Abstract
Limited data on the correlation between the perineal body (PB) and stress urinary incontinence (SUI) are available. The objectives of this study were to quantify the PB using shear wave elastography (SWE) technology with a high-frequency linear array probe to evaluate the relationship between the properties of PB and stress urinary incontinence (SUI). This study included 64 women with SUI and 70 female control participants. The length, height, perimeter, and area of PB in all participants were calculated using transperineal ultrasound, and the elasticity of PB was assessed by SWE at rest and during the maximal Valsalva maneuver, respectively. In addition, the comparison of PB parameters between the patients with SUI and the healthy participants was conducted. The transperineal ultrasound and SWE examination was performed in 134 participants, and the elastic modulus values were significantly increased from participants at rest to those during the maximal Valsalva maneuver in all participants (Emax: 35.59 versus 53.13 kPa, P < 0.001; and Emean: 26.97 versus 40.25 kPa, P < 0.001). Emax and Emean of PB exhibited significant differences during the maximal Valsalva maneuver between the SUI group and the control group (47.73 versus 58.06 kPa, P < 0.001; and 35.78 versus 44.33 kPa, P < 0.001) and had a negative correlation with SUI. The BMI and PB height during the maximal Valsalva maneuver in the SUI group were found to be significantly higher than that in healthy volunteers. Emax and Emean of PB negatively correlated with BMI during the maximal Valsalva maneuver (r = -0.277, P = 0.001 and r = -0.211, P = 0.014). ROC curve analysis demonstrated that PB perimeter of less than 12.68mm was strongly associated with SUI during the maximal Valsalva maneuver, and an Emax of less than 55.76 kPa had a 100% specificity in predicting SUI. SWE can quantify the elasticity of PB, identifying a significant difference between participants at rest and during Valsalva maneuver. In addition, the stiffness of the PB was significantly lower in women with SUI than in healthy women, which may provide a noninvasive clinical practice in SUI prediction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Stress urinary incontinence (SUI) is the complaint of involuntary urine leakage on increased abdominal pressure. SUI is a common gynecological urinary system disease, which has a significant impact on the quality of life. The prevalence of SUI greatly varies and is highly population-dependent1,2. SUI is more common in women. It has been reported that the urethral support structure has been confirmed as an important factor in the pathophysiology of SUI3,4. The urethrovaginal sphincter attaches to the perineal body (PB), and both spontaneous or deliberate injury of PB might be associated with SUI5,6,7.
The PB, a complex fibromuscular mass, was first named by MacAlister in 18898. It is the confluence of many pelvic floor structures insert and serves as the central anchor for the urogenital and anal triangles of the perineum9. The levator ani muscle and urethral vaginal sphincter play an important role in the pathogenesis of urinary incontinence, and they are all attached to the PB7,10. The PB, an extremely important structure, not only prevents expansion of the urogenital hiatus but also maintains urinary and fecal continence9. The PB could decrease its stiffness significantly during delivery with minimal injury and return to its predelivery state by the end of puerperium11,12. Because of its small size and superficial location, the PB makes it difficult to assess in detail using MRI and CT13. Ultrasound might be a more suitable approach to observe PB using a high-frequency linear array probe.
Emerging ultrasound technologies, such as strain elastography (SE) and shear wave elastography (SWE), can access tissue or mass stiffness based on different imaging principles. SE is performed using internal physiologic pulsation such as respiratory motion, cardiovascular pulsation or muscular contractions, and very small manual mechanical compression14. So, the operator repeatability of SE was poor to moderate15,16. Meanwhile, reproducibility is vital for the broad clinical application of elastography. For SWE, acoustic pressure waves produce transverse waves in tissue and the propagation velocity of the shear wave is related to softness for shear waves travel more quickly in harder tissue17,18. Unlike SE operation, the mechanical impulse is operator-independent in SWE and the tissue stiffness measurement is reliable. The PB plays an important role in supporting the pelvic floor, therefore the stiffness of the PB might be different in women with and without SUI. However, the current state of knowledge about the relationship between PB and SUI is limited. Accordingly, our primary objective was to demonstrate the feasibility of estimating PB elasticity using a quantitative SWE technology. Our secondary objective was to assess whether there is a relationship between PB parameters, including elasticity, and SUI patients, and to evaluate whether poor PB quality is a risk factor and predictor for SUI.
Materials and methods
Study design and participants
The study population comprised 134 participants between December 2018 and August 2021 at the Affiliated Hospital of Qingdao University. This study was conducted in accordance with the tenets of the Declaration of Helsinki. The Institutional Review Board of the Affiliated Hospital of Qingdao University (committee numbers: QYFYWZLL26065) approved this study, and written informed consent was obtained from all participants prior to their enrolment. All participants had a clinical assessment by an experienced gynecologist according to the Pelvic Organ Prolapse Quantification System (POP). Of these seventy healthy parous volunteers without SUI had normal pelvic support and all vaginal points above the hymen ≥ 1cm. The inclusion criteria for women with SUI were cough stress test ( +), involuntary loss of urine during increased abdominal pressure caused by coughing, laughing, sneezing, exercising, or walking and without POP above the hymen ≥ 1cm19,20. Exclusion criteria for all participants were a medical history of neurogenic urinary incontinence, prior pelvic or pelvic floor surgery, pelvic floor muscle avulsion, presence of a pelvic mass ≥ 5 cm, recent use of medications that affect mules function, genital anomalies, neurologic disorder, urinary infection, and inability to perform an acceptable Valsalva maneuver.
Transperineal ultrasound examination
Transperineal ultrasound (US) examination was performed by an operator who had more than 5 years of experience in pelvic floor US. A Resona 8T system (Mindray Medical International, Shenzhen, China) equipped with an L14-5WU linear transducer was used. Before the examination, all participants were asked to empty their bladder and scan in the lithotomy position with hip and knees flexed, and knees and ankles apart. The distance between the knees was kept the same between measurements. The probe was lightly positioned on the tissue between the vaginal and anal sphincter complexes and the depth of the image was adjusted to 3-4cm. A midsagittal view of PB was clearly visualized as hyperechoic wedge-shaped tissue between the vaginal opening and anal sphincter complex. Once the PB was clearly identified, the length, height, perimeter, and area of PB were measured thrice at rest and during the maximal Valsalva maneuver, respectively (Fig. 1).
The SWE procedures
The SWE examination was performed after the transperineal US examination. The other two sonographers, who performed the SWE and the analysis, had more than 5 years of experience in pelvic floor US and more than 2 years of experience in SWE. Both sonographers were blinded to the clinical history and the transperineal US findings.
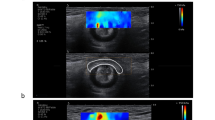
The transducer was placed lightly on the PB, avoiding any tissue pressure. The SWE imaging mode was initiated after the PB was clearly identified. The valid SWE area was shown as green and invalid areas were shown as purple in the region of interest box. A stable and high-quality SWE image with a movement-stability (M-STB) index of 4 or 5 green stars and > 90% validity could be stored in the system. Three high-quality images were stored for each participant. The region of interest (ROI) for SWE was drawn along the edge of the PB for automatic measurement of Young’s modulus (kPa).
To evaluate intra- and inter-observer repeatability, 20 randomly selected women with SUI were independently assessed by two operators. The first operator performed the SWE measurement on the PB twice in one week for the intra-observer test. The second operator performed the same measurement on the same day to reduce the risk of inter-observer bias. Each operator was blinded to the measurements of the other.
Statistical analysis
Statistical analysis was carried out using the SPSSAU project (version 21.0) (Online Application Software; https://www.spssau.com]). Quantitative data were expressed as mean ± standard deviation (SD) and comparisons between groups were made using the Student’s T test or Mann–Whitney U test. All significant variables were correlated with SUI by a Spearman correlation analysis and SWE findings were correlated with BMI by a Pearson correlation analysis. A receiver operating characteristic (ROC) curve analysis was performed to determine the optimal cut-off values of PB measurements during the maximal Valsalva maneuver for predicting SUI. The intra- and inter-observer repeatability of SWE measurements was assessed by Bland–Altman analysis and the intra-class correlation coefficient (ICC). A P-value of less than 0.05 was considered statistically significant.
Results
During the study period, 134 women were enrolled. Out of these participants, 64 were consecutive patients on the waiting list for SUI. The control group consisted of 70 healthy volunteers who had given birth and with normal pelvic support. As shown in Table 1, the average patient age was 50.2 ± 9.0 (range, 27–65) years in the SUI group and 49.0 ± 8.6 (range, 28–69) years in the control group (P = 0.460). A significant difference in BMI (P < 0.001) was observed between the control and SUI groups. Spearman analysis exhibited a positive correlation between BMI and SUI In addition, no significant difference was found in the PB measurements, including length, height, perimeter, area, Emax, and Emean elastic modulus values at rest between the SUI and the healthy participants. During the maximal Valsalva maneuver, significant differences in all PB measurements, including 2D measurements (length, height, perimeter, and area), Emax, and Emean elastic modulus values, were observed between the control and the SUI participants. The value of PB height in patients with SUI was significantly higher than in healthy participants. While the values of other measurements were significantly lower in the SUI patients than in the healthy participants. Furthermore, during the maximal Valsalva maneuver, Spearman analysis exhibited a positive correlation between PB height and SUI (Table 1).
We also compared the PB parameter between participants at rest and during the maximal Valsalva maneuver. The length and perimeter of PB were significantly increased from the participants at rest to those during the maximal Valsalva maneuver in all subjects (P < 0.001). Although the height of PB decreased and the area increased, the results were not statistically significant (P = 0.994 and P = 0.615, respectively). The elastic modulus values were significantly increased from participants at rest to those during the maximal Valsalva maneuver in all participants (Emax: 35.59 versus 53.13 kPa, P < 0.001; and Emean: 26.97 versus 40.25 kPa, P < 0.001) (Fig. 2). All elastic modulus values of PB were further analyzed with BMI in all patients using Pearson correlation coefficient analysis. Emax and Emean of PB had no significant association with BMI at rest (P = 0.367 and P = 0.799) while had a negative correlation with BMI during the maximal Valsalva maneuver (r = -0.277, P = 0.001 and r = -0.211, P = 0.014).
Stability and validity of shear waves and the elastographic image of the PB. The validity was 92% (a) at rest and 94% during the maximal Valsalva maneuver (d); (b) and (e) shown the outlined PB and the calculation of the E values; (c) and (f) shown good stability with an M-STB index of 5 stars at rest and the maximal Valsalva maneuver, respectively.
We further analyzed elastic modulus values of PB during the maximal Valsalva maneuver in predicting women with SUI using the ROC curve (Fig. 3). The area under curves (AUCs) for Emax and Emean of PB were 0.872 and 0.832, respectively. The cut-off of Emax and Emean was 55.76 kPa and 33.88 kPa, with a sensitivity of 62.9% and 81.4%, and specificity of 100.0% and 68.8%, respectively. Among two-dimensional ultrasound measurements of PB, the AUC and cut-off for PB perimeter were 0.986 and 12.68mm, respectively, with a sensitivity of 97.1% and specificity of 92.2% (Table 2).
Intra-observer differences for the same operator and inter-observer differences between two different operators were evaluated using Bland–Altman plots (Fig. 4). There were no significant differences between intra- and inter-observer variability for PB measurements using SWE (Table 3). Whether the measurements with SWE were performed by the same operator or between the two different operators, ICC values were all greater than 0.75, indicating excellent consistency (Table 3).
Discussion
SUI is a significant health problem for women, negatively affecting their quality of life, including physical activity, social relationships, and emotional health21,22. PB, which serves as the anchor of the pelvis, is a functionally and anatomically complex tissue that maintains urinary continence9. However, the current state of knowledge about the correlation between PB and SUI is limited, and further investigation is needed to understand the role of PB in SUI pathogenesis. In this study, we comprehensively measured the PB using 2D ultrasound and SWE technology to assess whether the two-dimensional measurements and elasticity may differ between the SUI and the healthy participants at rest and during the maximal Valsalva maneuver.
To our knowledge, this study was the first to quantitatively evaluate the elasticity of the PB by SWE using a high-frequency linear array probe in parous women to compare the PB properties between healthy and SUI participants. First, we evaluated the repeatability of elastic quantitative values of PB between- and within- two operators. Emax and Emean of PB had excellent reproducibility with ICC values of higher than 0.75. This demonstrated the feasibility of the use of transperineal elastography in clinical settings. A previous study by Victoria Asfour et al.13 showed poor repeatability for PB measurement, which may be due to them acquiring the entire pelvic floor images using a low-frequency curved probe. So, they maximally zoomed-in images optimized specifically for the PB using a 7-MHz curved linear probe. And their measurements of PB showed satisfactory repeatability. Based on this study and owing to PB being a small and superficial tissue, we used a high-frequency linear array probe, with a central frequency of 12 MHz, to optimize images to acquire an accurate and repeatable measurement of PB in our study.
We also exhibited that using transperineal elastography has a satisfactory repeatability to that reported for evaluating levator ani muscle stiffness in SUI and uterine cervix stiffness in order to evaluate outcome of labor induction23,24,25. Previously, Chen et al.26 have shown that it is feasible to calculate the compressive elastic modulus of the nulliparous PB in vivo.
We then compared the PB characteristics between the SUI patients and the healthy participants at rest and during the maximal Valsalva maneuver. We found that the stiffness of PB was significantly increased from the participants at rest to those during the maximal Valsalva maneuver in all participants using the SWE approach. In 2D measurements, the length and perimeter of PB were also significantly increased. These findings indicated that the PB increased hardness by increasing the length against the compression of intra-abdominal pressure on the pelvic floor support structure. The study by Chen et al.26 showed that the mean elasticity modulus in nulliparous women was 28.0 ± 4.7 kPa. We found that the Emean of PB in parous women was 26.97 ± 4.7 kPa. Our findings were consistent with a previous study demonstrating that the mean elasticity modulus of PB was decreased in multiparous women (the estimated elastic moduli was 21.5 kPa)27.
Consistent with the results of Digesu et al.28 in POP, we also found 2D PB measurements, including length, perimeter, and area, to be smaller in the SUI patients. Furthermore, the stiffness of PB during the maximal Valsalva maneuver was found to be softer in the SUI patients than in the control group. However, the stiffness of PB at rest had no significant difference between the healthy and the SUI participants. These findings help understand changes in PB from participants at rest to those during the maximal Valsalva maneuver and suggested that the differences in the PB hardness between the two groups can only be identified during the Valsalva maneuver. In addition, the elasticity of PB negatively correlated with BMI during the maximal Valsalva maneuver. The reason might be that a higher BMI increases the intramuscular adipose tissue, which could decrease the hardness of PB. This claim is supported by a previous study that determined the structural and mechanical parameters of the PB29.
The interlocking muscular, fascial, and fibrous components make the echo complex, to that extent, the PB is a heteroplasmic hyperechoic tissue in our high-frequency 2D imaging. It is covered with subcuticular fatty tissue on its surface. The PB is ovate round or wedge-shaped at rest and gradually becomes elongated to a long oval during the Valsalva maneuver. In our study, the height of PB during the maximal Valsalva maneuver was significantly higher in the SUI patients than in the control group with normal pelvic support. The PB is commonly injured during labor9,30, so we conjecture that this finding may be attributed to the damage of muscular, fascial, or fibrous components. When pelvic floor muscle contraction acts against increased intra-abdominal pressure, the injured PB in SUI cannot be pulled entirely and thin. Therefore, a PB height of greater than 8.89 mm during the maximal Valsalva maneuver might be a predictor of SUI.
In the study by Asfour et al.13, a small PB area of less than 2.4 cm2 was strongly associated with posterior compartment prolapse. In our study, the PB area obtained during Valsalva maneuver is less than 3.2cm2 in women with SUI. The disease type, probe frequency, sample size, and race might be causing the change. Compared with the PB area, a PB perimeter of less than 12.68 mm during the maximal Valsalva maneuver with a sensitivity of 97.1% and specificity of 92.2% has been shown to be strongly associated with SUI. Additionally, a retrospective study with more than 400 women demonstrated that the perimeter of PB measured during the Valsalva maneuver was a superior predictor of POP31. Hence, we recommend using the perimeter of PB obtained during the Valsalva maneuver rather than the area to assess SUI.
The strength of this study is employing the novel ultrasound method to assess the PB characteristics and determine the difference in PB parameters between the SUI patients and the healthy participants at rest and during the maximal Valsalva maneuver. Using a high-frequency linear transducer to acquire a clear and optimized image makes the SWE procedure more refined and enables the accurate measurement of the PB. Further studies with more subjects are needed to extend and confirm our study. Notably, SWE has been used to assess PB stiffness during labor, showing that primiparous women in the late stage of labor have softer PB than women in early labor27. Furthermore, studies on PB can be considered to address other clinical issues, including POP, fecal incontinence, predicting labor induction, and prevention of perineal lacerations during delivery.
In conclusion, our studies demonstrate that a high-frequency linear transducer can obtain clear PB imaging, and the elasticity of the PB can be quantitatively assessed by SWE to compare PB properties between the healthy and the SUI participants at rest and during maximal Valsalva maneuver. This method provides an additional approach for quantitative measurement of PB, which can be employed in comprehensive pelvic floor assessment.
Data availability
Data is provided within the manuscript or supplementary information files.
References
Haylen, B. T. et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol. Urodyn. 29, 4–20. https://doi.org/10.1002/nau.20798 (2010).
Rubilotta, E. et al. Pure stress urinary incontinence: analysis of prevalence, estimation of costs, and financial impact. BMC Urol. 19, 44. https://doi.org/10.1186/s12894-019-0468-2 (2019).
van Veelen, A., Schweitzer, K. & van der Vaart, H. Ultrasound assessment of urethral support in women with stress urinary incontinence during and after first pregnancy. Obstet. Gynecol. 124, 249–256. https://doi.org/10.1097/AOG.0000000000000355 (2014).
Ling, C., Shek, K. L., Gillor, M., Caudwell-Hall, J. & Dietz, H. P. Is location of urethral kinking a confounder of association between urethral closure pressure and stress urinary incontinence?. Ultrasound Obstet. Gynecol. 57, 488–492. https://doi.org/10.1002/uog.22153 (2021).
DeLancey, J. O. Structural anatomy of the posterior pelvic compartment as it relates to rectocele. Am. J. Obstetr. Gynecol. 180, 815–823. https://doi.org/10.1016/s0002-9378(99)70652-6 (1999).
Sleep, J. & Grant, A. West Berkshire perineal management trial: three year follow up. Br. Med. J. (Clin Res Ed) 295, 749–751. https://doi.org/10.1136/bmj.295.6601.749 (1987).
Oelrich, T. M. The striated urogenital sphincter muscle in the female. Anat. Rec. 205, 223–232. https://doi.org/10.1002/ar.1092050213 (1983).
Oh, C. & Kark, A. E. Anatomy of the perineal body. Dis. Colon. Rectum. 16, 444–454. https://doi.org/10.1007/BF02588867 (1973).
Woodman, P. J. & Graney, D. O. Anatomy and physiology of the female perineal body with relevance to obstetrical injury and repair. Clin. Anat. 15, 321–334. https://doi.org/10.1002/ca.10034 (2002).
DeLancey, J. O. et al. Stress urinary incontinence: relative importance of urethral support and urethral closure pressure. J. Urol. https://doi.org/10.1016/j.juro.2008.01.098 (2008).
Feola, A. et al. Impact of pregnancy and vaginal delivery on the passive and active mechanics of the rat vagina. Ann. Biomed. Eng. 39, 549–558. https://doi.org/10.1007/s10439-010-0153-9 (2011).
Weli, H. K. et al. Advanced glycation products’ levels and mechanical properties of vaginal tissue in pregnancy. Eur. J. Obstetr. Gynecol. Reprod. Biol. 214, 78–85. https://doi.org/10.1016/j.ejogrb.2017.04.037 (2017).
Asfour, V., Digesu, G. A., Fernando, R. & Khullar, V. Ultrasound imaging of the perineal body: A useful clinical tool. Int. Urogynecol. J. 31, 1197–1202. https://doi.org/10.1007/s00192-019-04166-7 (2020).
Ophir, J. et al. Elastography: Ultrasonic estimation and imaging of the elastic properties of tissues. Proc. Inst. Mech. Eng. H 213, 203–233. https://doi.org/10.1243/0954411991534933 (1999).
Dong, Y. et al. Breast strain elastography: Observer variability in data acquisition and interpretation. European journal of radiology 101, 157–161. https://doi.org/10.1016/j.ejrad.2018.02.025 (2018).
Park, C. S. et al. Interobserver variability of ultrasound elastography and the ultrasound BI-RADS lexicon of breast lesions. Breast Cancer 22, 153–160. https://doi.org/10.1007/s12282-013-0465-3 (2015).
Sarvazyan, A. P., Rudenko, O. V., Swanson, S. D., Fowlkes, J. B. & Emelianov, S. Y. Shear wave elasticity imaging: A new ultrasonic technology of medical diagnostics. Ultrasound Med. Biol. 24, 1419–1435. https://doi.org/10.1016/s0301-5629(98)00110-0 (1998).
Athanasiou, A. et al. Breast lesions: Quantitative elastography with supersonic shear imaging–preliminary results. Radiology 256, 297–303. https://doi.org/10.1148/radiol.10090385 (2010).
Al Adem, K. M. et al. Implantable Systems for Stress Urinary Incontinence. Ann. Biomed. Eng. 45, 2717–2732. https://doi.org/10.1007/s10439-017-1939-9 (2017).
Committee Opinion No. 603: Evaluation of uncomplicated stress urinary incontinence in women before surgical treatment. Obstet. Gynecol. 123, 1403–1407. https://doi.org/10.1097/01.AOG.0000450759.34453.31 (2014).
Sangsawang, B. & Sangsawang, N. Stress urinary incontinence in pregnant women: a review of prevalence, pathophysiology, and treatment. Int. Urogynecol. J. 24, 901–912. https://doi.org/10.1007/s00192-013-2061-7 (2013).
Xu, P. et al. Barriers and enablers of pelvic floor rehabilitation behaviours in pregnant women with stress urinary incontinence: A qualitative analysis using the theoretical domains framework. BMC Pregnancy Childbirth 23, 300. https://doi.org/10.1186/s12884-023-05633-2 (2023).
Li, X. M. et al. Usefulness of transperineal shear wave elastography of levator ani muscle in women with stress urinary incontinence. Abdom. Radiol. (NY) 47, 1873–1880. https://doi.org/10.1007/s00261-022-03478-5 (2022).
Li, X. et al. Usefulness of Transperineal Virtual Touch Quantification in the Cervix for Predicting Outcome of Labor Induction. Ultrasound Med. Biol. 46, 2207–2214. https://doi.org/10.1016/j.ultrasmedbio.2020.04.037 (2020).
Zhou, M., Shui, W., Bai, W., Wu, X. & Ying, T. Ultrasonographic study of female perineal body and its supportive function on pelvic floor. Front Med (Lausanne) https://doi.org/10.3389/fmed.2023.1176360 (2023).
Chen, L., Low, L. K., DeLancey, J. O. & Ashton-Miller, J. A. In vivo estimation of perineal body properties using ultrasound quasistatic elastography in nulliparous women. J. Biomech. 48, 1575–1579. https://doi.org/10.1016/j.jbiomech.2015.02.056 (2015).
Rostaminia, G. et al. Shear wave elastography to assess perineal body stiffness during labor. Female Pelvic. Med. Reconstr. Surg. 25, 443–447. https://doi.org/10.1097/SPV.0000000000000585 (2019).
Digesu, G. A., Chaliha, C., Salvatore, S., Hutchings, A. & Khullar, V. The relationship of vaginal prolapse severity to symptoms and quality of life. BJOG 112, 971–976. https://doi.org/10.1111/j.1471-0528.2005.00568.x (2005).
Kochova, P. et al. The histological microstructure and in vitro mechanical properties of the human female postmenopausal perineal body. Menopause 26, 66–77. https://doi.org/10.1097/GME.0000000000001166 (2019).
Kamisan Atan, I., Shek, K. L., Furtado, G. I., Caudwell-Hall, J. & Dietz, H. P. The association between levator-urethra gap measurements and symptoms and signs of female pelvic organ prolapse. Female Pelvic. Med. Reconstr. Surg. 22, 442–446. https://doi.org/10.1097/SPV.0000000000000311 (2016).
Ow, L. L. et al. Should Genital Hiatus/Perineal Body Be Measured at Rest or on Valsalva?. Female Pelvic. Med. Reconstr. Surg. 25, 415–418. https://doi.org/10.1097/SPV.0000000000000608 (2019).
Author information
Authors and Affiliations
Contributions
ZongLi Yang: Conceptualization and Methodology; XiuMei Li and LiMin Zhang: Writing- Original draft preparation and Software; Yong Li: Data curation and Writing- Reviewing and Editing; Yushan Jiang: Prepared Figs. 1–4; Cheng Zhao and ShiBao Fang: Supervision and Validation; LiWen Sun: Writing- Reviewing and Editing; All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics
The studies involving human participants were reviewed and approved by the ethics review committee of the Affiliated Hospital of Qingdao University. The patients/participants provided their written informed consent to participate in this study.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, X., Zhang, L., Li, Y. et al. Assessment of perineal body properties in women with stress urinary incontinence using Transperineal shear wave elastography. Sci Rep 14, 21647 (2024). https://doi.org/10.1038/s41598-024-72429-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-72429-5
- Springer Nature Limited