckert C., Hofmann S., Seifert H., Cornford P., Stieltjes B., Wetterauer C. Competing interest to declare: Engesser C., Henkel M., Stieltjes B., received financial support as part of a research fund by Siemens Healthineers Wetterauer C. worked as a consultant for Siemens Healthineers for development of the software. Stalder A. is an employee of Siemens Healthineers.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Engesser, C., Henkel, M., Alargkof, V. et al. Clinical decision making in prostate cancer care—evaluation of EAU-guidelines use and novel decision support software. Sci Rep 14, 19113 (2024). https://doi.org/10.1038/s41598-024-70292-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-70292-y
- Springer Nature Limited