Abstract
Background
Epidermal growth factor receptor gene copy number (EGFR GCN) has been heavily investigated as a potential predictive biomarker for the treatment of metastatic colorectal cancer (mCRC) with anti-EGFR monoclonal antibodies (MAbs). The objective of this study was to systematically review current evidences on this issue.
Methods
PubMed, EMBASE, The Cochrane Library, Chinese Biomedical Literature Database, Wanfang Data, and the conference abstracts of American Society of Clinical Oncology and European Society of Medical Oncology were comprehensively searched. Studies that reported the objective response rate (ORR), progression-free survival, and/or overall survival of mCRC patients treated with anti-EGFR MAbs, stratified by EGFR GCN status, were included. The effect measures for binary outcome (response) and time-to-event outcomes (progression-free survival and overall survival) were risk difference and hazard ratio, respectively. Statistical heterogeneity among the studies was assessed by the Cochran’s Q-test and the I2 statistic. If appropriate, a quantitative synthesis of data from different studies would be conducted with a random-effects model.
Results
Nineteen eligible studies were identified. The criteria for increased EGFR GCN (GCN+) were highly inconsistent across different studies. The prevalence of GCN + ranged from 6.9% to 88.9%, and the difference in ORR between patients with GCN + and those with non-increased EGFR GCN (GCN-) varied from −28% to 84%. Because of the significant heterogeneity, no quantitative synthesis of data was performed. There was a general trend towards higher ORR in patients with GCN+. The difference in ORRs between patients with GCN + and those with GCN- was even greater in KRAS wild-type patients, while in KRAS mutated patients the difference often did not exist. Almost all patients with EGFR amplification responded to the treatment. However, the prevalence of EGFR amplification was generally low. Incomplete data on progression-free survival and overall survival seemingly supported the findings on ORR.
Conclusions
Although increased EGFR GCN is generally associated with a better outcome of anti-EGFR MAbs treatment, especially among patients with wild-type KRAS, the clinical utility of this biomarker for selecting recipients of anti-EGFR MAbs would be severely limited by the heterogeneous scoring system and the poor reproducibility of EGFR GCN enumeration due to technical reasons.
Similar content being viewed by others
Background
Colorectal cancer (CRC) is the third most common malignant disease and the fourth leading cause of cancer-related deaths worldwide [1]. Synchronous metastases have occurred in about 25% of patients at the time of diagnosis, and an additional 40% to 50% develop secondary metastases during the course of their disease after diagnosis [2]. For most patients with metastatic CRC (mCRC), chemotherapy is traditionally the first choice. However, the response rate is usually less than 50% [2] and the five-year survival rate of mCRC patients remains below 10% [3].
The chimeric IgG1 cetuximab and the fully humanized IgG2 panitumumab, two monoclonal antibodies (MAbs) targeted at epidermal growth factor receptor (EGFR), were found effective in combination with chemotherapy or as a single agent for the treatment of chemotherapy-resistant mCRC [4–6]. However, the tumor response rate increased by anti-EGFR MAbs was only 10%-20%, whether it be used as the 1st- or 2nd-line treatment [4, 6–9]. As anti-EGFR MAbs were associated with significant increase in toxicities [5] and costs [10], it is important to identify the responsive patients for treatment and prevent non-responsive ones from exposure to unnecessary treatment.
It has been established that KRAS mutations are a strong predictor of resistance to anti-EGFR MAbs [11–13]. However, a significant proportion of patients with wild-type KRAS remain unresponsive to anti-EGFR MAbs. Therefore, the identification of new biomarkers that can be used jointly with KRAS has become appealing in predicting treatment response.
Moroni and colleagues reported for the first time a strong relation between EGFR gene copy number (GCN) and the response of patients to anti-EGFR MAbs [14]. This relation has since been substantially investigated. However, published studies on this topic are generally small in sample size, which may have led to inconsistent results, and thus each study alone may not be strong enough to produce a firm conclusion [15]. In addition, sparse data from individual studies is available to assess the impact of EGFR GCN on such patient-important outcomes as progression-free survival (PFS) and overall survival (OS) [16, 17].
Therefore, we conducted a systematic review of current evidences to assess the predictive role of an increase of EGFR GCN in the treatment of mCRC with anti-EGFR MAbs, with a hope to take a step further towards the ultimate end of personalized treatment of mCRC.
Results
Figure 1 shows the inclusion and exclusion of studies step by step. In total, 19 eligible studies were identified [14–32], of which 17 provided data on ORR [14–26, 28–31] and 15 on PFS or OS [15–21, 24, 25, 27–32].
Description of the studies
The basic characteristics of these studies were summarized in Table 1. Most of them were retrospective studies, with sample sizes varying from 27 to 155. Three studies were conducted in KRAS wild-type patients only [16, 31, 32], and another eight studies reported the data on KRAS wild-type and mutant patients separately [14, 18, 19, 22, 24–26, 28], providing us the opportunity to examine the impact of KRAS status on the predictive power of GCN+. The anti-EGFR MAb administered, the response criteria, and the assay for EGFR GCN quantification were generally consistent across different studies. However, the lines of treatment and the sources of tumor samples used for GCN testing were relatively inconsistent.
Most notably, the criteria for GCN + were highly heterogeneous among different studies. In one study [26], only gene amplification was considered as GCN+. In six studies [15, 16, 22–24, 30], GCN + included both high level of polysomy and amplification. In two studies [17, 21], all levels of polysomy and amplification were considered as GCN+. The definitions of polysomy, high polysomy, and amplification, respectively, also varied across studies. The most commonly used criteria for high polysomy and amplification were “≥ 4 gene copies in ≥ 40 % of cells” [15, 16, 23, 24, 30] and “gene/CEP7 ≥ 2, or ≥ 15 gene copies in ≥ 10% of cells” [15, 23, 24, 30], respectively. In seven studies [14, 18–20, 27, 28, 31], only the average gene copies per nucleus was used to define GCN+, with the cutoff points varying from 2.6 to 3. For two of the seven studies [14, 27] where the cutoff point was “gene copies/nucleus ≥ 3”, GCN + could be viewed as polysomy according to the definition given in the study of Sartore-Bianchi et al. [17]. Similarly, the criteria used in the study of Tol et al. [32] was “gene copies/nucleus ≥3, or gene/CEP7 ≥ 2”, which could be viewed as approximate to “polysomy or amplification” according to the definitions from the studies of Campanella et al., Sartore-Bianchi et al., and others (Table 1).
The prevalence of GCN + in these studies ranged from 6.9% to 88.9%, partly reflecting the significant heterogeneity in the criteria for GCN+. Even in studies that used the same criteria to define GCN+, the prevalence of GCN + also varied considerably. For example, see the studies of Bengala et al. and Cappuzzo et al.; the studies of Gevorgyan et al., Goncalves et al., Italiano et al. and Sastre et al.; the studies of Mancuso et al. and Moroni et al.; or the studies of Perrone et al. and Personeni et al. (Table 1). As shown in Table 2, the prevalence of gene amplification was generally low, ranging from 0 to 10%, except in two studies.
The association of EGFR gene copy number status with clinical outcomes
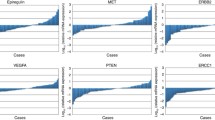
The ORRs stratified by EGFR GCN status were summarized Figure 2. There was significant statistical heterogeneity among the studies (P < 0.00001, I2 = 78%). Even when we pooled only the studies using identical criteria for GCN+, the heterogeneity sustained. In view of this, and especially considering the heterogeneous methodological as well as clinical characteristics, we decided not to perform quantitative synthesis of the studies, for it would be clinically meaningless and the results would be difficult to interpret.
The difference in ORRs between patients with GCN + and those with GCN- varied from −28% to 84%. Visually, there was a general trend towards higher ORR in patients with GCN + (Figure 2). Five studies [14, 19, 22, 26, 28] provided data on the ORR of EGFR amplified patients, which also indicated a trend that the ORR increased with GCN (Table 2), although the sample sizes were too small to produce a firm conclusion. Of the 22 EGFR amplified patients, 18 experienced an objective response, representing an ORR of 82%. Among the four patients who did not respond, three had KRAS or PIK3CA exon 20 mutations [14, 22].
Based on the data from 10 studies [14, 16, 18, 19, 22, 24–26, 28, 31], we further examined the association of EGFR GCN status with objective response in wild-type and mutant KRAS patients, respectively (Figure 3). Apparently, the difference in ORRs between GCN + and GCN- patients was much greater in wild-type than in mutant KRAS patients. Among patients with KRAS mutations, there was usually no difference between GCN + and GCN- patients. The only exception is the study of Moroni et al. (Figure 3), in which the sample size was quite small, and both patients in the GCN + group had EGFR amplification [14].
Difference in objective response rate between GCN + and GCN- patients, stratified by KRAS status. In patients with wild-type KRAS , the total events and patients were 73 and 124, respectively, for GCN + group, and were 61 and 230, respectively, for GCN- group. Heterogeneity test: P =0.02, I 2 = 54%. In patients with mutant KRAS, the total events and patients were 7 and 44, respectively, for GCN + group, and were 2 and 97, respectively, for GCN- group. Heterogeneity test: P =0.005, I2 = 70%.
PFS data was reported in 15 studies (Table 3), of which 13 showed a trend of longer PFS in GCN + patients than in GCN- patients, although the difference was tested for significance in only ten studies and was statistically significant only in six of them. Two studies [21, 29] reported hazard ratios for the comparison of the PFS of GCN + versus GCN- patients, which were 0.54 (95% CI: 0.32-0.93) and 0.82 (95% CI: 0.29-2.26), respectively, both favoring GCN + patients. Eight studies provided data on OS [15–18, 20, 28, 31, 32], and six of them reported a longer OS in GCN + than in GCN- patients, although the difference was statistically significant in only two studies.
Publication bias
Because of the substantial heterogeneity among the included studies, we did not conduct the test for publication bias using funnel plot, for it would probably be misleading in this case [33, 34].
Discussion
This systematic review summarized the evidences on the predictive value of EGFR GCN + for clinical outcomes of mCRC treated with anti-EGFR MAbs. The data we collected showed that generally GCN + was associated with a better objective response, especially among patients with wild-type KRAS, which supports the notions that KRAS mutations are a strong predictor of non-response to the anti-EGFR MAbs treatment [11–13], and new biomarkers for the treatment would be primarily useful in KRAS wild-type patients [35].
However, the present systematic review was limited by the following factors. First, the majority of the included studies was retrospective in their nature, and thus might have suffered from some important bias. Second, there was significant heterogeneity among the studies, which precluded a clinically meaningful meta-analysis of the quantitative data. Third, although the PFS and OS were seemingly longer in GCN + than in GCN- patients, the data on these outcomes was relatively incomplete to convincingly support our conclusion on objective response.
More importantly, current evidences suggest that the clinical utility of EGFR GCN would be severely limited by two major problems. First, the scoring system of EGFR GCN has a high inter-laboratory variability, and none of the criteria used to define GCN + universally outperformed other criteria in terms of the discriminatory power. In some studies, the cutoff point for GCN + was identified by Receiver Operating Characteristics analysis, but frequently a cutoff value shown to have good sensitivity and specificity in one study performed less well in another. For example, in the study of Cappuzzo et al. [18], the cutoff point “gene copies/nucleus ≥ 2.92” categorized the patients into two groups in which the ORR were 33% (14/43) and 2% (1/42), respectively, with a sensitivity of 58.6% and a specificity of 93.3%. However, when the cutoff value was applied to the patients in the study of Personeni et al. [28], the corresponding sensitivity and specificity were only 56.0% and 75.8%, respectively. A standard cutoff value that can be used as a reference is yet to be established. Of note, even in studies that used the same criteria for GCN+, there was also significant variability in the difference of ORRs between GCN + and GCN- patients. For example, see the studies of Gevorgyan et al., Goncalves et al., Italiano et al. and Sastre et al. (Figure 2).
The criteria for EGFR gene amplification have been relatively consistent across studies [15, 16, 21, 24], and patients with this molecular alteration generally had good response to anti-EGFR MAbs. In addition, it is readily identifiable by fluorescent in situ hybridization (FISH) assay. However, EGFR gene amplification proved to be a rare event, rendering it clinically less significant. Most patients defined as GCN + in the studies were actually harboring “polysomy” or “high polysomy”. Whether these statuses are equal to amplification in terms of their biological effects and especially the impact on the response to anti-EGFR MAbs remains unclear.
Second, the enumeration of EGFR GCN suffers from poor reproducibility. One reason for this is the within-tumor variation [36]. For example, the mean EGFR GCN of different sections within a tumor could be highly heterogeneous, leading to potential misclassification of EGFR GCN status in up to 39% of patients [28]. To a greater degree, the poor reproducibility is due to technical factors. For example, the thickness of tumor sections might affect the EGFR GCN detected, with thinner sections possibly responsible for a lower GCN cutoff value [18]. Notably, a recent international inter-laboratory reproducibility ring study [37] conducted by five “highly experienced molecular diagnostic centers” showed that even under standardized conditions, the results of FISH analysis, which was the most commonly used method the determine EGFR GCN, could still vary drastically from one laboratory to another. The low consensus rate was proposed to be related with such technical factors as the equipment used for the analyses, the skills necessary to perform enumeration of GCN, and the personnel difference in interpreting the pre-specified guidelines [37]. Although it is possible to enhance the consensus by intensive staff training in a research setting, it would be difficult to achieve this goal in routine practice. To date, scientifically validated and widely accepted protocol and guidelines for detecting EGFR GCN, which have been available for non-small cell lung cancer [38], remain to be developed for mCRC. This may partly explain why EGFR GCN has not yet been incorporated into clinical practice.
Conclusions
Although increased EGFR GCN is generally associated with a better outcome of anti-EGFR MAbs treatment, especially among patients with wild-type KRAS, the clinical utility of this biomarker for selecting recipients of anti-EGFR MAbs would be severely limited by the heterogeneous scoring system and the poor reproducibility of EGFR GCN enumeration due to technical reasons.
Methods
Literature search
We performed a systematic search of PubMed, EMBASE, The Cochrane Library, Chinese Biomedical Literature Database, and Wanfang Data from inception to 22 November 2010. The detailed search strategy was described in the Additional file 1. Briefly, both the MeSH terms and various text words for CRC, MAbs and EGFR were used to identify relevant publications. The search was in the end limited to “human studies”. In the light of the results of our pilot search, we did not include the terms related to the biomarker (i.e. “gene copy number”) and concerned outcomes (e.g., “objective response” and “overall survival”) in the final search strategy so as to increase the search sensitivity. In addition to searching the above electronic databases, we also tried to identify eligible studies from the conference abstracts of American Society of Clinical Oncology and European Society of Medical Oncology via their official websites. All potentially relevant studies were retrieved and their references were scrutinized for further relevant publications.
Study selection
All “potentially eligible” studies were reviewed independently and then agreed on their eligibility by two reviewers. Studies that met all of the following four criteria were considered eligible for this review: 1) patients: mCRC; 2) treatment: MAbs as monotherapy or in combination with other agents for treatment of any lines; 3) biomarker: EGFR GCN; and 4) outcomes: one or more of the following outcomes stratified by EGFR GCN status: objective response (the sum of complete response and partial response), PFS, and OS. Although PFS theoretically differs from time-to-progression, the two outcomes were often used interchangeably in existing clinical cancer research. Therefore, we did not distinguish them in this meta-analysis, but used PFS alone to denote either of the two. When the same patient population was used in more than one publication, only the one with most relevant data was included in this review. Disagreements between the two reviewers were resolved by discussion. Unsettled disagreements which were few were referred to the “third wise man” for final verdict.
Data extraction
The following data were collected from each eligible study: first author’s name, year of publication, study design, total number of patients eligible to be included in this systematic review, KRAS mutation status, number of patients with increased EGFR GCN (GCN+) (stratified by KRAS mutation status, if applicable), number of patients with non-increased GCN (GCN-) (stratified by KRAS mutation status, if applicable), line of treatment, treatment regimen, response criteria, original location of tumor tissues used for analysis, method for EGFR GCN analysis, criteria for “GCN+”, objective response rate (ORR), PFS, OS, and hazard ratio for the comparison of PFS/OS. Data on ORR, PFS, and OS were extracted separately according to EGFR GCN status (further according to KRAS mutation status, if applicable).
With respect to the line of treatment, we pragmatically categorized a study as “1st-line” if ≥ 90% of the patients received 1st-line MAbs treatment. Similarly, a study was considered as “≥ 2nd-line” if ≥ 90% of the patients received 2nd-line or higher anti-EGFR MAbs treatment. All other studies were categorized as “mixed”. The same principle was applied to “treatment regimen” (monotherapy vs combined-therapy vs mixed) and “original location of tumor tissues used for analysis” (primary vs metastatic vs mixed).
If any key data (e.g. the number of patients responsive to anti-EGFR MAbs by EGFR GCN status) was absent in the original paper, authors were contacted by e-mail for relevant information.
Statistical methods
The outcomes of interest included objective response, PFS, and OS. The impact of EGFR GCN status on objective response was measured by risk difference, which was the ORR of patients with GCN + subtracted by that of patients with GCN-. The association of EGFR GCN status with PFS or OS was denoted by hazard ratio. A hazard ratio equal to one means no difference between the compared groups. A hazard ratio less than one indicates that the risk for disease progression or death was lower in patients with GCN + than in those with GCN-, i.e. the PFS or OS of patients with GCN + was longer than that of patients with GCN-, and vice versa.
The statistical heterogeneity among studies was assessed by the Cochran’s Q-test [39, 40] and the I2 statistic [40, 41]. A P value ≤ 0.10 for the Q-test or an I2 > 50% was suggestive of substantial between-study heterogeneity. The clinical and methodological characteristics of the eligible studies were also examined to see if a quantitative synthesis of the collected data was appropriate. If not, then the data was summarized and presented in a descriptive manner; if yes, then the risk differences and hazard ratios respectively from different studies were combined by using a random-effects model (DerSimonian and Laird method) [41, 42]. Further meta-analyses of risk difference and/or hazard ratio, stratified by KRAS status, would be performed wherever possible.
If appropriate and data allowed us to do so, pre-specified subgroup analyses were conducted to explore the source of the heterogeneity according to treatment regimen, line of treatment, response criteria, original location of tumor tissues used for analysis, method for EGFR GCN analysis, and the cutoff value for GCN+. Egger’s funnel plot was planned to be used to assess the possibility of publication bias as appropriate [43]. All statistical analyses were performed in RevMan 5.0.
Abbreviations
- CEP7:
-
chromosome 7
- EGFR:
-
epidermal growth factor receptor
- GCN:
-
gene copy number
- GCN+:
-
increased epidermal growth factor receptor gene copy number
- GCN-:
-
non-increased epidermal growth factor receptor gene copy number
- mCRC:
-
metastatic colorectal cancer
- MAbs:
-
monoclonal antibodies
- PFS:
-
progression-free survival
- ORR:
-
objective response rate
- OS:
-
overall survival.
References
GLOBOCAN: Cancer fact sheet. 2008, [http://globocan.iarc.fr/factsheets/cancers/colorectal.asp#INCIDENCE1]
Meyerhardt JA, Mayer RJ: Systemic therapy for colorectal cancer. N Engl J Med. 2005, 352: 476-487. 10.1056/NEJMra040958.
Sargent DJ, Wieand HS, Haller DG: Disease-free survival versus overall survival as a primary end point for adjuvant colon cancer studies: individual patient data from 20,898 patients on 18 randomized trials. J Clin Oncol. 2005, 23: 8664-8670. 10.1200/JCO.2005.01.6071.
Bokemeyer C, Bondarenko I, Makhson A: Fluorouracil, leucovorin, and oxaliplatin with and without cetuximab in the first-line treatment of metastatic colorectal cancer. J Clin Oncol. 2009, 27: 663-671. 10.1200/JCO.2008.20.8397.
Tol J, Punt CJ: Monoclonal antibodies in the treatment of metastatic colorectal cancer: a review. Clin Ther. 2010, 32: 437-453. 10.1016/j.clinthera.2010.03.012.
Van Cutsem E, Köhne CH, Hitre E: Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. N Engl J Med. 2009, 360: 1408-1417. 10.1056/NEJMoa0805019.
Sobrero AF, Maurel J, Fehrenbacher L: EPIC: phase III trial of cetuximab plus irinotecan after fluoropyrimidine and oxaliplatin failure in patients with metastatic colorectal cancer. J Clin Oncol. 2008, 26: 2311-2319. 10.1200/JCO.2007.13.1193.
Peeters M, Price TJ, Cervantes A: Randomized phase III study of panitumumab with fluorouracil, leucovorin, and irinotecan (FOLFIRI) compared with FOLFIRI alone as second-line treatment in patients with metastatic colorectal cancer. J Clin Oncol. 2010, 28: 4706-4713. 10.1200/JCO.2009.27.6055.
Douillard JY, Siena S, Cassidy J: Randomized, phase III trial of panitumumab with infusional fluorouracil, leucovorin, and oxaliplatin (FOLFOX4) versus FOLFOX4 alone as first-line treatment in patients with previously untreated metastatic colorectal cancer: the PRIME study. J Clin Oncol. 2010, 28: 4697-4705. 10.1200/JCO.2009.27.4860.
Schrag D: The Price Tag on Progress — Chemotherapy for Colorectal Cancer. N Engl J Med. 2004, 351: 317-319. 10.1056/NEJMp048143.
Dahabreh IJ, Terasawa T, Castaldi PJ: Systematic review: Anti-epidermal growth factor receptor treatment effect modification by KRAS mutations in advanced colorectal cancer. Ann Intern Med. 2011, 154: 37-49.
Linardou H, Dahabreh IJ, Kanaloupiti D: Assessment of somatic k-RAS mutations as a mechanism associated with resistance to EGFR-targeted agents: a systematic review and metaanalysis of studies in advanced non-small-cell lung cancer and metastatic colorectal cancer. Lancet Oncol. 2008, 9: 962-972. 10.1016/S1470-2045(08)70206-7.
Qiu LX, Mao C, Zhang J: Predictive and prognostic value of KRAS mutations in metastatic colorectal cancer patients treated with cetuximab: a meta-analysis of 22 studies. Eur J Cancer. 2010, 46: 2781-2787. 10.1016/j.ejca.2010.05.022.
Moroni M, Veronese S, Benvenuti S: Gene copy number for epidermal growth factor receptor (EGFR) and clinical response to antiEGFR treatment in colorectal cancer: a cohort study. Lancet Oncol. 2005, 6: 279-286. 10.1016/S1470-2045(05)70102-9.
Italiano A, Follana P, Caroli FX: Cetuximab shows activity in colorectal cancer patients with tumors for which FISH analysis does not detect an increase in EGFR gene copy number. Ann Surg Oncol. 2008, 15: 649-654. 10.1245/s10434-007-9667-2.
Laurent-Puig P, Cayre A, Manceau G: Analysis of PTEN, BRAF, and EGFR status in determining benefit from cetuximab therapy in wild-type KRAS metastatic colon cancer. J Clin Oncol. 2009, 27: 5924-5930. 10.1200/JCO.2008.21.6796.
Sartore-Bianchi A, Moroni M, Veronese S: Epidermal growth factor receptor gene copy number and clinical outcome of metastatic colorectal cancer treated with panitumumab. J Clin Oncol. 2007, 25: 3238-3245. 10.1200/JCO.2007.11.5956.
Cappuzzo F, Finocchiaro G, Rossi E: EGFR FISH assay predicts for response to cetuximab in chemotherapy refractory colorectal cancer patients. Ann Oncol. 2008, 19: 717-723.
Perrone F, Lampis A, Orsenigo M: PI3KCA/PTEN deregulation contributes to impaired responses to cetuximab in metastatic colorectal cancer patients. Ann Oncol. 2009, 20: 84-90.
Bengala C, Bettelli S, Fontana A: EGFR gene copy number, KRAS and BRAF status, PTEN and AKT expression analysis in patients with metastatic colon cancer treated with anti-EGFR monoclonal antibodies ± chemotherapy [abstract]. J Clin Oncol. 2009, 27: 15055-
Campanella C, Mottolese M, Cianciulli A: Epidermal growth factor receptor gene copy number in 101 advanced colorectal cancer patients treated with chemotherapy plus cetuximab. J Transl Med. 2010, 8: 36-43. 10.1186/1479-5876-8-36.
Frattini M, Saletti P, Romagnani E: PTEN loss of expression predicts cetuximab efficacy in metastatic colorectal cancer patients. Br J Cancer. 2007, 97: 1139-1145. 10.1038/sj.bjc.6604009.
Gevorgyan A, Di Bartolomeo M, Andreola S: Epidermal Growth Factor Receptor (EGFr) status detection in correlation to objective response on cetuximab-based therapy in patients (pts) with advanced colorectal cancer (ACC) [abstract]. In: 2007 ASCO Annual Meeting Proceedings Part I. J Clin Oncol. 2007, 25 (18): 21070-
Goncalves A, Esteyries S, Taylor-Smedra B: A polymorphism of EGFR extracellular domain is associated with progression free-survival in metastatic colorectal cancer patients receiving cetuximab-based treatment. BMC Cancer. 2008, 8: 169-179. 10.1186/1471-2407-8-169.
Khambata-Ford S, Garrett CR, Meropol NJ: Expression of epiregulin and amphiregulin and K-ras mutation status predict disease control in metastatic colorectal cancer patients treated with cetuximab. J Clin Oncol. 2007, 25: 3230-3237. 10.1200/JCO.2006.10.5437.
Lievre A, Bachet JB, Le Corre D: KRAS mutation status is predictive of response to cetuximab therapy in colorectal cancer. Cancer Res. 2006, 66: 3992-3995. 10.1158/0008-5472.CAN-06-0191.
Mancuso A, Leone A, Vigna L: EGFR, DCC, and K-RAS mutations as predictive factors for cetuximab sensitivity in metastatic colorectal cancer (mCRC) [abstract]. J Clin Oncol. 2008, 26 (20): 4128-
Personeni N, Fieuws S, Piessevaux H: Clinical usefulness of EGFR gene copy number as a predictive marker in colorectal cancer patients treated with cetuximab:a fluorescent in situ hybridization study. Clin Cancer Res. 2008, 14: 5869-5876. 10.1158/1078-0432.CCR-08-0449.
Razis E, Briasoulis E, Vrettou E: Potential value of PTEN in predicting cetuximab response in colorectal cancer:an exploratory study. BMC Cancer. 2008, 8: 234-243. 10.1186/1471-2407-8-234.
Sastre J, Aranda E, Grávalos C: First-line single-agent cetuximab in elderly patients with metastatic colorectal cancer. A phase II clinical and molecular study of the Spanish group for digestive tumor therapy (TTD). Crit Rev Oncol Hematol. 2011, 77: 78-84. 10.1016/j.critrevonc.2009.11.005. Epub 2009 Dec 29
Scartozzi M, Bearzi I, Mandolesi A: Epidermal Growth Factor Receptor (EGFR) gene copy number (GCN) correlates with clinical activity of irinotecan-cetuximab in K-RAS wild-type colorectal cancer:a fluorescence in situ (FISH) and chromogenic in situ hybridization (CISH) analysis. BMC Cancer. 2009, 9: 303-311. 10.1186/1471-2407-9-303.
Tol J, Dijkstra JR, Klomp M: Markers for EGFR pathway activation as predictor of outcome in metastatic colorectal cancer patients treated with or without cetuximab. Eur J Cancer. 2010, 46: 1997-2009. 10.1016/j.ejca.2010.03.036.
Lau J, Ioannidis JP, Terrin N, Schmid CH, Olkin I: The case of the misleading funnel plot. BMJ. 2006, 333: 597-600. 10.1136/bmj.333.7568.597.
Tang JL, Liu JL: Misleading funnel plot for detection of bias in meta-analysis. J Clin Epidemiol. 2000, 53: 477-84. 10.1016/S0895-4356(99)00204-8.
Mao C, Yang ZY, Hu XF: PIK3CA exon 20 mutations as a potential biomarker for resistance to anti-EGFR monoclonal antibodies in KRAS wild-type metastatic colorectal cancer:a systematic review and meta-analysis. Ann Oncol. 2012, 23: 1518-1525. 10.1093/annonc/mdr464.
Ooi A, Takehana T, Li X: Protein overexpression and gene amplification of HER-2 and EGFR in colorectal cancers:an immunohistochemical and fluorescent in situ hybridization study. Mod Pathol. 2004, 17: 895-904. 10.1038/modpathol.3800137.
Sartore-Bianchi A, Fieuws S, Veronese S: Standardisation of EGFR FISH in colorectal cancer:results of an international interlaboratory reproducibility ring study. J Clin Pathol. 2012, 65: 218-223. 10.1136/jclinpath-2011-200353.
Varella-Garcia M, Diebold J, Eberhard DA: EGFR fluorescence in situ hybridisation assay:guidelines for application to non-small-cell lung cancer. J Clin Pathol. 2009, 62: 970-977. 10.1136/jcp.2009.066548.
Cochran WG: The combination of estimates from different experiments. Biometrics. 1954, 10: 101-129. 10.2307/3001666.
Higgins JPT, Thompson SG, Deeks JJ, Altman DG: Measuring inconsistency in meta-analyses. BMJ. 2003, 327: 557-560. 10.1136/bmj.327.7414.557.
Deeks JJ, Higgins JPT, Altman DG: Analysing and presenting results. 2006, In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions 4.2.6 [updated September 2006], Section 8, Chichester, UK: John Wiley & Sons, Ltd, 4-
DerSimonian R, Laird N: Meta-analysis in clinical trials. Control Clin Trials. 1986, 7: 177-188. 10.1016/0197-2456(86)90046-2.
Egger M, Smith DG, Schneider M, Minder C: Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997, 315: 629-634. 10.1136/bmj.315.7109.629.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Competing interests
The authors have declared no conflicts of interest.
Authors’ contributions
ZYY, WXS, CM, and JLT designed the systematic review; ZYY, WXS, XFH, DYZ, XYW, YFH, JZC, and CM were involved in the literature search and study selection; ZYY, XFH, XYW, YFH, and CM extracted the data from eligible studies; ZYY and CM conducted the analysis; ZYY, WXS, DYZ, JZC, CM, and JLT were involved in the interpretation of the results. ZYY, WXS, CM, and JLT were responsible for the writing and critical revisions of the manuscript. All authors read and approved the final manuscript.
Zu-Yao Yang, Wei-Xi Shen contributed equally to this work.
Electronic supplementary material
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Yang, ZY., Shen, WX., Hu, XF. et al. EGFR gene copy number as a predictive biomarker for the treatment of metastatic colorectal cancer with anti-EGFR monoclonal antibodies: a meta-analysis. J Hematol Oncol 5, 52 (2012). https://doi.org/10.1186/1756-8722-5-52
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1756-8722-5-52