Abstract
Ureteral obstruction is a prevalent urological condition associated with significant complications. The purpose of our study was to assess the safety and efficacy of a novel self-expanding, large caliber, biocompatible polymer-coated ureteral stent (Allium) for the treatment of ureteral obstructions. We conducted a retrospective analysis of data from patients who underwent Allium ureteral stent placement at our institute between November 2018 and May 2023. Demographic, clinical, and perioperative parameters were collected and analyzed. Logistic regression analyses were performed to identify preoperative factors predicting Allium stent migration. The study cohort comprised 30 patients who received a total of 40 successfully implanted Allium stents. No significant adverse events related to the insertion procedure were observed. During a median follow-up period of 29 months (range: 1–60 months), migration occurred in 11 (27.5%) stents while encrustation was noted in 8 (20%) stents. The median functional duration of the Allium stents was found to be 22 months (range:1–60 months), with an overall functioning rate at last follow-up being recorded as 59.5%. Multivariate analysis revealed that the glomerular filtration rate of the ipsilateral kidney was the sole risk factor predictive of Allium stent migration. With its minimal invasiveness and good tolerability, the Allium stent represents a safe and viable management option for treating ureteric obstructions; however, it should not be considered as definitive treatment but rather as an alternative option for patients unwilling or unsuitable for definitive treatment, particularly high-risk individuals or elderly patients exhibiting decreased ipsilateral glomerular filtration rates.
Similar content being viewed by others
Introduction
Ureteral obstruction is a prevalent urological condition that can arise from either malignancies or benign factors, such as impacted calculi, radiotherapy, or other diseases. It can be asymptomatic or manifests as flank pain, urinary tract infection, and may even result in non-functioning kidneys1. Various treatment options are available for managing ureteral obstructions including reconstructive surgery, percutaneous nephrostomy, or double-J stents2. Despite the satisfactory outcomes achieved with robot-assisted ureteroplasty nowadays, it is associated with relatively high rates of complications3. In patients who are unwilling or unfit for definitive treatment—especially those at high risk or elderly individuals—ureteral stents can be employed.
Despite the advantages of minimal invasiveness and ease of insertion, double-J stents are associated with potential adverse side effects such as pain, hematuria, infection, symptoms of bladder irritation, stent migration, and encrustation necessitating frequent replacement (every few months)4. Moreover, the placement of double-J stents usually leads to lower urinary tract symptoms (LUTS), resulting in a diminished quality of life. Consequently, several segmental stents made preferably from metal have been introduced to address the aforementioned issues and limitations by allowing long-term or permanent indwelling5.
The Allium stent (Allium, Allium LTD, Caesarea, Israel) is a novel large caliber self-expanding ureteral stent composed of nitinol and coated with a biocompatible polymer to prevent tissue ingrowth and encrustation6. The initial study on the use of the Allium stent for managing chronic ureteral obstructions was conducted by Moskovitz et al. in 20127. However, limited research has been conducted thus far regarding its safety and feasibility8. In this study, our objective is to present the long-term outcomes of all patients treated with the Allium stent at our institution, assess its safety and feasibility, analyze factors predicting stent migration, the most commonly encountered long-term complications in segmental stents, and provide relevant technical recommendations.
Materials and methods
Patient selection
Data were obtained from patients with ureteric obstructions and treated with the endoscopic placement of the Allium stent. in our hospital between November 2018 and May 2023. All patients underwent antegrade and/or retrograde urography as well as computed tomography (CT) ureteric coronal reconstruction before surgery to identify the length and location of the ureteric obstruction. Tc-99 m-DTPA renography was used to evaluate the function (glomerular filtration rate, GFR) of the affected kidney.
Surgical technique
Prior to surgery, patients with positive preoperative urine cultures were treated based on results from antibiotic sensitivity testing. Cephalosporins or quinolones were prescribed for patients who had sterile urine as antibiotic prophylaxis. The initial dosage was given intravenously during the anesthetic induction process, and the subsequent doses were given 12–24 h following the prophylactic treatment.
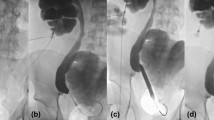
The insertion of the Allium stent was performed under general anesthesia. For obstructions in the upper ureter or ureteropelvic junction site, the Allium stent was placed in an antegrade fashion. Briefly, a 5Fr ureter catheter was externally inserted to the obstruction site via cystoscopy in lithotomy position. Renal access was then achieved using an 18-G coaxial needle (Urovision, Germany) under ultrasound guidance in prone position. After introducing a 3.5-Fr stiff J-tip guidewire (Urovision, Germany) into the collecting system through the access needle, tract dilation up to 24 F was performed using a “two-step” method without fluoroscopy assistance9. A hydrophilic guide wire was passed through the obstruction segment under nephroscope guidance and retrograde injection of methylene blue through the ureteral catheter could be employed if necessary for indicating the ureteral lumen. Following advancement of an ureteral balloon dilator (X Force U30; Bard Urological, USA) over the guidewire to reach the site of obstruction, direct vision-guided dilation of obstruction (25 atm for 3 min) took place. The Allium stent was then deployed according to the manufacturer’s instruction. Subsequently, antegrade pyelography was performed to ensure proper placement of an Allium ureteric stent (24 F, 10 cm) into the obstruction site.
For obstructions in the middle or distal ureter, retrograde placement of the Allium stent was performed. Briefly, a 0.035-inch guide wire was inserted through the double-J stent to reach the renal pelvis with the patient in lithotomy position. Subsequently, a ureteroscope was utilized to traverse the obstruction segment over the guide-wire for pre-dilation of the ureter. An ureteral balloon dilator (X Force U30; Bard Urological, USA) was then advanced along the guide wire to reach the site of stenosis and inflated to 25 atm (2.15 MPa), maintaining this pressure for 3–5 min. Following confirmation of successful dilation via ureteroscopy, retrograde insertion of the Allium stent into the obstruction site was performed. Finally, retrograde pyelography was conducted to confirm successful treatment of the ureteric obstruction at the end of the procedure.
For patients with complete ureteral obstruction or obstructions in the ureteroenteric and ureterovesical anastomosis, a combined antegrade and retrograde approach can be employed. To navigate through the completely obstructed segment, it is recommended to use a hydrophilic guide wire for achieving through-and-through access under direct visualization. If necessary, the previously mentioned modified ‘cut-to-the-light’ technique can be utilized10.
Follow-up
Plain film of the kidney, ureters and bladder (KUB) was obtained on the first or second postoperative day. CT and diuretic renography was performed 1 month after the stent insertion. The patients were subsequently followed up every 3–6 months with serum creatinine and renal sonography. If ultrasound showed increasing hydronephrosis, CT scan were repeated. Stent functioning at last follow-up was defined as no deterioration of renal function, no increase in hydronephrosis and no requirement for the stent to be replaced or removed due to intolerance, migration or encrustation.
Statistical analysis
Statistical analysis was performed using SPSS software version 22.0. Continuous variables were described as the mean ± standard deviation when normally distributed, or as median (range) for skew distribution data. The categorical variables were described as numbers or percentages. Time to the last follow-up in functioning stent was considered a censor point and time to stent removal/failure was considered as an end point for plotting the functioning stent survival using Kaplan-Meier analysis. Univariate and multivariate logistic regression analyses were performed to test preoperative factors predicting Allium stent migration. Values of P < 0.05 were considered to be statistically significant.
Results
The characteristics of ureteral obstructions and demographic data of the patients were summarized in Table 1. The study cohort comprised 30 patients with a mean age of 47.3 ± 12.3, including five patients with bilateral ureteral obstructions and two patients who underwent replacement of a new Allium stent during the follow-up period. In three renal units, two Allium stents were placed in one ureter due to long segment stricture. A total of 40 Allium stents were successfully inserted, with proper positioning confirmed by intraoperative antegrade or retrograde pyelography as well as postoperative KUB. The perioperative and long-term outcomes of the patients were presented in Table 2. No significant adverse events related to the insertion procedure were recorded. During a median follow-up period of 29 months (range: 1–60 months), migration occurred in 11 stents (27.5%), with a median time of 7 months (range: 1–24 months) after insertion; four migrated towards the bladder and seven towards the renal pelvis. Following migration, one patient underwent Allium stent replacement, three patients required ureteral reconstructive surgery, five patients received double-J stent insertion, and one patient underwent nephrectomy. In one case where the stent migrated into the bladder one month after insertion, significant relief of hydronephrosis was observed during continued periodic follow-up. Encrustation was found in eight stents (20%) at a median time of 23.5 months (range: 3–34 months) after insertion; five remained functional while three had to be removed. In a patient with obstruction progression, severe pelvic adhesions and risk of ureteroenteric fistula following stent removal necessitated leaving the Allium stent in place along with long-term nephrostomy tube placement. One patient died from primary malignancy despite having a patent stent in place. Another patient experienced failure to seal rectoureteral fistula leading to recurrent fever and urinary infection within one month after insertion, resulting in subsequent removal of the stent.
The functioning survival duration for Allium stents ranged from 1 to 60 months (median: 22 months), as depicted by Kaplan-Meier analysis shown in Fig. 1.The univariate and multivariate analyses revealed that preoperative GFR of ipsilateral kidney was identified as the sole predictive factor for Allium Stent migration (Table 3).
Discussion
Ureteral reconstructive surgeries, such as ureteroureterostomy, ureteral reimplantation or replacement procedures, are considered the gold standard for managing ureteral obstructions11. Although minimally invasive, the insertion of a double-J stent or nephrostomy tube is associated with various side effects including frequent replacements and compromised quality of life. With advancements in material science, metallic stents have emerged as an alternative approach to address ureteral obstructions. In this study, we utilized the Allium stent - a coated self-expanding metallic stent - to treat patients with complex ureteric obstructions following open ureteroplasty or multiple endoscopic interventions. After a median follow-up duration of 29 months (range 1–60 months), functional stents were observed in 59.5% of the treated ureters. Our findings demonstrate that for patients who are unsuitable for or unwilling to undergo definitive surgical treatment, Allium stent insertion represents a favorable choice.
Other studies have also assessed the safety and feasibility of the Allium stent in patients with ureteral obstruction. Moskovitz et al. reported their experiences and outcomes of utilizing the Allium stent in 40 patients (49 ureters) with ureteral obstruction. The insertion of all stents was successful, and no significant adverse events related to the stent or procedure were documented. During a mean follow-up period of 21 months (range 1–63 months), the average duration of indwelling time was 17 months (range 1–63 months). Notably, eight patients (16.3%) remained asymptomatic without new hydronephrosis during a periodical follow-up ranging from 6 to 45 months after scheduled stent removal7. However, in our study, only four renal units (11.4%) exhibited asymptomatic patency of the ureter following stent removal. In another retrospective cohort study involving 17 patients treated with the Allium stent, the mean indwelling time was reported as being 14.29 ± 1.29 months, with a minimum duration of three months due to stent migration. Furthermore, they observed an overall success rate of 35.29% after stent removal during an average follow-up period of 10.42 ± 2.39 months12. The discrepancies in these studies regarding mean indwelling time and success rate after stent removal may be attributed to variations in etiology, location, and length of obstructions.
Stent migration has been consistently reported as the most common long-term complication in segmental stents8. Moskovitz et al. and Guandalino et al. reported migration rates of 14.3% and 18.9%, respectively, for Allium stents7,13. These stents were characterized by a short intravesical anchor portion connected to the main segment through a single wire. The authors speculated that the anchoring segment may be less effective when located within the ureter, thereby increasing the risk of stent migration, particularly in cases with middle ureter obstructions. Agrawal et al., studying Memokath 051 stents, another type of metallic segmental ureteral stent, documented a migration rate of 17.6% and concluded that obstructions at the PUJ site had the highest migration rate (66.7%), although statistical validity was limited due to small sample size (2 out of 3 stents)14. Forster et al., in a similar study, recorded a migration rate of 46%15. In our study, to minimize bladder irritation symptoms and other discomfort associated with Allium stents, we intentionally excluded an anchoring segment from all inserted stents; this may explain the higher observed migration rate compared to previous studies. Furthermore, after conducting uni- and multivariate analysis on potential preoperative factors related to stent migration risk, our data indicated that higher GFR (glomerular filtration rate) in the ipsilateral kidney prior to surgery was significantly associated with an increased risk of stent migration, which means low GFR was a protective factor. None of the four poorly functioning obstructed kidneys (GFR < 10 ml/min) included in this study exhibited any instances of stent migration during a follow-up period exceeding two years. However, the underlying reason was unknown.
Various minimally invasive therapies are available for ureteral obstruction, each with its own advantages and disadvantages. Endourological treatments such as balloon dilation, acucise, cold-knife or laser endoureterotomy have shown favorable outcomes in patients with benign ureteral obstructions16. These approaches can achieve satisfactory success rates ranging from 60 to 85.7%, but are limited to intrinsic stenosis within 2 cm17,18. Surgical ureteroplasty, whether performed laparoscopically or robot-assisted, can even exceed a success rate of 90%19,20, but is associated with a significantly higher complication rate compared to endoscopic treatment. For instance, Carbonara et al. reported an overall complication rate of 33.3% for robot-assisted ureteral reimplantation in the treatment of distal ureteral obstructions21. Fan et al., who documented the use of robot-assisted laparoscopic ileal ureter replacement for managing long and complex obstructions, reported a Clavien-Dindo grade II-III complication rate of 27.7%22. Additionally, if the initial surgical pyeloplasty or ureteroplasty failed, the difficulty of second surgical repair will be significantly increased due to local scar and tissue adhesion, which may affect the outcome of the operation and increase the incidence of complications. Therefore, when the endourological treatment is ineffective or surgical ureteroplasty is not feasible or failed, the Allium stent becomes an appealing option due to its minimal invasiveness and endoscopic approach. In our series, although we achieved a functioning rate of 59.5% without any complications greater than Clavien-Dindo grade II occurring, it remains less effective than surgical ureteroplasty. Hence, careful discussion with patients regarding the decision to opt for the Allium stent should be conducted prior to surgery. While on one hand treatment with the Allium stent is less invasive than surgical repair; on the other hand, long-term complications such as migration, encrustation and recurrent urinary infections may necessitate reoperation.
The management of stenosis following the failure of the Allium stent remains a matter of concern. Apart from double-J stent insertion, nephrostomy, and nephrectomy for non-functioning kidneys, laparoscopic ureteral repair was performed in four patients after removal of the Allium stent in our study. This included pyeloureteroplasty in three patients and Boari flap-psoas hitch in one patient. In the procedure, no significant damage was found in the normal ureteral segment covered by the Allium stent. The presence of the Allium stent did not significantly increase the difficulty associated with subsequent surgical ureteroplasty. During regular follow-up, all four patients experienced a significant reduction in hydronephrosis; however, due to limited sample size, statistical significance could not be established. Further large-scale case-control studies are warranted to investigate the impact of Allium stent insertion on subsequent surgical repair.
Our study had several limitations. Firstly, it was constrained by its retrospective design and small sample size. Secondly, the assessment of split renal function through renography was not adequately performed in all patients during follow-up. Thirdly, we did not compare the outcomes of the Allium stent with other segmental or metallic ureteral stents such as the Memokath 051 sent, Uventa stent, or Resonance stent. Therefore, future prospective multi-center randomized controlled studies are strongly encouraged and warranted to obtain more realistic and accurate results.
Conclusion
Due to its minimal invasiveness and excellent tolerability, the Allium stent represents a safe and viable management option for ureteric obstructions. In our assessment, while not serving as a definitive treatment modality, it can still serve as an alternative therapeutic approach for patients who are unwilling or unsuitable for definitive treatment, particularly high-risk individuals and elderly patients with reduced ipsilateral glomerular filtration rate.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CT:
-
Computed tomography
- GFR:
-
Glomerular filtration rate
- BMI:
-
Body mass index
- KUB:
-
Kidney, ureters and bladder
References
Ulvik, O., Harneshaug, J. R. & Gjengsto, P. Ureteral strictures following ureteroscopic stone treatment. J. Endourol. 35(7), 985–990 (2021).
Yang, K. et al. Robotic-assisted lingual mucosal graft ureteroplasty for the repair of complex ureteral strictures: technique description and the medium-term outcome. Eur. Urol.81(5), 533–540 (2022).
Elbers, J. R. et al. Robotic repair of ureteral strictures: techniques and review. Curr. Urol. Rep.22(8), 39 (2021).
Lundeen, C. J. et al. Ureteral stents: the good the bad and the ugly. Curr. Opin. Urol.30(2), 166–170 (2020).
Lange, D. et al. Ureteral stent-associated complications–where we are and where we are going. Nat. Rev. Urol.12(1), 17–25 (2015).
Gao, W., Xing, T. & Ou, T. The resonance and the Allium ureteral stents in the treatment of non-malignant refractory ureterostenosis. BMC Urol.21(1), 53 (2021).
Moskovitz, B., Halachmi, S. & Nativ, O. A new self-expanding, large-caliber ureteral stent: results of a multicenter experience. J. Endourol. 26(11), 1523–1527 (2012).
Corrales, M. et al. A systematic review of long-duration stents for ureteral stricture: which one to choose? World J. Urol.39(9), 3197–3205 (2021).
Su, B. et al. Long-term outcomes of ultrasound-guided percutaneous nephrolithotomy in patients with solitary kidneys: a single-center experience. World J. Urol.37(5), 951–956 (2019).
Hu, W. et al. Simultaneous antegrade and retrograde endoscopic treatment of non-malignant ureterointestinal anastomotic strictures following urinary diversion. BMC Urol.17(1), 61 (2017).
Gao, X. et al. Step-by-step technique for the endoscopic treatment of ureteric stricture. BJU Int.128(6), 692–696 (2021).
Avitan, O. et al. Allium ureteral stent as a treatment for ureteral stricture: results and concerns. Urol. Int.106(5), 482–486 (2022).
Guandalino, M. et al. The Allium ureteral stent in the management of ureteral stenoses, a retrospective, multicenter study. Prog. Urol.27(1), 26–32 (2017).
Agrawal, S. et al. The thermo-expandable metallic ureteric stent: an 11-year follow-up. BJU Int. 103(3), 372–376. (2009).
Forster, L. R. et al. The fate of ureteral memokath stent(s) in a high-volume referral center: an independent long-term outcomes review. J. Endourol. 35(2), 180–186 (2021).
Lucas, J. W. et al. Endoscopic management of ureteral strictures: an update. Curr. Urol. Rep.19(4), 24 (2018).
Lu, C. et al. Endoscopic balloon dilatation in the treatment of benign ureteral strictures: a meta-analysis and systematic review. J. Endourol. 33(4), 255–262 (2019).
Rassweiler, J. J. et al. Minimally invasive treatment of ureteropelvic junction obstruction: long-term experience with an algorithm for laser endopyelotomy and laparoscopic retroperitoneal pyeloplasty. J. Urol.177(3), 1000–1005 (2007).
Kolontarev, K., Kasyan, G. & Pushkar, D. Robot-assisted laparoscopic ureteral reconstruction: small a, cyrillic systematic review of literature. Cent. Eur. J. Urol.71(2), 221–227 (2018).
Kapogiannis, F. et al. Laparoscopic and robotic management of ureteral stricture in adults. Vivo34(3), 965–972 (2020).
Carbonara, U. et al. Robot-assisted ureteral reimplantation: a single-center comparative study. J. Endourol. 35(10), 1504–1511 (2021).
Fan, S. et al. Robot-assisted laparoscopic ileal ureter replacement with extracorporeal ileal segment preparation for long ureteral strictures: a case series. BMC Surg.22(1), 435 (2022).
Funding
Supported by Beijing Municipal Natural Science Foundation (Grant No. 7222239).
Author information
Authors and Affiliations
Contributions
S.B.X.: Protocol development, Data collection and management, Data analysis, Manuscript writing/editing. H.W.G., X.B. and Z.G. : Data collection. X.B.: Data analysis, Manuscript editing. L.Y.B.: Manuscript editing, data analysis. T.Y.Z.: Data analysis. L.J.X.: Protocol development, Project development, Data analysis, Manuscript editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
Written informed consent was obtained from all subjects to use their data and information for publication.
Ethical approval and consent to participate
This study was approved by the Beijing Tsinghua Changgung Hospital Ethics Committee and conducted in accordance with the standards laid down in the Declaration of Helsinki. All patients provided informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Su, B., Hu, W., Xiao, B. et al. Long-term outcomes of Allium ureteral stent as a treatment for ureteral obstruction. Sci Rep 14, 21958 (2024). https://doi.org/10.1038/s41598-024-73125-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-73125-0
- Springer Nature Limited