Abstract
Background
In the pediatric population, Staphylococcus aureus infections are responsible for increased morbidity and mortality, length of hospitalization and the cost of inpatient treatment. The aim of this study is to describe the antimicrobial resistance profile of S. aureus isolated in clinical specimens from pediatric patients admitted to a tertiary hospital in Rio de Janeiro, Brazil.
Methods
Culture reports and medical records of hospitalized patients under 18 years of age with S. aureus infections between January 2015 and December 2022 were retrospectively analyzed. Information was collected on recent antibiotic use, previous hospital admission, inpatient unit, clinical specimen, time of infection (community or nosocomial), classification according to susceptibility to methicillin (methicillin sensitive - MSSA or methicillin resistant - MRSA) and sensitivity to other antimicrobials. We analyzed the distribution of the sensitivity profile of S. aureus infections over the 7 years evaluated in the study.
Results
Were included 255 unique clinical episodes, among which the frequencies of MSSA and MRSA were 164 (64%) and 91 (36%), respectively. Over the 7 years evaluated, there was stability in the prevalence percentage, with a predominance of MSSA in the range of 60 to 73.3%, except in 2020, when there was a drop in the prevalence of MSSA (from 73.3% in 2019 to 52.5%) with an increase in MRSA (from 26.7% in 2019 to 47.5%). Ninety-seven (38%) infections were community-acquired and 158 (62%) were healthcare-associated. The main clinical specimens collected were blood cultures (35.2%) and wound secretions (17%). The MRSA isolates presented percentages of sensitivity to trimethoprim-sulfamethoxazole from 90.4 to 100%, and to clindamycin from 77 to 89.8% in MRSA healthcare associated and MRSA community respectively.
Conclusion
There was a constant predominance in the prevalence of MSSA with percentage values maintained from 2015 to 2022, except in 2020, in which there was a specific drop in the prevalence of MSSA with an increase in MRSA. MSSA infections are still predominant in the pediatric population, but MRSA rates also present significant values, including in community infections, and should be considered in initial empiric therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Staphylococcus aureus (S. aureus) is a human commensal bacterium and a common component of the skin flora, preferentially inhabiting the nasal cavities, armpits, anterior nares, pharynx, vagina, rectum, perineum and damaged skin [1]. Symptomatic infection by S. aureus can occur after barrier breakdown in the skin or mucous membranes, with its severity influenced by bacterial virulence and host factors [2]. Illnesses caused by S. aureus range from skin and soft tissue infections to more serious infections. Currently, Methicillin-susceptible S. aureus (MSSA) is reported to be primarily responsible for cases of invasive infections in children in the USA (approximately 80%), with bloodstream infection rates progressively higher since 2009 [3].
In Brazil, S. aureus infections are extremely relevant in the pediatric population, but few studies have attempted to determine the prevalence of MSSA and Methicillin-resistant S. aureus (MRSA), both in cases originating in the community and in those related to healthcare. The main objective of this study is to describe the antimicrobial resistance profile of S. aureus isolated in clinical specimens from pediatric patients admitted to a tertiary hospital, also describing the clinical and demographic characteristics of this population.
Methods
This is a retrospective and observational study that analyzed culture reports and medical records of patients under 18 years of age, hospitalized at the Instituto Nacional de Saúde da Mulher, da Criança e do Adolescente Fernandes Figueira (IFF), with S. aureus infections between January 2015 and December 2022. The IFF is a pediatric care, teaching, research and technological development unit of the Fundação Oswaldo Cruz (FIOCRUZ) located in Rio de Janeiro/RJ, which has 83 pediatric inpatient beds.
Patients who had S. aureus identified in the cultures of clinical specimens, such as blood, urine, cerebrospinal fluid, pleural fluid, sputum and secretions (from wounds, abscesses, ocular, ear or other secretions) were included. Their total number and their respective antibiotic sensitivity tests (AST) were described, and the results were correlated with clinical data obtained from their medical records.
Wound or abscess secretions were included only if they were collected using an aseptic technique; sputum were included only if collected from patients with Cystic fibrosis, during a clinical exacerbation of the disease; and eye secretions, only if collected from patients with clinical symptoms of conjunctivitis. Bronchoalveolar lavage was excluded due to the impossibility of collecting it in a protected manner in the pediatric age group, which does not guarantee that the material will not be contaminated.
All samples considered in the study were collected from hospitalized pediatric patients who presented clinical signs of infection when the samples were obtained or had an adequate therapeutic response to Staphylococcal antibiotic therapy, thus justifying the diagnostic suspicion and collection of the material. Therefore, we considered that all positive cultures presented a high clinical correlation with the etiological agent.
S. aureus strains were identified, and their antibiotic susceptibility profiles were performed using the automated BioMérieux VITEK® 2 system. The following antibiotics were tested: linezolid, clindamycin, erythromycin, trimethoprim-sulfamethoxazole, vancomycin, penicillin, rifampicin, oxacillin, gentamicin and teicoplanin.
Community infections were those in which the positive culture was collected within 48 h of hospital admission. Nosocomial infections were considered in cases where the positive culture was collected after 48 h of hospital admission, if there was a report of surgery in the last 30 days and/or a report of surgery with implant placement in the last 90 days [4].
A form for data collection was created and the variables were analyzed and stored in a database in the Epi Info™ software version 7.2.5.0. Data were collected on sex, age, inpatient unit, patient origin, clinical specimen, classification regarding susceptibility to oxacillin (MSSA or MRSA), sensitivity to other antimicrobials, underlying disease, time of infection (community or hospital), use of antibiotics in the last month, hospital admission in the last year and presence of invasive medical devices. The results were presented in the form of absolute frequencies, mean, median, standard deviation and/or rates for categorical variables. To calculate the significance value, Pearson’s, χi2 test was used. p < 0.05 was considered statistically significant. We analyzed the distribution of the sensitivity profile of S. aureus infections over the 7 years evaluated in the study.
Results
Were identified 536 positive cultures for S. aureus. Of these, 245 (45.7%) did not meet the inclusion criteria. Of the 291 cases included in the research, 36 (12.3%) were excluded. Our sample was therefore composed of 255 cases. Figure 1 presents the flowchart detailing the case selection process.
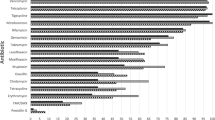
The frequencies of MSSA and MRSA were 164 (64%) and 91 (36%), respectively. When classifying MRSA strains, the frequency of Community-associated methicillin-resistant S. aureus (CA-MRSA) was 87 (95.6%) and of Hospital-acquired methicillin-resistant S. aureus (HA-MRSA) 4 (4.4%). No vancomycin-intermediately susceptible S. aureus (VISA - MIC 4–8 µg/mL for vancomycin) or vancomycin-resistant S. aureus (VRSA - MIC ≥ 16 µg/mL for vancomycin) strains were isolated during the study period. Due to the small number of HA-MRSA cases, data are presented grouped as MRSA cases. The distribution of the sensitivity profile of S. aureus infections over the 7 years evaluated in the research is shown in Graph 1.
The clinical and demographic characteristics of the studied population are presented in Table 1. The patients were predominantly male, 148 (58%) cases, and were less than one year old in 159 (62.4%) clinical episodes. The average age was 32 months, and the median was 2 months. One hundred and ninety-five (76.4%) patients had comorbidities, 124 (48.6%) had used antimicrobials in the last month and 115 (45%) patients had a history of hospitalization in the last year. Among the patients who had cultures with MRSA isolation, 53 (58.2% - p = 0.022) had used antimicrobials in the last month, 59 (64.8% - p = 0.001) had underlying disease, 15 (16.5% - p = 0.022) had admission to the Pediatric Intensive Care Unit and 13 (14.2% - p = 0.016) used an indwelling urinary catheter. There was no statistically significant difference between patients with isolation of MSSA or MRSA in other variables.
Regarding the place of acquisition of S. aureus and its susceptibility to methicillin, 97 (38%) infections were acquired in the community and 158 (62%) were associated with healthcare, with the distribution between MRSA and MSSA presented in the Table 1. Regarding the disposition by hospital inpatient unit, the sectors that presented the highest number of S. aureus isolates were the neonatal intensive care unit, the pediatric infectious diseases ward and the pediatric ward, with 28.2%, 23.5% and 14.1% of cases respectively. All sectors mostly isolated MSSA in cultures, except the pediatric intensive care unit and the semi-intensive unit, with an MRSA rate of 55.5% and 58.3% respectively. The invasive medical device most frequently found in healthcare-associated S. aureus infections was a central venous catheter, in 72 (45.5%) cases. Demographic and clinical characteristics of the pediatric patients in cases of MSSA and MRSA are presented in Table 1.
The types of clinical culture specimens and the respective isolated pathogens are shown in Table 2. The main specimens collected were blood (35.2%) and wound secretions (17%). MSSA isolation predominated in all types of samples, except in abscess secretions and pleural fluid, in which the frequency of MRSA was 55.5% and 77.7%, respectively. The 4 strains of HA-MRSA were isolated from blood cultures.
The susceptibility of S. aureus to other antimicrobials is shown in Tables 3 and 4. S. aureus MSSA showed a low rate of resistance to trimethoprim-sulfamethoxazole (1.8%) and a high rate of resistance to clindamycin and erythromycin (44.5% and 50.6%, respectively). Community-acquired S. aureus MRSA showed a high rate of resistance to erythromycin (38.4%), but with high susceptibility to trimethoprim-sulfamethoxazole and clindamycin, being 100% and 89.8%, respectively. Healthcare-associated S. aureus MRSA had a high susceptibility rate to clindamycin and trimethoprim-sulfamethoxazole (77% and 90.4%, respectively), and a low susceptibility rate to erythromycin (52%).
No resistance to vancomycin, linezolid or teicoplanin was observed in any of the samples, and only 3 isolates showed resistance to rifampicin: 1 from community-acquired infection (MSSA) and 2 from healthcare-associated infections (1 MSSA and 1 MRSA). Only 5 isolates were sensitive to Penicillin, a resistance rate of 98%.
Discussion
There are few articles that have determined the percentage of antimicrobial resistance in Staphylococcus aureus in clinical samples of hospitalized pediatric patients in Brazil, which makes our work very relevant to the community [5,6,7]. In the present study, the percentage of MSSA was 64% and of MRSA was 36%, rates like those reported in the Brazilian literature (66.7% for MSSA and 33.3% for MRSA) [5]. The CA-MRSA infection rate was 34.1%, a much higher value when compared to other Brazilian studies, which range from 8.6 to 17.2% [8, 6]. This result confirms a scenario of high resistance to methicillin/oxacillin, the antibiotic of choice in the empirical treatment of community-acquired staphylococcal diseases [3].
When analyzing the distribution of the sensitivity profile of S. aureus infections over the 7 years evaluated in our research, there was a stability in the prevalence percentage, with a predominance of MSSA in the range of 60 to 73.3%. However, rates in 2020 did not follow the pattern of previous years, showing a drop in the prevalence of MSSA (from 73.3% in 2019 to 52.5%) with an increase in MRSA (from 26.7% in 2019 to 47.5%). This same assessment of the evolution of susceptibility rates of isolates throughout the research period also occurred in the study carried out from January 2013 to December 2020 in a tertiary hospital in a state in southern Brazil, which analyzed and collected data from 563 patients under 18 years on site of infection, type of infection and susceptibility to methicillin and other antimicrobials. A discrepancy was observed between the proportion of CA-MRSA and HA-MRSA in 2020, with a drop in community-acquired staphylococcal infections (from 53.2% in 2019 to 37.5%) and an increase in those associated with healthcare (from 3.3% in 2019 to 7.3%). This result may coincide with social isolation due to the Sars-CoV-2 pandemic, impacting the reduction in the circulation of other infectious agents and a reduction in pediatric hospitalizations in general, with the isolation of MRSA prevailing in likely more serious cases of hospitalized patients [7].
Regarding the clinical and demographic characteristics of our series, there was a predominance of males, the median age was 2 months, 76.4% of patients had comorbidities, half had used antimicrobials in the last month and had a history of hospitalization in the last year. In a study carried out from January 2010 to December 2017 with pediatric patients in three hospitals in Turkey, the following characteristics were described: median age of 51 months; male prevalence (67.4%); mean ages of patients with MRSA and MSSA isolates of 51 and 50 months, respectively; half of the children had underlying illnesses and recent need for hospital care. Comparatively, our median age was lower and the number of patients with underlying disease was higher, but the other characteristics were similar [9].
Considering the various risk factors for CA-MRSA infections described in the literature, 76.4% patients had comorbidities, 48.6% had used antimicrobials in the last month and 45% had a history of hospitalization in the last year. Recent use of antimicrobials was the risk factor with the greatest statistical significance in our series (p < 0.05). Regarding predisposing factors for HA-MRSA infections, in the present study it was observed that the invasive medical device most frequently found in healthcare-associated infections was a central venous catheter, but the one with the greatest statistical significance was the indwelling bladder catheter (p < 0.05). A case-control study carried out in Portugal with adult patients hospitalized between September 1, 2015 and August 31, 2016 analyzed risk factors for the development of MRSA infection compared with MSSA infection, identifying the presence of bladder catheter (OR = 10.62, 95% CI 3.66–30.78), antibiotic therapy in the last 30 days (OR = 5.60, 95% CI 2.15–14.62) and recent hospital admission (OR = 2.66, 95% CI 1.14–6.23) [10]. The results of the present study are compatible with the care profile of our Institute, which in addition to receiving pediatric patients transferred from other hospital units for hospitalization in the ward and intensive care sectors, also has patients with chronic diseases and complex malformations with prolonged hospitalization, mainly in the newborn age group.
Regarding the place of acquisition of S. aureus and its susceptibility to methicillin, the prevalence of MRSA among community-acquired and healthcare-related infections in the present study were 40.2% and 32.9%, respectively. The rate of methicillin resistance reported worldwide in community strains is variable, being more than 70% in the USA [11], 25 to 62% in Latin America [12,13,14], and 46% in Brazil [7]. Thus, the hypothesis that MRSA is no longer an exclusively nosocomial pathogen is strengthened, and brings the warning that, when starting the empirical antibiotic therapy regimen for patients coming from the community with suspected staphylococcal disease, it should be discuss the choice of agents with coverage for CA-MRSA [6, 8].
When analyzing the prevalence of MRSA in the hospital admission sectors in the present study, it was observed that the main locations were the two intensive care units (neonatal and pediatric intensive care units) and the pediatric infectious diseases ward. Another Brazilian study carried out at a University Hospital in a state located in the South region, from April to June 2009, characterized the prevalence and susceptibility profile of S. aureus and showed no significant difference in the prevalence of MRSA between the different hospital units, including the areas inpatient (10%), outpatient (13.3%), emergency (10%) and surgical center, both pediatric and adult, but a higher frequency in surgical units (20%) was noted [5]. The IFF is a reference for high fetal risk prenatal care in Rio de Janeiro, receiving extremely premature newborns, with malformations, genetic diseases to be clarified and congenital infections, which makes up a highly complex profile in the neonatal intensive care unit. Due to the severity of these patients, they are exposed to the main risk factors for S. aureus infection in a nosocomial environment, such as the presence of invasive medical devices, the use of broad-spectrum antibiotic therapy and prolonged hospitalization [2, 15].
The main materials collected in the present study were blood, followed by wound secretions. These results differ from other articles, which present skin and soft tissue infections as the main primary site, with a predominance of S. aureus isolation in abscess secretions [6]. Regarding susceptibility to methicillin, in our series MSSA was the main isolate in most materials, except in abscess secretions and pleural fluid, in which the frequency of MRSA was 55.5% and 77.7%, respectively. This prevalence of MRSA in abscess secretions differs from the literature, which showed a predominance in the isolation of MSSA in skin and soft tissue infections, making the choice of methicillin/oxacillin for the empirical treatment of these conditions an option to be discussed [9].
When evaluating the susceptibility of S. aureus to other antimicrobials, our study shows a low rate of susceptibility to clindamycin among MSSA (55.5%), with a significant increase in the rate to 89.8% in CA-MRSA strains. Compared to trimethoprim-sulfamethoxazole, the sensitivity rate was higher, being 98.2% for MSSA and 100% for CA-MRSA. Fassbind reports a 96.1% susceptibility rate to trimethoprim-sulfamethoxazole in CA-MRSA strains, and a 64.9% susceptibility rate of MSSA to clindamycin. These results raise reservations regarding the empirical use of clindamycin, especially for cases in which MSSA infection is suspected, making trimethoprim-sulfamethoxazole a possible therapeutic alternative for uncomplicated infections in tissues and soft tissues [7].
Our study has several limitations, the main one being the fact that it was unicentric and retrospective based on the analysis of physical records and culture reports. Another important limitation was the failure to perform a molecular and genetic evaluation of the S. aureus strains, the isolates were classified exclusively on the presumed location of acquisition and pattern of susceptibility to antimicrobials.
Conclusion
In conclusion, there was a constant predominance in the prevalence of MSSA with percentage values maintained from 2015 to 2022, except in 2020, in which there was a specific drop in the prevalence of MSSA with an increase in MRSA. MSSA infections are still predominant in the pediatric population, but MRSA rates also present significant values, especially in community-acquired infections. Among the risk factors for CA-MRSA and HA-MRSA infections, we mainly highlight the recent use of antimicrobials in the last month and the presence of the central venous catheter as an invasive medical device in healthcare-associated infections, respectively.
Finally, our findings reinforce the need for further research to monitoring the antimicrobial resistance profile of S. aureus according to local epidemiology, to guide the best choice of empirical therapy.
Data availability
All data generated or analyzed during this study are included in this manuscript.
Abbreviations
- CA-MRSA:
-
Community-associated methicillin-resistant Staphylococcus aureus
- FIOCRUZ:
-
Fundação Oswaldo Cruz
- HA-MRSA:
-
Hospital-acquired methicillin-resistant Staphylococcus aureus
- IFF:
-
Instituto Nacional de Saúde da Mulher, da Criança e do Adolescente Fernandes Figueira
- MRSA:
-
Methicillin-resistant Staphylococcus aureus
- MSSA:
-
Methicillin-susceptible Staphylococcus aureus
- AST:
-
Antibiotic Sensitivity Test
- VISA:
-
Vancomycin-intermediately susceptible Staphylococcus aureus
- VRSA:
-
Vancomycin-resistant Staphylococcus aureus
References
Bes TM, Martins RR, Perdigão L, Mongelos D, Moreno L, Moreno A, et al. Prevalence of methicillin-resistant Staphylococcus aureus colonization in individuals from the community in the city of São Paulo, Brazil. Rev Inst Med Trop Sao Paulo. 2018;60:e58.
Loewen K, Schreiber Y, Kirlew M, Bocking N, Kelly L. Community-associated methicillin-resistant Staphylococcus aureus infection: Literature review and clinical update. Can Fam Physician. 2017;63(7):512–520. Erratum in: Can Fam Physician. 2017;63(8):596.
Crandall H, Kapusta A, Killpack J, Heyrend C, Nilsson K, Dickey M et al. Clinical and molecular epidemiology of invasive Staphylococcus aureus infection in Utah children; continued dominance of MSSA over MRSA. 2020 Plos One, 15(9), e0238991.
Agência Nacional de Vigilância Sanitária (Brasil). Nota técnica GVIMS/GGTES/DIRE3/ANVISA nº 03/2023. Critérios Diagnósticos das infecções relacionadas à assistência à saúde (IRAS) de notificação nacional obrigatória para o ano de 2023. Janeiro; 2023.
Tizotti MK, Horner R, Kempfer CB, Martini R, Mayer LE, Roehrs M, et al. Prevalência E Perfil De Sensibilidade De Staphylococcus aureus isolados em um hospital escola na cidade de Santa Maria, Brasil. Saúde (Sta Maria). 2011;36(1):47–56.
Penteado FD, Tubero TZ, Hein N, Gilio AE. Frequency of community-acquired Methicillin-resistant Staphylococcus aureus in Pediatric Population in a General Hospital in São Paulo, Brazil, over 5 years. Pediatr Infect Dis J. 2019;38(5):e87–9.
Fassbind DA, Rezende RQ, Dias CAG, Motta F. Community-acquired and healthcare-associated Staphylococcus aureus infections in a pediatric hospital in southern Brazil over 8 years: how common is MRSA? Front Pediatr. 2023;11:1212239.
Gelatti LC, Bonamigo RR, Inoue FM, do Carmo MS, Becker AP, Castrucci FMS, et al. Community-acquired methicillin-resistant Staphylococcus aureus carrying SCC mec type IV in southern Brazil. Rev Soc Bras Med Trop. 2013;46(1):34–8.
Arikan K, Karadag-Oncel E, Aycan AE, Yuksekkaya S, Sancak B, Ceyhan M. Epidemiologic and molecular characteristics of Staphylococcus aureus strains isolated from hospitalized pediatric patients. Pediatr Infect Dis J. 2020;39(11):1002–6.
Rodrigues R, Passadouro R, Gomes O, Castro R, Risk, Factors. Length of Stay and In-Hospital mortality of Methicillin-Resistant Staphylococcus aureus infections: a case-control study. Acta Med Port. 2020;33(3):174–82.
Grundmann H, Aires-de-Sousa M, Boyce J, Tiemersma E. Emergence and resurgence of meticillin-resistant Staphylococcus aureus as a public-health threat. Lancet. 2006;368(9538):874–85.
Paganini H, Della Latta M, Muller B. Estudio multicéntrico Sobre las infecciones pediátricas por Staphylococcus aureus meticilino-resistente provenientes de la comunidad en La Argentina. Arch Argent Pediatr. 2008;106(5):397–403.
Romero MC, Mas M, Giachetto G, Algorta G, Pírez MC, Cúneo A, et al. Etiología y presentación clínica de las infecciones osteoarticulares en niños hospitalizados en El Hospital Pediátrico Del Centro Hospitalario Pereira Rossell 2003–2005. Rev med Urug. 2008;24:238–45.
Sosa Ávila Luis Miguel. Machuca Pérez Mayra Alejandra, Sosa Ávila Carlos Arturo, González Rugeles Clara Isabel. Infecciones por Staphylococcus aureus meticilino resistente en niños en Bucaramanga Colombia. Rev. Univ. Ind. Santander. Salud [Internet]. 2010 Dic [citado 2024 Jul 14]; 42 (3): 248–255. Disponible en: http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S0121-08072010000300008&lng=es
American Academy of Pediatrics. Staphylococcus aureus In: Kimberlin DW, Barnett ED, Lynfield R, Sawyer MH, eds. Red Book: 2021 Report of the Committee on Infectious Diseases. Itasca, IL:American Academy of Pediatrics: 202, pages 678–692.
Acknowledgements
Not applicable.
Funding
This project had its own financing and used the infrastructure available at our Institute.
Author information
Authors and Affiliations
Contributions
The authors ILM, SMP and MVSP made substantial contributions to the conception, writing and review of the work, in addition to the analysis and interpretation of the data. Everyone approved the submitted version and agreed to be personally accountable for their contributions and to ensure that questions related to the accuracy or integrity of any part of the work are investigated, resolved, and the resolution documented in the literature.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This project was approved by the Human Research Ethics Committee of the Instituto Nacional de Saúde da Mulher, da Criança e do Adolescente Fernandes Figueira/Fiocruz, CAAE 61334922.6.0000.5269, on 10/20/2022. The study is in accordance with the ethical principles of non-maleficence, beneficence, justice and autonomy, contained in resolution 466/12 of the National Health Council and its complements (BRAZIL, 2012). The confidentiality of data and patient identification when used for scientific dissemination purposes was guaranteed.
Consent for publication
The Free and Informed Consent Form was requested from the legal guardian of the study volunteer, via telephone contact. For cases in which contact was unsuccessful, release of the term was requested from the Research Ethics Committee.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lessa de Menezes, I., Moura Pone, S. & da Silva Pone, M.V. Clinical, demographic characteristics and antimicrobial resistance profile of Staphylococcus aureus isolated in clinical samples from pediatric patients in a tertiary hospital in Rio de Janeiro: 7-year longitudinal study. BMC Infect Dis 24, 1081 (2024). https://doi.org/10.1186/s12879-024-09986-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09986-7