Abstract
Insomnia is a major concern among stressed workers worldwide. Although stress generally has a detrimental effect on sleep quality, the impact of biological stress, especially the immunological stress response, on sleep quality is not yet fully understood. Stressed workers were recruited through a screening process using a Brief Job Stress Questionnaire. The participants were asked to complete various occupation-related questionnaires. Additionally, saliva samples were collected to assess interleukin-6 (IL-6) levels as an immunological stress response. Subsequently, they were asked to wear an Apple Watch to record their sleep pattern for one week. Their sleep architecture was estimated using a previously published and validated method. Finally, data from 73 participants were analyzed. Our multivariable analysis revealed that shorter durations of slow-wave sleep (non-rapid eye movement sleep stage 3) were significantly associated with elevated IL-6 levels (p = 0.005) and greater daytime sleepiness (p = 0.002) after controlling for total sleep time. Our finding that a higher immunological stress response is associated with poor sleep quality contributes to a better understanding of insomnia in stressed workers and emphasizes the importance of stress management in this population.
Similar content being viewed by others
Introduction
Occupational stress is a significant concern worldwide due to its association with psychological and physiological stress responses, ultimately resulting in decreased productivity and increased sick leave1,2,3. According to a survey about occupational stress-related mental health problems conducted by the Japanese government, 8.8% of all workers required medical leave, and 4.1% had to permanently leave their companies4. According to the diathesis-stress model and the model proposed by the National Institute for Occupational Safety and Health, it has been considered that the combination of occupational stress and individual vulnerability can induce various mental health problems5,6, such as insomnia, adjustment disorder and depression7,8,9. Unfortunately, in some cases, individuals experiencing extremely high occupational stress commit suicide10. While the overarching objective is to reduce occupational stress, practical approaches involve the comprehensive management of occupational stress and its associated detrimental consequences. In this context, preserving high-quality sleep can act as a resilience factor against occupational stress-related mental health problems5 because stress is considered one of the major causes of sleep disturbances11,12, and sleep disturbances in stressed workers are well-known risk factors and/or major components of adjustment disorder, burnout and depression12,13,14.
While sleep assessment in stressed workers may be critical in identifying sleep disturbance as a great risk for occupational stress-related mental health problems, previous studies have primarily focused on sleep duration rather than sleep quality because of the difficulty in objectively evaluating sleep quality. Methods for assessing sleep quality vary among research groups; however, non-REM stage 3 (N3; also known as deep sleep or slow wave sleep), is considered a representative marker of sleep quality because it is believed to underlie multiple restorative functions of sleep and the lack thereof has been associated with depression and subjective complaints of insomnia15,16,17,18,19,20.
The sleep architecture consists of non-rapid eye movement (non-REM) stages 1, 2, and 3 and REM sleep. N3 is predominantly observed during the first half of sleep. The gold standard tool for assessing sleep architecture is polysomnography (PSG)21. A study using PSG in workers suffering from burnout revealed a reduction in both N3 and REM sleep compared with healthy controls13. However, due to the limited accessibility and availability of PSG-based sleep assessment in clinical settings, stemming from time and cost constraints, the use of such specialized equipment is impractical for the early detection of daily sleep disturbances in high-stress workers, necessitating a more accessible assessment tool. Even for research use, the significant financial resources required for the necessary equipment and trained personnel, the time-consuming setup and execution, and participant discomfort affecting natural sleep patterns make PSG less practical for large-scale studies. Thus, we recently developed a highly precise and user-friendly method utilizing an Apple Watch, which has already undergone validation and publication22,23. Specific algorithms based on the heart rate obtained from the Apple Watch during sleep can categorize the time spent in each sleep stage, allowing for an accurate assessment of sleep quality in daily life.
Similar to sleep quality, occupational stress is typically evaluated using questionnaires. Stress is a broad concept that can be divided into stressors and stress responses24. Following this fundamental division, the model presented by the National Institute for Occupational Safety and Health posits that occupational stressors, such as excessive workload and interpersonal conflict, trigger stress responses and ultimately result in mental health problems5. Generally, the stress response triggers the activation of the hypothalamic–pituitary–adrenal (HPA) axis and autonomic nervous system as adaptive reactions to the encountered stressors during the acute phase. Subsequently, the immune system is activated but becomes dysregulated under chronic stress exposure25. Recent advancements in identifying biological markers of stress responses have highlighted salivary interleukin-6 (IL-6) as a suitable non-invasive biological marker for stress responses26. Furthermore, various psychiatric disorders, including depression, are associated with alterations in cytokine levels27. While chronic inflammation is a common mechanism in various mental and physical illnesses, an increase in cytokine levels (such as IL-6) can induce neuroinflammation in the brain, ultimately leading to depression28, although the clinical definition of chronic inflammation and the threshold of cytokine increases have not yet been established.
Stress responses, including the activation of the HPA axis, autonomic nervous system, and immune system, cause major changes in the levels of glutamate, serotonin, and orexin29,30. From the perspective of sleep–wake cycles, these neurotransmitters, particularly those in the orexin system, play a critical role in maintaining wakefulness, which is beneficial for coping with encountered stressors. The multilevel effects of stress responses, including the activation of the aforementioned systems, on the arousal system have been suggested31,32. Furthermore, these neurotransmitters contribute to the development of sleep architecture in general33. Conversely, inflammation-induced alterations in various neurotransmitters may cause modifications in sleep architecture30,33. Thus, measuring IL-6 levels may be beneficial for identifying the risk of sleep disturbances. Along with individual vulnerability, including severe social factors, sleep disturbances can contribute to the development of occupational stress-related mental health problems, such as adjustment disorders and depression.
Therefore, in the present study, we focused on stressed workers with the aim of uncovering the relationship between sleep quality, assessed in natural sleep settings using an Apple Watch, and levels of IL-6, which serves as a biological marker for stress responses. The aim is in line with the clinical meaning of sleep disturbance in the occupational settings, i.e. a great risk of occupational stress-related mental health problems. While various factors collectively contribute sIL-6 elevation itself, they were not the focus of this paper directly.
Methods
Ethical approval
This prospective observational study was conducted at the Keio University School of Medicine in accordance with the ethical guidelines of the Declaration of Helsinki. This study was approved by the ethics committee of the Keio University School of Medicine (2021–1031- 4) and has been registered at UMIN (UMIN000045528), named “A survey for Japanese Office workers to Assess Stress Issues and Sleep problems (J-OASIS)”. All participants provided written informed consent prior to participation.
Participants
Participants were recruited through a web-based patient recruitment company (3H medi solution: https://global-3h.com/). In the present study, our main focus was occupation-related psychological stress, and we specifically recruited office workers to minimize heterogeneity in the working environment. Furthermore, we exclusively recruited high-stress workers for our study, as our primary research objective was to explore the relationship between sleep and stress in this population, who are at a higher risk of developing insomnia34. The inclusion criteria were: (1) aged 20–65 years and full-time workers; (2) Individuals who provided written informed consent; and (3) Individuals who could easily attend the research interviews; and (4) Those who experienced high levels of occupation-related stress. The high-stress workers were identified in accordance with the job demand-control model of occupational stress35. Participants were first screened using the following two factors from the Brief Job Stress Questionnaire (BJSQ)36: job demand and job control. Workers with a severity higher than the average of the Japanese population in both scores (2.14 for job demand and 2.53 for job control37) were identified as high-stress workers. The exclusion criteria were: (1) Workers on leave; (2) Workers working night shifts (10 pm—5 am); (3) Workers who are directly engaged in manufacturing processes/fieldwork, such as manufacturing, construction, restaurants, mining, agriculture, forestry, and fishing; (4) Workers with any psychiatric history and/or psychiatric illnesses; (5) Workers currently taking psychotropic drugs; (6) Workers experiencing difficulty wearing an Apple Watch correctly and consistently over a given time period; and (7) The principal investigators/members of this research project were considered ineligible to participate in this study.
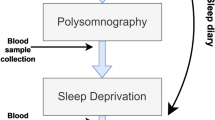
Procedure
Questionnaires
The following questionnaires were used: BJSQ36, Job Contents Questionnaire (JCQ)37, Dutch Work Addiction Scale (DUWAS)38, WHO-Health and Work Performance Questionnaire Short Form (WHO-HPQ-SF)39, Pittsburgh Sleep Quality Index (PSQI)40, Epworth Sleepiness Scale (ESS)41, Quick Inventory of Depressive Symptomatology (QIDS)42, Multidimensional Assessment of Interoceptive Awareness (MAIA)43, Mindful Attention Awareness Scale (MAAS)44, and the Satisfaction With Life Scale (SWLS)45.
In addition, the characteristics of the participants were assessed via self-report. The following items were asked and grouped for our analysis based on the meaning of each item and the number of participants falling into each category. As general information, we asked about age, sex, educational years, height and weight (for calculating body mass index), marriage status (married/common-law marriage or unmarried/divorced/bereaved), and home environment (living alone, with spouse, with spouse and children, with partner, multi-generational). Regarding lifestyle, we inquired about the frequency of exercise (not at all, once a month, once a week, several times a week, and almost every day), frequency of meals (one to two meals/day or three meals/day), frequency of eating snacks (not at all-rarely, once a day, several times a day), frequency of eating vegetables (not at all-rarely, sometimes, once a day, every meal), frequency of drinking alcohol (no drinking, less than once a month, 2–4 times a month, 2–3 times a week, 4 or more times a week), smoking status (smoker or non-smoker), caffein consumption before sleep or not (defined as drinking coffee or tea within 4 h before sleep), time spent using any devices for personal use (not at all/very little, 1 h a day or less, 1–2 h a day, 3–4 h a day, more than 1 h a day), time spent playing games (not at all/very little, 1 h a day or less, 1–2 h a day, 3–4 h a day, more than 1 h a day), use of LED in bedrooms or not, taking a bath or not, and bath time (minutes). As for working style, we asked about job category (technical work, clerical work, system engineering, sales, and others), job position (manager level or not), years of employment, years of current employment, working hours/day, time spent using computers (hours/day), rest time (hours/day), days of working (days/week), days of commuting (days/week), commuting time (minutes), previous leave of absence or not, and telework (≥ 1 time/week or not) were asked. Furthermore, participants were asked to assess their daily work stress using a visual analogue scale and to record their sleep and awake time as a daily record during the research period. Subjective daily work stress was estimated as the average of their daily stress assessment. Social jetlag was estimated based on the difference in the average midsleep times between workdays and holidays46.
Saliva samples
Saliva was collected to assess the validity of IL-6 and secretory immunoglobulin A (sIgA) as markers of the immunological stress response with less daily variation than other markers, such as cortisol and amylase47,48,49. Saliva was deposited into the test tubes using a straw and immediately stored in a freezer. While frozen, the samples were transported to LSI Medience Inc. and tested for saliva components. Saliva collection was conducted once before the week of sleep stage estimation.
Sleep stage estimation using an Apple Watch
Participants were instructed to wear an Apple Watch Series 6 during their sleep to evaluate sleep quality during the week. They provided simple daily recordings, including subjective bedtime and wake-up times, working hours, and their perception of occupational stress on each day using a visual analog scale. Using our specific algorithm based only heart rate, which has previously been validated22,23, the actual duration of each sleep stage, that is, non-REM sleep (sleep stage 1–3), REM sleep, the nocturnal awakening time, and total sleep time were estimated. The estimation was conducted on a laboratory personal computer after the completion of one week of recording, and the average duration of each sleep stage, nocturnal awakening time, and total sleep time per day was calculated.
The proposed method classifies sleep time into five stages (non-REM sleep (sleep stage 1–3), REM sleep, and the nocturnal awakening time), irrespective of the type of monitoring device used, as long as the heart rate and heart rate variability are accurately recorded. In this approach, real-time display of heart rate data was not implemented. Instead, we adopted an offline analysis method in which the acquired heart rate data were processed daily. The key features of this approach included: (1) Device Flexibility: The proposed method is effective for various types of heart rate monitoring devices, ensuring data reliability and consistency. This flexibility enables researchers and healthcare professionals to work with different hardware while maintaining their ability to classify sleep stages; (2) Offline Analysis: The Offline analysis of acquired heart rate data enhances data accuracy and reliability. Offline analysis allows data validation, noise filtering, and precise results; and (3) Daily analysis: Analyzing heart rate data on a daily basis offers detailed insights into sleep patterns. This enables a better understanding of sleep quality and its variations, potentially allowing for adjustments and interventions as needed.
Statistical analysis
The duration of N3 sleep was set as a primary outcome. First, to determine the association between N3 duration and patient information, including questionnaire scores and immunological stress markers, Welch’s t-test or analysis of variance was performed when the variables of interest were qualitative variables. Pearson or Spearman’s correlation analysis was employed when the variables were quantitative. In this step, factors with a P-value < 0.1 were considered to be potentially associated with N3 duration. Subsequently, a multivariable general linear model was conducted with N3 duration as the dependent variable and potential factors as independent variables. As the distribution of IL-6 was heavily skewed to the right, it was used in the multivariable analysis after logarithmic transformation. The total sleep time measured using the Apple Watch22,23 was included in the multivariable analysis instead of sleep duration assessed using the PSQI because it is much more accurate. As an additional validation technique, correlation analyses were conducted between the level of IL-6 and each sleep stage, as well as between the ESS scores and each sleep stage. Furthermore, the fragmentation of N3 was estimated to assess its alteration. Statistical significance was set at P < 0.05. Statistical analyses were performed using R (4.1.3 or later).
Results
Characteristics of the participants
In total, 130 participants were initially recruited (Fig. 1). However, during the initial stage of this research, we encountered technical problems that prevented the collection of sleep data from 44 participants via the Apple Watch. Because we assessed twenty participants using twenty Apple Watches concurrently, many participants were affected by this initial technical issue. Additionally, one participant withdrew their consent. After addressing these problems by improving the settings of the Apple Watch and the instructions for wearing it, we collected data from 85 participants. Unfortunately, 12 out of 85 data points were of insufficient quality to estimate the sleep stage. A sleep consultant (R.S.) made this judgment based on data generated by the hypnogram.
Finally, data of 73 participants (mean ± standard deviation [SD] age: 41.9 ± 10.4 years old, male/female: 35/38) were analyzed. As per our inclusion criteria, they reported high occupational stress as assessed by the BJSQ, including greater job demand (mean ± SD: 1.64 ± 0.50) and smaller job control (mean ± SD: 2.16 ± 0.52). These stress levels were more severe than the national average (2.14 in job demand and 2.53 in job control)29, affirming the validity of our recruitment process based on the established inclusion criteria. The majority of the participants (95.9%) worked 5 days per week for an average of 8.9 ± 1.5 h per day. Some participants (17.8%) reported telework on one or more days per week. Regarding saliva samples, the median (interquartile range) levels of IL-6 and sIgA were 4.5 (8.7) pg/ml and 163 (96) μg/ml, respectively. Their sleep architecture was estimated as follows: N1, 31.1 ± 11.2 min (9.0%): N2, 66.6 ± 44.4 min (18.2%): N3, 86.4 ± 32.7 min (24.0%): REM, 102.6 ± 32.1 min (28.9%), awaking time, 71.1 ± 35.9 min (19.9%): and total sleep time: 357.9 ± 100.9 min. As for the fragmentation of stage N3 sleep, a count of 9.8 ± 3.2 fragments per night was observed.
Factors associated with the duration of N3 sleep
The results of the analysis exploring potential factors are shown in Table 1. The following factors were identified as potential factors associated with shorter N3 sleep durations: greater IL-6 levels (rho = − 0.282, p = 0.016), shorter sleep durations assessed by the PSQI (where a higher score indicates shorter sleep durations) (rho = − 0.296, p = 0.011), greater daytime sleepiness as assessed by the ESS (r = − 0.263, p = 0.025), anger irritability as assessed by the BJSQ (r = 0.226, p = 0.055), and noticing (a subscale in MAIA) (r = 0.205, p = 0.081).
Our multivariable analysis (Table 2, Fig. 2) revealed that shorter N3 durations were significantly associated with a greater level of IL-6 (log transformation) (β = − 7.555, p = 0.005) and greater daytime sleepiness as assessed by the ESS (β = − 2.208, p = 0.002), after controlling for total sleep time.
Association between IL-6, daytime sleepiness, and each sleep stage
IL-6 levels were not associated with any other sleep stages besides N3; specifically, not with N1 (r = − 0.054, p = 0.652), N2 (r = − 0.042, p = 0.724), REM (r = 0.051, p = 0.668), nocturnal awakening (r = 0.091, p = 0.442), or total sleep time (r = − 0.242, p = 0.917). Furthermore, daytime sleepiness, as assessed using the ESS, was not associated with any other sleep stage besides N3, that is, N1 (r = − 0.202, p = 0.087), N2 (r = − 0.082, p = 0.488), REM (r = 0.053, p = 0.656), awake (r = 0.144, p = 0.225), or total sleep time (r = − 0.109, p = 0.357).
Discussion
To the best of our knowledge, this is the first study to investigate sleep quality (duration of N3 sleep) in a natural sleep setting among stressed workers using an Apple Watch. Our cross-sectional data cannot disentangle a bidirectional relationship and a vicious circle, while IL-6 was measured before sleep estimation. However, we believe it is noteworthy that our findings revealed a significant association between sleep quality and the immunological stress response, as assessed by IL-6 levels. In addition, sleep quality significantly correlated with daytime sleepiness, emphasizing the importance of N3 sleep. The absence of correlations between other sleep stages and total sleep time further highlights the significance of the total N3 sleep time. The average estimated N3 time in our study was comparable to the PSG-measured N3 time in the general population21, validating our research methods. This also suggests the existence of varying levels of sleep quality, even among stressed workers. Nocturnal awakenings and repetitive interruptions of N3 sleep also characterize alterations in sleep architecture.
Daytime sleepiness was predicted by the N3 sleep duration, but not by other sleep stages. These findings support the current consensus that N3 sleep underlies multiple restorative functions of sleep16,50, including memory consolidation, energy restoration, hormone release and regulation, immune functions, and metabolite clearance from the brain. Our findings are also compatible with those of previous studies that demonstrated a significant causal link between the enhancement of N3 sleep facilitated by specific drugs and a reduction in daytime sleepiness in both healthy subjects with sleep deprivation51,52 and patients with Parkinson’s disease53. While our research was cross-sectional, our findings provide additional evidence of the potential causality between a shorter duration of N3 sleep and a greater level of daytime sleepiness in stressed workers in a natural setting. Daytime sleepiness has previously been shown to have a detrimental effect on task performance54, underscoring the importance of addressing sleepiness for all individuals in the workplace and necessitating improvements in the factors influencing N3 reduction. In our non-clinical sample, N3 time, rather than total sleep time, was associated with daytime sleepiness. This finding contradicts studies in clinical samples, where a correlation between total sleep time and daytime sleepiness has been observed55,56. Our findings suggest that, in a non-clinical population, sleep quality, as indicated by the N3 time, plays a more significant role in daytime sleepiness. This finding implies that maintaining adequate N3 sleep may be crucial for preventing the progression to clinical conditions.
The significant association between IL-6 and N3 levels implies that elevated IL-6 levels may disrupt N3 sleep in stressed workers. This disruption could be underpinned by glutamatergic system dysfunction, which plays a pivotal role in the transition from light NREM to deep NREM (i.e., N3 sleep)33. The dysfunction of this system can be induced by inflammatory mechanisms in major depression and suicidal ideation20, suggesting the pathological role of inflammation in sleep disturbances. Sleep and arousal circuits consist of glutamatergic and GABAergic neurons, which are modulated by neuromodulatory systems comprising various neurotransmitters such as dopamine, serotonin, noradrenaline, acetylcholine, histamine, orexin, and melatonin-concentrating hormone neurons33. Ketamine, a drug that selectively acts on the glutamatergic system, has been shown to increase the N3 sleep time57. In contrast, a specific substance or molecule, including IL-6, can shorten N3 sleep. A study involving the subcutaneous injection of IL-6 or a placebo in healthy men showed that IL-6 injection shortened N3 in the first half of sleep when N3 was predominantly observed58. This suggests that proinflammatory cytokines can disrupt the N3 mechanism. In addition, nocturnal awakenings and repetitive interruptions of N3 sleep further underscore alterations in the sleep–wake cycle. These cycles operate based on the actions of various neurotransmitters, among which orexin plays a central role in switching between the sleep and wake states. Thus, inflammation-induced activation of arousal mechanisms may contribute to nocturnal awakening and the repetitive interruption of N3 sleep32,59.
In more detailed molecular mechanisms, pro-inflammatory cytokines, including IL-6, activate the kynurenine pathway and decrease tetrahydrobiopterin (BH4) bioavailability. This causes major changes in the metabolism of glutamate, serotonin, melatonin, and dopamine, ultimately leading to sleep disturbances and further contributing to depression. Under inflammatory conditions, activation of glial cells and the subsequent alteration of the kynurenine pathway leads to an increase in quinolinic acid, which has neurotoxic effects, whereas the synthesis of neuroprotective kynurenic acid is reduced28,60,61,62. It has been demonstrated that these alterations are associated with sleep disturbances in depression60. BH4 is a key cofactor for the optimal functioning of certain enzymes, including those associated with dopamine and serotonin synthesis. Under inflammatory conditions, the altered bioavailability of BH4 results in a reduced capacity for the synthesis of such neurotransmitters. Several studies have suggested impaired BH4 metabolism in patients with depression (for a review, see29). There is a known crosstalk between the kynurenine and BH4 pathways29,63. Furthermore, the relationship between orexins and inflammation remains unclear. Studies on delirium, which is characterized by severe sleep disturbances along with abnormal behaviors, have indicated that inflammation may disrupt the sleep–wake cycle, wherein the activation of the awakening system, including the orexin system, may contribute to its pathogenesis30,59. Other studies have suggested that orexins, especially orexin A, could have a protective role against neuroinflammation64,65. These studies suggest a complex molecular relationship between orexin and neuroinflammation, suggesting that an appropriate level of orexin is crucial for regulating neuroinflammation. Further studies are required to elucidate this relationship, particularly under conditions of chronic stress66.
The relationship between IL-6 levels and sleep quality may also affect each other. As mentioned earlier, triggering inflammation can disrupt sleep quality, but it is worth noting that sleep deprivation can also increase inflammation, including the levels of IL-667. In this study, it was challenging to determine whether IL-6 expression was induced by occupational stress or insomnia as a mutual interaction between the two exists, creating a vicious circle. Occupational stress induces insomnia, and in turn, insomnia can lead to increased levels of subjectively reported occupational stress34. This is caused by dysregulation of the stress response, emotional instability, and cognitive dysfunction68. Therefore, the relationship between IL-6, occupational stress, and sleep quality is complex in real-world scenarios and can contribute to a vicious cycle. Comprehensive stress and sleep management may be beneficial for the prevention of occupational-related mental health problems.
One strength of this study lies in the sophisticated assessment of sleep quality, which goes beyond merely evaluating total sleep time. Moreover, the study is conducted in a more natural sleep setting than monitoring by PSG. These findings outside the experimental room may have broader applicability to the general population. Furthermore, our assessment using the Apple Watch enabled a greater number of participants compared to PSG, given its lower costs, greater accessibility, and less reliance on device availability. Another strength is the objective assessment of the stress response through immunological measures, which is less susceptible to bias than self-reporting and provides more direct evidence of the stress response. However, this study has a few limitations. First, given the cross-sectional design of the study, we could not infer the causal direction from the statistical associations, which limits our directional interpretation. Second, we did not assess other stress responses, such as cortisol levels, in the present study. This makes it impossible to validate our finding using other stress markers. Third, although no association was found between BMI and N3 time, we did not assess sleep apnea, which is a potential confounder that could affect our findings. Fourth, recording failures occurred for many participants during the initial stages of the research. Since the decision on which subjects to initially enroll was not artificially determined, this would not significantly bias the results. Fifth, while our study focused on stressed workers to enhance the sensitivity in detecting abnormalities, we could not provide any evidence for less stressed workers. Sixth, IL-6 levels can be influenced by acute stress, such as injury and infection, even if minor. This influence has not been controlled, potentially affecting our findings. Thus, further studies are required to address these limitations.
Conclusion
Our finding that a higher immunological stress response was associated with poor sleep quality, defined by a shorter N3 time, enhances our understanding of insomnia in stressed workers and emphasizes the importance of stress management for such individuals. We believe that our findings will contribute to the development of strategies for managing stressed workers and exploring innovative treatment targets.
Data availability
The datasets generated during the current study will be made available by the corresponding author upon reasonable request and are subject to regulatory approval.
References
Chung, J. et al. The Association between occupational stress level and health-related productivity loss among Korean employees. Epidemiol. Health. https://doi.org/10.4178/epih.e2023009 (2022).
Dewa, C. S., Loong, D., Bonato, S. & Hees, H. Incidence rates of sickness absence related to mental disorders: A systematic literature review. BMC Public Health 14, 205. https://doi.org/10.1186/1471-2458-14-205 (2014).
Jensen, I., Arapovic-Johansson, Z. & Aboagye, E. The cost-effectiveness analysis of the productivity measurement and enhancement system intervention to reduce employee work-related stress and enhance work performance. Int. J. Environ. Res. Public Health. 19(4), 2431. https://doi.org/10.3390/ijerph19042431 (2022).
Ministry of health, lobour and welfare. The report of occupational safety and health [Roudou-anzen-eisei-tyousa] 2022. https://www.mhlw.go.jp/toukei/list/dl/r03-46-50_gaikyo.pdf
Hurrell, J. J. Jr. & McLaney, M. A. Exposure to job stress—A new psychometric instrument. Scand. J. Work. Environ. Health. 14(Suppl 1), 27–28 (1988).
Ministry of health, lobour and welfare. The document for authorizing worker’s compensation for mental disorders. The report of occupational safety and health [Seishinsyougai-no-rousainintei] 2024. https://www.mhlw.go.jp/content/001168576.pdf
Tanaka, M. et al. Measurement of work-related psychological injury with depressive symptoms. BMC Psychiatry. 23(1), 681. https://doi.org/10.1186/s12888-023-05178-w (2023).
Yang, B. et al. Association between insomnia and job stress: A meta-analysis. Sleep Breath. 22(4), 1221–1231. https://doi.org/10.1007/s11325-018-1682-y (2018).
Madsen, I. E. H. et al. Job strain as a risk factor for clinical depression: Systematic review and meta-analysis with additional individual participant data. Psychol. Med. 47(8), 1342–1356. https://doi.org/10.1017/S003329171600355X (2017).
Yamauchi, T., Sasaki, T., Yoshikawa, T., Matsumoto, S. & Takahashi, M. Incidence of overwork-related mental disorders and suicide in Japan. Occup. Med. (Lond). 68(6), 370–377. https://doi.org/10.1093/occmed/kqy080 (2018).
Kalmbach, D. A., Anderson, J. R. & Drake, C. L. The impact of stress on sleep: Pathogenic sleep reactivity as a vulnerability to insomnia and circadian disorders. J. Sleep Res. 27(6), e12710. https://doi.org/10.1111/jsr.12710 (2018).
Doherty, A. M., Lorenz, L., Jabbar, F., O’Leary, E. & Casey, P. Sleep disturbance in adjustment disorder and depressive episode. Int. J. Environ. Res. Public Health. 16(6), 1083. https://doi.org/10.3390/ijerph16061083 (2019).
Ekstedt, M. et al. Disturbed sleep and fatigue in occupational burnout. Scand. J. Work. Environ. Health. 32(2), 121–131. https://doi.org/10.5271/sjweh.987 (2006).
Riemann, D., Krone, L. B., Wulff, K. & Nissen, C. Sleep, insomnia, and depression. Neuropsychopharmacology. 45(1), 74–89. https://doi.org/10.1038/s41386-019-0411-y (2020).
American Academy of Sleep Medicine. The AASM manual for the scoring of sleep and associated events: Roles, terminology and technical specifications. Westchester, IL, 2007.
Baglioni, C. et al. Sleep changes in the disorder of insomnia: A meta-analysis of polysomnographic studies. Sleep Med Rev. 18(3), 195–213. https://doi.org/10.1016/j.smrv.2013.04.001 (2014).
Baril, A. A. et al. Slow-wave sleep and MRI markers of brain aging in a community-based sample. Neurology. 96(10), e1462–e1469. https://doi.org/10.1212/WNL.0000000000011377 (2021).
Hein, M., Lanquart, J. P., Loas, G., Hubain, P. & Linkowski, P. Similar polysomnographic pattern in primary insomnia and major depression with objective insomnia: A sign of common pathophysiology?. BMC Psychiatry. 17(1), 273. https://doi.org/10.1186/s12888-017-1438-4 (2017).
Pillai, V., Kalmbach, D. A. & Ciesla, J. A. A meta-analysis of electroencephalographic sleep in depression: Evidence for genetic biomarkers. Biol. Psychiatry 70(10), 912–919. https://doi.org/10.1016/j.biopsych.2011.07.016 (2011).
Zeoli, I. et al. Polysomnographic markers of suicidal ideation in untreated unipolar major depressed individuals. Int. J. Psychophysiol. 166, 19–24. https://doi.org/10.1016/j.ijpsycho.2021.05.001 (2021).
Boulos, M. I. et al. Normal polysomnography parameters in healthy adults: A systematic review and meta-analysis. Lancet. Respir. Med. 7(6), 533–543. https://doi.org/10.1016/S2213-2600(19)30057-8 (2019).
Mitsukura, Y., Fukunaga, K., Yasui, M. & Mimura, M. Sleep stage detection using only heart rate. Health Inform. J. 26(1), 376–387 (2020).
Mitsukura, Y., Sumali, B., Nagura, M., Fukunaga, K. & Yasui, M. Sleep stage estimation from bed leg ballistocardiogram sensors. Sensors 20(19), 5688 (2020).
Selye, H. The Story of the Adaption Syndrome (ACTA INC., Medical Publisher, 1952).
Sanada, K. et al. Effects of mindfulness-based interventions on biomarkers and low-grade inflammation in patients with psychiatric disorders: A meta-analytic review. Int. J. Mol. Sci. 21(7), 2484. https://doi.org/10.3390/ijms21072484 (2020).
Shah, K., Kumari, R. & Jain, M. Unveiling stress markers: A systematic review investigating psychological stress biomarkers. Dev. Psychobiol. 66(5), e22490. https://doi.org/10.1002/dev.22490 (2024).
Himmerich, H., Patsalos, O., Lichtblau, N., Ibrahim, M. A. A. & Dalton, B. Cytokine research in depression: Principles, challenges, and open questions. Front. Psychiatry. 10, 30. https://doi.org/10.3389/fpsyt.2019.00030 (2019).
Hassamal, S. Chronic stress, neuroinflammation, and depression: An overview of pathophysiological mechanisms and emerging anti-inflammatories. Front. Psychiatry. 14, 1130989. https://doi.org/10.3389/fpsyt.2023.1130989 (2023).
Vancassel, S., Capuron, L. & Castanon, N. Brain kynurenine and BH4 pathways: Relevance to the pathophysiology and treatment of inflammation-driven depressive symptoms. Front. Neurosci. 12, 499. https://doi.org/10.3389/fnins.2018.00499 (2018).
Wilson, J. E. et al. Delirium. Nat. Rev. Dis. Primers. 6(1), 90. https://doi.org/10.1038/s41572-020-00223-4 (2020).
Grafe, L. A. & Bhatnagar, S. Orexins and stress. Front. Neuroendocrinol. 51, 132–145. https://doi.org/10.1016/j.yfrne.2018.06.003 (2018).
Hamasaki, M. Y. et al. Neuropeptides in the brain defense against distant organ damage. J. Neuroimmunol. 290, 33–35. https://doi.org/10.1016/j.jneuroim.2015.11.014 (2016).
Jones, B. E. Arousal and sleep circuits. Neuropsychopharmacology. 45(1), 6–20. https://doi.org/10.1038/s41386-019-0444-2 (2020).
Garefelt, J. et al. Reciprocal relations between work stress and insomnia symptoms: A prospective study. J. Sleep Res. 29(2), e12949. https://doi.org/10.1111/jsr.12949 (2020).
Karasek, R. A. Jr. Job demands, job decision latitude, and mental strain: Implications for job redesign. Adm. Sci. Quart. 24, 285–308 (1979).
Shimomitsu T, Haratani T, Nakamura K, Kawakami N, Hayashi T, Hiro H, Arai M, Miyazaki S, Furuki K, Ohya Y, Odagiri Y. Final development of the Brief Job Stress Questionnaire mainly used for assessment of the individuals. The Ministry of Labor sponsored grant for the prevention of work-related illness, FY 1999 report, Kato M(Ed.) 2000; 126–64, Tokyo Medical University, Tokyo (in Japanese).
Kawakami, N. Investigation of penetration methods for the primary prevention of workers’ mental health problems. Ministry of health, lobour and welfare. 2012. https://mental.m.u-tokyo.ac.jp/old/NBJSQ/001.pdf. (in Japanese).
Borges, E., Sequeira, C., Martins, T., Queirós, C. & Mosteiro-Díaz, M. P. Psychometric properties of the Portuguese Dutch Work Addiction Scale. Rev. Esc. Enferm. USP. 55, e03765. https://doi.org/10.1590/S1980-220X2020029603765 (2021).
Kessler, R. C. et al. The world health organization health and work performance questionnaire (HPQ). J. Occupat. Environ. Med. 45(2), 156–174 (2003).
Buysse, D. J., Reynolds, C. F., Monk, T. H., Berman, S. R. & Kupfer, D. J. The Pittsburgh Sleep Quality Index (PSQI): A new instrument for psychiatric research and practice. Psychiatry Res. 28, 193–213 (1989).
Johns, M. W. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep. 14(6), 540–545. https://doi.org/10.1093/sleep/14.6.540 (1991).
Rush, A. J. et al. The 16-item quick inventory of depressive symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biol. Psychiatry. 54(5), 573–583. https://doi.org/10.1016/s0006-3223(02)01866-8 (2003).
Mehling, W. E. et al. The multidimensional assessment of interoceptive awareness (MAIA). PLoS One. 7(11), e48230. https://doi.org/10.1371/journal.pone.0048230 (2012).
Brown, K. W. & Ryan, R. M. The benefits of being present: Mindfulness and its role in psychological well-being. J. Pers. Soc. Psychol 84(4), 822–848 (2003).
Diener, E., Emmons, R. A., Larsen, R. J. & Griffin, S. The satisfaction with life scale. J. Pers. Assess. 49(1), 71–75. https://doi.org/10.1207/s15327752jpa4901_13 (1985).
Taillard, J., Sagaspe, P., Philip, P. & Bioulac, S. Sleep timing, chronotype and social jetlag: Impact on cognitive abilities and psychiatric disorders. Biochem. Pharmacol. 191, 114438. https://doi.org/10.1016/j.bcp.2021.114438 (2021).
Izawa, S., Miki, K., Liu, X. & Ogawa, N. The diurnal patterns of salivary interleukin-6 and C-reactive protein in healthy young adults. Brain Behav. Immun. 27(1), 38–41. https://doi.org/10.1016/j.bbi.2012.07.001 (2013).
Okamura, H. et al. Short sleeping time and psychobiological responses to acute stress. Int. J. Psychophysiol. 78(3), 209–214. https://doi.org/10.1016/j.ijpsycho.2010.07.010 (2010).
Gallagher, S. et al. Caregiving is associated with low secretion rates of immunoglobulin A in saliva. Brain Behav. Immun. 22(4), 565–572. https://doi.org/10.1016/j.bbi.2007.11.007 (2008).
Léger, D. et al. Slow-wave sleep: From the cell to the clinic. Sleep Med. Rev. 41, 113–132. https://doi.org/10.1016/j.smrv.2018.01.008 (2018).
Walsh, J. K. et al. Slow wave sleep enhancement with gaboxadol reduces daytime sleepiness during sleep restriction. Sleep. 31(5), 659–672. https://doi.org/10.1093/sleep/31.5.659 (2008).
Walsh, J. K. et al. Enhancing slow wave sleep with sodium oxybate reduces the behavioral and physiological impact of sleep loss. Sleep. 33(9), 1217–1225. https://doi.org/10.1093/sleep/33.9.1217 (2010).
Büchele, F. et al. Sodium oxybate for excessive daytime sleepiness and sleep disturbance in parkinson disease: A randomized clinical trial. JAMA Neurol. 75(1), 114–118. https://doi.org/10.1001/jamaneurol.2017.3171 (2018).
Edinger, J. D., Bathgate, C. J., Tsai, S. & Khassawneh, B. Impact of daytime sleepiness and insomnia on simple and complex cognitive task performances. Sleep Med. 87, 46–55. https://doi.org/10.1016/j.sleep.2021.08.004 (2021).
Olson, L. G., Cole, M. F. & Ambrogetti, A. Correlations among Epworth Sleepiness Scale scores, multiple sleep latency tests and psychological symptoms. J. Sleep Res. 7(4), 248–253. https://doi.org/10.1046/j.1365-2869.1998.00123.x (1998).
Kelly, M. R. et al. Actigraphy prior to multiple sleep latency test: Nighttime total sleep time predicts sleep-onset latency. J. Clin. Sleep Med. 18(1), 161–170. https://doi.org/10.5664/jcsm.9528 (2022).
Kwaśny, A., Włodarczyk, A., Ogonowski, D. & Cubała, W. J. Effect of ketamine on sleep in treatment-resistant depression: A systematic review. Pharmaceuticals (Basel). 16(4), 568. https://doi.org/10.3390/ph16040568 (2023).
Späth-Schwalbe, E. et al. Acute effects of recombinant human interleukin-6 on endocrine and central nervous sleep functions in healthy men. J. Clin. Endocrinol. Metab. 83(5), 1573–1579. https://doi.org/10.1210/jcem.83.5.4795 (1998).
Hatta, K. et al. Preventive effects of suvorexant on delirium: A randomized placebo-controlled trial. J. Clin. Psychiatry. 78(8), 970–979. https://doi.org/10.4088/JCP.16m11194 (2017).
Cho, H. J. et al. Sleep disturbance and kynurenine metabolism in depression. J. Psychosom. Res. 99, 1–7. https://doi.org/10.1016/j.jpsychores.2017.05.016 (2017).
Erabi, H. et al. Kynurenic acid is a potential overlapped biomarker between diagnosis and treatment response for depression from metabolome analysis. Sci. Rep. 10, 16822. https://doi.org/10.1038/s41598-020-73918-z (2020).
Bay-Richter, C. et al. A role for inflammatory metabolites as modulators of the glutamate N-methyl-D-aspartate receptor in depression and suicidality. Brain Behav. Immun. 43, 110–117. https://doi.org/10.1016/j.bbi.2014.07.012 (2015).
Staats Pires, A., Tan, V. X., Heng, B., Guillemin, G. J. & Latini, A. Kynurenine and tetrahydrobiopterin pathways crosstalk in pain hypersensitivity. Front. Neurosci. 14, 620. https://doi.org/10.3389/fnins.2020.00620 (2020).
Couvineau, A. et al. Orexins as novel therapeutic targets in inflammatory and neurodegenerative diseases. Front. Endocrinol. (Lausanne). 10, 709. https://doi.org/10.3389/fendo.2019.00709 (2019).
Ishioh, M., Nozu, T. & Okumura, T. Brain neuropeptides, neuroinflammation, and irritable bowel syndrome. Digestion. https://doi.org/10.1159/000533275 (2023).
Sargin, D. The role of the orexin system in stress response. Neuropharmacology. 154, 68–78. https://doi.org/10.1016/j.neuropharm.2018.09.034 (2019).
Thompson, K. I. et al. Acute sleep deprivation disrupts emotion, cognition, inflammation, and cortisol in young healthy adults. Front. Behav. Neurosci. 16, 945661. https://doi.org/10.3389/fnbeh.2022.945661 (2022).
Palagini, L., Hertenstein, E., Riemann, D. & Nissen, C. Sleep, insomnia and mental health. J. Sleep Res. 31(4), e13628. https://doi.org/10.1111/jsr.13628 (2022).
Acknowledgements
We are grateful to 3H medi solution and LSI Medience Inc. for their support of the current study. We would also like to express our gratitude to all the staff who supported our research.
Funding
This research was funded by Eisai Co., Ltd.
Author information
Authors and Affiliations
Contributions
A.K., M.S., Y.M., H.T., A.K., A.N., H.M., A.F., K.I., and M.M. designed the study. A.K., Y.K., A.K., M.U., and S.U. collected data. A.K., Y.M., and H.T. analyzed the data. The R.S. judged data quality and provided professional suggestions. M.S., H.M., and M.M. developed the experimental environment. A.K. and M.S. wrote the first draft. A.F. and K.I. critically reviewed the manuscript, and all co-authors approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
MS has received honoraria from Takeda Pharmaceutical Company Ltd., Kyowa Kirin Co., Viatris Inc., Shionogi & Co., Ltd., Meiji Seika Pharma, Yoshitomiyakuhin Corporation, and Mochida Pharmaceutical outside of the submitted work. MM has received speaker’s honoraria from Biogen Japan, Byer Pharmaceutical, Daiichi Sankyo, Dainippon-Sumitomo Pharma, Demant Japan, Eisai, Eli Lilly, Fuji Film RI Pharma, Hisamitsu Pharmaceutical, H.U. Frontier, Janssen Pharmaceutical, Mochida Pharmaceutical, MSD, Mylan EPD, Nippon Chemipher, Novartis Pharma, Ono Yakuhin, Otsuka Pharmaceutical, Pfizer, Shionogi, Takeda Yakuhin, Teijin Pharma, and Viatris within the past two years. Also, he received grants from Daiichi Sankyo, Eisai, Fronteo, Shionogi, Takeda, Tanabe Mitsubishi and Tsumura within the past three years outside the submitted work. AF and KI are employees of Eisai Co., Ltd. This study was partly supported by Joint Research Grant from Eisai Co., Ltd. All other remaining authors have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Koreki, A., Sado, M., Mitsukura, Y. et al. The association between salivary IL-6 and poor sleep quality assessed using Apple watches in stressed workers in Japan. Sci Rep 14, 22620 (2024). https://doi.org/10.1038/s41598-024-70834-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-70834-4
- Springer Nature Limited