Abstract
Background
Evaluation of the effect of additional surgical margin parameters on biochemical recurrence (BCR) in patients with positive surgical margins (PSM) after radical prostatectomy (RP).
Methods
Clinicopathological and outcome data from 91 patients with PSM who underwent RP were retrospectively analyzed. Additional surgical margin parameters (PSM length, highest Gleason grade (GG), localization of PSM (apex, bladder neck, or posterolateral), and unifocality or multifocality) were examined and their effects on BCR were investigated.
Results
Fifty patients with PSM were included in the study. The mean age of the patients was 63.6 ± 6.9 years. The laparoscopic approach was undertaken more frequently, used for 36 (72%) patients compared to open RP performed in 14 cases (28%). The median follow-up time was 57.0 months (24.0–125.0 months). BCR developed in 14 (28%) patients during the follow-up period. Although mean BCR-free survival was shorter in cases with PSM length ≥ 3 mm compared to those with PSM length < 3 mm (90.4 vs. 108.2 months), multifocality compared to those with unifocality (62 vs. 97.4 months) and surgical margin GG ≥ 4 compared to those with GG 3 (87.4 vs. 97.5 months), the differences were not statistically significant (p = 0.251, p = 0.509 and p = 0.317, respectively). In addition, none of the PSM localizations affected BCR-free survival (p = 0.619). In univariate Cox regression analysis, PSM length affected BCR at a level close to statistical significance (HR = 1.16; p = 0.052). In multiple Cox regression analysis, main tumor Gleason score was determined to be a risk factor associated with BCR (HR = 4.75; p = 0.041).
Conclusions
Although BCR-free survival was shortened in the presence of poor prognostic features (multifocal PSM, PSM length ≥ 3 mm, surgical margin GG ≥ 4) at the surgical margin, none of these parameters affected BCR at a statistically significant level. Gleason score of the main tumor was found to be a better prognostic factor for BCR.
Similar content being viewed by others
1 Background
Radical prostatectomy (RP) is the gold standard treatment for localized prostate cancer [1]. After RP, biochemical recurrence (BCR) develops in 16–31% of patients within 5 years, and in 25–53% of patients within 10 years [2,3,4]. BCR occurs before clinical and metastatic progression. Studies reported that BCR is associated with preoperative PSA level, postoperative Gleason score (GS), pathological tumor stage, and positive surgical margins (PSM) [5, 6].
The presence of PSM has been reported in 11–38% of patients undergoing RP [7]. PSM is associated with clinical progression and was linked with poor cancer-specific survival [8]. Boorjian et al. reported that although the presence of PSM increases the risk of BCR and local recurrence, it does not affect cancer-specific survival and overall mortality with appropriate salvage treatment [9]. Therefore, it is important to identify those at high risk of early BCR among patients with PSM. Since patients with PSM are a heterogeneous group and not all of them develop BCR during follow-up, it is necessary to divide them into subgroups according to surgical margin (SM) characteristics and investigate their relationship with oncological outcomes. The relationship between additional SM parameters and oncological outcomes has not been adequately investigated, and it is controversial as to whether adjuvant treatment is necessary in PSM patients [10]. It was reported that GS in PSM is associated with BCR, but the relationships between PSM length, localization, and multifocality status and BCR have not been fully elucidated [11,12,13,14,15]. Therefore, we aimed to evaluate the factors associated with BCR in PSM patients and the effect of additional SM parameters (unifocal/multifocal PSM, SM length, and highest Gleason Grade (GG) at PSM) on BCR.
2 Methods
Data from 421 patients who underwent RP were examined retrospectively. Ninety-one patients with PSM (pT2, pT3, Nx, N0, N1) were identified. Exclusion criteria and numbers of excluded patients are schematized in Fig. 1.
The minimum postoperative follow-up period was two years. The clinical data examined for patients included age, preoperative prostate-specific antigen (PSA) level, surgery method (open or laparoscopic), postoperative follow-up time, and BCR. The pathological data examined are as follows: pathological tumor stage after RP, tumor volume, presence of perineural invasion (PNI), lymph node involvement (LNI), and additional SM parameters (PSM localization, number, length, and highest GG). Within the scope of this study, the pathological specimens from patients were re-examined by a uropathologist, and additional SM parameters not specified in previous pathology reports were recorded. All operations were performed using the open or transperitoneal laparoscopic method by three surgeons experienced in the field of uro-oncology. Extended lymph node dissection was performed in patients with preoperative indications.
3 Study outcome
The primary endpoint of the study was determined as the effect of additional SM parameters on BCR, and the secondary endpoint was determined as the factors affecting BCR. BCR was defined as PSA measurement ≥ 0.2 ng/ml in two consecutive measurements during the postoperative follow-up.
4 Follow-up
Patients were called for follow-up every 3 months in the first 2 years, every 6 months in the next 3 years, and annually thereafter. When relapse was considered in patients evaluated with PSA measurement, conventional imaging methods (such as bone scintigraphy, computed tomography, and magnetic resonance imaging) were used until 5 years before the study, while evaluation was performed with prostate specific membrane antigen positron emission tomography in the last 5 years.
5 Ethics approval
The study was conducted in compliance with the principles of the Declaration of Helsinki and additional approval was obtained from the local ethics committee (number of meeting: 125; number of decision: 82).
6 Pathological examination
Hematoxylin–eosin–stained preparations of the RP materials from the cases were accessed from the pathology archive of our hospital. GGs were reviewed by a single uropathologist according to the latest World Health Organization classification. In patients with PSM, SM length, highest GG, localization of PSM (apex, bladder neck, posterolateral), and unifocality/multifocality were examined. The steps of the pathological examination can be summarized as follows; at the end of RP, the prostate tissues were fixed in 10% formalin solution for 24–48 h without losing their integrity, and after fixation, the right half was identified with green tissue dye while the left half used black tissue dye. After the prostate tissues, ductus deferens SMs, and seminal vesicles were sampled, all areas from the apex to the base were mapped, the blocks were prepared, and subjected to routine follow-up. In the routine follow-up, prostate tissues were soaked in alcohol, xylol, and paraffin solutions, embedded in paraffin, and then the tissues were cut into 4-micron thin sections and stained with routine hematoxylin–eosin stain. The preparations were evaluated by light microscopy (using an Olympus microscope).
7 Statistical analysis
Categorical variables are expressed as numbers and percentages, whereas continuous variables are summarized as mean and standard deviation and as median and minimum–maximum, where appropriate. The chi-square test was used to compare categorical variables between the groups. For comparison of continuous variables between the two groups, the Student’s t-test or Mann–Whitney U test was used depending on whether the statistical hypotheses were fulfilled. BCR-free survival was calculated by the Kaplan–Meier method and the log rank test was performed. Cox proportional hazard regression analysis was performed to determine significant predictors of BCR. In univariate analysis, variables significant at the p < 0.25 level were entered into multiple Cox regression analysis (backward procedure, Wald method). All analyses were performed using the IBM SPSS Statistics version 20.0 statistical software package. The statistical significance level for all tests was set at p < 0.05.
8 Results
Fifty patients with PSM were included in the study. The mean age of the patients was 63.6 ± 6.9 years. The laparoscopic approach was undertaken more frequently in 36 (72%) patients than open RP performed in 14 cases (28%). Altogether, 31 (62%) patients had localized disease. In this study, 9 (18%) of the patients had PNI and 7 (14%) had LNI. RP GS was ≥ 8 in 5 (10%) patients. The median follow-up time was 57.0 months (24.0–125.0 months). BCR developed in 14 (28%) patients during the follow-up period.
Although the incidence of PSM length ≥ 3 mm, multifocal tumor and surgical margin GG ≥ 4 was high in BCR patients, the results were not statistically significant (p = 0.295, p = 0.670 and p = 0.511, respectively). The tumor was located posterolaterally in 26 (52%) of the patients. There was no difference between the groups in terms of PSM localizations (p = 0.619). Comparison of the demographic, clinical, and PSM characteristics according to the BCR groups is presented in Table 1.
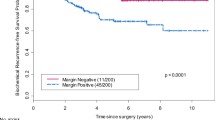
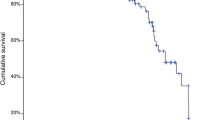
Although mean BCR-free survival was shorter in cases with SM length ≥ 3 mm compared to those with SM length < 3 mm (90.4 vs. 108.2 months), multifocality compared to those with unifocality (62 vs. 97.4 months) and surgical margin GG ≥ 4 compared to those with GG 3 (87.4 vs. 97.5 months), the differences were not statistically significant (Fig. 2; p = 0.251, Fig. 3; p = 0.509 and Fig. 4; p = 0.317, respectively) (Table 2). In addition, none of the PSM localizations affected BCR-free survival (Fig. 5; p = 0.619) (Table 2).
In univariate Cox regression analysis, PSM length affected BCR at a level close to statistical significance (HR = 1.16, 95%CI = 0.99–1.35; p = 0.052). Other additional surgical margin parameters did not affect BCR. Tumor volume had a statistically significant effect on BCR in univariate Cox regression analysis (HR = 1.05, 95% CI = 1.01–1.09; p = 0.008), but this effect was not significant in multiple Cox regression analysis. In multiple Cox regression analysis, RP GS was determined to be the only significant risk factor associated with BCR (HR = 4.75, 95% CI = 1.026–21.3; p = 0.041) (Table 3).
9 Discussion
Various pathological variables, such as the location and extent of PSM, were suggested to be possible prognostic factors in patients with PSM, and routine evaluation of these factors in RP specimens was recommended at the recent International Society of Urological Pathology consensus meeting [16]. By including only PSM patients, we aimed to identify factors that could predict BCR. However, in this study, statistical analysis showed that these parameters did not significantly affect BCR. We found that GS in the main tumor was a prognostic factor for BCR.
Studies showed that GS of the main tumor does not have a significant effect on BCR in PSM patients [17, 18]. Furthermore, RP GS ≥ 8 was found to be significantly associated with BCR in other studies [11, 19]. Due to these uncertainties about the effect of GS in the main tumor on BCR in PSM patients, studies predicted that GS in PSM may be a better predictive factor [16, 20]. Cao et al. found that GS in both PSM and the main tumor were predictive of BCR [21]. In their study with 112 PSM patients, Kurose et al. found that GS of the main tumor was not predictive, and GS in PSM was a predictive factor for BCR [12]. In this study, main tumor GS was found to be predictive of BCR.
Bladder neck SM consists of bladder muscle bundles. PSM with this localization is usually associated with extraprostatic spread of the tumor from the base of the prostate [22]. Since the posterolateral part of the prostate is close to the neurovascular bundle, PSM can be seen during nerve-sparing surgery [22]. Apical PSM is one of the most common localizations [22,23,24]. Eastham et al. reported that BCR is greatly affected by the specific location of PSM, and that the posterolateral region is at highest risk for relapse [25]. Contrary to this, Aydın et al. reported an increased risk of BCR in cases with bladder neck PSM [26]. Few studies have reported that PSM localization does not affect BCR [22,23,24, 27]. In this study, none of the PSM localizations were found to be associated with BCR.
Obek et al. reported that the recurrence rate was 43% in patients with multifocal PSM and 24% in patients with unifocal PSM with a mean follow-up of 25 months [28]. They also stated that patients with two or more PSMs were 2.5 times more likely to relapse in a short time [28]. Sofer et al. reported that BCR was higher in those with multifocal PSM [27]. In this study, the presence of multifocal tumor in PSM was not associated with BCR.
In some studies, PSM length of ≥ 3 mm was found to be a predictive factor for BCR [29, 30]. In this study, PSM length did not affect BCR at a statistically significant level.
Although PSM was found to be associated with an increased risk of BCR, its clinical impact on overall survival and cancer-specific survival remains controversial [31]. Specific subgroups have a higher risk for metastasis and prostate cancer-related mortality (especially those with stage T3b, surgical margin GG 4/5 and those who develop BCR in the first 3 years) [32].
The limitations of the present study are that it was retrospective, single-center, had a short follow-up period, and included a small number of patients.
10 Conclusion
Although BCR-free survival was shortened in the presence of poor prognostic features (multifocal PSM, PSM length ≥ 3 mm, surgical margin GG ≥ 4) at the surgical margin, none of these parameters affected BCR at a statistically significant level. Gleason score in the main tumor was found to be more prognostic factor for BCR. To further investigate the relationship between additional SM parameters and BCR, multicenter studies with more patients and long follow-up periods are recommended.
Availability of data and material
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BCR:
-
Biochemical recurrence
- GG:
-
Gleason grade
- GS:
-
Gleason score
- LNI:
-
Lymph node involvement
- PNI:
-
Perineural invasion
- PSA:
-
Prostate specific antigen
- PSM:
-
Positive surgical margins
- RP:
-
Radical prostatectomy
- SM:
-
Surgical margin
References
Van Poppel H, Everaerts W, Tosco L, Joniau S (2019) Open and robotic radical prostatectomy. Asian J Urol 6:125–128
Lowrance WT, Eastham JA, Savage C, Maschino AC, Laudone VP, Dechet CB et al (2012) Contemporary open and robotic radical prostatec tomy practice patterns among urologists in the United States. J Urol 187:2087–2092
Hull GW, Rabbani F, Abbas F, Wheeler TM, Kattan MW, Scardino PT (2002) Cancer control with radical prostatectomy alone in 1000 consecutive patients. J Urol 167:528–534
Stephenson AJ, Kattan MW, Eastham JA, Dotan ZA, Bianco FJ Jr, Lilja H et al (2006) Defining biochemical recurrence of prostate cancer after radical prostatectomy: a proposal for a standardized definition. J Clin Oncol 24:3973–3978
Novara G, Ficarra V, Mocellin S, Ahlering TE, Carroll PR, Graefen M et al (2012) Systematic review and meta-analysis of studies reporting oncologic outcome after robot-assisted radical prostatectomy. Eur Urol 62:382–404
Liesenfeld L, Kron M, Gschwend JE, Herkommer K (2017) Prognostic factors for biochemical recurrence more than 10 years after radical prostatectomy. J Urol 197:143–148
De La Roca RL, Da Cunha IW, Bezerra SM, Da Fonseca FP (2014) Radical prostatectomy and positive surgical margins: relationship with prostate cancer outcome. Int Braz J Urol 40:306–315
Chalfin HJ, Dinizo M, Trock BJ, Feng Z, Partin AW, Walsh PC et al (2012) Impact of surgical margin status on prostate-cancer-specific mortality. BJU Int 110:1684–1689
Boorjian SA, Karnes RJ, Crispen PL, Carlson RE, Rangel LJ, Bergstralh EJ et al (2010) The impact of positive surgical margins on mortality following radical prostatectomy during the prostate specific antigen era. J Urol 183:1003–1009
Ghabili K, Park HS, Yu JB, Sprenkle PC, Kim SP, Nguyen KA et al (2021) National trends in the management of patients with positive surgical margins at radical prostatectomy. World J Urol 39(4):1141–1151
Morizane S, Yumioka T, Makishima K, Tsounapi P, Iwamoto H, Hikita K et al (2021) Impact of positive surgical margin status in predicting early biochemical recurrence after robot-assisted radical prostatectomy. Int J Clin Oncol 26:1961–1967
Kurose H, Ueda K, Ogasawara N, Chikui K, Nakiri M, Nishihara K et al (2022) Impact of Gleason score of the tumor at the positive surgical margin as a prognostic factor. Mol Clin Oncol 16:82
Pettenati C, Neuzillet Y, Radulescu C, Hervé JM, Molinié V, Lebret T (2015) Positive surgical margins after radical prostatectomy: what should we care about? World J Urol 33:1973–1978
Bianchi L, Schiavina R, Borghesi M, Casablanca C, Chessa F, Mineo Bianchi F et al (2020) Patterns of positive surgical margins after open radical prostatectomy and their association with clinical recurrence. Minerva Urol Nefrol 72:464–473
Dev HS, Wiklund P, Patel V, Parashar D, Palmer K, Nyberg T et al (2015) Surgical margin length and location affect recurrence rates after robotic prostatectomy. Urol Oncol 33(109):e7-13
Savdie R, Horvath LG, Benito RP, Rasiah KK, Haynes AM, Chatfield M et al (2012) High Gleason grade carcinoma at a positive surgical margin predicts biochemical failure after radical prostatectomy and may guide adjuvant radiotherapy. BJU Int 109:1794–1800
Servoll E, Vlatkovic L, Sæter T, Nesland JM, Axcrona U, Waaler G et al (2014) The length of a positive surgical margin is of prognostic significance in patients with clinically localized prostate cancer treated with radical prostatectomy. Urol Int 93:289–295
Koparal MY, Acar C, Ögüt B, Tokat E, Biçaklioglu F, Gönül II et al (2017) Do length and tumor grades of positive surgical margin have an impact on biochemical recurrence after prostatectomy? Bull Urooncology 16:86–92
Preisser F, Heinze A, Abrams-Pompe RS, Budäus L, Chun FK, Graefen M et al (2022) Impact of positive surgical margin length and Gleason grade at the margin on oncologic outcomes in patients with nonorgan-confined prostate cancer. Prostate 82:949–56
Lysenko I, Mori K, Mostafaei H, Enikeev DV, Karakiewicz PI, Briganti A et al (2020) Prognostic value of Gleason score at positive surgical margin in prostate cancer: a systematic review and meta-analysis. Clin Genitourin Cancer 18:517–522
Cao D, Kibel AS, Gao F, Tao Y, Humphrey PA (2010) The Gleason score of tumor at the margin in radical prostatectomy is predictive of biochemical recurrence. Am J Surg Pathol 34(7):994–1001
Çelik S, Aslan G, Sözen S, Özen H, Akdoğan B, Baltaci S et al (2020) Factors Affecting Surgical Margin Positivity after Radical Prostatectomy in the Turkish Population: A Multicenter Study of the Urooncology Association. Urol Int 104:724–730
Udo K, Cronin AM, Carlino LJ, Savage CJ, Maschino AC, Al-Ahmadie HA et al (2013) Prognostic impact of subclassification of radical prostatectomy positive margins by linear extent and Gleason grade. J Urol 189:1302–1307
Chapin BF, Nguyen JN, Achim MF, Navai N, Williams SB, Prokhorova IN et al (2018) Positive margin length and highest Gleason grade of tumor at the margin predict for biochemical recurrence after radical prostatectomy in patients with organ-confined prostate cancer. Prostate Cancer Prostatic Dis 21:221–227
Eastham JA, Kuroiwa K, Ohori M, Serio AM, Gorbonos A, Maru N et al (2007) Prognostic significance of location of positive margins in radical prostatectomy specimens. Urology 70:965–969
Aydin H, Tsuzuki T, Hernandez D, Walsh PC, Partin AW, Epstein JI (2004) Positive proximal (bladder neck) margin at radical prostatectomy confers greater risk of biochemical progression. Urology 64:551–555
Sofer M, Hamilton-Nelson KL, Civantos F, Soloway MS (2002) Positive surgical margins after radical retropubic prostatectomy: the influence of site and number on progression. J Urol 167:2453–2456
Obek C, Sadek S, Lai S, Civantos F, Rubinowicz D, Soloway MS (1999) Positive surgical margins with radical retropubic prostatectomy: anatomic site-specific pathologic analysis and impact on prognosis. Urology 54:682–688
Preisser F, Coxilha G, Heinze A, Oh S, Chun FK, Sauter G et al (2019) Impact of positive surgical margin length and Gleason grade at the margin on biochemical recurrence in patients with organ-confined prostate cancer. Prostate 79:1832–1836
Koskas Y, Lannes F, Branger N, Giusiano S, Guibert N, Pignot G et al (2019) Extent of positive surgical margins following radical prostatectomy: impact on biochemical recurrence with long-term follow-up. BMC Urol 19:37
Zhang L, Wu B, Zha Z, Zhao H, Yuan J, Jiang Y et al (2018) Surgical margin status and its impact on prostate cancer prognosis after radical prostatectomy: a meta-analysis. World J Urol 36:1803–1815
John A, John H, Catterwell R, Selth LA, Callaghan MO (2021) Primary Gleason grade and Gleason grade group at positive surgical margins: a systematic review and meta-analysis. BJU Int 127:13–22
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
MA, NA, MD did the conceptualization, methodology of the research, supervised the research and manuscript writing, and validated results of the research. IOY, TT performed the data collection, investigation, and completion of the original draft. SE, VI, YB helped in methodological input, supervised the research, and also reviewed and edited the overall draft. SPYK performed the data collection, methodological, and statistical analysis of the research. Ensuring issues concerning the accuracy or integrity of the study have been examined and resolved by all contributors who agreed to be held accountable for the study.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in compliance with the principles of the Declaration of Helsinki and additional approval was obtained from the Ethics Committee of Cukurova University, Medical Faculty, Adana, Turkiye (number of meetings: 125; number of decisions: 82).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Aydamirov, M., Deger, M., Akdogan, N. et al. The effect of surgical margin features on oncologic outcomes after radical prostatectomy. Afr J Urol 30, 41 (2024). https://doi.org/10.1186/s12301-024-00445-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12301-024-00445-y