Abstract
Background
Upper respiratory tract infections (URTIs) are among the most frequent reasons for physician office visits in paediatrics. Despite their predominant viral aetiology, URTIs continue to be treated with antimicrobials. We explored general practitioners' (GPs) prescribing behaviour for antimicrobials in children (≤ 16 years) with URTIs in Trinidad, using the guidelines from the Centers for Disease Control and Prevention (CDC) as a reference.
Methods
A cross-sectional study was conducted on 92 consenting GPs from the 109 contacted in Central and East Trinidad, between January to June 2003. Using a pilot-tested questionnaire, GPs identified the 5 most frequent URTIs they see in office and reported on their antimicrobial prescribing practices for these URTIs to trained research students.
Results
The 5 most frequent URTIs presenting in children in general practice, are the common cold, pharyngitis, tonsillitis, sinusitis and acute otitis media (AOM) in rank order. GPs prescribe at least 25 different antibiotics for these URTIs with significant associations for amoxicillin, co-amoxiclav, cefaclor, cefuroxime, erythromycin, clarithromycin and azithromycin (p < 0.001). Amoxicillin alone or with clavulanate was the most frequently prescribed antibiotic for all URTIs. Prescribing variations from the CDC recommendations were observed for all URTIs except for AOM (50%), the most common condition for antibiotics. Doctors practicing for >30 years were more likely to prescribe antibiotics for the common cold (p = 0.014). Severity (95.7%) and duration of illness (82.5%) influenced doctors' prescribing and over prescribing in general practice was attributed to parent demands (75%) and concern for secondary bacterial infections (70%). Physicians do not request laboratory investigations primarily because they are unnecessary (86%) and the waiting time for results is too long (51%).
Conclusions
Antibiotics are over prescribed for paediatric URTIs in Trinidad and amoxicillin with co-amoxiclav were preferentially prescribed. Except for AOM, GPs' prescribing varied from the CDC guidelines for drug and duration. Physicians recognise antibiotics are overused and consider parents expecting antibiotics and a concern for secondary bacterial infections are prescribing pressures. Guidelines to manage URTIs, ongoing surveillance programs for antibiotic resistance, public health education on non-antibiotic strategies, and postgraduate education for rational pharmacotherapy in general practice would decrease inappropriate antibiotic use in URTIs.
Similar content being viewed by others
Introduction
Respiratory tract infections are among the most frequently encountered clinical conditions and URTIs are one of the most common reasons for paediatric consultations in primary health care [1, 2]. Children in developing countries suffer an annual average of six URTIs [3], with a high incidence in the first 7 years of life, which are termed the "catarrhal" stage [4]. These infections impose a burden on the health care system and are a major reason for absenteeism from school and work by children and parents respectively [5]].
Antimicrobials are the second leading therapeutic drug category office based physicians prescribe. Even though current evidence does not warrant their routine use in upper respiratory tract infections [6, 7], their injudicious use in family practice in the United States revealed 79% of prescriptions were unnecessary according to the CDC guidelines [8]. The pandemic increase in multiple antimicrobial-resistant strains of Streptococcus pneumoniae, Haemophilus influenzae and Moraxella catarrhalis [9, 10] the major pathogens of otitis media and sinusitis [11] has been attributed to irrational prescribing, fuelling the move to reduce unnecessary antimicrobial use. Despite a viral aetiology antimicrobials continue to be accepted treatment for 50%-70% of patients seeking medical care for URTIs [12]. A 1998 report from the United States estimated 6.5 million prescriptions annually (paediatric use was 12%) were for URTIs or the common cold and children were a target for reduction of unnecessary antimicrobial use [13]. Antimicrobial misuse or overuse promotes public perception that these drugs are preferred treatment for URTIs, encourages patient demand and promotes an increased pool of resistant bacteria. The CDC in collaboration with the American Academy of Paediatrics (AAP) and the American Academy of Family Physicians (AAFP), recommend stringent diagnostic criteria for URTIs to avoid misdiagnosis and inappropriate antibiotic prescriptions [14]. Family physicians manage URTIs with considerable variation [15] and we undertook this study to provide insight into this variation in Trinidad, since there is no information on prescribing patterns in general practice in Trinidad or the Caribbean. We explored physician behaviour of antimicrobial prescribing for URTIs in children, and practice variations based on the CDC principles of judicious antibiotic use [16, 17].
Methods
A cross-sectional survey was conducted between January to June 2003 on office based GPs listed in the Trinidad and Tobago Medical Association. The Association has four branches with approximately 270 subscribing members in Trinidad. We approached doctors in Central and East Trinidad, from the respective branches of the Trinidad and Tobago Medical Association. A "child" was defined as a person sixteen years or younger and a "general practitioner" was a doctor with a practice not confined to any particular specialty of medicine besides family practice. The Ethics Committee of the Faculty of Medical Sciences, The University of the West Indies approved the study. Specialists, consultants and doctors working in primary health care in the public sector were excluded. Prescribing for patients who were immuno-compromised, malnourished, infected by laboratory-proven resistant strains of pathogens and/or who suffered from chronic respiratory tract disease was not investigated. Letters were mailed to doctors followed by a telephone call, inviting their participation. Student researchers were trained to ask questions and practiced among themselves to ensure consistency in administering the pilot-tested questionnaire. Two researchers interviewed physicians who identified and ranked the five most common URTIs in their practice. Practice variations in the management of URTIs were observed for the prescribed antimicrobials of choice, the duration of administration for each drug for each of the identified URTIs, and factors that could influence the physician's choice of antimicrobial agent. Physicians identified three characteristic signs and symptoms for each URTI, and reasons which they believed contributed to antimicrobial over prescribing for paediatric URTIs in general practice.
Data were analysed using the Statistical Program for Social Sciences (SPSS; Chicago, Illinois, version 9.0). Differences in categorical data were analysed using Chi-square tests, and p values < 0.05 were considered statistically significant.
Results
Of 109 listed GPs, 92 (response rate 84.4%) consented to participate; and representation from Central and East Trinidad was 40.2% (37) and 59.8% (55) respectively. There were 81 (88%) male and 11 (12%) female physicians and the doctors' mean age was 52.55 years (SE= ± 1.34). Approximately a quarter of the sample (24, 26.1%) had > 30 years of practice, 38 (41.3%) doctors were practicing for < 20 years, and 30 (32.6%) had between 20–30 years of practice. There were 51 (54.4%) graduates of the University of the West Indies and 41 (45.6%) doctors were trained abroad.
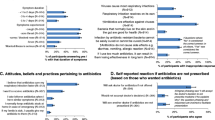
In rank order, physicians see the common cold, pharyngitis, tonsillitis, sinusitis and AOM in their office practice. All but one doctor (91, 98.9%) (a naturopath) would prescribe antimicrobials for at least one of the five listed URTIs and 5 GPs (5.4%) said antimicrobials do not modify the course of URTIs GPs recommend at least 25 different antimicrobials to treat the 5 investigated URTIs in children. Prescribing was highest for AOM and least for the common cold (Table 1) and amoxicillin alone or with clavulanate was the most frequently prescribed antimicrobial. Among the cephalosporins (cefaclor, cefuroxime, cefadroxil, cefalexin,), cefuroxime was the most frequently recommended. Several macrolides (erythromycin, josamycin, clarithromycin, roxithromycin) were prescribed, but azithromycin was preferred for all URTIs. Quinolones and tetracylines were seldom prescribed (<9, 9.8%), except for sinusitis by 13 (14.1%) and 12 (13%) GPs respectively. Doctors practicing for > 30 years were more likely to prescribe antibiotics for the common cold (p = 0.014). With the exception of azithromycin, doctors would prescribe antibiotics for between 5–7 days for all the URTIs. (Fig 1. Number and duration of antimicrobial prescriptions made for each URTI). For AOM doctors' prescriptions were in approximately equivalent proportions for durations of 5–7 days or 10 days, though the CDC recommends antibiotics for 7 days for this condition.
Significant associations were found between the 5 investigated URTIs and prescribed antimicrobials (p < 0.001) (Table 2). Amoxicillin was most frequently recommended for pharyngitis and tonsillitis (47, 51.6% each) and at least 36 (39.6%) GPs prescribed it for both conditions. Erythromycin (21, 23%) and azithromycin (27, 29.7%) were also prescribed for pharyngitis and tonsillitis respectively. Amoxicillin/clavulanate (55, 60.4%), azithromycin, cefaclor (each 29, 29.7%) and clarithromycin (19, 20.8%) were recommended for AOM, and for sinusitis physicians preferentially prescribed cefuroxime (20, 22%) and clarithromycin (19, 20.8%). Sixteen (17.5%) GPs prescribed azithromycin for both tonsillitis and AOM and 12 (13%) prescribed clarithromycin for both sinusitis and AOM. Fever was one of the three cardinal signs/symptoms, physicians consistently associated with all 5 URTIs (Table 3).
Doctors reported their prescribing was influenced by the severity of illness (88, 95.7%), duration of infection (76, 82.6%), suspected secondary bacterial infection (64, 69.6%), cost of treatment (63, 68.5%), past clinical experience (56, 60.9%), ease of drug administration (52, 56.5%), drug allergy (49, 53.3%) and medication taste (28, 30.4%). Very few GPs said they felt pressured to prescribe by pharmaceutical companies (9, 9.8%), or parents/guardians (7, 7.6%). Nevertheless, doctors (77, 83.7%) admitted antimicrobials were over-prescribed in general practice and most (86, 93.5%) believed parents/guardians have misconceptions about antibiotics and associate recovery with antimicrobials. Interestingly physicians' reported personal practices were at odds with cited reasons they offered for antibiotic over-prescription and 75% agreed demands of worried parents do increase antibiotic prescribing rates in general practice. (Figure 2. Reasons physicians offered for antimicrobial overprescription in general practice). Twenty-seven (29.3%) physicians stated community pharmacists dispense antibiotics over-the-counter and are responsible for their overuse in the community.
All doctors advised patients on the prescribed duration of treatment, but 68 (73.9%) were of the opinion that the general population was unaware of the importance of complying with this instruction. Just 11 (12%) doctors would request laboratory tests before prescribing antimicrobials. Seventy of the 80 (87.5%) doctors not requesting laboratory investigations considered them unnecessary, 10 (12.5%) would not request them even if they thought the tests necessary and 27 physicians (30%) felt a clinical diagnosis was sufficient. About half (41, 51.3%) the doctors said laboratory tests were futile because of the long waiting period for results. The cost of tests (28, 35%) and the unavailability of adequate laboratory facilities (24, 30%) also discouraged physicians from requesting these investigations.
No less than 20 different drugs were widely prescribed singly or in various combinations and included antipyretics, analgesics, antihistamines, decongestants, antitussives, expectorants and mucolytic agents. Supportive therapy comprised fluids, rest, vitamins, tepid sponging, dietary recommendations, steam inhalation, gargling and keeping warm.
Discussion
Paediatric URTIs in general practice in Trinidad are in rank order, the common cold, pharyngitis, tonsillitis, sinusitis and AOM. In Trinidad as in the USA, AOM is the leading URTI for antimicrobial prescriptions [18]. Amoxicillin alone or with clavulanate was the preferred drug for all URTIs and penicillin V was never recommended. In New Zealand, GPs also prescribed amoxicillin and amoxicillin-clavulanate most frequently to treat URTIs. [19]. Unnecessary use of amoxicillin and co-amoxiclav can increase the risk of selective pressure and colonisation with resistant organisms.
In the United States, AOM, acute sinusitis, bronchitis, pharyngitis and non-specific URTIs (common colds) account for most antibiotic use in paediatric outpatients [16]. In the present study, prescriptions were highest for AOM and least for the common cold, a pattern observed in Turkey [20] and Scandinavia [21]. The common cold is never an indication for antibiotic treatment and its natural history suggests mucopurulent rhinitis or cough for even upto 2 weeks does not necessarily point to bacterial infection [17]. Antibiotic treatment is beneficial to children with this syndrome only if symptoms persist for 10–14 days without improvement [22]. Several (70.3%) of our participating doctors were concerned about secondary bacterial infection, and we speculate high amoxicillin and co-amoxiclav prescribing represents an anxiety to prevent bacterial complications. In Britain, GPs believe people with severe symptoms are at risk of bacterial complications and prescribing antibiotics will prevent or reduce such complications [23] a practice not encouraged as effective prescribing strategy by the CDC [17]. Azithromycin's use for all URTIs (except the common cold) warrants concern in light of increasing macrolide-resistant pneumococci [24]. In sinusitis, cefuroxime use may point towards a concern about lactamase producing Haemophilus influenzae infection in the community, and the use of quinolones (11.1%) and tetracycline (14.9%) in children is worrying.
Senior physicians practicing for >30 years would prescribe antimicrobials for the common cold. In Hong Kong [25] this practice characteristic was associated with inappropriate prescribing for the common cold, and doctors assumed patients expected antibiotics from them. Younger doctors prescribe judiciously suggesting medical curricula incorporate appropriate prescribing principles. Emphasising rational pharmacotherapy in postgraduate vocational training will heighten family practitioners' competence on selective decisions on the need, choice and duration of antimicrobials for URTIs.
The CDC does not recommend antimicrobials for pharyngitis in the absence of undiagnosed Group A Streptococci (GAS) where viral aetiology is generally prevalent, and does not recognise tonsillitis as an independent URTI. Penicillin V remains specifically recommended for pharyngitis, (expressly GAS infections which account for just 15% of all cases) particularly as GAS resistance to β-lactams has not been documented [26]. The clinical presentation of pharyngitis does not permit differentiation between streptococcal and viral aetiology or reliably predict those who will benefit from antimicrobial therapy. Untreated GAS uncommonly causes potentially fatal rheumatic fever and physicians probably overestimate streptococcal infection. Penicillin V, the recommended antimicrobial for pharyngitis was never prescribed, despite its safety, efficacy, narrow spectrum and low cost, even though cost influenced GPs' prescribing.
Though doctors (50%) met the CDC recommendations for AOM, existing research nonetheless, offers no compelling evidence that outcomes are better in treated children [27] and clinicians are advised to reconsider routine antimicrobial use for AOM in children. Antimicrobial prescribing for uncomplicated sinusitis with amoxicillin/clavulanate (52.9%), azithromycin (25.3%) and amoxicillin (25.3%), did not concur with the CDC guidelines, which recommend narrow-spectrum antimicrobials for 10 days. Duration of therapy is as important a determinant as dosage for success or failure of antimicrobial therapy in paediatric patients, yet physicians widely prescribed for 5–7 days for all URTIs.
High empirical antimicrobial prescribing (87.0%) provided evidence for physicians' reluctance for laboratory investigations in private practice. Diagnostic uncertainty prompted antimicrobial prescribing (58.7%) emphasising the CDC's recommendation for accessible laboratory diagnosis with rapid reporting. We hasten to add such counsel may be feasible in economically advanced countries with managed health care but remains to be accepted by physicians and patients when cost is a crucial consideration of treatment.
Declaring antibiotics are overused in general practice, doctors (83.7%) offered parental expectation of receiving antibiotics as the leading reason, yet only 7.6% in contrast admitted this influenced their personal prescribing. In California, physicians' perceptions of parental expectations for antimicrobials in conditions of presumed viral aetiology were a significant predictor of prescribing antimicrobials in community and university based paediatric practices [28]. Patients and/or their parents reportedly associated recovery with antimicrobial use and those physicians who met parental expectations of receiving an antimicrobial believed a bacterial diagnosis was present. In our study GPs perceived antimicrobials were more likely to be prescribed when parents wanted them. Personal, family or friends' experiences mould patient/parent expectations [29] and pressure to fulfil these expectations drives over prescribing.
Our data highlights the responsibility of pharmacists to control antibiotic use and doctors' concern about this accountability. Parimi et al [30] reported 19% of Trinidad and Tobago's general public self-medicated with antimicrobials from private pharmacies, though these are controlled 'prescription only medication' by the Food and Drugs Division, Ministry of Health. The Pharmacy Board and the Ministry of Health in the country are obliged to monitor and enforce regulations for antimicrobial dispensing in community pharmacies.
Our study has limitations. Responses were dependent on the doctors' honesty and fidelity of recall. Time and busy practices may have constrained doctors from seeking clarifications on questions or giving detailed answers to open-ended questions. There are no guidelines for antimicrobial prescribing in the Caribbean and we referred to guidelines tailored for health care systems that do not exist locally or regionally.
International guidelines for rational pharmacotherapy have emerged following growing global concerns on increasing multiple resistant strains of upper airway pathogens from antibiotic overuse and misuse in URTIs [16, 17, 31, 32]. Reported low antimicrobial resistance in the Netherlands, is attributed to Dutch family physicians prescribing with relative restriction and selectivity for URTIs. [33]. In Sicily, macrolides, cephalosporins, penicillins with β-lactamase inhibitors and even extended spectrum penicillins were extensively prescribed by GPs for URTIs and attributed to unavailability or non-awareness of local or national guidelines [15]. Surveillance data from The Caribbean Epidemiology Centre on local patterns of pathogen susceptibility to antimicrobials can be employed to develop regional guidelines. Prescribing principles are nevertheless unlikely to evoke substantial change unless their dissemination and promotion is sustained through intensive continuing educational programmes for physicians and pharmacists. While practitioners may be encouraged to recognize and contain antimicrobial resistance, public educational campaigns on symptomatic care, the expected course of illness, viral aetiology of URTIs and the risks of inappropriate antimicrobial use will halt their misuse and encourage non-antibiotic strategies.
Conclusion
General practitioners in Trinidad preferentially prescribe antimicrobials in children, for AOM, tonsillitis, sinusitis and pharyngitis and their prescribing differed from the CDC recommendations for each disease (except AOM) for drug of choice and/or duration of prescription. Amoxicillin is the preferred agent for all URTIs and penicillin V was never recommended. GPs view parental pressure/expectations and secondary bacterial infections as determinants for antimicrobial overprescription in paediatric URTIs. Senior practitioners were more likely to prescribe antibiotics for the common cold. In the absence of local or regional guidelines or data on resistance patterns in the community, doctors remain unaware of appropriate prescribing recommendations. Educational interventions for parents and primary care providers can promote judicious use of antimicrobials in this comparatively benign condition in the community and contain development of resistance.
References
Teng CL, Shajahan Y, Khoo EM, Nurjahan I, Leong KC, Yap TG: The management of upper respiratory tract infection. Med J Malaysia. 2001, 56: 260-266.
Mlynarczyk G, Mlynarczyk A, Jeljaszewicz J: Epidemiological aspects of antibiotic resistance in respiratory pathogens. Int J Antimicrob Agents. 2001, 18: 497-502. 10.1016/S0924-8579(01)00455-1
Roncevic N, Popadic J, Stojadinovic A: Treatment of acute infections of the lower respiratory tract in children. Med Pregl. 2002, 55: 299-304.
Curro V, Soavi N, Grimaldi V, Bembo V, Procaccini M, Di Paolo R, Lanni R, Bianchi A, Polidori G: The catarrhal child. Pediatr Med Chir. 1992, 14: 183-191.
West JV: Acute upper airway infections. Br Med Bull. 2002, 61: 215-230. 10.1093/bmb/61.1.215
Arroll B, Kenealy T: Antibiotics for the common cold. Cochrane Database Syst Rev. 2002, 3: CD000247-
Fahey T, Stocks N, Thomas T: Systematic review of the treatment of upper respiratory tract infection. Arch Dis Child. 1998, 79: 225-230.
Scott JG, Cohen D, DiCicco-Bloom B, Orzano AJ, Jaen CR, Crabtree BF: Antibiotic use in acute respiratory infections and the ways patients pressure physicians for a prescription. J Fam Pract. 2001, 50: 853-858.
Herruzo R, Chamorro L, Garcia ME, Gonzalez MC, Lopez AM, Mancenido N, Yebenes L: Prevalence and antimicrobial-resistance of S. pneumoniae and S. pyogenes in healthy children in the region of Madrid. Int J Pediatr Otorhinolaryngol. 2002, 65: 117-123. 10.1016/S0165-5876(02)00145-3
Dajani AS: Beta-lactam resistance: clinical implications for pediatric patients [abstract]. J Int Med Res. 2002, 30 (Suppl 1): 2A-9A.
Brook I: Microbiology of common infections in the upper respiratory tract. Prim Care. 1998, 25: 633-648.
Larrabee T: Prescribing practices that promote antibiotic resistance: strategies for change. J Pediatr Nurs. 2002, 17: 126-132. 10.1053/jpdn.2002.124130
Hueston WJ, Eberlein C, Johnson D, Mainous AG: Criteria used by clinicians to differentiate sinusitis from viral upper respiratory tract infection. J Fam Pract. 1998, 46: 487-492.
Antibiotic Resistance – Technical Inforamtion. http://www.cdc.gov/drugresistance/community/technical.htm#pedprin
Mazzaglia G, Greco S, Lando C, Cucinotta G, Caputi AP: Adult acute upper respiratory tract infections in Sicily: pattern of antibiotic drug prescription in primary care. J Antimicrob Chemother. 1998, 41: 259-266. 10.1093/jac/41.2.259
Dowell SF, Schwartz B, Phillips WR: Appropriate use of antibiotics for URIs in children: Part I. Otitis media and acute sinusitis. The Pediatric URI Consensus Team. Am Fam Physician. 1998, 58: 1113-1118.
Dowell SF, Schwartz B, Phillips WR: Appropriate use of antibiotics for URIs in children: Part II. Cough, pharyngitis and the common cold. The Pediatric URI Consensus Team. Am Fam Physician. 1998, 58: 1335-1342.
Arroll B, Goodyear-Smith F: General practitioner management of upper respiratory tract infections:when are antibiotics prescribed?. N Z Med J. 2000, 113: 493-496.
Dowell S, Marcy SM, Phillips WR, Gerber MA, Schwartz B: Principles of judicious use of antimicrobial agents. Pediatrics. 1998, 101: 165-171.
Leblebicioglu H, Canbaz S, Peksen Y, Gunaydin M: Physician's antibiotic prescribing habits for upper respiratory tract infections in Turkey. J Chemother. 2002, 14: 181-184.
Andre M, Odenholt I, Schawn A, Axelsson I, Eriksson M, Hoffman M, Molstad S, Runehagen A, Lundborg CS, Wahlstrom R: Swedish Study Group on Antibiotic Use: Upper respiratory tract infections in general practice: diagnosis, antibiotic prescribing, duration of symptoms and use of diagnostic tests. Scand J Infect Dis. 2002, 34: 880-886. 10.1080/0036554021000026952
Rosenstein N, Phillips WR, Gerber MA, Marcy MS, Schwartz B, Dowell SF: The Common Cold-Principles of Judicious Use of Antimicrobial Agents. Pediatrics. 1998, 101: 181-184.
Satinder Kumar , Paul Little , Nicky Britten : Why do general practitioners prescribe antibiotics for sore throat? Grounded theory interview study. BMJ. 2003, 326: 138- 10.1136/bmj.326.7381.138
McCaig LF, Besser RE, Hughes JM: Antimicrobial drug prescription in ambulatory care settings, United States, 1992–2000. Emerg Infect Dis. 2003, 9: 432-437.
Lam TP, Lam KF: Management of upper respiratory tract infection by family doctors. Int J Clin Pract. 2001, 55: 358-360.
Schwartz B, Marcy SM, Phillips WR, Gerbert MA, Dowell SF: Pharyngitis- principles of judicious use of antimicrobial agents. Pediatrics. 1998, 101: 171-174.
Froom J, Culpepper L, Jacobs M, DeMelker RA, Green LA, van Buchem L, Grob P, Heeren T: Antimicrobials for acute otitis media? A review from the International Primary Care Network. BMJ. 1997, 315: 98-102.
Mangione-Smith R, McGlynn EA, Elliot MN, Krogstad P, Brook RH: The relationship between perceived parental expectations and pediatrician antimicrobial behaviour. Pediatrics. 1999, 103: 711-718.
Gonzales R, Malone DC, Maselli JH, Sande MA: Excessive antibiotic use for respiratory infections in the United States. Clin Infect Dis. 2001, 33: 757-762. 10.1086/322627
Parimi N, Pinto Pereira LM, Prabhakar P: The general public's perceptions and use of antimicrobials in Trinidad and Tobago. Rev Panam Salud Publica. 2002, 12: 11-18.
Dagnelie CF, Zwart S, Balder FA, Romeijnders ACM, Geijer RMM: NHG Standard "Acute sore throat". 2002, Utrecht: Dutch College of General Practitioners, http://nhg.artsennet.nl/guidelines2/E11.htm
Scottish Intercollegiate Guidelines Network: Guideline 34: management of sore throat and indications for tonsillectomy. 2001, Edinburgh: Royal College of Physicians, http://www.sign.ac.uk/guidelines/fulltext/34/
Melker RA, Kuyvenhoven MM: Management of upper respiratory tract infection in Dutch general practice. Br J Gen Pract. 1992, 42: 169-170.
Acknowledgements
We are grateful to participating doctors for their spontaneous co-operation, time and support. Dr. Celia Poon-King and Mr. Rudranath Singh reviewed the protocol and Dr Donald Simeon critiqued the manuscript. Drs. Roxanne Tantoco and Omar Ali, Presidents, Branches of the Trinidad and Tobago Medical Association, facilitated the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors Contributions
SM, KD, RD, DM, VP, and JR participated in the design of the study, executed data collection and entry, and early draft of the manuscript. JM performed the statistical analysis and contributed to the draft manuscript. LMPP conceived and designed the study, participated in its co-ordination and prepared the final manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Mohan, S., Dharamraj, K., Dindial, R. et al. Physician behaviour for antimicrobial prescribing for paediatric upper respiratory tract infections: a survey in general practice in Trinidad, West Indies. Ann Clin Microbiol Antimicrob 3, 11 (2004). https://doi.org/10.1186/1476-0711-3-11
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1476-0711-3-11