Abstract
Background
Pulmonary hypertension (PH) is present in a significant proportion of patients with end stage renal disease (ESRD) and is of prognostic importance. Data on the effect of renal transplant on PH is very limited. In this study, the aim was to examine the effect of renal transplant on systolic pulmonary artery pressure (SPAP) determined by Doppler echocardiography.
Methods
Analysis was performed on the records of 500 consecutive patients who underwent renal transplant at our center between the years 1999 to 2008. The prevalence of PH in the preoperative assessment period was established. Patients were diagnosed as having PH when measured SPAP values were > 35 mm Hg.
Results
Pulmonary hypertension was detected in 85 of the 500 (17%) patients under pre-transplant evaluation. At post-transplant follow up Doppler echocardiographic examination was performed on 50 of the 85 patients. After exclusion of 8 cases (1 due to massive pulmonary thromboemboli; 7 due to graft failure requiring dialysis therapy) analyses were performed on 42 patients who had undergone both pre- and post-transplant echocardiographic examination. Mean SPAP at pre-transplant evaluation was 45.9 ± 8.8 mm Hg and in 6 (14.3%) cases SPAP was above 50 mm Hg.
Compared to pre-transplant values, a significant decrease was observed in mean SPAP values in an average of 53 months of postoperative follow up (41.8 ± 7.4 mm Hg vs. 45.9 ± 8.8 mm Hg, p < 0.0001).
Conclusion
These findings indicate that patients with ESRD accompanied by PH may benefit from renal transplant. Further research is required for more concrete conclusions to be drawn on this subject.
Riassunto
Razionale
L’ipertensione polmonare (PH) è presente in una quota rilevante di pazienti con grave insufficienza renale ed ha rilevanza prognostica. Dati sugli effetti del trapianto renale sulla PH sono molto limitatı. Scopo di questo studio era valutare gli effetti del trapianto renale sulla pressione arteriosa polmonare sistolica (SPAP) stimata con l’ecocardiografia Doppler.
Metodi
Analisi retrospettiva dei dati di 500 pazienti consecutivi sottoposti a trapianto renale presso il nostro centro tra il 1999 ed il 2008. È stata individuata la prevalenza di PH nel periodo di valutazione pre-trapianto, definita come valore di SPAP > 35 mm Hg.
Risultati
Una ipertensione polmonare è stata diagnosticata in 85 (17%) dei 500 pazienti sottoposti a valutazione pre-trapianto. Al follow up post-trapianto 50 degli 85 pazienti sono stati sottoposti ad una ecocardiografia Doppler. Dopo avere escluso 8 casi (1 per tromboembolia polmonare massiva, 7 per fallimento del trapianto che ha reso necessario proseguire con la dialisi) l’analisi è stata effettuata sui 42 pazienti di cui erano disponibili i dati pre- e post-trapianto. Il valore medio della SPAP alla valutazione pre-trapianto era 45,9 ± 8,8 mm Hg e in 6 (14,3%) casi la SPAP era oltre 50 mm Hg. Dopo trapianto si è osservata una riduzione significativa dei valori medi di SPAP nei 53 mesi di media del follow up post-trapianto (41,8 ± 7,4 mm Hg vs 45,9 ± 8,8 mm Hg, p < 0,0001).
Conclusioni
I nostri dati indicano che i pazienti con PH associata a ESRD possono trarre beneficio dal trapianto di rene, ma ulteriori studi saranno necessari per trarre conclusioni più certe su questo tema.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Pulmonary hypertension (PH) is seen in a significant proportion of patients with end stage renal disease (ESRD) [1–3]. The prevalence of PH has been reported to be as high as 48% [4]. A variety of mechanisms are proposed to contribute to the development of PH in uremic patients. Duration of renal replacement therapy, extraosseous pulmonary calcification, high cardiac output due to arterio-venous fistula or other causes, anemia, fluid overload, hormonal and metabolic imbalances associated with uremic milieu and impaired endothelial function are among various mechanisms responsible for elevation of pulmonary artery pressure (PAP) [4, 5].
It has been shown that PH is important prognostically in patients with ESRD as in other patient groups with this disorder [6, 7]. It is a progressive disease. Unless diagnosed early and treated appropriately, the course of PH is usually fatal due to the development of right ventricular failure. In addition to other comorbidities and age, it stands as an independent predictor of survival in patients with renal failure [8]. However, data about the impact of renal transplant on PH in patients with ESRD is limited. Therefore, in this study, the effect of renal transplant on PH determined by Doppler echocardiography in the pre-transplant and post-transplant period was examined.
Methods
Analyses of the records of 500 consecutive patients who underwent renal transplant at our center between the years 1999 to 2008 was undertaken. Demographic, clinical information and laboratory results were obtained. The prevalence of PH on preoperative assessment was obtained. At post-transplant follow up Doppler echocardiographic examination was performed on 50 patients. Eight patients were excluded due to rejection and massive pulmonary emboli. Thus 42 patients who had both pre-and postoperative Doppler echocardiographic examination were included for analysis.
In the absence of right ventricular outflow obstruction or pulmonary stenosis, non-invasive determination of pulmonary artery pressure by Doppler echocardiography has been shown to be closely correlated with that measured on catheterization [9, 10].
As part of the preoperative cardiopulmonary workup, a comprehensive transthoracic Doppler echocardiographic examination was performed. Using continuous wave Doppler the maximum tricuspid regurgitant flow (v) was determined. The modified Bernoulli equation was used to estimate right ventricular systolic pressure (RVP) which was considered to be equal to the systolic pulmonary artery pressure (SPAP) in the absence of right ventricular outflow obstruction or pulmonary valve stenosis: SPAP (mm Hg) = RVP = 4v2 + right atrial pressure [11]. Patients were diagnosed with PH when the Doppler echocardiographic SPAP values measured > 35 mm Hg. It was classified as mild to moderate when SPAP was 35-50 mm Hg, and severe when SPAP was > 50 mm Hg [12].
Left ventricular hypertrophy (LVH) was determined when the interventricular septum or posterior wall thickness was ≥ 12 mm. Left ventricular systolic dysfunction was defined as global or regional wall-motion abnormality on echocardiography or ventriculography, ejection fraction (EF) less than 50%, or fractional shortening less than 25%. Diastolic dysfunction was defined as mitral E/A ratio less than 1 and isovolumetric relaxation time ≥ 110 msec or mitral E-wave deceleration time ≥ 240 msec on Doppler echocardiography.
The study protocol was approved by the Institutional Ethics Committee.
Statistical analysis
Data were analyzed using the SPSS version 12.0 (Chicago, IL, USA) statistical program. The distribution of continuous variables for normality was tested with the one-sample Kolmogorov-Smirnov test, and data are presented as mean ± standard deviation (SD) or median and interquartile ranges, as appropriate. Differences between patients with and without PH in normally and abnormally distributed variables were evaluated using the unpaired t test and the Mann-Whitney U test, respectively. The chi-square test was employed to compare nonparametric variables. For comparison of the pre- and post-transplant values the paired t test was used. All p values are 2-sided, and the significance level was considered as p < 0.05.
Results
Pulmonary hypertension was detected in 85 of the 500 (17%) patients at pre-transplant evaluation based on Doppler echocardiographic examination. A comparison of the characteristics of patients with and without PH is presented in Table 1.
Post-transplant echocardiographic examination was performed on 50 of these 85 patients. After exclusion of 8 cases (1 due to massive pulmonary thromboemboli, 7 due to graft failure requiring dialysis therapy) analyses were performed. The demographic and clinical data of the study population with PH prior to renal transplant are shown in Table 2. The mean age was 33.9 ± 10.8 years and 12 (28.6%) were female. The mean duration of dialysis therapy prior to renal transplant was 47.1 months. With regard to type of renal replacement therapy, 41 patients were on hemodialysis and 1 patient was on peritoneal dialysis. Hypertension was the most common etiology of ESRD followed by glomerulo nephritis. Renal transplant was performed from living donors in 28 (66.7%) and from a deceased donor in 14 (33.3%) patients.
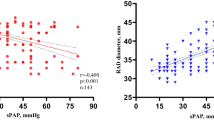
The mean value of systolic PAP on pre-transplant evaluation was 45.9 ± 8.8 mm Hg and in 6 (14.3%) cases systolic PAP was above 50 mm Hg. Compared to pre-transplant values a significant decrease was observed in mean SPAP values in an average 53 months of postoperative follow up (45.9 ± 8.8 mm Hg pre vs. 41.8 ± 7.4 mm Hg post, p < 0.0001). With regard to change in systolic PAP values, a decrease was noted in 25 (59.5%), an increase in 4 (9.5%) and no change in the remaining 13 (31%) patients following the transplantation. At post-transplant evaluation systolic PAP was above 50 mm Hg in 5 patients. Of these 5 cases 1 had angiographically proven coronary artery disease (CAD), 1 had left ventricular systolic and 2 had diastolic dysfunction on echocardiographic examination. No significant valvular heart disease was identified. With regard to type of dialysis all were on HD prior to transplant.
Although an increase was noted in mean left ventricular ejection fraction following the renal transplant, it did not reach a statistically significant level (pre-transplant 49.6 ± 8.2% vs. post-transplant 51.0 ± 7.1%, p = 0.1) (Table 3). At echocardiographic evaluation, left ventricular hypertrophy was identified in 33 (78.6%) patients. In 7 cases a mild degree of left ventricular systolic dysfunction was detected. Five patients had undergone coronary angiography and 1 of these was diagnosed with CAD. In 16 patients diastolic dysfunction was identified, in all cases of the grade 1 abnormal relaxation type. On preoperative evaluation no valvular stenosis was diagnosed in any of the participants. Only minor valvular insufficiency in 1 patient with mild to moderate aortic regurgitation and in 8 patients with mild to moderate mitral regurgitation was detected. At postoperative echocardiographic examination, a moderate to severe mitral insufficiency was detected in 1 case. No significant changes in other valvular pathologies were noted.
Discussion
It is well known that cardiovascular diseases are very common and are the most frequent cause of mortality in patients with ESRD. For this reason, the focus is on ischemic heart disease, heart failure and arrhythmias in these patients. In contrast to other forms of cardiovascular diseases, data on PH in patients with ESRD is limited.
In the general population left-sided heart disease and chronic hypoxic lung disorders are the most common causes of PH. Although the exact cause is not proven, a multifactorial etiology appears to be responsible for the development of PH in patients with renal failure. We previously identified, in a recent paper, that the duration of dialysis therapy, hemodialysis via arteriovenous fistula as the type of renal replacement therapy, and left ventricular ejection fraction were the independent predictors of PH [5]. Issa et al. also reported duration of dialysis as an independent predictor of PH in ESRD patients [13]. Low EF, ischemic heart disease, heart failure, valvular heart disease and arteriovenous fistulas are some of the other factors that appear to be responsible for the development of PH in the ESRD population [3, 4].
The prevalence of PH in our study group (17%) is slightly lower than that reported in the literature (Table 4). The low prevalence may be due to the young age of the study population. Additionally, in previous studies, echocardiography was performed on patients who were perceived as having an increased risk of heart disease. In our center, all pre-transplant patients are evaluated with Doppler echocardiography. This may be another reason for the low PH ratio in our patients. Since a large number of patients were enrolled and all patients underwent Doppler echocardiographic examination, it is our belief that these findings provide more representative data.
Data regarding the impact of renal transplant on PH are very limited. In a recent paper Issa et al. reported that pre-transplant PH correlates with survival after renal transplant [13]. In that paper the authors looked at the records of 215 patients who underwent renal transplant. Of these patients pre-transplant PH on Doppler echocardiography was detected in 69 (32%). It was mild to moderate (SPAP 3650 mm Hg) in 47 (22%) and severe (SPAP > 50 mm Hg) in 22 (10%) patients. Severe PH was identified as the independent predictor of post-transplant survival when adjusted for other variables such as age, low ejection fraction and hypoalbuminemia.
Regardless of etiology, PH has prognostic impact in this patient population and renal transplant appears to lower elevated SPAP. Unfortunately, there are limited data on drug therapy for PH in uremic patients. This study and the limited available data in the literature indicate that renal transplant provides an important therapeutic option for PH in this patient population.
Abasi et al. reported data from 5 patients with PH who underwent successful transplantation [4]. They detected a significant decrease in pulmonary artery pressure following renal transplant. The mean value of pre-transplant systolic pulmonary artery pressure was 47 ± 11 mm Hg which decreased to 32 ± 8 mm Hg after restoration of renal function with transplant. In accordance with these findings, we detected a significant decline in mean systolic pulmonary artery pressure following renal transplant. To the best of our knowledge, our study is the largest study to date on this topic.
Considering the common prevalence of cardiovascular diseases including PH, we suggest that all patients with ESRD being evaluated for renal transplant candidacy undergo a Doppler echocardiographic examination. In case of markedly elevated SPAP (> 50 mm Hg), right heart catheterization may be considered and pulmonary vascular resistance calculated. The decision for transplant may be reached in this way.
Limitations
This study has several limitations. Owing to its retrospective nature some tests were not able to be performed. Owing to the lack of indication and the invasive nature of the procedure, right heart catheterization was not performed to assess the severity and etiology of PH. If this had been undertaken, additional valuable data would have been obtained.
Conclusions
The development of cardiovascular disorders accelerates as the duration of dialysis increases. As documented by previous research, this is also the case in the development of PH. That is, the longer the time on dialysis the higher the prevalence of PH and other forms of cardiovascular diseases.
Therefore, we retain that renal transplant should be considered as soon as the patient requires dialysis therapy. As a result of its high prevalence and prognostic importance, increased attention should be paid to PH in patients with renal failure. This study provides important insight regarding the possibility that this problem might be ameliorated - at least to a degree - with a functioning kidney graft. Further research is needed to provide us with more concrete conclusions regarding this subject.
Conflict of interest statement
None of the authors has any conflict of interest to declare in relation to the subject matter of this manuscript.
References
Yigla M, Nakhoul F, Sabag A, Tov N, Gorevich B, Abassi Z, Reisner SA: Pulmonary hypertension in patients with end-stage renal disease. Chest. 2003, 123: 1577-1582. 10.1378/chest.123.5.1577.
Tarrass F, Benjelloun M, Medkouri G, Hachim K, Benghanem MG, Ramdani B: Doppler echocardiograph evaluation of pulmonary hypertension in patients undergoing hemodialysis. Hemodial Int. 2006, 10: 356-359. 10.1111/j.1542-4758.2006.00129.x.
Havlucu Y, Kursat S, Ekmekci C, Celik P, Serter S, Bayturan O, Dinc G: Pulmonary hypertension in patients with chronic renal failure. Respiration. 2007, 74: 503-510. 10.1159/000102953.
Abassi Z, Nakhoul F, Khankin E, Reisner SA, Yigla M: Pulmonary hypertension in chronic dialysis patients with arteriovenous fistula: pathogenesis and therapeutic prospective. Curr Opin Nephrol Hypertens. 2006, 15: 353-360. 10.1097/01.mnh.0000232874.27846.37.
Bozbas SS, Akcay S, Altin C, Bozbas H, Karacaglar E, Kanyilmaz S, Sayin B, Muderrisoglu H, Haberal M: Pulmonary hypertension in patients with end-stage renal disease undergoing renal transplantation. Transplant Proc. 2009, 41: 2753-2756. 10.1016/j.transproceed.2009.07.049.
Ifudu O: Care of patients undergoing hemodialysis. N Engl J Med. 1998, 339: 1054-1062. 10.1056/NEJM199810083391507.
Yigla M, Abassi Z, Reisner SA, Nakhoul F: Pulmonary hypertension in hemodialysis patients: an unrecognized threat. Semin Dial. 2006, 19: 353-357. 10.1111/j.1525-139X.2006.00186.x.
Yigla M, Fruchter O, Aharonson D, Yanay N, Reisner SA, Lewin M, Nakhoul F: Pulmonary hypertension is an independent predictor of mortality in hemodialysis patients. Kidney Int. 2009, 75: 969-975. 10.1038/ki.2009.10.
Kim WR, Krowka MJ, Plevak DJ, Lee J, Rettke SR, Frantz RP, Wiesner RH: Accuracy of Doppler echocardiography in the assessment of pulmonary hypertension in liver transplant candidates. Liver Transpl. 2000, 6: 453-458. 10.1053/jlts.2000.7573.
Marangoni S, Quadri A, Dotti A, Scalvini S, Volterrani M, Schena M, Foglio K, Errera D, Levi G: Noninvasive assessment of pulmonary hypertension: a simultaneous echo-Doppler hemodynamic study. Cardiology. 1988, 75: 401-408. 10.1159/000174410.
Berger M, Haimowitz A, Van Tosh A, Berdoff RL, Goldberg E: Quantitative assessment of pulmonary hypertension in patients with tricuspid regurgitation using continuous wave Doppler ultrasound. J Am Coll Cardiol. 1985, 6: 359-365. 10.1016/S0735-1097(85)80172-8.
Barst RJ, McGoon M, Torbicki A, Sitbon O, Krowka MJ, Olschewski H, Gaine S: Diagnosis and differential assessment of pulmonary arterial hypertension. J Am Coll Cardiol. 2004, 43 (12 Suppl S): 40S-47S.
Issa N, Krowka MJ, Griffin MD, Hickson LJ, Stegall MD, Cosio FG: Pulmonary hypertension is associated with reduced patient survival after kidney transplantation. Transplantation. 2008, 86: 1384-1388. 10.1097/TP.0b013e318188d640.
Abdelwhab S, Elshinnawy S: Pulmonary hypertension in chronic renal failure patients. Am J Nephrol. 2008, 28: 990-997. 10.1159/000146076.
Nakhoul F, Yigla M, Gilman R, Reisner SA, Abassi Z: The pathogenesis of pulmonary hypertension in haemodialysis patients via arterio-venous access. Nephrol Dial Transplant. 2005, 20: 1686-1692. 10.1093/ndt/gfh840.
Kumbar L, Fein PA, Rafiq MA, Borawski C, Chattopadhyay J, Avram MM: Pulmonary hypertension in peritoneal dialysis patients. Adv Perit Dial. 2007, 23: 127-131.
Amin M, Fawzy A, Hamid MA, Elhendy A: Pulmonary hypertension in patients with chronic renal failure: role of parathyroid hormone and pulmonary artery calcifications. Chest. 2003, 124: 2093-2097. 10.1378/chest.124.6.2093.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Bozbas, S.S., Kanyilmaz, S., Akcay, S. et al. Renal transplant improves pulmonary hypertension in patients with end stage renal disease. Multidiscip Respir Med 6, 155 (2011). https://doi.org/10.1186/2049-6958-6-3-155
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/2049-6958-6-3-155