Abstract
Background
Clinical examination of patients with chronic lumbar radiculopathy aims to clarify whether there is nerve root impingement. The aims of this study were to investigate the association between findings at clinical examination and nerve root impingement, to evaluate the accuracy of clinical index tests in a specialised care setting, and to see whether imaging clarifies the cause of chronic radicular pain.
Methods
A total of 116 patients referred with symptoms of lumbar radiculopathy lasting more than 12 weeks and at least one positive index test were included. The tests were the straight leg raising test, and tests for motor muscle strength, dermatome sensory loss, and reflex impairment. Magnetic resonance imaging (n = 109) or computer tomography (n = 7) were imaging reference standards. Images were analysed at the level of single nerve root(s), and nerve root impingement was classified as present or absent. Sensitivities, specificities, and positive and negative likelihood ratios (LR) for detection of nerve root impingement were calculated for each individual index test. An overall clinical evaluation, concluding on the level and side of the radiculopathy, was performed.
Results
The prevalence of disc herniation was 77.8%. The diagnostic accuracy of individual index tests was low with no tests reaching positive LR >4.0 or negative LR <0.4. The overall clinical evaluation was slightly more accurate, with a positive LR of 6.28 (95% CI 1.06–37.21) for L4, 1.74 (95% CI 1.04–2.93) for L5, and 1.29 (95% CI 0.97–1.72) for S1 nerve root impingement. An overall clinical evaluation, concluding on the level and side of the radiculopathy was also performed, and receiver operating characteristic (ROC) analysis with area under the curve (AUC) calculation for diagnostic accuracy of this evaluation was performed.
Conclusions
The accuracy of individual clinical index tests used to predict imaging findings of nerve root impingement in patients with chronic lumbar radiculopathy is low when applied in specialised care, but clinicians’ overall evaluation improves diagnostic accuracy slightly. The tests are not very helpful in clarifying the cause of radicular pain, and are therefore inaccurate for guidance in the diagnostic workup of the patients. The study population was highly selected and therefore the results from this study should not be generalised to unselected patient populations in primary care nor to even more selected surgical populations.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Lumbar radiculopathy is a common reason for physician consultations and imaging referrals [1–3]. Typical symptoms are radiating pain, often with numbness, paraesthesia, and/or muscle weakness [1, 4]. Clinical examination aims to clarify whether there is mechanical impingement of a nerve root [5]. The most common clinical diagnostic tests are the straight leg raising test, and tests for tendon reflexes, motor weakness, and sensory deficits [6]. An inaccurate clinical diagnosis may lead to unnecessary imaging and healthcare expenditure, and additional concerns for patients [7–12].
The aim with imaging is to confirm or disprove a clinical suspicion, and to provide a roadmap for planning of surgical or other intervention procedures, if indicated. Mechanical nerve root impingements demonstrated with magnetic resonance imaging (MRI) or computer tomography (CT) is an accepted reference standard [13].
Systematic reviews on the diagnostic properties of clinical diagnostic tests for lumbar radiculopathy report variable accuracy, with sensitivities ranging from 0.14 to 0.61 for sensory deficits and impaired tendon reflexes [14, 15], 0.27 to 0.62 for motor weakness [14, 16], and 0.35 to 0.81 for the straight leg raising test [17]. Most studies report likelihood ratios (LRs) suggesting negligible differences between pre- and post-test probabilities for presence of nerve root impingement as the target condition, indicating limited value of the tests in clinical decision-making. A recent Cochrane review confirmed poor diagnostic performance of diagnostic tests in 18 studies from specialised care [13].
This review raised concern that none of the reported studies specifically discriminated between nerve root impingement and just the presence of a disc herniation when using imaging as a reference standard. This could be a major bias, since the prevalence of disc bulging or herniation in unselected populations without radiculopathy symptoms is high [18].
The aims of this study are to investigate the association between findings at clinical examination and nerve root impingement, to evaluate the accuracy of clinical index tests in a specialised care setting, and to see whether imaging clarifies the cause of chronic radicular pain.
Methods
Study participants
The study was performed as part of a multicentre randomised controlled trial on the treatment effect of caudal epidural injections [19]. Eligible patients with suspected chronic lumbar radiculopathy, aged between 20 and 60 years, referred to outpatient multidisciplinary back clinics of five Norwegian hospitals, were consecutively assessed for inclusion. All patients were referred with a history suggesting chronic lumbar radiculopathy, and the clinical diagnosis was verified with at least one corresponding positive clinical test (index test) consistent with affection of a specific lumbar nerve root. These inclusion criteria ensured a homogenous patient population with clinically verified lumbar radiculopathy and a high pre-test probability of nerve root impingement. MRI or CT was used to specifically clarify whether the nerve root in question was impinged or not. The reference standard was set to be disc herniation causing impingement (compression and/or dislocation) of a spinal nerve root. Written informed consent was obtained, and the Regional Committee for Medical and Health Research Ethics in North Norway approved the study.
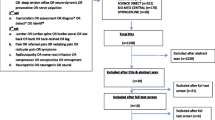
We assessed 461 patients with suspected lumbar radiculopathy for inclusion (Figure 1). 376 (81.6%) were referred from general practitioners, and 85 (18.4%) were internally referred in the participating hospitals. The inclusion criteria were unilateral lumbar radiculopathy lasting for more than 12 weeks and one or more positive index tests consistent with nerve root affection. The intensity of the leg pain, radiating from the back to below the knee, had to be comparable to or worse than the back pain. Whilst obtaining the patient’s history, enquiries were made about the intensity of leg and low back pain on a visual analogue scale, the possible dermatome distribution of the pain, the presence of paraesthesia in the leg, whether the pain was aggravated by forward flexion or sitting, and whether there was any muscle weakness in the lower extremity.
We excluded 345 (74.8%) patients fulfilling predefined exclusion criteria according to the original randomised control trial [19]: 146 (42.3%) due to unspecific low back pain with referred leg pain, 105 (30.4%) due to radiculopathy improving during the last two weeks, 24 (7.0%) due to radiculopathy requiring referral to surgery, 16 (4.6%) because of earlier back surgery, 37 (10.7%) due to different medical conditions (pregnancy, breast feeding, use of anticlotting medication), and 17 (4.9%) because they declined to participate.
Physical examination
The physical examination was performed according to the recommendations given by the American Spinal Injury Association [20–22]. It consisted of the following index tests: the straight leg raising test, the femoral nerve stretch test, testing of muscle power in seven muscle groups on a five-point scale, dermatome sensory loss using light touch and pin prick classified on a three-point scale, and reflex impairment testing on a four-point scale. Each index test was dichotomised as being normal or abnormal according to the standard neurological classification. The straight leg raising test was considered abnormal when pain occurred before 60 degrees passive elevation from horizontal, and the femoral nerve stretch test was considered positive when the patient experienced radiating pain [23].
Specialists in neurology or physical medicine and rehabilitation did the examination in cooperation with a physiotherapist. Prior to the study, they were trained to perform the tests in a standardised way.
Based on an overall evaluation of the patient history and results of all the index tests, a clinical decision was reached for each patient concerning the suspected level and side of nerve root affection [24–27]. The clinical decision for a nerve root involvement required a history of radicular pain accompanied by one or more corresponding positive index tests. The clinicians were blinded to the results of the imaging until this decision had been reached. To diagnose an L4 radiculopathy the clinician placed emphasis on the femoral nerve stretch test, the straight leg raise test, the knee reflex, sensory loss in the L4 dermatome and the muscle power for the ankle dorsiflexion. To diagnose an L5 radiculopathy the clinician focused on the straight leg raise test, sensory loss in the L5 dermatome, and the muscle power for the hip abduction, ankle dorsiflexion, ankle eversion, and the big toe extension. For an S1 radiculopathy the clinician emphasized the straight leg raise test, the ankle reflex, sensory loss in the S1 dermatome, and the muscle power for hip extension, knee flexion, ankle plantarflexion, and ankle eversion.
Imaging reference standard
MRI in 109 (94.0%) patients or CT in 7 (6.0%) patients was performed. Experienced radiologists evaluated the images, and a written report from the radiologists was available for the clinicians to be able to exclude patients with severe intra-spinal pathology obviously demanding surgery [19, 28].
All the MRI and CT scans were re-evaluated by two independent neuroradiologists using the Nordic Modic Classification [29]. They were blinded regarding patient history and clinical findings. The locations of the disc herniation were identified in the axial plane, and were categorised as being localised centrally or to the left or right in the spinal canal [30]. In cases of disagreement, a consensus was reached emphasising the most experienced.
Statistical analysis
We calculated means and standard deviations (SD) for continuous variables, and frequencies and proportions for categorical variables. The prevalence of nerve root impingement based on the reference standard and the post-test probabilities for a positive and negative test were calculated. Diagnostic accuracy was quantified by calculating sensitivities, specificities, and positive and negative likelihood ratios (LR), including 95% confidence intervals (CI), for each clinical test. In a multivariable logistic regression model we included all index tests as independent variables. The estimated model was used to predict the probability of a positive MRI/CT for each patient. These probabilities were used to produce a receiver operating characteristic (ROC) curve and an estimate for the area under the curve (AUC). All analyses were performed using the Statistical Package for the Social Sciences software (SPSS), version 19 (IBM Software, NY, USA).
Results
In total, 116 patients with unilateral chronic lumbar radiculopathy were included. Their clinical and demographic characteristics are summarised in Table 1. Mean age was 42.0 (SD 10.3) years, 68 (58.6%) were males, and the mean duration of symptoms on inclusion was 42.0 (SD 99.0) weeks. Figure 1 shows the results of MRI or CT for the included patients. The overall prevalence of disc herniation at any of the studied lumbar levels (L2 to S1) was 77.8%.
Table 2 shows the frequencies of positive index tests, the overall clinical evaluation, and the imaging findings. Table 3 shows the diagnostic accuracies for the different index tests for detection of the level and side of the nerve root impingement. None of the individual tests were highly accurate, as both sensitivities and specificities were low with wide CIs. All positive LRs were ≤4.0, and all negative LRs ≥0.4.
Table 4 shows that the clinicians’ overall evaluations using information from all relevant index tests to predict nerve root impingement were slightly more accurate than each of the individual index tests. ROC analysis of the diagnostic properties of the overall clinical evaluations showed AUCs of 0.95 (95% CI 0.90–1.00) for L4, 0.67 (95% CI 0.56–0.77) for L5, and 0.66 (95% CI 0.54–0.77) for S1 nerve root impingement.
Discussion
This study included patients with symptoms suggesting lumbar radiculopathy. Patients were recruited by screening and referral from general practitioners, and those with large disc herniation obviously requiring surgery were excluded. The sample emerging from these criteria is typical for the chronic radiculopathy population seen in specialised care. Results from the study are relevant for our understanding of diagnostic accuracy in the common clinical setting where specialists have access to imaging findings prior to the clinical examination, and often are challenged by having to evaluate which of numerous positive imaging findings are to be considered clinically relevant.
The main finding is that individual clinical index tests lack diagnostic accuracy for predicting whether a lumbar nerve root is impinged or not at a specific level in patients with chronic lumbar radiculopathy in specialised care. The overall clinical evaluation, consisting of the specialists’ combined interpretation of the patients’ history and all index tests, was somewhat more accurate. For L5 and S1 nerve root impingement, however, LRs did not reach the levels usually considered necessary to influence post-test probability and thereby clinical decision-making (positive LR >5.0 and negative LR <0.2) [31]. Accuracy was better (positive LR 6.28, negative LR 0.70) for L4 nerve root impingement. This was probably because L4 nerve root involvement occurred only in 3 (2.6%) cases, and was suspected after the overall clinical evaluation only in 7 (6.0%) cases. This resulted in a high number of true negatives, and thereby high specificity. Clinically, the low pre-test probability for L4 nerve root involvement is well known [32], and these test properties are therefore not very useful. Accordingly, clinical examination is inaccurate both for predicting the presence or absence of nerve root impingement, and for clarifying the relevant level and side in patients with multiple positive imaging findings.
Our findings are mainly in accordance with other studies of selected populations from specialised care [13]. Most previous studies have, however, aimed for a generalised understanding of test properties from such selected materials [13]. This approach is confusing, as the pre-test probability always must be taken into consideration. Recently, a study aimed to specifically investigate the accuracy of clinical index tests from the neurological examination for identification of the level of disc herniation in patients with the target condition already confirmed by MRI [33]. Unfortunately the study did not find evidence to support this. The results were disappointing, with no single test reaching an AUC >0.75, and only slightly better results (AUC = 0.80) for the neurologists’ overall evaluation.
It has been a weakness of most previous studies that interpretation of the imaging findings has been limited to categorising the target condition (usually a disc herniation) as present or not, without considering whether a nerve root actually was impinged at the relevant spinal level and side [34]. We therefore improved the study design by specifically addressing findings relevant for clinical decision-making: correspondence between index tests and impingement of specific nerve roots as revealed by MRI [32]. Disappointingly, this did not improve diagnostic accuracy, neither for individual tests nor for the clinicians’ overall evaluation. AUCs for L5 and S1 nerve root impingement did not reach levels above 0.66, which are even lower than those observed by Hancock et al. in an almost similar specialised care setting [33]. This could be because we used one or more positive index tests as an inclusion criterion, which probably increased both the proportion of false positives and false negatives. The false negatives increased because the index tests are not independent of each other, implying that inclusion based on one or more positive tests entails an increased proportion of false negatives, since many tests are performed in each patient. We do not consider the selection of patients in our study a methodological weakness, but rather an expression of clinical reality in specialised care. There should, however, be concern about both the definition of the target condition and the reference standard being subjects to bias. First, neuroanatomical overlap between spinal segments influences accuracy when the analysis is done on the level of each single nerve root [35–37]. Patients may have radiculopathy from causes other than ongoing nerve root impingement, and even when an impingement is present, this is not necessarily the cause of the pain. Imaging showed no sign of nerve root impingement in 56 (48.3%) of the included cases despite a clear history and clinical findings suggesting lumbar radiculopathy. This confirms that radiculopathy may have other causes, such as neuropathic and inflammatory conditions, or be mimicked by myofascial pain [6, 38–40]. Moreover, disc herniation without nerve root impingement was demonstrated in 25.9% of the included patients, and in 73.8% of those excluded due to symptoms classified as unspecific low back pain with referred leg pain. This is not surprising, since the prevalence of disc herniation revealed by MRI in the general population is known to be as high as 30% [3, 18, 41–44].
We suggest that our findings reflect clinical reality very well: in a population selected by referral from primary care and exclusion of the most obvious surgical cases, co-morbidity bias and imaging findings not related to the symptoms are common. Diagnostic imaging combined with clinical tests is therefore inaccurate for clarifying the cause of radicular pain. This is probably one of the reasons why these patients are so difficult to treat, and the same inaccuracy may cause significant inclusion bias in clinical trials evaluating treatments for lumbar radiculopathy.
The present study has weaknesses. We did not register inter-tester variability for the clinical tests and image interpretations. However, all clinicians were trained to perform the tests in a standardised manner, and agreement should thus be superior to that achieved between clinicians in daily practice [22]. MRI was substituted with CT in 7 (6.0%) of the study subjects. A few cases of nerve root impingement may have been missed, but this is unlikely to have influenced the results significantly. Further, the duration of symptoms (average 42 weeks) was relatively long. Development of chronic centralised pain followed by regression of nerve root impingement may have occurred in some patients, and our results may not be generalisable to situations with shorter symptom duration.
Finally, it must be emphasised that the index tests work differently when applied in other settings. In unselected primary care populations, the proportion of false positives will be lower and the specificity of the tests higher. Accordingly, the tests may be useful in primary care to reduce the post-test likelihood of lumbar radiculopathy, and thereby restrict unnecessary referrals for imaging and specialised care. On the other hand, when applied in a highly selected surgical patient population with shorter duration of symptoms and a large disc herniation obviously corresponding with the symptoms, the proportion of true positives will be high and the proportion of false positives low, resulting in high sensitivity and specificity. The results from the present study should therefore not be generalised to unselected patient populations in primary care nor to even more selected surgical populations.
Conclusions
In conclusion, the accuracy of individual clinical index tests used to predict imaging findings of nerve root impingement in patients with lumbar radiculopathy is low when applied in specialised care, and clinicians’ overall evaluation does not improve diagnostic accuracy significantly. Accordingly, the tests are not very helpful in clarifying the cause of radicular pain, and are therefore inaccurate for treatment guidance of patients who often have multiple positive imaging findings. These results suggest that previous belief in the benefit of combining different neurological tests to accurately diagnose the level of nerve root affection has been exaggerated [45, 46]. Co-morbidity and imaging findings not related to the symptoms are probably the most important causes for diagnostic inaccuracy in chronic lumbar radiculopathy [3, 28, 39, 47–49].
Abbreviations
- AUC:
-
Area under the curve
- CI:
-
Confidence interval
- CT:
-
Computer tomography
- LR:
-
Likelihood ratio
- MRI:
-
Magnetic resonance imaging
- ROC:
-
Receiver operating characteristic
- SD:
-
Standard deviation.
References
Masters S, Lind R: Musculoskeletal pain - presentations to general practice. Aust Fam Physician. 2010, 39: 425-428.
McGuirk B, Bogduk N: Evidence-based care for low back pain in workers eligible for compensation. Occup Med (Lond). 2007, 57: 36-42.
Li AL, Yen D: Effect of increased MRI and CT scan utilization on clinical decision-making in patients referred to a surgical clinic for back pain. Can J Surg. 2011, 54: 128-132. 10.1503/cjs.001510.
Waddell G, Main CJ, Morris EW, Venner RM, Rae PS, Sharmy SH: Normality and reliability in the clinical assessment of backache. Br Med J (Clin Res Ed). 1982, 284: 1519-1523. 10.1136/bmj.284.6328.1519.
Janardhana AP, Rajagopal , Rao S, Kamath A: Correlation between clinical features and magnetic resonance imaging findings in lumbar disc prolapse. Indian J Orthop. 2010, 44: 263-269. 10.4103/0019-5413.65148.
Cannon DE, Dillingham TR, Miao H, Andary MT, Pezzin LE: Musculoskeletal disorders in referrals for suspected lumbosacral radiculopathy. Am J Phys Med Rehabil. 2007, 86: 957-961. 10.1097/PHM.0b013e31815b614a.
Atlas SJ, Keller RB, Wu YA, Deyo RA, Singer DE: Long-term outcomes of surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: 10 year results from the maine lumbar spine study. Spine (Phila Pa 1976). 2005, 30: 927-935. 10.1097/01.brs.0000158954.68522.2a.
Martin BI, Turner JA, Mirza SK, Lee MJ, Comstock BA, Deyo RA: Trends in health care expenditures, utilization, and health status among US adults with spine problems, 1997–2006. Spine (Phila Pa 1976). 2009, 34: 2077-2084. 10.1097/BRS.0b013e3181b1fad1.
Deyo RA, Mirza SK, Turner JA, Martin BI: Overtreating chronic back pain: time to back off?. J Am Board Fam Med. 2009, 22: 62-68. 10.3122/jabfm.2009.01.080102.
Carragee EJ: Clinical practice. Persistent low back pain. N Engl J Med. 2005, 352: 1891-1898. 10.1056/NEJMcp042054.
Daffner SD, Hymanson HJ, Wang JC: Cost and use of conservative management of lumbar disc herniation before surgical discectomy. Spine J. 2010, 10: 463-468. 10.1016/j.spinee.2010.02.005.
Akobeng AK: Understanding diagnostic tests 2: likelihood ratios, pre- and post-test probabilities and their use in clinical practice. Acta Paediatr. 2007, 96: 487-491. 10.1111/j.1651-2227.2006.00179.x.
Van Der Windt DA, Simons E, Riphagen II, Ammendolia C, Verhagen AP, Laslett M: Physical examination for lumbar radiculopathy due to disc herniation in patients with low-back pain. Cochrane Database Syst Rev. 2010, 10.1002/14651858.CD007431.pub2. Issue 2, Art. No.: CD007431
Vroomen PC, de Krom MC, Wilmink JT, Kester AD, Knottnerus JA: Diagnostic value of history and physical examination in patients suspected of lumbosacral nerve root compression. J Neurol Neurosurg Psychiatry. 2002, 72: 630-634. 10.1136/jnnp.72.5.630.
Albeck MJ: A critical assessment of clinical diagnosis of disc herniation in patients with monoradicular sciatica. Acta Neurochir (Wien). 1996, 138: 40-44. 10.1007/BF01411722.
KNUTSSON B: Comparative value of electromyographic, myelographic and clinical-neurological examinations in diagnosis of lumbar root compression syndrome. Acta Orthop Scand Suppl. 1961, 49: 1-135.
Scaia V, Baxter D, Cook C: The pain provocation-based straight leg raise test for diagnosis of lumbar disc herniation, lumbar radiculopathy, and/or sciatica: a systematic review of clinical utility. J Back Musculoskelet Rehabil. 2012, 25: 215-223.
Borenstein DG, O’Mara JW, Boden SD, Lauerman WC, Jacobson A, Platenberg C: The value of magnetic resonance imaging of the lumbar spine to predict low-back pain in asymptomatic subjects: a seven-year follow-up study. J Bone Joint Surg Am. 2001, 83-A: 1306-1311.
Iversen T, Solberg TK, Romner B, Wilsgaard T, Twisk J, Anke A: Effect of caudal epidural steroid or saline injection in chronic lumbar radiculopathy: multicentre, blinded, randomised controlled trial. BMJ. 2011, 343: d5278-10.1136/bmj.d5278.
Linassi G, Li Pi SR, Marino RJ: A web-based computer program to determine the ASIA impairment classification. Spinal Cord. 2010, 48: 100-104. 10.1038/sc.2009.98.
Marino RJ, Barros T, Biering-Sorensen F, Burns SP, Donovan WH, Graves DE: International standards for neurological classification of spinal cord injury. J Spinal Cord Med. 2003, 26 (Suppl 1): S50-S56.
Waring WP, Biering-Sorensen F, Burns S, Donovan W, Graves D, Jha A: _ 2009 review and revisions of the international standards for the neurological classification of spinal cord injury. J Spinal Cord Med. 2010, 33: 346-352.
Charnley J: Orthopaedic signs in the diagnosis of disc protrusion. With special reference to the straight-leg-raising test. Lancet. 1951, 1: 186-192.
Stanley H: Orthopaedic Neurology. A Diagnostic Guide to Neurological Levels. 1997, Philadelphia: Lippincott-Raven
Malanga GA, Nadler SF: Musculoskeletal Physical Examination. An Evidence-Based Approach. 2006, Philadelphia: Mosby
Buckup K: Clinical Tests for the Musculoskeletal System. Examination-Signs-Phenomenan. 2008, Stuttgart: Thieme, 2
Andersson GB, Deyo RA: History and physical examination in patients with herniated lumbar discs. Spine (Phila Pa 1976). 1996, 21: 10S-18S. 10.1097/00007632-199612151-00003.
Suri P, Hunter DJ, Katz JN, Li L, Rainville J: Bias in the physical examination of patients with lumbar radiculopathy. BMC Musculoskelet Disord. 2010, 11: 275-10.1186/1471-2474-11-275.
Jensen TS, Sorensen JS, Kjaer P: Intra- and interobserver reproducibility of vertebral endplate signal (modic) changes in the lumbar spine: the Nordic Modic Consensus Group classification. Acta Radiol. 2007, 48: 748-754. 10.1080/02841850701422112.
Summers B, Malhan K, Cassar-Pullicino V: Low back pain on passive straight leg raising: the anterior theca as a source of pain. Spine (Phila Pa 1976). 2005, 30: 342-345. 10.1097/01.brs.0000152378.93868.c8.
Jaeschke R, Guyatt G, Sackett DL: Users’ guides to the medical literature. III. How to use an article about a diagnostic test. A. Are the results of the study valid? Evidence-Based Medicine Working Group. JAMA. 1994, 271: 389-391. 10.1001/jama.1994.03510290071040.
Valat JP, Genevay S, Marty M, Rozenberg S, Koes B: Sciatica. Best Pract Res Clin Rheumatol. 2010, 24: 241-252. 10.1016/j.berh.2009.11.005.
Hancock MJ, Koes B, Ostelo R, Peul W: Diagnostic accuracy of the clinical examination in identifying the level of herniation in patients with sciatica. Spine (Phila Pa 1976). 2011, 36: E712-E719. 10.1097/BRS.0b013e3181ee7f78.
Majlesi J, Togay H, Unalan H, Toprak S: The sensitivity and specificity of the Slump and the Straight Leg Raising tests in patients with lumbar disc herniation. J Clin Rheumatol. 2008, 14: 87-91. 10.1097/RHU.0b013e31816b2f99.
Beattie P, Nelson R: Clinical prediction rules: what are they and what do they tell us?. Aust J Physiother. 2006, 52: 157-163. 10.1016/S0004-9514(06)70024-1.
Mobbs RJ, Steel TR: Migration of lumbar disc herniation: an unusual case. J Clin Neurosci. 2007, 14: 581-584. 10.1016/j.jocn.2006.04.002.
Sucu HK, Gelal F: Lumbar disk herniation with contralateral symptoms. Eur Spine J. 2006, 15: 570-574. 10.1007/s00586-005-0971-x.
Riksman JS, Williamson OD, Walker BF: Delineating inflammatory and mechanical sub-types of low back pain: a pilot survey of fifty low back pain patients in a chiropractic setting. Chiropr Man Therap. 2011, 19: 5-10.1186/2045-709X-19-5.
Boden SD, McCowin PR, Davis DO, Dina TS, Mark AS, Wiesel S: Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990, 72: 1178-1184.
Lauder TD: Musculoskeletal disorders that frequently mimic radiculopathy. Phys Med Rehabil Clin N Am. 2002, 13: 469-485. 10.1016/S1047-9651(02)00007-4.
Gilbert JW, Martin JC, Wheeler GR, Storey BB, Mick GE, Richardson GB: Lumbar disk protrusion rates of symptomatic patients using magnetic resonance imaging. J Manipulative Physiol Ther. 2010, 33: 626-629. 10.1016/j.jmpt.2010.08.010.
Slavin KV, Raja A, Thornton J, Wagner FC: Spontaneous regression of a large lumbar disc herniation: report of an illustrative case. Surg Neurol. 2001, 56: 333-336. 10.1016/S0090-3019(01)00607-3.
el Barzouhi A, Vleggeert-Lankamp CLAM, à Nijeholt GJL, Van der Kallen BF, van den Hout WB, Jacobs WCH: Magnetic resonance imaging in follow-up assessment of sciatica. N Engl J Med. 2013, 368: 999-1007. 10.1056/NEJMoa1209250.
Jarvik JG, Hollingworth W, Heagerty PJ, Haynor DR, Boyko EJ, Deyo RA: Three-year incidence of low back pain in an initially asymptomatic cohort: clinical and imaging risk factors. Spine (Phila Pa 1976). 2005, 30: 1541-1548. 10.1097/01.brs.0000167536.60002.87.
Stankovic R, Johnell O, Maly P, Willner S: Use of lumbar extension, slump test, physical and neurological examination in the evaluation of patients with suspected herniated nucleus pulposus. A prospective clinical study. Man Ther. 1999, 4: 25-32. 10.1016/S1356-689X(99)80006-X.
Reihani-Kermani H: Correlation of clinical presentation with intraoperative level diagnosis in lower lumbar disc herniation. Ann Saudi Med. 2004, 24: 273-275.
Vucetic N, Svensson O: Physical signs in lumbar disc hernia. Clin Orthop Relat Res. 1996, 333: 192-201.
Kent P, Keating JL: Classification in nonspecific low back pain: what methods do primary care clinicians currently use?. Spine (Phila Pa 1976). 2005, 30: 1433-1440. 10.1097/01.brs.0000166523.84016.4b.
Cohen SP, Gupta A, Strassels SA, Christo PJ, Erdek MA, Griffith SR: Effect of MRI on treatment results or decision making in patients with lumbosacral radiculopathy referred for epidural steroid injections: a multicenter, randomized controlled trial. Arch Intern Med. 2012, 172: 134-142. 10.1001/archinternmed.2011.593.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2474/14/206/prepub
Acknowledgements
We thank Jan Inge Letto, Anne Sofie Broback, Dag Grindheim, Robert Kouwenhoven, Fredrik Granviken, Franz Hintringer, Svetlana Rasic, Helge Hartman, Sigrun Randen, and Einar Vegå for doing the assessments. A special thanks to the Clinical Research Centre at the University Hospital of North Norway and to Bjørn Odvar Eriksen, Inger Sperstad, May Greta Pedersen, Sameline Grimsgaard, Dag Grønvoll, Aslaug Jakobsen, Rolf Salvesen, Dagfinn Thorsvik, Tormod Hagen, Bjørn Skogstad, and all the patients who made this study possible.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
TI contributed to the study design, data collection, data analysis, interpretation, and writing of the manuscript. TKS, ØN, ToI, TW, and BR contributed to the study design, data analysis, interpretation, and writing of the manuscript. JIB and KW contributed to data analysis, interpretation, and writing of the manuscript. All authors reviewed and approved the final version of the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Iversen, T., Solberg, T.K., Romner, B. et al. Accuracy of physical examination for chronic lumbar radiculopathy. BMC Musculoskelet Disord 14, 206 (2013). https://doi.org/10.1186/1471-2474-14-206
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2474-14-206