Abstract
Introduction
Telemedicine encompasses all medical practices that allow patients to be remotely cared for through new information and communication technologies. This study aims to assess the remote management of patients consulting emergency services and not requiring in-hospital care during both pre-pandemic and pandemic periods of COVID-19.
Methods
This was a prospective, randomized, controlled study. The telemedicine group received follow-up at home after emergency room discharge according to a predefined protocol, with telephone calls on days 2, 7, 15, and 30. The control group received standard care without regular telephone follow-up (only a call on day 30). The study was conducted with patients consulting the emergency department of FarhatHached Hospital in Sousse. Patient inclusion occurred between November 1, 2019, and April 30, 2020. The primary outcome measures were the re-consultation rate and treatment adherence. The secondary outcome measure was patient satisfaction.SPSS version 23.0 for Windows was used for data analysis. Descriptive statistics calculated frequencies, percentages, means, standard deviations, medians, and range. Analytical study involved Student’s t-test and Pearson chi-square test for mean and frequency comparisons, respectively. Significance threshold (p) for all tests was set at 0.05.
Results
A total of 400 patients were included. The average age of patients was 40 years. Both groups were comparable in terms of demographics and clinical characteristics. Diagnoses included mainly benign infectious diseases, trauma, mild decompensations of chronic conditions (asthma, COPD, heart failure), and suspected COVID cases. Patients in the telemedicine group tended to reconsult less in the month following their initial emergency room visit (14% versus 26.5%) (p = 0.004). There was a significant difference in treatment adherence between the telemedicine group and the control group (97.5% versus 92%; p = 0.014). The satisfaction with telemedicine was higher than satisfaction with regard to an in-person consultation at the emergency department (90% versus 37.5%).
Conclusion
It is necessary to implement telemedicine in Tunisia, especially in emergency services. It ensures better remote patient care by reducing re-consultation rates, increasing treatment adherence, and improving patient satisfaction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Telemedicine is a remote medical practice that leverages new information and communication technologies to connect either the patient and one or more healthcare professionals or multiple healthcare professionals. According to the definition adopted by the World Health Organization (WHO) in 1997, “Telemedicine is the part of medicine that uses telecommunication transmission of medical information (images, reports, recordings, etc.) to obtain a diagnosis, specialized advice, continuous monitoring of a patient, or therapeutic decision remotely” [1].Its use is considered as an organizational response to various challenges: an epidemiological challenge related to the aging population and the increase in the number of patients suffering from chronic diseases, a demographic challenge with an uneven distribution of healthcare professionals across the territory, and an economic challenge with increasingly significant budget constraints.Telemedicine can also be a response to the challenges faced by healthcare services, particularly in emergency departments. Worldwide, during the lockdown, telemedicine ensured the continuity of care for patients with chronic diseases and facilitated the triage and monitoring of those with COVID-19 while adhering to safety and confidentiality rules [2, 3].Telemedicine offers the opportunity to provide timely medical assessments and care remotely, potentially reducing unnecessary emergency room visits and hospital admissions. This approach can improve healthcare accessibility, optimize emergency department resources, and enhance patient satisfaction by ensuring appropriate and efficient care delivery without the need for inpatient services. Like other countries, Tunisia adopted social distancing strategies to break the transmission chain. The health crisis became the starting point for the rapid development of telemedicine in Tunisia, benefitting from temporary easing of regulations governing its practice and facilitating its deployment during this crisis. While telemedicine has demonstrated significant benefits, particularly in improving healthcare access and efficiency, its implementation is not without challenges. Technological barriers, such as unreliable internet connectivity or limited digital literacy among certain patient demographics, can hinder widespread adoption. Additionally, concerns about data privacy and security remain pertinent, especially with the transmission of sensitive medical information over digital platforms. Emergency care often requires rapid diagnosis, intervention, and management to prevent further complications and ensure optimal outcomes for patients in critical situations. The aim of our study was to evaluate the impact of telemedicine in managing patients not requiring in-hospital care, in terms of re-consultations and treatment adherence and to assess patient satisfaction with telemedicine.
Materials and methods
Study design
It was a prospective, randomized, controlled interventional study and conducted at Farhat Hached Hospital, Sousse, from November 1, 2019, to April 30, 2020.
Participants
Patients aged 15 and above, seeking care at the emergency department, not requiring immediate hospitalization, and providing oral consent for phone number use were included. Patients who do not respond to any of the four calls for the telemedicine group and the call on day 30 for the control group, as well as patients presenting with life-threatening or potentially life-threatening conditions were excluded from the study.Only patients with a good socioeconomic status and residing in Sousse were included in the study.
Randomization
Patients consulting on odd days were assigned to the control group, and those consulting on even days were allocated to the telemedicine group. We adopted the method of even and odd days so that patients in both groups consult on different days of the week. And to eliminate bias where one group consults more on weekends.
Intervention
The telemedicine Group received home follow-up with telephone calls on days 2, 7, 15, and 30. Interventions taken for patients in the telemedicine group included stopping or changing treatment, adjusting dosage, or referring to a specialist. While the Control Group received standard care with only a call on day 30.
Sample size
Number of subjects required is calculated by BiostatTGV using a superiority difference of 5.5%, alpha risk of 5%, beta of 80%. This gives a number of subjects required in each group of 189.
Data collection and measuring instrument
The questionnaire used was developed for this study. Data, including demographic details, reason for consultation, clinical findings, diagnoses, and discharge treatment, were collected upon admission. The study had five stages: inclusion, randomization, and scheduled phone calls on days 2, 7, 15, and 30.The phone calls were conducted exclusively by a physician specially trained for this purpose. Each call lasted between 5 and 10 min and followed a structured grid capturing the diagnosed condition, symptom progression, need for follow-up consultations, treatment adherence, and referrals to specialists as necessary. Patient satisfaction was evaluated at day 30 in both study groups. For the telephone call, we used the hospital’s telephone, which is a secure method since we don’t yet have telemedicine platforms in our hospital.
Outcome criteria
Primary outcomes included re-consultation rate and treatment adherence. Secondary outcomes consisted of patient satisfaction levels.
Variable definition
Reconsultation: any patient consulting for the same reason during these 30 days of follow-up.Reconsultation was spontaneous or the investigator recommended reconsultation or referral to a specialist during telemedicine.
Adherence to treatment: is defined by the patient’s compliance with the dosage and duration of treatment prescribed in the prescription. Any jump, even in one take, the patient is considered non-compliant.
Statistical analysis
Data were entered and analyzed using SPSS version 23.0. Frequencies and percentages were calculated for qualitative variables, and means, standard deviations, medians, and range of extreme values were calculated for quantitative variables. Student’s t-test was used to compare the means of two independent series. Pearson’s chi-squared test was used to compare frequencies. Pearson’s correlation coefficient was used to examine the relationship between two quantitative variables. For all statistical tests, the P-significance level was set at 0.05.
Ethical considerations
This study was conducted in accordance with the ethical principles of the Declaration of Helsinki and was approved by the Ethical Committee of Faculty of medicine of Sousse (Reference: CEFMS 228/2024). Participation in the study was voluntary, and written informed consent was obtained from each participant after clarification of the study objectives. To ensure anonymity and confidentiality, full names were not collected.
Results
Patient demographic and baseline characteristics
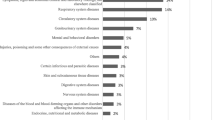
Out of 468 questionnaires collected over six months, 400 patients meeting the criteria were randomly included.A total of 68 questionnaires were excluded due to missing data.The average age of patients was 40 years. Both groups were comparable in terms of demographics and clinical characteristics. The distribution of patients according to gender in both groups was comparable, with a sex ratio of 1.02 (101 M/99F) in the telemedicine group and 0.96 (98 M/102F) in the control group. In our study, hypertension was the most frequent medical history in both groups.The reasons for consultation were mainly fever, abdominal pain, and dyspnea. In our research, we segmented our study population into four distinct subsets to assess the influence of telemedicine (Table 1). Among these subsets, the infectious diseases service exhibited the highest participation, encompassing 76 patients in the telemedicine group and 71 patients in the control group. Notably, the telemedicine group showed a gastroenteritis rate of 13.2%, whereas the control group had a rate of 7%. Pneumonia diagnoses were reported in 17.1% of telemedicine patients and 16.9% of control group patients. Examining respiratory infections, tracheobronchitis was identified in 34.2% of telemedicine patients and 43.7% of control group patients. Trauma cases comprised 12 patients in the telemedicine group and 20 patients in the control group. Additionally, instances of mild decompensations in chronic conditions, such as asthma crises, heart failure and Chronic Obstructive Pulmonary Disease (COPD), involved 30 patients in the telemedicine group and 28 patients in the control group. Furthermore, a subgroup focusing on suspected COVID cases, where PCR tests were conducted and individuals were contacted the day after receiving negative results to incorporate them into the protocol, included 50 patients in both the telemedicine and control groups (Table 1).
Outcomes
Patients in the telemedicine group tend to have fewer reconsultations within the month following their initial emergency consultation. The total rate of patients reconsulting within one month in the telemedicine group is 14%, with 28 patients, while 26.5%, with 53 patients in the control group with a significant difference (p = 0.004). This effect is particularly noticeable in the first week.No readmission for worsening symptoms was reported in both groups.
There was a significant difference in treatment adherence between the telemedicine group and the control group, with rates of 97.5% and 92%, respectively (p = 0.014) (Table 2).
The satisfaction with telemedicinewas higher thansatisfaction with regard to an in-person consultation at the emergency department (90% versus 37.5%)(p < 0.05) (Fig. 1).
Discussion
According to our study, there was a significant decrease in re-consultation rates within one month following their initial emergency room visits compared to those in the control group (14% vs. 26.5%, p = 0.004). This reduction was particularly pronounced during the first week post-consultation, highlighting the immediate impact of telemedicine interventions on reducing healthcare utilization and improving patient outcomes. Our findings corroborate existing research demonstrating the effectiveness of telemedicine across various medical specialties. Specifically, teleconsultations have consistently shown to reduce unnecessary in-person specialist appointments.For instance, Eldon Taylor and al. [4] evaluated a telepsychiatric consultation model, reporting statistically significant reductions in admissions and average length of stay post-implementation. Dermatology consultations reported reductions ranging from 38 to 88%, ophthalmology from 16 to 48%, and ENT (Otolaryngology) up to 89% [5].
Moreover, telemedicine interventions such as SMS reminders and telemonitoring have significantly enhanced medication adherence across diverse medical conditions. Patients with sleep apnea, psychiatric disorders, and cardiovascular diseases demonstrated improved adherence rates, which correlated with better clinical outcomes and reduced healthcare costs [6, 7].
Patient satisfaction with telemedicine consultations remained consistently high in our study, reflecting positive feedback on convenience, communication quality, and overall experience comparable to traditional in-person visits, similar to results reported by Agha and al., [8]. This satisfaction is particularly relevant in the context of the COVID-19 pandemic, where telemedicine played a pivotal role in ensuring continuity of care while minimizing infection risks. This was also confirmed by Gomes [9] in her study using the same Likert scale of satisfaction as our study conducted among 253 individuals, out of which 70.6% preferred contact via email or phone.
Our findings also underscore the broader implications of telemedicine in chronic disease management, including conditions such as asthma, COPD, and heart failure. Telemedicine interventions, such as structured remote monitoring and virtual consultations, have proven effective in improving disease control, reducing hospital admissions, and enhancing the quality of life for patients .A recent systematic review published in the Cochrane Library by BarisGencer et al. concluded that telemedicine in the form of structured telephone support and non-invasive telemonitoring helps reduce overall mortality and heart failure-related hospitalizations in patients with chronic heart failure. These interventions have a favorable impact on quality of life, disease understanding, and self-management [10]. Koehler showed that home-based telemonitoring of heart failure patients significantly reduces all-cause mortality and the number of days per year spent in the hospital due to unscheduled cardiology admissions, compared to their usual care [11].
The integration of telemedicine into routine clinical practice is further supported by its cost-effectiveness and scalability. Our study indicates significant presumable cost savings through reduced healthcare utilization, including fewer unnecessary visits, hospitalizations, and emergency room admissions.
According to a literature review by Kruse and al, low cost was an encouraging factor for telemedicine in 8% of patients [12]. Through the COMET study, it was found that telemedicine did reduce hospitalization days, deaths, and healthcare costs [13].
Despite its benefits, telemedicine poses challenges, including legal and regulatory considerations. Hajsalemand al. [14] discussed the evolving legal landscape of telemedicine in Tunisia, highlighting the importance of addressing potential medical-legal issues associated with remote consultations and prescriptions. While formally legalized in Tunisia since April 2022, the rapid expansion of telemedicine during the COVID-19 pandemic underscored the need for clear guidelines and regulations to ensure its safe and effective implementation.
Looking ahead, continued research and innovation in telemedicine technologies are critical to optimizing its potential in healthcare delivery. Addressing barriers to adoption, ensuring equitable access to digital health tools, and refining regulatory frameworks will be essential steps in expanding telemedicine’s reach and impact across diverse patient populations and healthcare settings.
Limitations
The sample size is relatively small, but we have slightly exceeded the number of subjects required, giving us a representative sample. Limiting inclusion to patients with a good socioeconomic status and residing in Sousse may introduce bias, as it excludes a broader demographic that may have different healthcare needs and outcomes. Due to the nature of the intervention (telemedicine calls), blinding of participants and healthcare providers was not feasible, potentially influencing subjective outcomes such as patient satisfaction. The study’s 30-day follow-up period may not capture long-term effects of telemedicine interventions on patient outcomes and healthcare utilization. However, we believe that this duration is sufficient for acute illnesses, which constitute the most common reason for emergency department visits. Conducting the study at a single center (Farhat Hached Hospital, Sousse) limits the generalizability of findings to other healthcare settings with different patient populations and resources. The outcome measures, such as patient satisfaction, are inherently subjective and may be influenced by factors beyond the telemedicine intervention itself, but it’s important to carry out this type of survey in order to improve the quality of care services.The study did not include an analysis of the cost-effectiveness of implementing telemedicine in emergency care settings, which could provide valuable insights into the economic feasibility and sustainability of such interventions.
Recommendations
As recommendations, we should strengthen training programs for physicians and nurses to optimize telemedicine care delivery. Include a broader range of patients, including those from diverse socioeconomic backgrounds, to assess telemedicine effectiveness more comprehensively. Replicate this study in multiple healthcare centers to confirm the validity and efficacy of telemedicine in different contexts. Maintain ongoing assessment of patient satisfaction over the long term to better understand the continued impact of telemedicine on patient experience. Perform cost-effectiveness analysis to evaluate the economic viability of integrating telemedicine into emergency care. And incorporating newer technologies and platforms in telemedicine interventions to enhance accessibility, reliability, and patient engagement including video-consultation.
Contribution of this work
This is a prospective interventional controlled study conducted on a sample of 400 patients.
This research enabled us to assess the feasibility of a telemedicine project in emergency services in Tunisia through a tertiary care emergency department, and the willingness of Tunisian patients to embrace this type of practice.
This work reaffirms the role of telemedicine in reducing re-consultations and increasing treatment adherence.
Conclusion
This research study underscores the pivotal role of telemedicine in modern medical practice, particularly in the effective management of non-emergency cases while enhancing patient outcomes. Its potential in reducing the number of patients presenting to emergency departments and the frequency of subsequent consultations, while also improving treatment adherence, could lead to a significant alleviation to overcrowded emergency departments.
The feasibility and acceptance of telemedicine in Tunisia are significantly enhanced by high patient satisfaction, particularly in the context of global health crises like the recent outbreak of the novel coronavirus (2019-nCoV). To integrate telemedicine into routine clinical practice, it is essential to address regulatory challenges and guarantee that all individuals have equitable access to digital health tools. To maximize the impact of telemedicine across diverse healthcare settings and develop a sustainable healthcare system that prioritizes efficiency, patient-centred care, and cost-effectiveness, it is vital to pursue ongoing research and innovation.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- COPD:
-
Chronic Obstructive Pulmonary Disease
- COVID 19:
-
Coronavirus Disease of 2019
- ENT:
-
Ear, Nose and Throat
- WHO:
-
World Health Organization
References
World Health Organization. Telemedicine: opportunities and developments in member states: report on the second global survey on eHealth. Geneva, Switzerland: World Health Organization; 2010. p. 93. (Global observatory for eHealth series).
PAHO/WHO | Pan American Health Organization Tool for. assessing the maturity level of health institutions to implement telemedicine services - [Internet]. [cited 2021 Oct 13]. https://www.paho.org/en/documents/tool-assessing-maturity-level-health-institutions-implement-telemedicine-services
Telemedicine takes center stage. in the era of COVID-19 [Internet]. [cited 2021 Oct 13]. https://www.science.org/content/article/telemedicine-takes-center-stage-era-covid-19
Eldon Taylor C, LoPiccolo CJ, Eisdorfer C, Clemence C. Best practices: reducing rehospitalization with Telephonic targeted Care Management in a Managed Health Care Plan. Psychiatr Serv. 2005;56(6):652–4.
Caffery LJ, Farjian M, Smith AC. Telehealth interventions for reducing waiting lists and waiting times for specialist outpatient services: a scoping review. J Telemed Telecare. 2016;22(8):504–12.
Khonsari S, Subramanian P, Chinna K, Latif L, Wan Ling L, Gholami O. Effect of a reminder system using an automated short message service on medication adherence following acute coronary syndrome. Eur J Cardiovasc Nurs. 2014;14.
Hamine S, Gerth-Guyette E, Faulx D, Green BB, Ginsburg AS. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: a systematic review. J Med Internet Res. 2015;17(2):e52.
Agha Z, Schapira RM, Laud PW, McNutt G, Roter DL. Patient satisfaction with physician-patient communication during telemedicine. Telemed J E-Health off J Am Telemed Assoc. 2009;15(9):830–9.
Gomes-de Almeida S, Marabujo T, do, Carmo-Gonçalves M. Telemedicine satisfaction of primary care patients during COVID-19 pandemics. Semergen. 2021 Mar 11.
Gagneux-Brunon A, Flocard F, Botelho-Nevers E. Telemedicine: a new tool for managing patients with heart failure. Rev Med Suisse [Internet]. 2016 Jul 12 [cited 2021 Jul 7];12(542). https://pubmed.ncbi.nlm.nih.gov/28700168/
Koehler F, Koehler K, Deckwart O, Prescher S, Wegscheider K, Kirwan B-A, et al. Efficacy of telemedical interventional management in patients with heart failure (TIM-HF2): a randomised, controlled, parallel-group, unmasked trial. Lancet Lond Engl. 2018;392(10152):1047–57.
Kruse CS, Krowski N, Rodriguez B, Tran L, Vela J, Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7(8):e016242.
Bourbeau J, Casan P, Tognella S, Haidl P, Texereau JB, Kessler R. An international randomized study of a home-based self-management program for severe COPD: the COMET. Int J Chron Obstruct Pulmon Dis. 2016;11:1447–51.
Haj Salem N, Ouelha D, Gharbaoui M, Saadi S, Ben Khelil M. Medico-legal aspects related to Telemedicine in Tunisia in the context of the covid-19 pandemic. Tunis Med. 2020;98(6):423–33.
Acknowledgements
We would like to thank the entire emergency team and all the patients who agreed to take part in the study.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
H BS: Conceptualization, Methodology, Writing. I L: Data Collection, Formal Analysis, Writing. S C: Review & Editing. M K: Project administration. S Y: Project administration. O H: Review & Editing. M M: Visualization, Supervision. Z M: Visualization, Supervision.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the ethical principles of the Declaration of Helsinki and was approved by the Ethical Committee of Faculty of medicine of Sousse (Reference: CEFMS 228/2024). Participation in the study was voluntary, and written informed consent was obtained from each participant after clarification of the study objectives. To ensure anonymity and confidentiality, full names were not collected. It is not a clinical trial.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Soltane, H.B., Lazrak, I., Chelly, S. et al. Place of telemedicine in the organization of emergency care: feasibility and benefits. BMC Emerg Med 24, 160 (2024). https://doi.org/10.1186/s12873-024-01074-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12873-024-01074-y