Abstract
Background
Retroperitoneal liposarcoma (RPLPS) is a relatively rare disease. Liposarcomas vary in size, but sizeable RPLPS larger than 30 cm in diameter are very rare, and their diagnosis and treatment present significant challenges.
Case presentation
We report a 58-year-old male patient who was admitted to the hospital with an increased abdominal circumference and was later diagnosed with a giant RPLPS. The liposarcoma was found to adhere to the right kidney and the entire ureter, invading the ascending colon. The patient underwent complete combined surgical resection. The tumor was removed intact, measured 55.0 cm × 30.0 cm × 18.0 cm, and weighed 19.8 kg. Histopathologic analysis revealed well-differentiated liposarcoma (WDLPS). The patient was successfully discharged from the hospital and followed up for 6 months with no signs of recurrence.
Conclusion
RPLPS is a rare tumor with atypical clinical presentation. Surgery remains the most effective method of treatment for retroperitoneal sarcomas, with complete removal if there is local invasion. Preoperative examination, including three-dimensional (3D) reconstruction, is essential for surgical success. The role of adjuvant radiotherapy or chemotherapy remains controversial. However, clinicians should not rule them out as viable options.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Retroperitoneal liposarcoma (RPLPS) is a rare, typically asymptomatic tumor that occurs in the retroperitoneal space [1]. It commonly occurs in patients 40–60 years old, and men and women are equally affected [2]. The retroperitoneal cavity is an ample space where the RPLPS can grow. In the clinical experience, RPLPS is usually asymptomatic in the early stages of the disease and causes symptoms when large growths occur mainly due to pressure effects on nearby structures (duodenum, ureters, kidneys, pancreas, blood vessels, or pelvic retroperitoneal organs) [3]. Giant liposarcomas, defined as those with a diameter of 30 cm or more or a weight of 20 kg or more, are extremely rare [4]. Here, we report a case of a massive RPLPS measuring 55.0 cm × 30.0 cm × 18.0 cm and weighing 19.8 kg. We also reviewed 34 cases of giant RPLPS with a more than 30 cm diameter from the PubMed database and proposed diagnostic management protocols based on our clinical experience.
Case presentation
A 55-year-old man presented with a complaint of progressive abdominal distension over the past two months, without significant abdominal pain, nausea, vomiting, constipation, dyspepsia, or dyspnea. On physical examination, abdominal obesity was noted, and a diffuse, hard, non-mobile mass with ill-defined margins was palpated in the abdominal area.
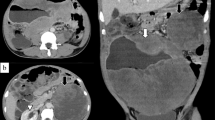
The patient underwent computed tomography urography (CTU) and abdominal magnetic resonance imaging (MRI). CTU was utilized to elucidate the relationship between the tumor and the urinary system, while MRI provided detailed visualization of the tumor boundaries, assisting surgeons in understanding the tumor’s relationship with surrounding organs, tissues, and blood vessels. The CTU scan revealed a large, fat-dense shadow on the right side of the abdominal cavity, measuring approximately 35.5 cm × 21.9 cm, extending from the sub-hepatic space to the anterior bladder (Fig. 1A). It encased the entire right kidney and compressed surrounding intestines and blood vessels (Fig. 1B). The MRI revealed a large shadow in the abdominal cavity and behind the peritoneum, enveloping the entire right kidney and pressing against the adherent surrounding intestine. The dimensions of the mass were 43.0 cm × 26.6 cm × 14.6 cm. The abdominal aorta, inferior vena cava, and bilateral renal vessels were not affected (Fig. 1C). Given the complex relationship between the mass and adjacent tissues, we performed a hyper-accuracy three-dimensional (3D) reconstruction to aid in selecting the optimal surgical approach and determining the extent of resection (Fig. 1D). A multidisciplinary team (MDT) consisting of gastrointestinal surgery, imaging, pathology, oncology, and vascular surgery was formed to treat the patient.
The MDT analyzed the relationship between the tumor and surrounding organs and blood vessels based on imaging and 3D reconstruction to evaluate the possibility of thorough surgical removal. It was observed that the lower pole of the tumor had a distinct boundary, which could serve as a starting point for gradual removal of the entire tumor. With the family’s consent, we proceeded with a comprehensive surgical resection in collaboration with the gastrointestinal surgery department. Preoperative intestinal preparation was done, and the patient’s physical tolerance was assessed. During the operation, a right subcostal margin curved incision was made, extending longitudinally along the outer margin of the right rectus abdominis muscle to the anterior superior iliac spine. Each layer of the abdominal wall was carefully incised to access the abdominal cavity. The tumor was found to involve the right kidney, the entire right ureter, the psoas muscle fascia, and part of the ascending colon. We proceeded with the removal of the primary tumor, the right kidney, and the ureter, as well as a portion of the ascending colon. The gastrointestinal tract was reconstructed by anastomosing the distal ileum to the remaining colon. The surgery was completed successfully with an estimated blood loss of 200 ml. The tumor, measuring 55.0 cm × 30.0 cm × 18.0 cm and weighing 19.8 kg, was entirely excised (Fig. 2). Postoperatively, the patient was monitored with ECG for 12 h and received supportive care, including antibiotics and fluid rehydration. The patient was encouraged to mobilize on the following day, and a liquid diet was started three days postoperatively. Postoperative pathologic analysis revealed a well-differentiated liposarcoma with a negative incisal margin (Fig. 3). The patient made an uneventful recovery and was discharged on the seventh postoperative day without complications. Follow-up at six months revealed no signs of recurrence.
This report complies with the ethical requirements of the Helsinki Declaration and was approved by the Ethics Committee of Yantai Yuhuangding Hospital, affiliated with Qingdao University, with the informed consent of the patient to publish the procedure and the case.
(A) The coronal section of the CT scan shows extension from the tumor subhepatic along the foramen to the anterior part of the bladder (white arrows). (B) The transverse section of the CT scan shows a tumor encasing the entire right kidney and compressing the surrounding intestinal canal. (C) Magnetic resonance imaging shows a tumor encasing the right kidney and squeezing the surrounding bowel. (D) 3D reconstruction: Translucent tumors reveal detailed changes in the anatomical relationship of the tumor to adjacent organs and blood vessels (Yellow: tumors, Red: arteries, Blue: veins)
Literature review
In all of the English literature in the PubMed database, only 34 cases of giant RPLPS with diameters greater than 30 cm have been reported [3, 5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37]. Of these 35 cases (including ours), 23 were male (65.7%) and 12 female (34.3%). CT is the primary imaging test used for diagnosis. In addition, 6 patients (17.1%) received preoperative fine-needle aspiration cytology (FNAC), and 1 patient (0.03%) underwent preoperative biopsy to clarify the diagnosis. Only 2 patients (0.06%) progressed to 3D reconstruction before surgery. Histopathological examinations of subtypes showed 21 well-differentiated (60.0%), 9 dedifferentiated (25.7%), 3 myxoid (8.6%), 1 myxoid pleomorphic (2.9%) and 1 mixed (2.9%). All patients underwent surgical treatment, and four of them also received adjuvant therapy. During the postoperative follow-up period, there were six cases of recurrence. Among these six patients, one died following the third postoperative recurrence, and another died after declining further surgical intervention (Table 1).
Discussion
RPLPS is the most common histological type of retroperitoneal sarcoma, accounting for approximately 20% of all adult sarcomas [38]. The 2020 World Health Organization Classification of Tumors of Soft Tissue and Bone recognizes five major liposarcoma subtypes: well-differentiated liposarcoma (WDLPS), dedifferentiated liposarcoma (DDLPS), myxoid liposarcoma (MLPS), pleomorphic liposarcoma (PLPS), and myxoid pleomorphic liposarcoma (MPLPS) [39]. The histological subtype of RPLPS is the main prognostic factor for local recurrence and distant metastasis. Among various sarcomas, the local recurrence-free survival rate (RFS) of DDLPS and PLPS was the worst, while distant metastasis was the most common in PLPS and MLPS [40]. RPLPS is potentially the largest tumor found in the human body [41]. Because the potential space of the retroperitoneum is loose and expandable without any bony boundaries, liposarcomas in this area tend to grow to huge sizes before they produce symptoms. However, RPLPS larger than 30 centimeters in diameter remain exceptionally rare. Most of these tumors are discovered incidentally as a result of abdominal distension, dyspepsia, dyspnea, or even regular abdominal examinations [18].
Surgery remains the primary treatment for RPLPS. Due to the large size of RPLPS, it easily invades other organs, tissues, and muscles in the surrounding area, adding significant difficulty to the surgery. Therefore, preoperative examination is crucial for the management of RPLPS. The diagnosis of RPLPS is commonly evaluated by abdominal computed tomography (CT) or MRI. These modalities determine the anatomical location, size, and possible origin of the tumor, the relationship of the tumor to adjacent visceral and neurovascular structures, possible compression or invasion, and the presence of trans-abdominal spread or metastasis. Liposarcoma presents characteristically on CT and MRI with a predominantly fatty component [42]. Additionally, the most common difficulty during surgery is penetrating through the tumor area to identify retroperitoneal structures and thus facilitate control of the major vessels of the resected organ. Hyper-accuracy 3D reconstruction provides more comprehensive organ information than conventional CT and MRI. It gives surgeons more detailed and macroscopic images of anatomical structures, showing close relationships between neighboring organs and vital vascular structures to select better surgical approaches and determine the extent of resection [22]. Among previously reported cases, 3D reconstruction was used in only one case, ours being the second, both with favorable results. Therefore, in addition to CT and MRI, 3D reconstruction is crucial in the preoperative examination of RPLPS. For patients with distant metastases or unresectable tumors, a histological biopsy is recommended to guide subsequent treatment decisions.
The definitive surgical treatment for RPLPS requires aggressive en bloc resection to attain microscopically negative (R0) margins. If localized invasion is confirmed, combined multiorgan resection and removal of adjacent structures, such as kidneys and intestines, surrounding fat, and muscle, are required. This approach maximizes the likelihood of R0 margins [43]. Previous studies have shown that patients undergoing extended resection have a lower rate of local recurrence than those undergoing standard resection [44, 45]. The prospective study by Lewis et al. demonstrated a median survival of 103 months for patients who underwent complete resection with apparently negative margins, compared with 18 months for patients who underwent incomplete resection [46]. Although extensive resection usually increases the risk of postoperative complications, patient complications due to combined multiorgan resection have been reported to have no substantial impact on overall survival (OS) [47]. Therefore, R0 resection should be performed whenever possible for tumors that are preoperatively assessed to be surgically resectable.
Indeed, surgical resection remains the method of choice for localized recurrent RPLPS. It often recurs 6 months to 2 years after the initial surgical resection and proliferates, with an average tumor volume doubling time of approximately 100 days [48]. Therefore, postoperative follow-up is crucial, especially in patients with a poor prognosis of the type of pathology. In case of recurrence, patients should be advised to undergo prompt surgical resection.
While complete surgical removal is the optimal treatment, some tumors cannot be excised during surgery due to distant metastases or invasion of vital organs. Therefore, in such cases, pre-surgical adjuvant therapy to intervene in tumor staging is a viable option [18]. Additionally, patients with positive surgical margins or high-grade liposarcoma also need consolidation from adjuvant therapy [49, 50]. In the case of Sarah et al., the patient was not suitable for one-stage surgical resection due to the large size of the tumor. Consequently, the patient underwent preoperative radiotherapy along with neoadjuvant therapy to downstage the tumor, followed by surgical resection [33]. The goal of chemotherapy is to alleviate tumor-related symptoms, improve quality of life, and possibly increase disease-specific survival [51]. Carboni et al. argue that chemotherapy serves as palliative care for patients with advanced or metastatic disease [52]. For unresectable or metastatic RPLPS, chemotherapy can alleviate some symptoms and partially improve quality of life. However, the therapeutic effect of chemotherapy remains controversial in clinical practice [53]. Despite this controversy, clinicians should not rule it out as viable options. For patients who cannot undergo full surgical treatment, this may be their only chance for a cure [43].
In this study, our tumor was more significant than 50 cm in diameter, which is larger than in other cases. In the vast majority of cases, only routine CT and MRI examinations were performed before surgery. Additionally, we used 3D reconstruction technology to more intuitively judge the specific condition of the tumor and aid in surgical planning. We also established an MDT team to evaluate treatment options for patients and complete tumor removal through interdisciplinary collaboration. However, our case is singular and requires more data validation before it can be generalized to a broader population. Moreover, our follow-up time was only six months, and long-term outcomes need to be further evaluated.
Conclusion
RPLPS is a rare malignant tumor with atypical clinical manifestations. R0 surgery is the first-line treatment for giant RPLPS. In the case of local invasion, it is reasonable for the MDT team to work together to remove extensive and adjacent organs to obtain a negative surgical margin. CT and MRI are practical preoperative diagnostic tools. Additionally, 3D reconstruction can more intuitively display the relationship between the tumor and nearby tissue anatomical structures, which is conducive to formulating a surgical plan. Therefore, when the tumor is large and invading surrounding organs and tissues, 3D reconstruction is a viable option. Surgical resection also remains the first option for postoperative local recurrence of liposarcoma. For metastatic or non-operable resectable tumors, radiotherapy and neoadjuvant therapy can be rationally selected.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- RPLPS:
-
Retroperitoneal liposarcomas
- US:
-
Ultrasound
- CTU:
-
Computed tomography urography
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- 3D reconstruction:
-
Three-dimensional reconstruction
- MDT:
-
Multidisciplinary team
- WDLPS:
-
Well-differentiated liposarcoma
- DDLPS:
-
Dedifferentiated liposarcoma
- MLPS:
-
Myxoid liposarcoma
- PLPS:
-
Pleomorphic liposarcoma
- MPLPS:
-
Myxoid pleomorphic liposarcoma
- M:
-
Male
- F:
-
Female
- FNAC:
-
Fine needle aspiration cytology
- AIM:
-
Ifosfamide, Mesna, and doxorubicin
References
Leao P, Vilaca S, Oliveira M, Falcao J. Giant recurrent retroperitoneal liposarcoma initially presenting as inguinal hernia: review of literature. Int J Surg Case Rep. 2012;3:103–6.
Hashimoto Y, Hatakeyama S, Tachiwada T, Yoneyama T, Koie T, Kamimura N, Yanagisawa T, Hakamada K, Ohyama C. Surgical treatment of a giant liposarcoma in a Japanese man. Adv Urol. 2010;2010:943073.
Mansour S, Azzam N, Kluger Y, Khuri S. Retroperitoneal liposarcoma: the giant type. J Med Cases. 2022;13(10):517–20.
Makni A, Triki A, Fetirich F, Ksantini R, Chebbi F, Jouini M, Kacem M, et al. Giant retroperitoneal liposarcoma. Report of 5 cases. Ann Ital Chir. 2012;83(2):161–6.
Yol S, Tavli S, Tavli L, et al. Retroperitoneal and scrotal giant liposarcoma: report of a case. Surg Today. 1998;28:339–42.
McCallum OJ, Burke JJ, Childs AJ, et al. Retroperitoneal liposarcoma weighing over one hundred pounds with review of the literature. Gynecol Oncol. 2006;103:1152–4.
Clar H, Leithner A, Gruber G, et al. Interdisciplinary resection of a giant retroperitoneal liposarcoma of 25 kg. ANZ J Surg. 2009;79:957.
Hashimoto Y, Hatakeyama S, Tachiwada T et al. Surgical treatment of a giant liposarcoma in a Japanese man. Adv Urol. 2010; 2010:943073.
Bansal VK, Misra MC, Sharma A, et al. Giant retroperitoneal liposarcoma - renal salvage by autotransplantation. Indian J Surg. 2013;75:159–61.
De Nardi P, Bissolati M, Cristallo M, et al. Recurrent giant liposarcoma of the spermatic cord. Urology. 2012;79:113–4.
Sharma M, Mannan R, Bhasin TS, et al. Giant inflammatory variant of well differentiated liposarcoma: a case report of a rare entity. J Clin Diagn Res. 2013;7:1720–1.
Zhang WD, Liu DR, Que RS, et al. Management of retroperitoneal liposarcoma: a case report and review of the literature. Oncol Lett. 2015;10:405–9.
Caizzone A, Saladino E, Fleres F, et al. Giant retroperitoneal liposarcoma: case report and review of the literature. Int J Surg Case Rep. 2015;9:23–6.
Hazen B, Cocieru A. Giant Retroperitoneal Sarcoma. J Gastrointest Surg. 2017;21:602–3.
Oh SD, Oh SJ, Suh BJ, et al. A Giant Retroperitoneal Liposarcoma encasing the entire left kidney and adherent to adjacent structures: a Case Report. Case Rep Oncol. 2016;9:368–72.
Zeng X, Liu W, Wu X, et al. Clinicopathological characteristics and experience in the treatment of giant retroperitoneal liposarcoma: a case report and review of the literature. Cancer Biol Ther. 2017;18:660–5.
Herzberg J, Niehaus K, Holl-Ulrich K, et al. Giant retroperitoneal liposarcoma: a case report and literature review. J Taibah Univ Med Sci. 2019;14:466–71.
Xu C, Ma Z, Zhang H, Yu J, Chen S. Giant retroperitoneal liposarcoma with a maximum diameter of 37 cm: a case report and review of literature. Ann Transl Med. 2020;8(19):1248.
Spicer JL. Retroperitoneal liposarcoma: an unusual presentation of a Rare Cancer. J Adv Pract Oncol. 2021;12(8):854–62.
Herrera-Almario G, Cabrera LF, Londoño-Schimmer EE, Pedraza M. Giant retroperitoneal liposarcoma surgical management. Ann R Coll Surg Engl. 2022;104(2):54–6.
Suryabanshi A, Timilsina B, Khadka N, Rijal A, Bhandari RS. Huge retroperitoneal liposarcoma encasing right kidney: a case report from Nepal. Int J Surg Case Rep. 2022;99:107647.
Ye MS, Wu HK, Qin XZ, Luo F, Li Z. Hyper-accuracy three-dimensional reconstruction as a tool for better planning of retroperitoneal liposarcoma resection: a case report. World J Clin Cases. 2022;10(1):268–74.
Xia H, Fang F, Yuan H, Tu Y. Survival of a patient with multiple-recurrent giant retroperitoneal dedifferentiated liposarcoma for 15 years: a case report. Front Surg. 2022;9:916802.
Liu T, Zhang J, Xu Z, Zhou H. Abdominal viscera and gone? A rare case of giant retroperitoneal liposarcoma. Asian J Surg. 2022;45(12):2963–4.
Lieto E, Cardella F, Erario S, Del Sorbo G, Reginelli A, Galizia G, Urraro F, Panarese I, Auricchio A. Giant retroperitoneal liposarcoma treated with radical conservative surgery: a case report and review of literature. World J Clin Cases. 2022;10(19):6636–46.
Trajkovski G, Antovic S, Kostovski O, Trajkovska V, Nikolovski A. Giant retroperitoneal low grade liposarcoma with left kidney displacement: a case report. Radiol Case Rep. 2022;17(11):4091–5.
Evola G, Schillaci R, Reina M, Caruso G, D’Angelo M, Reina GA. Giant retroperitoneal well-differentiated liposarcoma presenting in emergency with intestinal occlusion: case report and review of the literature. Int J Surg Case Rep. 2022;95:107152.
Wei X, Qin Y, Ouyang S, Qian J, Tu S, Yao J. Challenging surgical treatment of giant retroperitoneal liposarcoma: a case report. Oncol Lett. 2022;24(3):314.
Rachman Y, Hardja Y. Giant retroperitoneal liposarcoma: a case report. Int J Surg Case Rep. 2022;97:107465.
Tani A, Tarumi Y, Kakibuchi A, Aoyama K, Kokabu T, Kataoka H, Yoriki K, Nagamine M, Mori T. Giant retroperitoneal dedifferentiated liposarcoma mimicking ovarian cancer: a case report. Gynecol Oncol Rep. 2022;44:101088.
Chen BH, Tseng JS, Chiu AW. Increasing body weight of 20 kg in 3 months caused by a huge retroperitoneal liposarcoma. Asian J Surg. 2022;45(11):2490–1.
Luke ND, Gart A, Mohammad R, Raza A, Liposarcoma. A ‘Beer Belly’ in disguise. Cureus. 2022;14(8):e28067.
Cheng SH, Huang YS, Lee HH, Yen HH, Jhong YP, Chao TY. Case report and literature review: Conversion surgery for initially unresectable huge retroperitoneal liposarcoma after preoperative radiotherapy. Front Oncol. 2023;12:1096411.
Habonimana P, Niyonkuru E, Nisabwe S, Mazti A, Moataz A, Dakir M, Debbagh A, Aboutaieb R. A large dedifferentiated retroperitoneal liposarcoma extended to the testis: a rare case report. J Surg Case Rep. 2023;2023(5):rjad162.
Gutu C, Butnari V, Schiopu V. Giant retroperitoneal liposarcoma measuring 27 × 29 × 36 cm: a case report. J Surg Case Rep. 2023; 2023(1):rjac608.
Tripathi M, Pavithira GJ, Dubey S, Verma R, Garg V. Surgical excision of a giant retroperitoneal liposarcoma with renal cell carcinoma: a case report of the largest retroperitoneal sarcoma. Int J Surg Case Rep. 2023;109:108515.
Díaz de León-Romero CE, Jiménez-Yarza M, Pérez-Tristán CE, Jiménez-Yarza LE, Valdes-Ramos RL, Ortiz-Cisneros JD. Giant myxoid retroperitoneal liposarcoma in a 41-year-old patient: a case report. Int J Surg Case Rep. 2023;109:108572.
Horowitz J, Singhal M, Marrero D, et al. A multi-modality treatment of retroperitoneal dediferentiated liposarcoma. Am J Case Rep. 2020;21:e919245.
WHO Classifcation of Tumours Editorial Board. WHO classifcation of tumours of soft tissue and bone. 5th ed. Lyon: IARC; 2020.
Vos M, Koseła-Paterczyk H, Rutkowski P, et al. Differences in recurrence and survival of extremity liposarcoma subtypes. Eur J Surg Oncol. 2018;44:1391–7.
Liles JS, Tzeng CWD, Short JJ, et al. Retroperitoneal and intra-abdominal sarcoma. Curr Probl Surg. 2009;46:445–503.
Matthyssens LE, Creytens D, Ceelen WP. Retroperitoneal liposarcoma: current insights in diagnosis and treatment. Front Surg. 2015;2:4.
Liao T, Du W, Li X, He S, Guan G, Zhu H, Wu J. Recurrent metastatic retroperitoneal dedifferentiated liposarcoma: a case report and literature review. BMC Urol. 2023;23(1):63.
Bonvalot S, Rivoire M, Castaing M, et al. Primary retroperitoneal sarcomas: a multivariate analysis of surgical factors associated with local control. J Clin Oncol. 2009;27:31–7.
Gronchi A, Miceli R, Colombo C, et al. Frontline extended surgery is associated with improved survival in retroperitoneal low- to intermediategrade soft tissue sarcomas. Ann Oncol. 2012;23:1067–73.
Lewis JJ, Leung D, Woodruff JM, et al. Retroperitoneal soft tissue sarcoma: analysis of 500 patients treated and followed at a single institution. Ann Surg. 1998;228:355–65.
Bonvalot S, Miceli R, Berselli M, et al. Aggressive surgery in retroperitoneal soft tissue sarcoma carried out at high-volume centers is safe and is associated with improved local control. Ann Surg Oncol. 2010;17:1507–14.
Tseng WW, Madewell JE, Wei W, Somaiah N, Lazar AJ, Ghadimi MP, Hoffman A, Pisters PW, Lev DC, Pollock RE. Locoregional disease patterns in well-differentiated and dedifferentiated retroperitoneal liposarcoma: implications for extent of resection? Ann Surg Oncol. 2014;21(7):2136–43.
Lahat G, Tuvin D, Wei C, et al. New perspectives for staging and prognosis in soft tissue sarcoma. Ann Surg Oncol. 2008;15:2739–48.
Le Péchoux C, Musat E, Baey C, et al. Should adjuvant radiotherapy be administered in addition to front line aggressive surgery (FAS) in patients with primary retroperitoneal sarcoma? Ann Oncol. 2013;24:832–7.
Saponara M, Stacchiotti S, Gronchi A. Pharmacological therapies for Liposarcoma. Expert Rev Clin Pharmacol. 2017;10(4):361–77.
Carboni F, Valle M, Federici O, et al. Giant prim retroperitoneal dediferentiated liposarcoma. J Gastrointest Surg. 2019;23:1521–3.
Luo P, Cai W, Yang L, et al. Retroperitoneal dediferentiated liposarcoma: analysis of 61 cases from a large institution. J Cancer. 2018;9:3831–8.
Acknowledgements
Not applicable.
Funding
This article was supported by grants from the National Natural Science Foundation of China (No. 81972376), Taishan Scholars Program of Shandong Province (No. tsqn202211379) and Major Science and Technology Project of Shandong Antibody Drug Innovation and Entrepreneurship Community in 2023.
Author information
Authors and Affiliations
Contributions
JNS and RY drafted the manuscript. HWZ operated on the patient. XLJ and FZ collected the material. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Yuhuangding Hospital Ethics Committee. Written informed consent was obtained by the participants.
Consent for publication
Informed consent for publication was obtained from the participants.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sun, JN., Yang, R., Jiang, XL. et al. Giant retroperitoneal liposarcoma with multiple organ involvement: a case report and literature review. BMC Nephrol 25, 281 (2024). https://doi.org/10.1186/s12882-024-03701-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12882-024-03701-z