Abstract
Breast cancer metastasis is associated with a poor prognosis and a high rate of mortality. Cathepsin L (CTSL) is a lysosomal cysteine protease that promotes tumor metastasis by degrading the extracellular matrix. Gene set enrichment analysis revealed that CTSL expression was higher in tumorous than in non-tumorous tissues of breast cancer patients and that high-level CTSL expression correlated positively with the epithelial-mesenchymal transition. Therefore, we hypothesized that inhibiting CTSL activity in tumor cells would prevent metastasis. In this study, we characterized the inhibitory activity of SnuCalCpI15, the I29 domain of a CTSL-like cysteine protease from Calotropis procera R. Br., and revealed that the propeptide stereoselectively inhibited CTSL in a reversible slow-binding manner, with an inhibitory constant (Ki) value of 1.38 ± 0.71 nM, indicating its potency as an exogenous inhibitor in anti-cancer therapy. SnuCalCpI15 was localized intracellularly in MDA-MB-231 breast cancer cells and suppressed tumor cell migration and invasion. These results demonstrate the potential of SnuCalCpI15 as a novel agent to prevent breast cancer metastasis.
Similar content being viewed by others
Introduction
Breast cancer is the most common cancer among women worldwide and the second most common cause of cancer-related death in women1. Primary breast cancer is treated with radiation therapy, immunotherapy, chemotherapy, and surgery, but metastases to other organs drastically reduce survival rates2,3. Despite continuous research on breast cancer over the decades, the global incidence of breast cancer and the associated mortality rate remain high4. Recently, monoclonal antibody drugs targeting several oncoproteins overexpressed in triple-negative breast cancer (TNBC) have shown excellent patient prognosis, and immunotherapy, immune-based combination therapies, and immune checkpoint inhibitor therapies are playing an important role in TNBC treatment5,6,7,8. However, these drugs can cause side effects such as liver damage, vomiting, diarrhea, fatigue, and hearing loss9,10. Therefore, a better understanding of breast cancer and the development of new strategies to improve the survival of patients with breast cancer are needed.
Cathepsins are lysosomal proteases in the papain superfamily that promote cell migration and invasion by degrading extracellular matrix (ECM) components11. Cathepsin L (CTSL), a C1A-type protease, is overexpressed in breast, glioblastoma, lung, and colon cancers, and its high expression level are positively correlated with poor prognosis in these patients12,13,14,15. Cancer cells with elevated CTSL levels are characterized by high metastatic ability, colony formation, and proliferation16,17. Therefore, inhibiting CTSL activity may provide a strategy to reduce tumor malignancy.
According to the MEROPS database, cystatins (I25A), stefins (I25B), and kininogens (I25C) are endogenous protein inhibitors containing an I25 domain18. All three inhibitors reversibly suppress CTSL activity and compete for substrates, with inhibitory dissociation constant (Ki) values in the picomolar to nanomolar range19. An imbalance between CTSL and these endogenous protein inhibitors represents a significant form of dysregulation in breast cancer13. Uncontrolled CTSL activity can be targeted with synthetic exogenous inhibitors such as CLIK-148 (an E-64 derivative), which is a selective CTSL inhibitor that protects against tumor-induced hypercalcemia and distant bone metastasis20,21. Most exogenous inhibitors are small synthetic compounds with a short peptide chain that binds to the active-site cleft and contains an electrophilic domain that attacks the thiolate group at the catalytic cysteine22.
Exogenous, high-molecular-weight protein inhibitors have gained interest as functional alternatives for suppressing CTSL activity, offering higher selectivity through stereoselective protein–protein interactions compared to low-molecular-weight peptides or chemical inhibitors23,24. Structural investigations of the propeptide segment in the CTSL zymogen have demonstrated its potency and that of its analogs as exogenous CTSL protein inhibitors25. CTSL remains proteolytically inactive in its zymogen form until the N-terminal propeptide region (I29 domain) is enzymatically truncated by autocatalysis within the endolysosome26. Accordingly, the excessive proteolytic activity of CTSL could be inhibited by I29 domain-containing proteins that mimic the propeptide region of the CTSL zymogen, thereby keeping CTSL in its inactive state.
In previous studies, the I29 domain of a papain-like cysteine protease, SnuCalCp15, was isolated from Calotropis procera R. Br and named SnuCalCpI1527. SnuCalCpI15 exhibits inhibitory activity against papain28 and CTSL23, and the kinetic properties suggest its potential as a powerful anti-cancer agent. However, the lack of information on the cytotoxicity, dosage, and suppressive role of SnuCalCpI15 in tumor development has hindered researches into its anti-cancer activity and therapeutic potential. In this study, we evaluated the inhibitory characteristics of SnuCalCpI15 against four C1A-type cysteine proteases and determined its inhibitory constant for CTSL to assess its potency as a CTSL-selective inhibitor and a potential anti-cancer agent. Thus, a molecular docking simulation was performed followed by assays of cytotoxicity, tumor migration, and invasion in MDA-MB-231 breast cancer cells. The results demonstrated the potential of using SnuCalCpI15 as a novel agent to prevent breast cancer metastasis.
Results and discussions
Highly-expressed CTSL is strongly associated with a poor prognosis in breast cancer patients
CTSL promotes the growth of various cancers including breast cancers; thus, its high-level expression may be a predictor of prognosis13,15,29,30. First, we reconfirmed the clinical relevance of the association between CTSL expression and the prognosis of breast cancer patients. CTSL expression was quantified in breast tumor (T) and adjacent non-tumor (N) tissues and representative hematoxylin and eosin (H&E) and CTSL-stained images of breast cancer tissues (Fig. 1a). The immunohistochemical scores of the tissues were 4,348 ± 1,874 and 30,187 ± 17,656 for T and N, respectively (p < 0.01), indicating that higher CTSL expression was observed in breast cancer tissues (Fig. 1b). We also confirmed that the CTSL mRNA expression level was higher in breast tumor tissue (T) than in normal tissue (N) using the public GEO database (Fig. 1c, d). The CTSL mRNA expression levels for GSE 5364 were 720 ± 293 and 1,234 ± 539 for N and T, respectively (p < 0.001). They were 8.9 ± 0.3 and 9.6 ± 0.7 for N and T, respectively, for GSE 3744 (p = 0.017). Kaplan–Meier analysis of overall survival (OS) and recurrence-free survival (RFS) in breast cancer patients was carried out for the high CTSL and low CTSL groups (Fig. 1e, f). The hazard ratios were 1.44 (p < 0.001) and 1.36 (p < 0.001) for OS and RFS respectively, indicating that high CTSL expression is notably associated with a poor prognosis in breast cancer patients. Previous studies have reported that higher CTSL levels are associated with a lower survival rate in patients with hepatocellular carcinoma, glioblastoma, lung cancer, and breast cancer16,31,32. These results and our own suggest that CTSL as an attractive target for cancer treatment.
High-level CTSL expression is strongly associated with a poor prognosis in breast cancer patients. (a) Representative images of H&E and CTSL staining of breast cancer tissue. Dashed lines: interface between breast tumor (T) and adjacent non-tumor (N) tissues. Scale bar: 100 μm. N = 8. (b) Quantification of CTSL expression in breast tumor tissue and normal tissue using ImageJ. (c, d) mRNA expression of CTSL in breast cancer and normal tissue according to the breast cancer datasets GSE5364 (c, N = 13 and T = 183) and GSE 3744 (d, N = 7 and T = 40). (e, f) Kaplan–Meier analysis of OS (e) and RFS (f) in breast cancer patients divided into high and low CTSL groups (HR: hazard ratio).
Inhibitory characteristics of SnuCalCpI15 against CTSL
Among the four tested C1A-type proteases (bromelain, papain, CTSB, and CTSL), the inhibitory efficacy of SnuCalCpI15 was the highest for CTSL (Fig. 2a). The IC50 values of SnuCalCpI15 followed the order of bromelain (478 ± 77 nM), papain (291 ± 50 nM), and CTSL (6.5 ± 0.9 nM). In assays of CTSB, its activity was reduced by SnuCalCpI15 only at a millimolar concentration. To confirm that SnuCalCpI15 maintained its structural integrity during the enzyme assay, a proteolytic digestion assay was conducted (Fig. 2b, full-length gel image: Fig. S3). However, the appearance of an additional band (below 15 kDa) was observed after a longer incubation time in the papain and bromelain digestions but not in the CTSL or CTSB digestions. Proteolytic degradation of SnuCalCpI15 was more noticeable with papain; the protein lost its native conformation after 1 h of incubation. As SnuCalCpI15 is a protein comprised of 156 amino acids23, it may serve as an alternative substrate for papain and bromelain. Therefore, its degradation may have accounted for the higher apparent IC50 values of these two proteases, as hydrolysis of the fluorogenic substrate (Z-Phe-Arg-AMC) would have been accordingly reduced33. Structural integrity and proteolytic resistance are crucial for maintaining the function of therapeutic peptides or proteins34. Therefore, SnuCalCpI15 exhibited both inhibitory activity and proteolytic stability, suitable for CTSL-selective inhibition.
The inhibitory kinetic parameters were determined to identify the binding mode of SnuCalCpI15 against CTSL. The reaction curve in Fig. 2c shows the slow-binding inhibitory kinetics of SnuCalCpI15. Since the \(\:{k}_{\text{obs}}\:\)values increased linearly with increasing inhibitor concentration (Fig. 2d), the SnuCalCpI15 inhibitory reaction was characterized as a simple reversible slow-binding reaction35. As a result, the experimental inhibitory constant (Ki) of SnuCalCpI15 was 1.38 ± 0.71 nM, which was similar to the sequence-based putative dissociation constant (Kd = 52 nM) between SnuCalCpI15 and CTSL36.
Inhibitory characteristics of SnuCalCpI15 against CTSL. (a) The half-maximum inhibitory concentration of SnuCalCpI15 towards bromelain (square, 20 nM), papain (circle, 2 nM), CTSB (triangle, 0.4 nM), and CTSL (inverted triangle, 0.2 nM). Concentration of Z-Phe-Arg-AMC and SnuCalCpI15 were 0.5 mM and 100 nM–10 mM, respectively. (b) Proteolytic degradation of SnuCalCpI15 by C1A-type cysteine proteases detected by SDS-PAGE. Enzymes (bromelain, 20 nM; papain, 2 nM; CTSB, 0.4 nM; CTSL, 0.2 nM) were mixed with SnuCalCpI15 (10 µM) and incubated at 37 °C for 1 h. Arrows indicate intact SnuCalCpI15 and its degraded fragment. CON, SnuCalCpI15; 60 min*, SnuCalCpI15 incubated for 60 min without enzyme. The respective protease was analyzed in the respective gel and processed in parallel. The uncropped gels are shown in Supplementary Fig. S3. (c) Time-dependent progress curve of CTSL (0.2 nM) in the presence of varying concentrations of SnuCalCpI15 (0–16 nM) without pre-incubation. (d) Changes in kobs values according to the SnuCalCpI15 concentration (1, 2, 4, and 8 nM) in a simple inhibition model.
The SnuCalCp15 structural model indicates a CTSL-like I29 domain
A structural model of SnuCalCp15, incorporating the C1A domain of the native protease, was used to investigate the primary interactions of SnuCalCpI15 and the structural features of the protease − inhibitor complex. Among the five SnuCalCp15 structural models, the model with the highest pLDDT score (89.1) is shown in Fig. 3a. Previously, taxonomic annotation of SnuCalCp15 indicated that SnuCalCpI15 belongs to the N-terminal propeptides in CTSL-like precursors, rather than CTSB-like precursors within the C1A family12,27,28. The pLDDT score of the SnuCalCpI15 globular domain was more than 70, except for the prolonged N-terminal segment (L1p-K15p). Three helical segments were in contact with the propeptide binding loop segment, corresponding to S135–I145 in the C1A domain. This interaction is crucial for the I29 domain to bind with the C1A domain in CTSL-like proteases25. Another notable interaction involved the substrate binding cleft, with the S and S` subsites aligning with the catalytic diad (C24 and H156), where the long connecting loop that stems from the I29 domain served as a tether linking the globular domain to the C1A domain. The overall structural model confirmed the integrity of the I29 domain but with low accuracy in the extended C-terminal tail after spanning the pitted surface.
However, bias in the structural prediction due to steric hindrance at the C1A domain may complicate the interpretation of the data, as the SnuCalCp15 I29 domain does not accurately reflect the native structure of SnuCalCpI15. Therefore, the structure of SnuCalCpI15 was generated without the C1A domain (Fig. 3a). The reliable portion of the structural model of SnuCalCpI15 was consistent with the SnuCalCp15 I29 domain, although the C-terminal region after helix 3 was flexible and structurally unresolved.
Inhibitory characteristics of SnuCalCpI15 against CTSL. (a) Structural models of SnuCalCp15 and SnuCalCpI15. The segment corresponding to SnuCalCpI15 (I29 domain) is colored following the pLDDT score (range: 0–100). The catalytic diad at the active site cleft and propeptide binding loop (PBL) are shown in yellow and magenta, respectively. (b, c) Flexible docking analysis of SnuCalCpI15 using CTSL (b) and closed CTSB (c) as receptors. The mature enzyme and its zymogen are superimposed. The C1A domain, its native propeptide, and SnuCalCpI15 are shown in gray, green, and cyan, respectively. The occluding loop of CTSB is represented as red, blue, and dark green for closed CTSB (propeptide-free), proCTSB, and CTSB–SnuCalCpI15 complex, respectively. (d) Alignment of C-terminal residues of SnuCalCpI15 at the CTSL active site cleft. (e) Docking of substrate Z-Phe-Arg-AMC with CTSL (Vina score: −8.1).
SnuCalCpI15 binds stereoselectively to CTSL, unlike CTSB
A molecular docking simulation was conducted to investigate the selective inhibition of CTSL by SnuCalCpI15. The binding mode with the highest rank (docking score: -547.95, confidence score: 0.9997) between SnuCalCpI15 and CTSL showed that the propeptide − enzyme interaction was similar to that within proCTSL (Fig. 3b). In both cases, helix 3 was partially lodged on the S΄ subsites of the active site, while the loop immediately after the helix 3 occupied the active site cleft, thus hampering the access to the substrate. Similarly, the binding mode with the highest rank (docking score: -650.08, confidence score: 1.0000) between SnuCalCpI15 and CTSB showed that SnuCalCpI15 may mimic the CTSB propeptide (Fig. 3c). For both CTSB and CTSL, the loop region between helix 2 and helix 3 of SnuCalCpI15 was expected to play a pivotal role in moving the globular domain of SnuCalCpI15 toward the propeptide binding loop (PBL).
The docking analysis results suggested the potential of SnuCalCpI15 to inhibit CTSL and CTSB, which was contrary to the experimental data from Fig. 2. However, unlike CTSL, a marked displacement in the occluding loop was observed in CTSB. CTSB differs from canonical CTSL-like proteases in that it possesses an occluding loop (C108–C119) that restricts inhibitor access to the active site cleft depending on its position37. Therefore, displacing the occluding loop accommodates the binding region in the CTSB propeptide (from proCTSB) and CTSB-inhibitor complexes, which opens the CTSB38. However, the extent of the movement of the occluding loop was much larger for the CTSB–SnuCalCpI15 complex than proCTSB, to achieve blocking of the active site cleft and inhibit enzyme. Compared to the mature form of CTSB (closed form), the displacement of the N111-Cα atom inside the occluding loop was 6.7 Å for proCTSB, whereas it was 30.3 Å for the CTSB–SnuCalCpI15 complex (Fig. 3b, c). Furthermore, by using the open conformation of CTSB as a receptor for docking, SnuCalCpI15 was unable to interact with the propeptide binding loop and, thus, could not block the active site (Fig. S1). Therefore, we expected that SnuCalCpI15 would not be favorable for binding and changing the closed conformation of CTSB into its open form for inhibition, unlike CTSL.
K87–L89 were positioned at the CTSL S΄ subsites for SnuCalCpI15, while residues G90, T91, and R92 in the N-terminal portion of the connecting loop blocked the CTSL S1, S2, and S3 sites, respectively (Fig. 3d)13,25. Therefore, alignment of the C-terminal loop was favorable to block access to the substrate, Z-Phe-Arg-AMC (Fig. 3e). Additionally, the presence of Y84 at the S3΄ site, which is also a hotspot of protein-ligand affinity in reversible CTSL peptide-type inhibitors39, indicated that the overall SnuCalCpI15 binding mode toward CTSL hampered access of larger substrates (rather than Z-Phe-Arg-AMC, in this study), stereoselectively. The docking study provided structural insights into the stereoselectivity of SnuCalCpI15 for CTSL over CTSB. However, as the analysis relied on a structural model of SnuCalCpI15, further investigation (e.g., NMR) is necessary to characterize the protein dynamics of CTSL–SnuCalCpI15 complex and validate the actual structure.
SnuCalCpI15 inhibits intracellular and extracellular Z-Phe-Arg-AMC hydrolyzing activities in MDA-MB-231 breast cancer cells
Next, we evaluated whether SnuCalCpI15 applies to a human-derived breast cancer cell line. Based on previous studies, the MDA-MB-231 triple-negative breast cancer cell line with high CTSL expression, high CTSL secretion, and high metastatic potential among breast cancer cell lines was used for the experiment29,31. Cell viability was evaluated at different SnuCalCpI15 doses (0, 5, 10, and 20 µM) for 24 and 48 h using the MTT assay before determining the SnuCalCpI15 treatment concentration for MDA-MB-231 breast cancer cells (Fig. 4a). SnuCalCpI15 was non-toxic to MDA-MB-231 breast cancer cells at up to 20 µM during 24–48 h of exposure (109.5 ± 2.4 and 104.9 ± 1.2%), respectively. To verify whether SnuCalCpI15 entered the cells, FITC-labeled SnuCalCpI15 was observed with a confocal microscope (Fig. 4b). Interestingly, SnuCalCpI15 was localized in MDA-MB-231 breast cancer cells. Exposure of SnuCalCpI15 (20 µM) for 24 h resulted in changes of Z-Phe-Arg-AMC hydrolyzing activity in both culture media and cell lysates (represents extracellular and intracellular extract, respectively) from MDA-MB-231 breast cancer cells (Fig. 4c). The Z-Phe-Arg-AMC hydrolyzing activity of SnuCalCpI15 decreased by more than 20% in both intracellular and extracellular extracts (with relative activities of 74.8 ± 3.9% and 67.5 ± 3.5%, respectively). However, the reduction in activity in the intracellular extract was less marked compared to the canonical CTSL inhibitor Z-Phe-Tyr-CHO, which exhibited a relative activity of 52.6 ± 5.9%. Nevertheless, these results demonstrate that SnuCalCpI15 alters enzymatic activity (i.e., Z-Phe-Arg-AMC hydrolyzing activity) in human-derived breast cancer cells, but there are limitations in directly confirming its inhibitory effect on CTSL activity.
SnuCalCpI15 inhibits both intracellular and extracellular Z-Phe-Arg-AMC hydrolyzing activity in MDA-MB-231 breast cancer cells. (a) MDA-MB-231 breast cancer cells seeded in 96-well plates were treated with different doses (0, 5, 10, and 20 µM) of SnuCalCpI15 and Z-Phe-Tyr-CHO for 24 and 48 h. Cell viability was measured in MTT assays. (b) MDA-MB-231 breast cancer cells seeded in confocal plates were treated with FITC-labeled SnuCalCpI15 for 4 h. Representative FITC labeling images, phase-contrast microscopy images, and merged images are shown. Scale bar: 10 μm. (c) MDA-MB-231 breast cancer cells seeded in 60-mm culture plates were incubated with 20 µM SnuCalCpI15 and 20 µM Z-Phe-Tyr-CHO for 24 h, respectively. The medium and cell lysates were tested using a Z-Phe-Arg-AMC assay.
Anti-cancer agents targeting CTSL must prevent the altered traffic-driven secretion of the protease into the extracellular milieu and the resulting proteolytic degradation of ECM components that drive metastasis40,41. In contrast, the endogenous CTSL inhibitor cystatin is not internalized by endocytosis; rather, its anti-invasive properties involve inhibiting secreted CTSL, which is a major component of metastatic tumors42. Previous results have shown that SnuCalCpI15 can inhibit CTSL activity (Fig. 2), and considering its potential for internalization (Fig. 4b), it is anticipated that SnuCalCpI15 might also inhibit CTSL activity at the cellular level. Therefore, the results suggest that SnuCalCpI15 has potential as an anti-cancer agent with dual benefits due to its internalization capability. However, the inhibition of CTSL activity cannot be conclusively determined in vitro, as the substrate Z-Phe-Arg-AMC used in this study may also be acted upon by other cathepsins, such as CTSB or cathepsin S, which limits the ability to evaluate selective inhibition specifically against CTSL43.
SnuCalCpI15 suppresses metastasis of MDA-MB-231 breast cancer cells
Early-stage breast cancer can be treated surgically and/or with chemotherapy and/or radiotherapy, but patient survival decreases dramatically when metastasis occurs2,3. Therefore, therapeutic strategies and continued research aimed at preventing metastasis of breast cancer, and other tumors, are essential. Given the role of CTSL in promoting metastasis in various cancers, we examined whether high-level CTSL expression was correlated with the epithelial-mesenchymal transition (EMT)11. A gene set enrichment analysis (GSEA) of breast cancer tissue showed that high-level CTSL expression correlated positively with the EMT signature (Fig. 5a, b). The normalized enrichment scores of GSE12276 and GSE20194, were − 1.82 and − 1.59, respectively (p < 0.05). Therefore, we hypothesized that SnuCalCpI15 would suppress breast cancer metastasis by inhibiting CTSL activity. A wound-healing assay was carried out to determine whether SnuCalCpI15 suppressed the migration of breast cancer cells. Figure 5c shows representative images of MDA-MB-231 breast cancer cells after the 20 µM SnuCalCpI15 treatment for 24 h at 80–90% confluency, and Fig. 5d shows the quantification graph. The inhibitory activity of SnuCalCpI15 was as high as that of Z-Phe-Tyr-CHO. Furthermore, significant decreases in cell migration (cell number 36.7 ± 0.5%) and invasion (cell number 33.5 ± 10.9%) were observed in MDA-MB-231 breast cancer cells after 18 and 36 h incubation with 20 µM SnuCalCpI15, respectively (p < 0.001) (Fig. 5e, f). The Z-Phe-Tyr-CHO (20 µM) treatment also significantly reduced cell migration (p < 0.05, 66.9 ± 15.2%) and invasion (p < 0.01, 64.5 ± 9.5%), but was not as effective as SnuCalCpI15.
SnuCalCpI15 suppresses tumor metastasis in MDA-MB-231 breast cancer cells. (a, b) GSEA plot of breast cancer tissue divided into high and low CTSL groups. NES, normalized enrichment score. (c) MDA-MB-231 breast cancer cells were seeded in a 6-well plate. At 80–90% confluence, the cells were scratched using a 200-µL tip and treated with 20 µM SnuCalCpI15 and 20 µM Z-Phe-Tyr-CHO for 24 h. Representative images of the cell edge are shown. Scale bar: 200 μm. (d) The average number of wound-healing area in three random microscopic fields. (e) MDA-MB-231 breast cancer cells were seeded on an 8.0 μm pore size insert with 20 µM SnuCalCpI15 and incubated for 18–36 h. Representative images of the migrated and invaded cells are shown. Scale bar: 200 μm. (f) The average number of migrated and invaded cells in three random microscopic fields.
The overall results indicate that SnuCalCpI15, a high-molecular-weight protein inhibitor with a molecular mass of 15 kDa, was more effective at suppressing breast cancer metastasis than the canonical dipeptide aldehyde inhibitor Z-Phe-Tyr-CHO (Fig. 5c, f). As peptidic aldehyde inhibitors react with the CTSL active site to form thiohemiacetal adducts, they are characterized as reversible covalent inhibitors44. However, as shown in Fig. 3b, SnuCalCpI15 suppresses CTSL activity via stereoselective protein–protein interactions by mimicking the propeptide region in the CTSL zymogen25. Therefore, the Z-Phe-Tyr-CHO binding mode of the inhibitor differed from that of SnuCalCpI15 (Fig. 3b, S2). Because reversible slow-binding provides a longer residence time, prolonged efficacy, and enhanced selectivity45, the unique SnuCalCpI15 binding mode may endow higher anti-cancer activity via a different CTSL inhibitory mechanism.
Blocking CTSL activity suppresses tumor metastasis similar to SnuCalCpI15 in MDA-MB-231 breast cancer cells
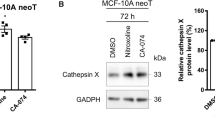
As a high level of CTSL expression was positively correlated with the EMT signature (Fig. 5a, b), the SnuCalCpI15 inhibitory mechanism was investigated by blocking CTSL activity in MDA-MB-231 breast cancer cells. Transfection with si-CTSL resulted in a significant reduction (p < 0.001) in CTSL mRNA (0.036 ± 0.005 and 0.032 ± 0.011 for si-CTSL #1 and si-CTSL #2, respectively) in cell lysates, compared with si-NTC (1.006 ± 0.147), as analyzed by qPCR (Fig. 6a). Western blotting was carried out to confirm the blockage of CTSL expression by si-CTSL treatment (Fig. 6b, full-length blot image: Fig. S4). The decrease in CTSL expression by the siRNAs significantly inhibited tumor metastasis in MDA-MB-231 breast cancer cells. Figure 6c shows representative images of MDA-MB-231 breast cancer cells after 24 h of treatment with si-NTC and si-CTSL at 80–90% confluency, and Fig. 6d shows the quantification graph. The inhibitory activity against wound healing was higher in si-CTSL than in si-NTC. As shown in Fig. 6e, f, significant decreases in cell migration (cell numbers 54.6 ± 1.8 and 49.9 ± 3.1%) and invasion (cell numbers 62.1 ± 9.7 and 58.6 ± 2.1%) were observed for MDA-MB-231 breast cancer cells after 18 and 36 h of transfection (48 h) of CTSL #1 and si-CTSL #2, respectively, compared with that of si-NTC (p < 0.01). These results indicate that blocking CTSL activity suppresses metastasis of MDA-MB-231 breast cancer cells as observed for SnuCalCpI15.
Blocking CTSL activity suppresses tumor metastasis similar to SnuCalCpI15 in MDA-MB-231 breast cancer cells. (a, b) MDA-MB-231 breast cancer cells were transfected with si-NTC or si-CTSL for 48 h. Cell lysates were analyzed by qPCR (a) and Western blotting (b). The uncropped blot of western blotting is shown in Supplementary Fig. S4. (c) MDA-MB-231 breast cancer cells transfected with si-NTC or si-CTSL for 48 h were grown to 80–90% confluence, then scratched using a 200 µL tip and incubated for 24 h. Representative images of the cell edge are shown. Scale bar: 200 μm. (d) The average number of wound-healing area in three random microscopic fields. (e) MDA-MB-231 breast cancer cells were transfected with si-NTC or si-CTSL for 48 h and then seeded on an 8.0 μm pore size insert for 18–36 h. Representative images of the migrated and invaded cells are shown. Scale bar: 200 μm. (f) The average numbers of migrated and invaded cells in three random microscopic fields.
Nevertheless, nonspecific bands were observed in the Western blot experiment (Fig. 6b). The anti-CTSL antibody used in this study is a polyclonal antibody. Polyclonal antibodies offer certain advantages such as broad epitope recognition, robustness, and cost-effectiveness, making them useful in many research and diagnostic applications. However, limitations including batch-to-batch variability, cross-reactivity, and low specificity should be carefully considered when selecting antibodies for specific applications. In this study, multiple bands were identified during CTSL protein analysis, but the location of CTSL could be clearly identified by utilizing si-RNA targeting two different sequences. Future studies will utilize monoclonal antibodies to improve these limitations.
Conclusions
In summary, this study revealed the inhibitory characteristics of SnuCalCpI15, an I29 segment of a CTSL-like cysteine protease against CTSL, and elucidated its potential as a high molecular anti-cancer agent in breast cancer metastasis by inhibiting CTSL activity. Based on the GSEA, we showed that CTSL expression was higher in breast cancer tissues compared to normal tissues, and that high CTSL expression was closely associated with low survival and the EMT signature of the tumor. Molecular docking and kinetic studies unraveled the stereoselective and slow binding mode of SnuCalCpI15 inhibitory activity against CTSL. In MDA-MB-231 breast cancer cells, SnuCalCpI15 was internalized, indicating its dual advantages as an anti-cancer agent. Reduced tumor cell migration and invasion suggested that SnuCalCpI15 has the potential to inhibit tumor metastasis in breast cancer by inhibiting CTSL activity. Nevertheless, the limitation of this study is the in vivo application of SnuCalCpI15. Recently, excellent protein-derived therapeutics have been developed one after another. However, protein therapeutics have clear limitations such as stability, immune response induction, administration route, and permeability. SnuCalCpI15 used in this study was confirmed to be a protein-derived substance that inhibits CTSL in vitro, but in order to verify it in vivo, it is necessary to overcome various limitations presented above. This will be a subject of future research.
Methods
Plant material
Cultivation and preparation of C. procera R. Br. were conducted following the previous method23. C. procera R. Br., cultivated in Myanmar, was kindly provided by 3 M Korea Ltd. (Seoul, South Korea). It was identified by Dr. Byoung-Cheorl Kang (Seoul National University) and grown in a greenhouse at the agricultural experiment farm of Seoul National University in Suwon, South Korea. The experimental research of the plant material used in this study complies with relevant institutional, national, and international guidelines and legislation.
Antibodies and reagents
Primary anti-CTSL antibodies (polyclonal) were purchased from Santa Cruz Biotechnology (Santa Cruz, CA, USA) and Abclonal Technology (Wuhan, China). Anti-α-tubulin antibody (monoclonal) was purchased from Abbkine (Wuhan, China). Horseradish peroxidase (HRP)-tagged anti-mouse and anti-rabbit secondary antibodies were purchased from Enzo Life Science (Farmingdale, NY, USA). 3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) was purchased from Duchefa Biochemie (Haarlem, Netherlands), and dimethyl sulfoxide (DMSO) from Junsei Chemical Co., Ltd. (Tokyo, Japan). Papain (CAS 9001-73-4), bromelain (CAS 37189-34-7), DL-Dithiothreitol (DTT), Cathpsin L inhibitor II (Z-Phe-Tyr-CHO), Z-Phe-Arg 7-amido-4-methylcoumarin hydrochloride (Z-Phe-Arg-AMC), and 7-amino-4-methyl coumarin (AMC) were purchased from Sigma-Aldrich (St. Louis, MO, USA). Human recombinant CTSL and cathepsin B (CTSB) were purchased from BioVision, Inc. (Waltham, MA, USA).
Cell culture
MDA-MB-231 breast cancer cells were obtained from the American Type Culture Collection and maintained in DMEM (Capricorn Scientific GmbH, Ebsdorfergrund, Germany) containing 10% fetal bovine serum (FBS; Capricorn Scientific GmbH) and 1% penicillin/streptomycin (Capricorn Scientific GmbH). The cells were incubated in a 5% CO2 incubator at 37 °C.
Heterologous expression and purification of SnuCalCpI15
SnuCalCpI15 was heterologously expressed in E. coli as described previously (Kwon et al. 2022a). The cDNA was synthesized using a PrimeScript™ First-Strand cDNA Synthesis Kit (Takara, Otsu, Japan) using total RNA extracted from lyophilized young leaves of C. procera. A partial cDNA fragment encoding a putative I29 domain was separated from the C1A domain of SnuCalCp15 and inserted into the vector pET29b(+) for expression in E. coli BL21 (DE3) Star (Invitrogen, Carlsbad, CA, USA). Expression was induced using 0.5 mM IPTG after the cells had reached the mid-exponential phase, followed by continuous shaking at 18 °C for 16 h. Cell lysates were prepared by probe sonication (10 s pulse, 10 cycles, and 35% power) of the harvested cells. The lysates were centrifuged at 12,000 g for 20 min and the supernatant was dialyzed against 50 mM Tris-HCl (pH 8.0) for 12 h at 4 °C. His-tagged SnuCalCpI15 was purified on a column pre-packed with QIAexpress Ni-NTA Agarose (Qiagen, Hilden, Germany). The protein was ultra-filtrated with 50 mM phosphate-buffered saline (PBS; pH 7.4) and filter-sterilized prior to its use.
Cysteine protease inhibition assay
The activity of purified SnuCalCpI15 was assayed in 50 mM sodium phosphate (pH 6.4) containing 5 mM EDTA and 1 mM DTT. The fluorogenic substrate Z-Phe-Arg-AMC was first dissolved in DMSO at a concentration of 1 mM and diluted with distilled water. Four enzymes (bromelain, papain, CTSB, and CTSL) were used to profile the inhibitory activity of SnuCalCpI15 against C1A-type cysteine proteases. Enzyme concentrations at which the concentration of AMC produced increased proportionally with reaction time when no inhibitor was present were used for experiment; bromelain, 20 nM; papain, 2 nM; CTSB, 0.4 nM; CTSL, 0.2 nM. First, 50 µL of SnuCalCpI15 at various concentrations was mixed with 100 µL of the substrate solution in 96-well microplates. After a 5 min incubation at 37 °C, the reaction was initiated by adding 50 µL of the enzyme solution with continuous stirring. The liberation of AMC was monitored at excitation and emission wavelengths of 355 and 460 nm, respectively. A SpectraMax® iD3 Plate Reader (Molecular Devices, LLC, San Jose, CA, USA) was used to measure the fluorescence intensity. A standard curve of AMC was generated to quantify the concentration of SnuCalCpI15.
Proteolytic digestion of SnuCalCpI15
To determine whether SnuCalCpI15 is degraded by cysteine proteases, the same concentrations of enzymes used previously (bromelain, 20 nM; papain, 2 nM; CTSB, 0.4 nM; CTSL, 0.2 nM) were mixed with SnuCalCpI15 (10 µM) in a 1.5-mL microcentrifuge tube and incubated at 37 °C for 1 h with continuous shaking. The reaction was sampled at 0, 15, 30, and 60 min and analyzed by SDS-PAGE on a 12% (v/v) resolving gel. Proteolytic degradation of SnuCalCpI15 was detected through the decrease of corresponding band intensity (15 kDa).
Determination of inhibitory kinetic parameters
SigmaPlot 12.5 (Systat Software, Inc., San Jose, CA, USA) was used to fit the experimental data in the non-linear regression analyses. To determine the half-maximal inhibitory concentration (IC50) of the respective protease, hydrolytic activity was measured in the presence of 100 nM–10 mM of inhibitor. The IC50 value of the respective protease was derived in four-parameter logistic curves46:
where \(\:y\) and \(\:x\) are the relative activity and concentration of the inhibitor, respectively. The lower asymptote, slope factor, and upper asymptote correspond to \(\:a\), \(\:b,\) and \(\:c\), respectively.
To determine the slow-binding inhibition kinetic parameters of SnuCalCpI15 towards CTSL, progress curves were fitted to the following Eq. (3)5:
where \(\:\left[\text{P}\right]\) is the concentration of the hydrolyzed products (AMC), \(\:{v}_{\text{i}}\) is the initial velocity of the reaction, \(\:{v}_{\text{s}}\) is the final steady velocity of the reaction, \(\:t\) is the reaction time, and \(\:{k}_{\text{obs}}\) is the rate constant for inhibition.
To estimate the mechanism of SnuCalCpI15 inhibition, i.e., simple reversible slow-binding enzyme isomerization or affinity labeling, \(\:{k}_{\text{obs}}\) was plotted as a function of the inhibitor concentration47. Afterward, following equation was used to determine the inhibitory parameters; a simple reversible slow-binding reaction where Ki is the inhibitory dissociation constant (koff / kon) and koff is one of the pre-steady state kinetic parameters in the relationship35:
Cell viability and wound healing assay
Cell viability was assayed using MDA-MB-231 breast cancer cells seeded in a 96-well plate (2 × 104 cells/well, SPL Life Sciences, Pocheon, Republic of Korea). The next day, SnuCalCpI15 and Z-Phe-Tyr-CHO were dose-dependently treated (0, 5, 10, and 20 µM) for 24 and 48 h, respectively, followed by MTT reagent for 2 h. The resulting purple formazan crystals were solubilized with DMSO and the absorbance at 570 nm was determined using a plate reader (Tecan, Männedorf, Switzerland). Wound healing was assayed using MDA-MB-231 breast cancer cells seeded in a 6-well plate (1 × 106 cells/well, SPL Life Sciences). When the cells reached 80–90% confluence, they were scratched using a 200-µL tip and treated with SnuCalCpI15 or Z-Phe-Tyr-CHO (20 µM) for 24 h. The migrated cells were analyzed using a microscope (Nikon Instruments Inc., Melville, NY, USA).
Transwell migration & invasion assay
MDA-MB-231 breast cancer cells in serum-free medium were seeded in a 24-well upper chamber on 8.0-µm pore size inserts (1 × 105 cells/well, Corning Life Sciences, Tewksbury, MA, USA). The medium in the lower chamber contained 10% (v/v) FBS to induce chemotaxis. The cells were then treated or not with SnuCalCpI15 (20 µM). After 18 h, the cells in the upper chamber were fixed and stained using a Diff-Quick Solution Kit (Sysmex Corp., Kobe, Japan). For invasion assays, the inserts were pre-coated with Matrigel Matrix solution (No. 356231, Corning Life Sciences) diluted 10-fold in serum-free medium before the cells were seeded. Z-Phe-Tyr-CHO was used for comparison.
Evaluation of in vitro Z-Phe-Arg-AMC hydrolyzing activity
MDA-MB-231 breast cancer cells seeded in 60 mm culture plates (1 × 106 cells/well, SPL Life Sciences) were incubated with 20 µM SnuCalCpI15 for 24 h. The cell culture medium was centrifuged at 1,300 rpm for 5 min to remove cell debris and then used in the experiment. The cells were rinsed three times with PBS, scraped carefully from the plate with a scraper, and centrifuged at 1,300 rpm for 5 min. They were then resuspended in 0.5 mL of 25 mM PBS and mixed thoroughly by gentle rocking at 4 °C for 1 h. Subsequently, the cells were disrupted by probe sonication using four 1 min pulses (36 cycles, 30% power) with an interval of 10 s. Cell lysates were prepared by centrifugation at 3,000 g for 5 min. The medium was ultra-filtrated with 25 mM PBS and 10-fold concentrated using a Pierce™ Protein Concentrator PES (Thermo Fisher Scientific, Waltham, MA, USA; 10 kDa cut-off) for further analysis. The medium and cell lysates were prepared as described above and changes in Z-Phe-Arg-AMC hydrolyzing activity were monitored for 50 min.
FITC-labeling
FITC-conjugated SnuCalCpI15 was prepared using the FluoReporter™ FITC protein labeling kit (Thermo Fisher Scientific) according to the manufacturer`s instructions. Briefly, SnuCalCpI15 was buffer-exchanged in 0.1 M sodium carbonate buffer (pH 9.0) at a concentration of 2 mg/mL. The reaction was initiated by the addition of 35 µL of 10 mg FITC/mL prepared in DMSO, followed by a 1 h incubation at 25 °C in the dark. FITC-labeled SnuCalCpI15 was purified on spin column resin and eluted with 200 µL of PBS. MDA-MB-231 breast cancer cells were seeded in 60 mm confocal dishes (SPL Life Sciences) and then treated with FITC-labeled SnuCalCpI15 for 4 h. After three rinses of the cells with PBS, their fluorescence was monitored using a confocal microscope (Leica Microsystems, Wetzlar, Germany).
siRNA transfection
The knock-down of CTSL expression was obtained by transfecting cells for 48 h with si-NTC (negative control, SI1027280; Qiagen) or si-CTSL (SI03117660 and SI00029897; Qiagen) using RNAiMax Reagent (Invitrogen, Waltham, MA, USA) according to the manufacturer’s protocol (Thermo Fisher Scientific).
Western blotting
Cells were lysed on ice with 1% (w/v) Triton X-100 lysis buffer containing protease inhibitors and phosphatase inhibitors. Proteins were separated by SDS-PAGE and then transferred to a nitrocellulose membrane (GE Healthcare Life Sciences, Chicago, IL, USA). The membrane was blocked for 1 h with 5% skim milk (LPS Solution, Daejeon, Republic of Korea) and then incubated with primary antibodies on an orbital shaker overnight at 4 °C. The next day, the membrane was incubated with HRP-conjugated secondary antibodies on an orbital shaker for 2 h at room temperature. The protein bands were visualized using an ECL Detection Kit (BioMax, Seoul, Republic of Korea).
Quantitative real-time polymerase chain reaction (qPCR)
Total RNA was isolated using RNAiso Plus (Takara) and cDNA was synthesized using ReverTra Ace qPCR RT Master Mix (Toyobo, Osaka, Japan) according to the manufacturer’s protocols. qPCR was performed using BlasTaq 2X qPCR MasterMix (Applied Biological Materials, Richmond, Canada); fluorescent signals were detected using a CFX Connect Real-time PCR Detection System (Bio-Rad Laboratories, Hercules, CA, USA). The qPCR primer sequences were as follows: CTSL forward, 5′ AAACACAGCTTCACAATGGCC 3′; CTSL reverse 5′ TTTGAAAGCCATTCATCACCTG 3′; GAPDH forward, 5′ CTGACTTCAACAGCGACACC 3′ and GAPDH reverse, 5′ TAGCCAAATTCGTTGTCATACC 3′.
Immunohistochemistry
Breast cancer tissues were provided by Seoul National University Hospital after approval from the Institutional Review Board (no. 1904-141-1029). The tissues were fixed in 4% (v/v) paraformaldehyde overnight at 4 °C and embedded in paraffin. Section (4 μm thick) were prepared from the paraffin blocks, deparaffinized with xylene, and hydrated in a graded ethanol series. Antigen was unmasked by boiling the sections in 100 mM citrate buffer (pH 6.0) for 10 min. Endogenous peroxidase activity was blocked by incubation with 3% hydrogen peroxide for 10 min. The slides were blocked for 1 h in 5% normal goat serum (Vector Laboratories, Burlingame, CA, USA), incubated first with primary CTSL antibodies (1:250) overnight at 4 °C in a humidified chamber and then for 1 h with biotin-conjugated secondary antibodies (Vector Laboratories), followed by a 1 h incubation with avidin-biotin complex (Vector Laboratories). The slides were stained with DAB (Dako, Santa Clara, CA, USA) and then counterstained with hematoxylin (Dako). Images of the stained tissues were analyzed using a LAS microscope (Leica Microsystems); relative CTSL expression was quantified using ImageJ.
Public databases and ethics approval
The databases used in this study were GSE5364, GS3744, GSE12276, and GSE20194 (https://www.ncbi.nlm.nih.gov/geo). Kaplan-Meier plots were generated to analyze the OS and RFS of breast cancer patients according to CTSL expression (http://kmplot.com/analysis/)48. GSEA was performed to analyze the enrichment of the tumor signature gene sets in breast cancer according to CTSL expression (https://www.gsea-msigdb.org). The patient tissues used in this study was tissue that had already been surgically removed and stored. The Seoul National University Hospital Institutional Review Board (IRB) committee may waive the informed consent of the subject by submitting a waiver of informed consent in the following two cases: (1) When obtaining the subject’s consent during the research process is practically impossible or would seriously affect the validity of the research. (2) When there is no reason to assume that the subject will refuse consent and the risk to the subject even if consent is waived is extremely low. Therefore, a waiver of informed consent was submitted and this document was verified and approved by the IRB. All procedures were approved by IRB (IRB No. 1904-141-1029), complied with the Declaration of Helsinki and the International Conference on Harmonization-Good Clinical Practice (ICH-GCP), and conducted following the ICH-GCP guidelines.
Structural modeling and docking analysis
The three-dimensional structures of SnuCalCp15 and SnuCalCpI15 were modeled using AlphaFold249. The amino acid sequence was deduced from the nucleotide sequences reported previously27. Flexible protein-protein docking was carried out using HDOCK server50. The 3D structures of CTSL (C1A of AlphafoldDB: AF-P07711-F1)51 and CTSB (PDB: 1HUC, closed form)52 were used as receptors. The structure of the CTSB-stefin A complex (PDB: 3K9M)38 was used to mimic the open CTSB conformation. Zymogen structures were used for comparison; proCTSL (AlphafoldDB: AF-P07711-F1)51 and proCTSB (PDB: 2PBH)53. Molecular docking of the substrate, Z-Phe-Arg-AMC, was performed based on the cavity detection of CTSL using CB-Dock254.
Statistical analysis
Statistical analyses were performed with Microsoft Excel (Redmond, WA, USA). Results are reported as the mean ± standard deviation of at least three replicate independent experiments. All significances were determined using an unpaired Student’s t-test (*p < 0.05, **p < 0.01, and ***p < 0.001).
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
American Cancer Society. Cancer Facts & Fig. Cancer Statistics (2022). https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2022.html (2022).
Weigelt, B. & Peterse, J. L. T veer, L. J. Breast cancer metastasis: Markers and models. Nat. Rev. Cancer. 5, 591–602. https://doi.org/10.1038/nrc1670 (2005). van.
Dahan, M., Cortet, M., Lafon, C. & Padilla, F. Combination of focused ultrasound, immunotherapy, and chemotherapy. J. Ultrasound Med. 42, 559–573. https://doi.org/10.1002/jum.16053 (2023).
Lei, S. et al. Global patterns of breast cancer incidence and mortality: A population-based cancer registry data analysis from 2000 to 2020. Cancer Commun. (Lond). 41, 1183–1194. https://doi.org/10.1002/cac2.12207 (2021).
Caputo, R. et al. Sacituzumab Govitecan for the treatment of advanced triple negative breast cancer patients: A multi-center real-world analysis. Front. Oncol. 14, 1362641. https://doi.org/10.3389/fonc.2024.1362641 (2024).
Rizzo, A., Cusmai, A., Acquafredda, S., Rinaldi, L. & Palmiotti, G. Ladiratuzumab vedotin for metastatic triple negative cancer: preliminary results, key challenges, and clinical potential. Expert Opin. Investig. Drugs. 31, 495–498. https://doi.org/10.1080/13543784.2022.2042252 (2022).
Rizzo, A. et al. Hypertransaminasemia in cancer patients receiving immunotherapy and immune-based combinations: the MOUSEION-05 study. Cancer Immunol. Immunother. 72, 1381–1394. https://doi.org/10.1007/s00262-023-03366-x (2023).
Schipilliti, F. M. et al. Datopotamab deruxtecan: a novel antibody drug conjugate for triple-negative breast cancer. Heliyon. 10, e28385. https://doi.org/10.1016/j.heliyon.2024.e28385 (2024).
Guven, D. C. et al. Immune checkpoint inhibitor-related hearing loss: A systematic review and analysis of individual patient data. Support Care Cancer. 31, 624. https://doi.org/10.1007/s00520-023-08083-w (2023).
Guven, D. C. et al. The association between albumin levels and survival in patients treated with immune checkpoint inhibitors: A systematic review and meta-analysis. Front. Mol. Biosci. 9, 1039121. https://doi.org/10.3389/fmolb.2022.1039121 (2022).
Tan, G. J., Peng, Z. K., Lu, J. P. & Tang, F. Q. Cathepsins mediate tumor metastasis. World J. Biol. Chem. 4, 91–101. https://doi.org/10.4331/wjbc.v4.i4.91 (2013).
Rawlings, N. D. et al. The MEROPS database of proteolytic enzymes, their substrates and inhibitors in 2017 and a comparison with peptidases in the PANTHER database. Nucleic Acids Res. 46, 624–632. https://doi.org/10.1093/nar/gkx1134 (2017).
Sudhan, D. R. & Siemann, D. W. Cathepsin L targeting in cancer treatment. Pharmacol. Ther. 155, 105–116. https://doi.org/10.1016/j.pharmthera.2015.08.007 (2015).
Lah, T. T. et al. Stefins and lysosomal cathepsins B, L and D in human breast carcinoma. Int. J. Cancer. 50, 36–44. https://doi.org/10.1002/ijc.2910500109 (1992).
Thomssen, C. et al. Prognostic value of the cysteine proteases cathepsins B and cathepsin L in human breast cancer. Clin. Cancer Res. 1, 741–746 (1995).
Ruan, J. et al. Increased expression of cathepsin L: A novel independent prognostic marker of worse outcome in hepatocellular carcinoma patients. PLoS One. 9, e112136. https://doi.org/10.1371/journal.pone.0112136 (2014).
Zhang, L. et al. Cathepsin L is involved in proliferation and invasion of ovarian cancer cells. Mol. Med. Rep. 11, 468–474. https://doi.org/10.3892/mmr.2014.2706 (2015).
Rawlings, N. D., Tolle, D. P. & Barrett, A. J. Evolutionary families of peptidase inhibitors. Biochem. J. 378, 705–716. https://doi.org/10.1042/bj20031825 (2004).
Pogorzelska, A., Żołnowska, B. & Bartoszewski, R. Cysteine cathepsins as a prospective target for anticancer therapies-current progress and prospects. Biochimie. 151, 85–106. https://doi.org/10.1016/j.biochi.2018.05.023 (2018).
Hanada, K. et al. Isolation and characterization of E–64, a new thiol protease inhibitor. Agric. Biol. Chem. 42, 523–528. https://doi.org/10.1080/00021369.1978.10863014 (1978).
Katunuma, N., Tsuge, H., Nukatsuka, M., Asao, T. & Fukushima, M. Structure-based design of specific cathepsin inhibitors and their application to protection of bone metastases of cancer cells. Arch. Biochem. Biophys. 397, 305–311. https://doi.org/10.1006/abbi.2001.2709 (2002).
Cianni, L. et al. Can cysteine protease cross-class inhibitors achieve selectivity? J. Med. Chem. 62, 10497–10525. https://doi.org/10.1021/acs.jmedchem.9b00683 (2019).
Kwon, C. W., Yeo, S. & Chang, P. S. Characterization and molecular docking study of cathepsin L inhibitory peptides (SnuCalCpIs) from Calotropis procera R. Br. Sci. Rep. 12, 5825. https://doi.org/10.1038/s41598-022-09854-x (2022).
Shi, X. & Zhang, Y. A humanized antibody inhibitor for cathepsin L. Protein Sci. 29, 1924–1930. https://doi.org/10.1002/pro.3913 (2020).
Coulombe, R. et al. Structure of human procathepsin L reveals the molecular basis of inhibition by the prosegment. Embo J.15, 5492–5503 (1996).
Jerala, R., Zerovnik, E., Kidric, J. & Turk, V. pH-induced conformational transitions of the propeptide of human cathepsin L. A role for a molten globule state in zymogen activation. J. Biol. Chem.273, 11498–11504. https://doi.org/10.1074/jbc.273.19.11498 (1998).
Kwon, C. W. et al. Cysteine protease profiles of the medicinal plant Calotropis procera R. Br. revealed by de novo transcriptome analysis. PLoS One 10, e0119328, doi: (2015). https://doi.org/10.1371/journal.pone.0119328
Han, H. L., Kwon, C. W., Choi, Y. & Chang, P. S. Antifungal activity of α-helical propeptide SnuCalCpI15 derived from Calotropis procera R. Br. Against food spoilage yeasts. Food Control. 133, 108628. https://doi.org/10.1016/j.foodcont.2021.108628 (2022).
Qin, G. et al. Cathepsin L is involved in proliferation and invasion of breast cancer cells. Neoplasma. 63, 30–36. https://doi.org/10.4149/neo_2016_004 (2016).
Harbeck, N. et al. Prognostic impact of tumor biological factors on survival in node-negative breast cancer. Anticancer Res. 18, 2187–2197 (1998).
Sudhan, D. R., Rabaglino, M. B., Wood, C. E. & Siemann, D. W. Cathepsin L in tumor angiogenesis and its therapeutic intervention by the small molecule inhibitor KGP94. Clin. Exp. Metastasis. 33, 461–473. https://doi.org/10.1007/s10585-016-9790-1 (2016).
Zhang, L. et al. COVID-19 receptor and malignant cancers: Association of CTSL expression with susceptibility to SARS-CoV-2. Int. J. Biol. Sci. 18, 2362–2371. https://doi.org/10.7150/ijbs.70172 (2022).
Huang, Z. Impact of impurities on IC50 values of P450 inhibitors. Drug Metab. Lett. 5, 156–162. https://doi.org/10.2174/187231211796905008 (2011).
Böttger, R., Hoffmann, R. & Knappe, D. Differential stability of therapeutic peptides with different proteolytic cleavage sites in blood, plasma and serum. PLoS One. 12, e0178943. https://doi.org/10.1371/journal.pone.0178943 (2017).
Morrison, J. F. The slow-binding and slow, tight-binding inhibition of enzyme-catalysed reactions. Trends Biochem. Sci. 7, 102–105. https://doi.org/10.1016/0968-0004(82)90157-8 (1982).
Abbasi, W. A., Yaseen, A., Hassan, F. U., Andleeb, S. & Minhas, F. U. A. A. ISLAND: in-silico proteins binding affinity prediction using sequence information. BioData Min. 13, 20. https://doi.org/10.1186/s13040-020-00231-w (2020).
Quraishi, O. et al. The occluding loop in cathepsin B defines the pH dependence of inhibition by its propeptide. Biochem. 38, 5017–5023. https://doi.org/10.1021/bi981950o (1999).
Renko, M., Požgan, U., Majera, D. & Turk, D. Stefin A displaces the occluding loop of cathepsin B only by as much as required to bind to the active site cleft. FEBS J. 277, 4338–4345. https://doi.org/10.1111/j.1742-4658.2010.07824.x (2010).
Chowdhury, S. F. et al. Exploring inhibitor binding at the S′ subsites of cathepsin L. J. Med. Chem. 51, 1361–1368. https://doi.org/10.1021/jm701190v (2008).
Levicar, N. et al. Selective suppression of cathepsin L by antisense cDNA impairs human brain tumor cell invasion in vitro and promotes apoptosis. Cancer Gene Ther. 10, 141–151. https://doi.org/10.1038/sj.cgt.7700546 (2003).
Novinec, M. et al. Interaction between human cathepsins K, L, and S and elastins: Mechanism of elastinolysis and inhibition by macromolecular inhibitors. J. Biol. Chem. 282, 7893–7902. https://doi.org/10.1074/jbc.M610107200 (2007).
Gianotti, A., Sommer, C. A., Carmona, A. K. & Henrique-Silva, F. Inhibitory effect of the sugarcane cystatin CaneCPI-4 on cathepsins B and L and human breast cancer cell invasion. Biol. Chem. 389, 447–453. https://doi.org/10.1515/bc.2008.035 (2008).
Creasy, B. M., Hartmann, C. B., White, F. K. & McCoy, K. L. New assay using fluorogenic substrates and immunofluorescence staining to measure cysteine cathepsin activity in live cell subpopulations. Cytometry A. 71, 114–123. https://doi.org/10.1002/cyto.a.20365 (2007).
Zhu, J. et al. Self-masked aldehyde inhibitors of human cathepsin L are potent anti-CoV-2 agents. Front. Chem. 10, 867928. https://doi.org/10.3389/fchem.2022.867928 (2022).
Masson, P. & Lushchekina, S. V. Slow-binding inhibition of cholinesterases, pharmacological and toxicological relevance. Arch. Biochem. Biophys. 593, 60–68. https://doi.org/10.1016/j.abb.2016.02.010 (2016).
Sebaugh, J. L. Guidelines for accurate EC50/IC50 estimation. Pharm. Stat. 10, 128–134. https://doi.org/10.1002/pst.426 (2011).
Cha, S. Tight-binding inhibitors-I. kinetic behavior. Biochem. Pharmacol. 24, 2177–2185. https://doi.org/10.1016/0006-2952(75)90050-7 (1975).
Győrffy, B. Survival analysis across the entire transcriptome identifies biomarkers with the highest prognostic power in breast cancer. Comput. Struct. Biotechnol. J. 19, 4101–4109. https://doi.org/10.1016/j.csbj.2021.07.014 (2021).
Mirdita, M. et al. ColabFold: making protein folding accessible to all. Nat. Methods. 19, 679–682. https://doi.org/10.1038/s41592-022-01488-1 (2022).
Yan, Y., Zhang, D., Zhou, P., Li, B. & Huang, S. Y. HDOCK: a web server for protein-protein and protein-DNA/RNA docking based on a hybrid strategy. Nucleic Acids Res. 45, 365–373. https://doi.org/10.1093/nar/gkx407 (2017).
Varadi, M. et al. AlphaFold protein structure database: Massively expanding the structural coverage of protein-sequence space with high-accuracy models. Nucleic Acids Res. 50, 439–444. https://doi.org/10.1093/nar/gkab1061 (2021).
Musil, D. et al. The refined 2.15 Å X-ray crystal structure of human liver cathepsin B: The structural basis for its specificity. Embo J. 10, 2321–2330. https://doi.org/10.1002/j.1460-2075.1991.tb07771.x (1991).
Turk, D., Podobnik, M., Kuhelj, R., Dolinar, M. & Turk, V. Crystal structures of human procathepsin B at 3.2 and 3.3 angstroms resolution reveal an interaction motif between a papain-like cysteine protease and its propeptide. FEBS Lett. 384, 211–214. https://doi.org/10.1016/0014-5793(96)00309-2 (1996).
Liu, Y. et al. CB-Dock2: Improved protein-ligand blind docking by integrating cavity detection, docking and homologous template fitting. Nucleic Acids Res. 50, 159–164. https://doi.org/10.1093/nar/gkac394 (2022).
Acknowledgements
This work was supported by the Cooperative Research Program for Agriculture Science & Technology Development (Project No. RS-2021-RD009467) provided by the Rural Development Administration, Republic of Korea. This work was also supported by the “National Research Foundation of Korea” grant funded by the Korean Government (NRF-2022R1A2C1011914 and NRF-2018R1A5A2025964).
Author information
Authors and Affiliations
Contributions
Yong-Jin Kwon and Juno Lee: Conceptualization, Data curation, Investigation, Project administration, Writing – original draft. Eun-Bi Seo: Investigation. Juchan Lee and Jaehyeon Park: Methodology. Seul-Ki Kim: Investigation. Hyunjong Yu: Data curation. Sang-Kyu Ye and Pahn-Shick Chang: Conceptualization, Supervision, Project administration, Funding acquisition, Writing - Review & Editing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics declarations
This research was approved by the SNUH Institutional Review Board (No. 1904-141-1029). All experiments complied with the Declaration of Helsinki and International Conference on Harmonization-Good Clinical Practice.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kwon, YJ., Lee, J., Seo, EB. et al. Cysteine protease I29 propeptide from Calotropis procera R. Br. As a potent cathepsin L inhibitor and its suppressive activity in breast cancer metastasis. Sci Rep 14, 23218 (2024). https://doi.org/10.1038/s41598-024-73578-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-73578-3
- Springer Nature Limited