Abstract
Background
Early diagnosis and control of risk factors affecting frailty syndrome (FS) in older adults may lead to changes in the health/disease process, prevention of disability and dependency in the older adults, and reduction of health care costs and mortality rates. The aim of this study was to determine the predictive role of CVD risk factors and FS in community-dwelling older adults of Amirkola city in Iran.
Methods
This descriptive-analytic cross-sectional study is part of the second phase of the Amirkola Health and Aging Project (AHAP) cohort study conducted since 2011 on all individuals ≥ 60 years in the city of Amirkola in northern Iran. Totally, 1000 older adults were included in the study and divided into three groups: frail (n = 299), pre-frail (n = 455), and non-frail (n = 246) older adults. In the present study, age ≥ 60 years, female sex, fasting blood sugar (FBS) ≥ 126 mg/dl, affected diabetes mellitus (DM), body mass index (BMI) ≥ 27 kg/m², waist circumference (WC) or abdominal obesity > 102 cm in men and > 88 cm in women, low-density lipoprotein (LDL) > 100 mg/dl, triglyceride > 150 mg/dl, cholesterol > 200 mg/dl, high-density lipoprotein (HDL) < 40 mg/dl and blood pressure (BP) > 90/140 mmHg, uric acid > 7 mg/dl and a positive smoking history were considered CVD risk factors.
Results
The results showed that with each centimeter increase in WC, the odds of frailty compared with non-frailty was 79% higher, and the odds of frailty compared with pre-frailty was 1.43 times higher in older adults. In addition, the prevalence of pre-frailty compared with non-frailty, pre-frailty, and non-frailty was 10.59 times, 6.08 times, and 73.83 times higher in older individuals > 84 years old, respectively. The results of the present study indicated that the prevalence of pre-frailty compared with non-frailty, frailty compared with pre-frailty, and frailty compared with non-frailty was 2.86 times, 3.01 times, and 14.83 times higher in older adults women, respectively. The comparison between frail and non-frail groups represented that in DM older adults, the prevalence of frailty compared with non-frailty was 1.84 times higher and that of frailty compared with pre-frailty was 98% higher. The older adults with an FBS ≥ 126 mg/dl were 53% more likely to become frail, and with each unit increase in uric acid, the odds of becoming frail increased 2.05 times compared with non-frail older adults, and pre-frail compared with non-frail increased 99%.
Conclusion
The results demonstrated that CVD risk factors predictive of FS included central obesity, age > 84 years, female sex, DM, FBS ≥ 126, and uric acid > 7. This problem highlights the need for preventive strategies in the older adults who are simultaneously vulnerable to CVD and frailty.
Highlights
Frailty syndrome (FS) is an important health challenge for older adults in various dimensions.
Studying the health problems of the older adults such as FS and the factors affecting them in the growing older adults in countries such as Iran is one of the priorities of research.
Few population-based studies have described cardiovascular disease (CVD) risk factors that influence FS.
This study was conducted on 1000 community-dwelling older adults.
The results showed that CVD risk factors such as abdominal obesity, age over 84 years, female sex, DM, FBS ≥ 126, and URIC acid > 7 were predictors of FS.
Screening for CVD risk factors during visits of older adults to clinics and health centers can help identify older adultsat risk of frailty and pre-frailty.
Management of CVD risk factors can lead to evidence-based interventions and reduce the burden of care for these individuals.
Similar content being viewed by others
Introduction
According to the statistics of the World Health Organization, 80% of the older adults will live in low- and middle-income countries in 2050 [1]. It is projected that by 2030, the older adults population worldwide, particularly in Asia, will account for at least 30% of the total population [2]. It is also anticipated that by 2060, the number of older adults Asians will exceed 1.2 billion, meaning that one in every ten people globally will be an older adults Asian [3]. In Iran, the number of older adults has also increased significantly in recent years [4]. Therefore, the need to address the health of this population in various physical, psychological, and social dimensions is becoming increasingly evident. The increasing number of older adults is considered an important public health challenge to improve health and social care for this population group [5].
One of the particular concerns in the older adults is the occurrence of frailty syndrome (FS) [6], which is considered a clinical syndrome and vulnerable condition [7]. FS is actually not a disease, but a complex combination of the natural aging process and various medical problems [8], which is defined as a dynamic clinical condition associated with the degeneration of mental, physical, and social functions in the older adults [9].
The results of epidemiological studies in this area have shown that this phenomenon has a significant prevalence in the older adults. Thus, the prevalence in the older adults ≥ 65 years has been reported to range from 4 to 59% [10]. The worldwide incidence of FS in the older adults ≥ 60 years per 1000 population per year is estimated to be 33.4-95% (CI: 31.37–35.50%) [11]. Results from the Amirkola Health and Aging Project (AHAP) cohort in Iran also suggested that out of 2135 older adults ≥ 60 years, 672 cases (33.4%;95% CI: 31.37–35.50%) had FS and 874 (43.5%) people were classified as pre-frailty. The prevalence of FS was significantly higher in women (50.8%; 95% CI: 47.58–54.05%) than in men (18.7%; 95% CI: 16.41–21.05%) [12].
FS as a complex situation is accompanied by weakness, slowness, decreased energy, reduced physical activities, and in more severe cases, unwanted weight loss [13]. The results of numerous studies show that older adults with FS are at higher risk for problems such as disability, risk of falls [14], fractures [15, 16], frequent hospitalization in medical centers, and premature death [17]. By increasing the susceptibility of the older adults to stressors, FS leads to a decrease in physiological reserves in various body systems and has negative effects on the health of the older adults. Thus, frail older adults have poorer health status compared with non-frail older adults, especially in the area of physical health [18] .
Since FS in the older adults may cause the onset and increase of health problems as well as increase the financial burden on healthcare systems [19], the goal of researchers around the world is to increase knowledge of potential risk factors and strategies to prevent its occurrence [20].
Because of the high prevalence of cardiovascular disease (CVD) in the older adults [21] and its reciprocal association with FS [22, 23], researchers today have paid special attention to the role of CVD risk factors in the incidence of FS, with the goal of reducing the incidence of FS by controlling the factors influencing it [24,25,26]. Most CVD risk factors considered by researchers in various studies include unsuitable eating habits, diabetes mellitus (DM), hypertension, sedentary lifestyle, and smoking. Although the results of some studies revealed that the main CVD risk factors could predict FS in the older adults [24,25,26,27], the results of the study by Vaes et al. (2017) showed that there was no significant relationship between traditional CVD risk factors and mortality in the frail older adults studied [28].
The results of a systematic review by Shakya et al. (2022) indicated that abdominal obesity, hyperglycemia, and the co-occurrence of multiple cardiometabolic risk factors were consistently associated with increased frailty risk in both cross-sectional and longitudinal studies, after adjusting for potential variables including social age, gender, education, lifestyle factors such as physical activity, smoking, and alcohol use, and chronic diseases such as diabetes, arthritis, CVD, stroke, chronic lung disease, and kidney disease. However, the results of examining the relationship between dyslipidemia, hypertension, and FS were inconsistent in some studies included in this systematic review [29].
Therefore, further studies are needed to confirm the predictive and clinically important association between cardiometabolic risk factors and FS. Since early detection and control of risk factors affecting FS in the older adults can lead to changes in the health/disease process, prevention of disability and long-term care in the older adults, and reduction of health care costs and mortality [26, 30] and no study in Iran has investigated the possible relationship between CVD risk factors and FS, the aim of the present study was to determine the predictive role of CVD and FS risk factors in the community-dwelling older adults of Amirkola city, Iran.
Methods
This descriptive-analytic cross-sectional study is part of the second phase of the AHAP cohort study conducted since 2011 on all individuals ≥ 60 years in the city of Amirkola in northern Iran [31]. Amirkola city is located in Mazandaran province of Iran and has two health centers where the list of all older adults and their addresses are available. The researchers invited all the older adults to participate in the study by calling them and visiting them at home while giving them the necessary information about the project. The number of older adults in the second phase of the AHAP was 2135, who were enrolled in the study through a census. Inclusion criteria included older adults who were residents of the city of Amirkola.
Exclusion criteria were deficiencies in the collected data, lack of ability to answer questions (due to severe speech impairment or hearing loss), and cognitive impairment. Cognitive impairments were assessed by Mini-Mental State Examination (MMSE). The Foroughan study demonstrated satisfactory reliability and validity for the MMSE, with a Cronbach’s alpha of 0.78. At a cutoff point of 21, the MMSE exhibited a sensitivity of 90% and a specificity of 84% [30]. Data were collected by trained individuals. A total of 1000 older adults were enrolled in the current study and divided into three groups: frail (n = 299), pre-frail (n = 455), and non-frail (n = 246) older adults.
To identify the older adults with FS, the indicators defined by Fried et al. [7] were used, including 1- Exhaustion, 2- muscle weakness, 3- slowness to walk, 4- low physical activity level, and 5- weight loss. This instrument was completed through interviews with older adults. In the current study, frailty and pre-frailty were defined as ≥ 3 indicators and 1–2 indicators out of 5 indicators, respectively [32]. The validity and reliability of this instrument were confirmed by the study of Dent et al. (2016) [33]. In the Iranian older adults, this instrument also demonstrated acceptable validity and reliability [34].
In the present study, CVD risk factors were considered as exposure, which included the following: age ≥ 60 years [35], female sex [36], fasting blood sugar (FBS) ≥ 126 mg/dl, affected DM, body mass index (BMI) ≥ 27 kg/m², waist circumference (WC) or abdominal obesity > 102 cm in men and > 88 cm in women [37], low-density lipoprotein (LDL) > 100 mg/dl, triglyceride > 150 mg/dl, cholesterol > 200 mg/dl, high-density lipoprotein (HDL) < 40 mg/dl and blood pressure (BP) > 90/140 mmHg, and uric acid > 7 mg/dl [38] and a positive smoking history. In the ongoing study, DM was diagnosed when FBS ≥ 126 mg/dl 2 times or a history of diabetes was established from medications and a physician’s prescription. Blood samples were analyzed at an accredited laboratory approved by Babol University of Medical Sciences.
Statistical analysis
Descriptive and inferential data analysis was performed using SPSS® 26.0 (SPSS, Inc., Chicago, IL, USA), with the significance level set at 5% for all statistical tests. In this study, descriptive and inferential statistics were used to investigate the research objectives. In descriptive statistics, mean, standard deviation, frequency, and percentage indicators were reported. In inferential statistics, analysis of variance (ANOVA) and chi-square tests were used to compare three groups. Moreover, in order to identify CVD risk factors affecting FS, multinominal regression test was used. In this test, demographic variables were included as controls. Since the dependent variable was nominal with three categories (non-frailty, per-frailty, and frailty), multinomial logistic regression was employed in this study.
Results
In the current study, the mean age of the 1000 (47.4%= women, 52.6%=men) older adults of Amirkola city was 69.83 ± 7.40 years (for women = 68.93 ± 7.08, for men = 70.64 ± 7.59) in the age range of 60–94 years. Most of the older adults studied were aged 60–74 years (75%) and had a BMI ≥ 27 kg/m² (58.4%). Regarding CVD risk factors, FBS was high in 45.9% of the older adults (FBS ≥ 126). LDL was high in 56.2% (LDL > 100), triglycerides were high in 36.9% (TG > 150), cholesterol was high in 39% (cholesterol > 200), HDL was low in 19% of the older adults (HDL < 40), diastolic BP (DBP) was high in 26.7% (DIA > 90), systolic BP (SBP) was high in 49.4% (SBP > 140), uric acid was high in 11.1% (uric acid > 7), and WC was high in 17.7% (Table 1).
The results of ANOVA revealed that there was a significant difference between the three groups in terms of age (p < .001) and BMI (p < .001). Thus, mean age and BMI were higher in frail than in pre-frail and non-frail older adults, and higher in pre-frail than in non-frail older adults. The prevalence of abdominal obesity was higher in frail (23.4%) than in pre-frail (14.1%) and non-frail (17.5%) older adults.
Chi-square test results indicated a significant difference between the three groups in gender (p < .001), age (p < .001), BMI (p = .002), DM (p < .001), smoking (p = .003), FBS (p = .021), LDL (p = .004), and WC (p = .004). Therefore, the prevalence of frailty was higher in women (72.6%) than in men (27.4%). Among men, the prevalence of non-frailty was much higher (80.1%). Among the older adults > 84 years of age, the prevalence of frailty was 8.7%, while this rate was 3.1% in the pre-frail group and 5.5% in the non-frail group. The results also showed that the prevalence of frailty was higher in the older adults with a BMI ≥ 27 kg/m² (65.2%) than in other older adults (34.8%).
Moreover, the prevalence of frailty in older adultswith DM was 40.8%, while the proportion of DM was low in the pre-frail and non-frail groups. In addition, the proportion of smokers was higher in the non-frail (9.8%) and pre-frail (6.8%) groups than in the frail (2.7%) group. The results of the present study suggested that the prevalence of frailty in the older adults with an FBS ≥ 126 was 52.2%, whereas this prevalence was 44.6% and 40.7% in the pre-frail and non-frail groups, respectively. The results also showed that high LDL was higher in the non-frail group (63.8%) than in the other two groups. However, the results demonstrated that indices of TG, cholesterol, HDL, DBP, SBP, and uric acid were similar in the three frail, pre-frail, and non-frail groups (Table 1).
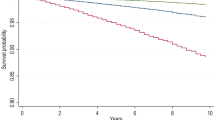
The results of ANOVA represented that there was a significant difference between the three groups in terms of WC (p = .010) and height (p < .001) (Figs. 1 and 2, and 3). Hence, the WC of the frail group was higher than that of the pre-frail group, and the height of the frail group was lower than that of the pre-frail and non-frail groups. However, the weight of the older adults in the three groups was similar (p = .058).
Multinominal logistic regression was used to investigate the relationship between demographic variables and CVD risk factors with frailty in the older adults. The results are illustrated in Tables 2 and 3, with non-frail older adults considered as the reference class (zero level). The independent variables (CVD risk factors) and the control variables (demographics) were entered into the model simultaneously.
The results exhibited that there was a significant relationship between pre-frail and non-frail older adults in terms of gender. Hence, the prevalence of pre-frailty than non-frailty was 2.86 times higher in older adults women. The results also indicated that the prevalence of pre-frailty than non-frailty was 10.59 times higher in older adults > 84 years old. In addition, the prevalence of pre-frailty was 73% higher than that of non-frailty in the older adults 75–84 years. The model obtained was also significant (LR χ2 (32) = 300.995, p < .001) and showed a similar pattern of results when comparing the frail and pre-frail groups with the non-frail group.
The comparison between the pre-frail and non-frail groups revealed that only uric acid (OR = 1.99, P < .05) was a significant predictor of FS after controlling for demographic variables. The odds ratio also indicated that with each unit increase in uric acid, the odds of an older adults having pre-frailty compared with non-frailty was 99%. Additionally, after controlling for demographic variables, the results suggested that other CVD risk factors had no significant predictive role on the incidence of FS when comparing the pre-frail and non-frail groups.
There was a significant relationship between the frail and non-frail groups for the gender variable. Thus, the prevalence of frailty was 14.83 times higher than that of non-frailty in older women. Furthermore, the results represented that the prevalence of frailty compared with non-frailty was 73.83 times higher in the older adults > 84 years old. Further, the prevalence of frailty compared with non-frailty was 2.33 times higher in older adults aged 75–84 years. Comparison between frail and non-frail groups revealed that DM (OR = 2.84, P < .01), FBS (OR = 1.53, P < .05), LDL (OR = 0.459, P < .01), uric acid (OR = 3.05, P < .01) and WC (OR = 1.79, P < .05) were significant predictors of FS after controlling for demographic variables.
Therefore, the prevalence of frailty compared with non-frailty was 1.84 times higher in the older adults with DM. In addition, the results manifested that the odds of frailty was 53% higher in the older adults with high FBS. Older adults with LDL > 100 were 54.1% less likely to be frail compared with non-frail older adults. The odds ratio also suggested that with each unit increase in uric acid and with each centimeter increase in WC, the odds of becoming frail compared with non-frail was 2.05 times and 79% higher, respectively. Controlling for demographic variables, the results indicated that other CVD risk factors did not play a significant predictive role for the incidence of FS when comparing the frail and non-frail groups.
For more accurate extraction, a comparison was made between CVD risk factors in frail and pre-frail older adults. The demographic variable of gender had a significant relationship in the comparison between the frail and pre-frail groups. Hence, the prevalence of frailty compared with pre-frailty was 3.01 times higher in older women. The results also represented that the prevalence of frailty compared with pre-frailty was 6.08 times higher in the older adults > 84 years. Furthermore, the prevalence of frailty compared with pre-frailty was 99% higher in older adults aged 75–84 years.
Comparison between frail and pre-frail groups illustrated that the risk factors of DM (OR = 1.98, P < .01), SBP (OR = 0.68, P < .05) and WC (OR = 2.43, P < .01) were significant predictors of FS after controlling for demographic variables. Therefore, the odds of frailty compared with pre-frailty was 98% higher in the older adults with DM. Moreover, the results suggested that the odds of frailty compared with pre-frailty was 32% lower in the older adults with high SBP. In addition, it was observed that with each centimeter increase in WC, the odds of frailty compared with pre-frailty was 1.43 times higher in older adults. Controlling for demographic variables, it was found that other CVD risk factors had no significant predictive role on the incidence of FS when comparing the frail and pre-frail groups (Table 4).
Discussion
The aim of this study was to determine the predictive role of CVD risk factors and FS in community-dwelling older adults of Amirkola city in Iran. In this study, we utilized Fried’s five-item index for the assessment of frailty. The psychometric characteristics and threshold values of this tool differ across countries due to variations in cultural, social, nutritional, and even phenotypic factors relative to other indices [33]. Consequently, for this research, we employed this instrument, which is one of the most widely used scales for frailty screening. Its validity and reliability have been rigorously evaluated and established within the Iranian older adults [34, 39]. The results showed that with each centimeter increase in WC, the odds of frailty compared with non-frailty was 79% higher and the odds of frailty compared with pre-frailty was 1.43 times higher in older adults. Ramsay et al. (2014) also reported that frail compared with non-frail older adults (OR 2.30, 95% CI 1.67 to 3.17) had higher WC [32]. The results of Uchai, et al. (2023) in a 21-year follow-up of adults suggested that individuals with high (OR 2.14, 95% CI 1.59 to 2.87) or relatively high (OR 1.57, 95% CI 1.21 to 2.03) WC were more affected by frailty and pre-frailty compared with normal WC [40]. A positive association between higher WC and frailty in the older adults was also found in a 3.5-year follow-up study of two prospective Spanish cohorts [41]. This finding in the current study highlighted the importance of considering a high WC as a risk factor for FS and the importance of assessing WC in adulthood to reduce the risk of frailty in old age.
Moreover, the results of the present study showed that the prevalence of pre-frailty compared with non-frailty, frailty compared with pre-frailty, and frailty compared with non-frailty was 10.59 times, 6.08 times, and 73.83 times higher in the older adults > 84 years old, respectively. This finding is consistent with the results of other studies [42, 43]. This finding indicates that older adultsare more likely to be frail and pre-frail. Age can be used as a rapid and cost-effective screening for people who are potentially frail or at risk of FS.
The results revealed that the prevalence of pre-frailty compared with non-frailty, frailty compared with pre-frailty, and frailty compared with non-frailty was 2.86 times, 3.01 times, and 14.83 times higher in older adults women, respectively, which is in agreement with other results [44,45,46,47]. Consideration of the gender factor in the incidence of FS may be useful in planning public health interventions to prevent FS.
In the present study, the rate of smoking was higher in non-frail and pre-frail individuals than in frail people. Nevertheless, the results of the study by Graciani et al. (2016) represented that not smoking was associated with a decrease in all frailty indices [48]. Ricci et al. also stated that smoking was associated with a higher likelihood of frailty in older adults [47]. However, Wang et al. (2022) concluded that the lowest prevalence of CVD risk factors as a predictor of FS was related to smoking risk factor (10.4%) [26].
The comparison between frail and non-frail groups exhibited that in DM older adults, the prevalence of frailty compared with non-frailty was 1.84 times higher and the odds of frailty compared with pre-frailty was 98% higher. Additionally, the odds of frailty was 53% higher in the older adults with high FBS. In the study by Ricci et al., it was observed that among CVD risk factors, DM was most common among frail and pre-frail participants [26]. This finding is consistent with the results of other studies on older adults in Brazil [49] and China [50].
A similar result was found in the Cardiovascular Health Study, in which DM was present in 25% of frail individuals, in 18.2% of pre-frail persons, and in only 12% of non-frail participants [51]. Nevertheless, the results of Barbosa et al. (2012) indicated that fasting glucose levels were similar in the frail and non-frail groups [24]. Diabetes and increased FBS are thought to promote frailty and increase the risk of long-term care and death due to insulin resistance and inflammation [52].
The results of several prospective cohorts on older adults ≥ 60 years have indicated that diabetes increases the incidence of new cases of frailty [53, 54]. On the other hand, some longitudinal studies have shown that frailty is a risk factor for the development of diabetes and that diabetes and frailty may interact and form a vicious cycle [55]. Because lifestyle-related diseases such as diabetes can be risk factors for frailty, careful control is important, at least in middle age.
In the ongoing study, with each unit increase in uric acid, the odds of frailty compared with non-frailty was 2.05 times, and the odds of pre-frailty compared with non-frailty was 99%. García-Esquinas et al. (2016) suggested that after multivariable adjustment, the odds ratio of FS between the second and third tertile of uric acid with the lowest tertile was 1.18 (0.83–1.68) and 1.57 (1.11–2.22) p-linear trend = 0.01, respectively [56]. However, the results of the study by Hwang et al. (2015) showed that there was no significant relationship between uric acid and frailty [57]. Further studies are needed to evaluate whether specific dietary recommendations or pharmacological strategies to lower serum uric acid can prevent the development of FS.
The results demonstrated that the odds of frailty compared with pre-frailty was 32% lower in the older adults with high SBP. Nevertheless, the results of the study by Graciani et al. (2016) on 1745 older adults ≥ 60 years represented that BP < 140/90 mm Hg was associated with a decrease in all frailty indices [48]. In the study of Ricci et al. (2014), hypertension was the most common risk factor (84.4%) for CVD in the older adults, regardless of FS classification (Fisher’s exact test: P = .005; P = .021) [26]. Ramsay et al. (2014) concluded that high BP (OR 1.79, 95% CI 1.27 to 2.54) was observed more frequently in the frail group than in the pre-frail group [32]. The study conducted by Liu et al. (2022) also demonstrated that hypertension represents a significant risk factor for cardiovascular disease among the older adults in Brazil [49].
Also, the results of a systematic review showed that 14% of people with hypertension had FS [58]. Although there was no relationship between high SBP and FS in the present study, given the results of other studies and considering the potential impact of frailty on the risk-benefit ratio of hypertension treatment and the high prevalence of hypertension, it is important to evaluate frailty in people with hypertension [58].
In addition, the results of the current study showed that older adults with LDL > 100 were 54.1% less likely to be frail compared with those who were not frail. Previous studies have indicated an association between elevated serum LDL levels and the risk of FS [59]. Therefore, the use of lipid-lowering agents with different mechanisms of action could be an effective measure to reduce FS.
Strengths
The present study was strengthened by using data from the AHAP, a well-known national study on health and aging in Iran, which is one of the few population-based studies that includes valid criteria. The use of a cohort database, which is characterized by high reliability and minimal attrition rates, may be one of the strengths of this study. A large sample of community-dwelling older adults men and women who were cognitively well-functioning and the fact that we presented results on a wide range of CVD risk factors and their association with FS in a community-dwelling older adults sample of older Iranian men and women are additional strengths of the present study. Data were collected through interviews and standard questionnaires.
Limitations
In the present study, a cross-sectional analysis was performed, which limits conclusions about causality. In addition, the Frail Scale was used to assess frailty in AHAP participants, and it is unclear whether other scales may yield different results. Another limitation is that the sample is not geographically representative of the entire older adults of Iran, even if it is demographically representative. This is because the genetic, geographic, and cultural structure of the Amirkola region in northern Iran could affect the prevalence of CVD risk factors. One of the exclusion criteria in this study was the presence of cognitive impairments. Consequently, we encourage other researchers to conduct further studies to explore the complex relationship between cognitive deficits and frailty. We believe that this will aid in a deeper understanding of frailty and its associated risk factors. The exclusion criteria applied in our research, which excluded individuals with severe speech impairment, hearing loss, and cognitive impairment, were implemented to ensure data quality and the ability of participants to provide accurate information. However, we acknowledge that these exclusions may have introduced a selection bias, as certain groups of older adults who may exhibit different frailty statuses or cardiovascular risk profiles were systematically excluded. Particularly notable is the non-inclusion of individuals with cognitive impairment, a prevalent condition among older adults, which could significantly influence both frailty development and cardiovascular risk factors. Consequently, while our study provides valuable insights into frailty and cardiovascular risk among older adults in Amirkola, the findings may not be fully generalizable to the broader population of older adults in the region or beyond. Furthermore, the applicability of our conclusions to older adults with cognitive impairment is limited, highlighting the need for future studies specifically targeting this subgroup to better understand their health profiles and needs.
Conclusion
The findings of the current study revealed that frail and pre-frail older adults, especially those with central obesity, age over 84 years, female sex, DM, FBS ≥ 126, and uric acid > 7, are more susceptible to developing CVD. This underscores the need for preventive strategies to avoid the concurrent occurrence of CVD and FS.
This problem highlights the need for preventive strategies in the older adults who are simultaneously vulnerable to CVD and frailty. Therefore, healthcare providers should look for CVD risk factors and take measures to prevent or control them to reduce the incidence of FS and CVD during visits of older adultsto clinics and health centers.
Data availability
Data generated or analysed during this study are included in this published article and are available from the corresponding author on reasonable request.
Abbreviations
- FS:
-
Frailty Syndrome
- CVD:
-
Cardiovascular Disease
- AHAP:
-
Health and Aging Project
- FBS:
-
Fasting Blood Sugar
- DM:
-
Diabetes Mellitus
- BMI:
-
Body Mass Index
- WC:
-
Waist Circumference
- LDL:
-
Low-Density Lipoprotein
- HDL:
-
High-Density Lipoprotein
- BP:
-
Blood Pressure
- DBP:
-
Diastolic BP
- SBP:
-
Systolic BP
- ANOVA:
-
Analysis of Variance
- MMSE:
-
Mini-Mental State Examination
References
Health UDo, Services H. Aging statistics. In.; 2014.
Jayawardhana T, Anuththara S, Nimnadi T, Karadanaarachchi R, Jayathilaka R, Galappaththi K. Asian ageing: the relationship between the elderly population and economic growth in the Asian context. PLoS ONE. 2023;18(4):e0284895.
He W, Goodkind D, Kowal P, Almasarweh I, Giang T, Islam M. Asia aging: demographic, economic, and health transitions. US Department of Commerce, Washington, DC, USA, Report 2022(P95/22):1.
Doshmangir L, Khabiri R, Gordeev VS. Policies to address the impact of an ageing population in Iran. Lancet. 2023;401(10382):1078.
Samouei R, Keyvanara M. Explaining the challenges of the Iranian health system in the face of future aging: qualitative study. Iran J Ageing. 2022;16(4):608–23.
Jang H-Y, Kim J-H. Factors associated with frailty according to gender of older adults living alone. In: Healthcare: 2021. MDPI: 475.
Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. Journals Gerontol Ser A: Biol Sci Med Sci. 2004;59(3):M255–63.
Walston J, Robinson TN, Zieman S, McFarland F, Carpenter CR, Althoff KN, Andrew MK, Blaum CS, Brown PJ, Buta B. Integrating frailty research into the medical specialties—report from a U13 conference. J Am Geriatr Soc. 2017;65(10):2134–9.
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752–62.
Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc. 2012;60(8):1487–92.
Ofori-Asenso R, Chin KL, Mazidi M, Zomer E, Ilomaki J, Zullo AR, Gasevic D, Ademi Z, Korhonen MJ, LoGiudice D. Global incidence of frailty and prefrailty among community-dwelling older adults: a systematic review and meta-analysis. JAMA Netw open. 2019;2(8):e198398–198398.
Boura FT, Hosseini SR, Mouodi S, Ghadimi R, Bijani A. Frailty syndrome in older adults and related sociodemographic factors in the north of Iran: a population-based study. Iran Red Crescent Med J 2021, 23(1).
Vermeulen J, Neyens JC, van Rossum E, Spreeuwenberg MD, de Witte LP. Predicting ADL disability in community-dwelling elderly people using physical frailty indicators: a systematic review. BMC Geriatr. 2011;11(1):1–11.
Fhon JRS, Rosset I, Freitas CP, Silva AO, Santos JLF, Rodrigues RAP. Prevalência De quedas de idosos em situação de fragilidade. Rev Saúde Pública. 2013;47:266–73.
Ensrud KE, Ewing SK, Taylor BC, Fink HA, Stone KL, Cauley JA, Tracy JK, Hochberg MC, Rodondi N, Cawthon PM. Frailty and risk of falls, fracture, and mortality in older women: the study of osteoporotic fractures. Journals Gerontol Ser A: Biol Sci Med Sci. 2007;62(7):744–51.
Van Den Bergh JP, Van Geel TA, Geusens PP. Osteoporosis, frailty and fracture: implications for case finding and therapy. Nat Rev Rheumatol. 2012;8(3):163–72.
Collard R. Frailty & late-life depression: a delicate balance. [Sl]:[Sn]; 2015.
Ritt M, Bollheimer L, Sieber C, Gaßmann K. Prediction of one-year mortality by five different frailty instruments: a comparative study in hospitalized geriatric patients. Arch Gerontol Geriatr. 2016;66:66–72.
Tavares DMS, Colamego CG, Pegorari MS, Ferreira PCS, Dias FA, Bolina AF. Cardiovascular risk factors associated with frailty syndrome among hospitalized elderly people: a cross-sectional study. Sao Paulo Med J. 2016;134(5):393–9.
Hubbard RE, Lang IA, Llewellyn DJ, Rockwood K. Frailty, body mass index, and abdominal obesity in older people. Journals Gerontol Ser A: Biomedical Sci Med Sci. 2009;65(4):377–81.
Aïdoud A, Gana W, Poitau F, Debacq C, Leroy V, Nkodo JA, Poupin P, Angoulvant D, Fougère B. High prevalence of geriatric conditions among older adults with cardiovascular disease. J Am Heart Association. 2023;12(2):e026850.
Afilalo J, Alexander KP, Mack MJ, Maurer MS, Green P, Allen LA, Popma JJ, Ferrucci L, Forman DE. Frailty assessment in the cardiovascular care of older adults. J Am Coll Cardiol. 2014;63(8):747–62.
Ekram AS, Tonkin AM, Ryan J, Beilin L, Ernst ME, Espinoza SE, McNeil JJ, Nelson MR, Reid CM, Newman AB. The association between frailty and incident cardiovascular disease events in community-dwelling healthy older adults. Am Heart J plus: Cardiol Res Pract. 2023;28:100289.
Bastos-Barbosa RG, Ferriolli E, Coelho EB, Moriguti JC, Nobre F, da Costa Lima NK. Association of Frailty syndrome in the elderly with higher blood pressure and other cardiovascular risk factors. Am J Hypertens. 2012;25(11):1156–61.
Pereira JC, Barreto SM, Passos V. Cardiovascular risk profile and health self-evaluation in Brazil: a population-based study. Revista Panam De Salud Publica = Pan Am J Public Health. 2009;25(6):491–8.
Ricci NA, Pessoa GS, Ferriolli E, Dias RC, Perracini MR. Frailty and cardiovascular risk in community-dwelling elderly: a population-based study. Clin Interv Aging 2014:1677–85.
Bouillon K, Batty GD, Hamer M, Sabia S, Shipley MJ, Britton A, Singh-Manoux A, Kivimäki M. Cardiovascular disease risk scores in identifying future frailty: the Whitehall II prospective cohort study. Heart. 2013;99(10):737–42.
Vaes B, Depoortere D, Van Pottelbergh G, Matheï C, Neto J, Degryse J. Association between traditional cardiovascular risk factors and mortality in the oldest old: untangling the role of frailty. BMC Geriatr. 2017;17(1):1–8.
Shakya S, Bajracharya R, Ledbetter L, Cary MP Jr. The association between cardiometabolic risk factors and frailty in older adults: a systematic review. Innov Aging. 2022;6(5):igac032.
Wleklik M, Denfeld Q, Lisiak M, Czapla M, Kałużna-Oleksy M, Uchmanowicz I. Frailty Syndrome in older adults with Cardiovascular diseases–what do we know and what requires further research? Int J Environ Res Public Health. 2022;19(4):2234.
Bijani A, Ghadimi R, Mikaniki E, Kheirkhah F, Mozaffarpur SA, Motallebnejad M, Esmaili H, Majidi F, Cumming RG, Hosseini SR. Cohort profile update: the Amirkola health and ageing project (AHAP). Caspian J Intern Med. 2017;8(3):205.
Ramsay S, Arianayagam D, Whincup P, Lennon L, Cryer J, Papacosta A, Iliffe S, Wannamethee S. Cardiovascular risk profile and frailty in a population-based study of older British men. Heart. 2015;101(8):616–22.
Dent E, Kowal P, Hoogendijk EO. Frailty measurement in research and clinical practice: a review. Eur J Intern Med. 2016;31:3–10.
Tavan F, Asadollahi A. Psychometric properties of Frailty Syndrome Checklist 5-Items in Frail older adults in Iran. Journal Health Sciences Surveillance System. 2021;9(3):162–8.
Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR. Heart disease and stroke statistics—2019 update: a report from the American Heart Association. Circulation. 2019;139(10):e56–528.
Rodgers JL, Jones J, Bolleddu SI, Vanthenapalli S, Rodgers LE, Shah K, Karia K, Panguluri SK. Cardiovascular risks associated with gender and aging. J Cardiovasc Dev Disease. 2019;6(2):19.
Zhao M, Vaartjes I, Graham I, Grobbee D, Spiering W, Klipstein-Grobusch K, Woodward M, Peters SA. Sex differences in risk factor management of coronary heart disease across three regions. Heart. 2017;103(20):1587–94.
Yang T-Y, Fang C-Y, Chen J-S, Po HL, Chou L-P, Chiang C-Y, Ueng K-C. Association of serum uric acid with cardiovascular disease in Taiwanese patients with primary hypertension. Acta Cardiol Sinica. 2015;31(1):42.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G. Frailty in older adults: evidence for a phenotype. Journals Gerontol Ser A: Biol Sci Med Sci. 2001;56(3):M146–57.
Uchai S, Andersen LF, Hopstock LA, Hjartåker A. Body mass index, waist circumference and pre-frailty/frailty: the Tromsø study 1994 – 2016. BMJ open. 2023;13(2):e065707.
García-Esquinas E, José García‐García F, León‐Muñoz LM, Carnicero JA, Guallar‐Castillón P, Gonzalez‐Colaço Harmand M, López‐García E, Alonso‐Bouzón C, Rodríguez‐Mañas L, Rodríguez‐Artalejo F. Obesity, fat distribution, and risk of frailty in two population‐based cohorts of older adults in S pain. Obesity. 2015;23(4):847–55.
Eyigor S, Kutsal Y, Duran E, Huner B, Paker N, Durmus B, Sahin N, Civelek GM, Gokkaya K, Doğan A. Frailty prevalence and related factors in the older adult—FrailTURK Project. Age. 2015;37:1–13.
Martins BA, Visvanathan R, Barrie H, Huang CH, Matsushita E, Okada K, Satake S, Uno C, Kuzuya M. Frailty prevalence using Frailty Index, associated factors and level of agreement among frailty tools in a cohort of Japanese older adults. Arch Gerontol Geriatr. 2019;84:103908.
Melo Filho J, Moreira NB, Vojciechowski AS, Biesek S, Bento PCB, Gomes ARS. Frailty prevalence and related factors in older adults from southern Brazil: a cross-sectional observational study. Clinics 2020, 75.
Delbari A, Zanjari N, Momtaz YA, Rahim F, Saeidimehr S. Prevalence of frailty and associated socio-demographic factors among community-dwelling older people in southwestern Iran: a cross-sectional study. J Diabetes Metabolic Disorders. 2021;20:601–10.
Merchant RA, Chen MZ, Tan LWL, Lim MY, Ho HK, van Dam RM. Singapore healthy older people everyday (HOPE) study: prevalence of frailty and associated factors in older adults. J Am Med Dir Assoc. 2017;18(8):734. e739-734. e714.
Wang X, Hu J, Wu D. Risk factors for frailty in older adults. Medicine 2022, 101(34).
Graciani A, García-Esquinas E, López-García E, Banegas JR, Rodríguez-Artalejo F. Ideal cardiovascular health and risk of frailty in older adults. Circulation: Cardiovasc Qual Outcomes. 2016;9(3):239–45.
Liu X, Tou NX, Gao Q, Gwee X, Wee SL, Ng TP. Frailty and risk of cardiovascular disease and mortality. PLoS ONE. 2022;17(9):e0272527.
He D, Li J, Li Y, Zhu J, Zhou T, Xu Y, Wu Q, Cheng Z, Chen Q, Liu Z. Frailty is associated with the progression of prediabetes to diabetes and elevated risks of cardiovascular disease and all-cause mortality in individuals with prediabetes and diabetes: evidence from two prospective cohorts. Diabetes Res Clin Pract. 2022;194:110145.
Walston J, McBurnie MA, Newman A, Tracy RP, Kop WJ, Hirsch CH, Gottdiener J, Fried LP, Investigators CHS. Frailty and activation of the inflammation and coagulation systems with and without clinical comorbidities: results from the Cardiovascular Health Study. Arch Intern Med. 2002;162(20):2333–41.
Morley JE, Malmstrom TK, Rodriguez-Mañas L, Sinclair AJ. Frailty, Sarcopenia and diabetes. J Am Med Dir Assoc. 2014;15(12):853–9.
García-Esquinas E, Graciani A, Guallar-Castillón P, López-García E, Rodríguez-Mañas L, Rodríguez-Artalejo F. Diabetes and risk of frailty and its potential mechanisms: a prospective cohort study of older adults. J Am Med Dir Assoc. 2015;16(9):748–54.
Espinoza SE, Jung I, Hazuda H. Frailty transitions in the San Antonio longitudinal study of aging. J Am Geriatr Soc. 2012;60(4):652–60.
Veronese N, Stubbs B, Fontana L, Trevisan C, Bolzetta F, De Rui M, Sartori L, Musacchio E, Zambon S, Maggi S. Frailty is associated with an increased risk of incident type 2 diabetes in the elderly. J Am Med Dir Assoc. 2016;17(10):902–7.
García-Esquinas E, Guallar-Castillón P, Carnicero JA, Buno A, García-García FJ, Rodríguez-Mañas L, Rodríguez-Artalejo F. Serum uric acid concentrations and risk of frailty in older adults. Exp Gerontol. 2016;82:160–5.
Hwang A-C, Liu L-K, Lee W-J, Chen L-Y, Peng L-N, Lin M-H, Chen L-K. Association of frailty and cardiometabolic risk among community-dwelling middle-aged and older people: results from the I-Lan longitudinal aging study. Rejuven Res. 2015;18(6):564–72.
Vetrano DL, Palmer KM, Galluzzo L, Giampaoli S, Marengoni A, Bernabei R, Onder G. Hypertension and frailty: a systematic review and meta-analysis. BMJ open. 2018;8(12):e024406.
Wang Q, Wang Y, Lehto K, Pedersen NL, Williams DM, Hägg S. Genetically-predicted life-long lowering of low-density lipoprotein cholesterol is associated with decreased frailty: a mendelian randomization study in UK Biobank. EBioMedicine. 2019;45:487–94.
Acknowledgements
The authors would like to thank the Deputy of the Research and Technology of Babol University of Medical Sciences and the AHAP team.
Funding
The study was funded by the Babol University of Medical Sciences. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization: SRH, AB, RGH, ASH and FG; Methodology: FG, MK and KS; Formal analysis: FGH, MRK and AB; Writing Original Draft: KS and ASH; Writing Review & Editing: RGH, SRH, AS, KS.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study is part of the AHAP, Babol, Iran. The present study was approved by the Ethics Committee of Babol University of Medical Sciences (IR.MUBABOL.HRI.REC.1397.018). Informed consent was obtained from all subjects. The methods involved in our research are carried out in accordance with relevant guidelines and regulations (Declaration of Helsinki).
Consent to publish
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Shamsalinia, A., Hosseini, S.R., Bijani, A. et al. Cardiovascular disease risk factors and frailty syndrome in community-dwelling older adults: Results from the Amirkola Health and Aging Project Cohort Study. BMC Geriatr 24, 665 (2024). https://doi.org/10.1186/s12877-024-05268-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-05268-8