Abstract
Background
Uncontrolled gout can cause articular impairment but is also associated with a global and cardiovascular excess mortality, especially in dialysis population.
Data documented within existing research is not conclusive regarding gout flares evolution during hemodialysis and their control by urate lowering therapy (ULT).
Without clear guidelines concerning hemodialysis patients management with chronic gout, this study proposes to investigate whether gout flare incidence reduction could be observed on this population treated by urate lowering therapy versus patients without treatment.
Methods
We performed a retrospective cohort study in two hemodialysis centers in France. Were selected patients over 18 years old with a gout history who started hemodialysis between January 2005 and September 2015.
Demographics and clinicals data were recorded at hemodialysis start and throughout 5 years of follow up. Gout flare was defined as presence of uric acid crystal in joint punction or clinically diagnosed as such with a colchicine prescription.
All statistical analysis were performed in SAS® version 9.4 (SAS Institute Inc., Cary, NC).
Results
One hundred eighty-one patients have been included, mean age at dialysis initiation was 68.6 years (± 12.4) with 72% of men, 54% were treated by ULT: 89.7% by allopurinol and 9.3% by febuxostat. One patient received both treatments successively. After hemodialysis initiation, 35.36% patients had experienced at least one gout flare. The appearance of at least one gout flare concerned 50% of patients in no ULT group and 22.68% patients in ULT group (p = 0.0002).
Dialysis efficiency was measured at regular interval during follow-up and was similar in both groups.
To study the association strength between clinical factors and gout flares occurrences, a Cox model was performed; ULT is a protector factor of gout flare (HR:0,42, CI 95: 0,25-0,71).
The proportion of serum urate values within the target (median 53% vs 29.3%, p < 0.0001) was significantly higher in ULT group versus no ULT group (median 53% vs 29.3%, p < 0.0001).
Conclusion
Urate lowering therapy limit new gout flares occurrence in hemodialysis patients with gout historyCollaboration between rheumatologists and nephrologists may help to update guidelines for urate-lowering therapies in patients on dialysis.
Similar content being viewed by others
Introduction
Patients with chronic kidney disease (CKD) are at greater risk of developing gout flares due to a reduction of uric acid renal clearance [1]. It is known in the literature that the decrease of renal function generates a state of hyperuricemia, also a vector of urate nephropathy aggravating gouty pathology [2].
Data resulting of current research are contradictory on the evolution of gout flares during hemodialysis leading to the perception that hemodialysis alone would achieve extra-renal purification of uric acid without requiring urate lowering therapy (ULT) [3,4,5].
However, several studies have proven the persistence of gout flares in hemodialysis patients: a 2020 US study show that the incidence of active gout was 15.4% in the first five years [6]. Nevertheless, preliminary data suggests that the incidence of gout in patients with end-stage renal disease (ESRD) may be low, perhaps secondary to clearance of inflammatory mediators on hemodialysis [3].
It has also been shown that pharmacological management of gout in patients with chronic kidney disease is still suboptimal and subject of difficulties in clinical practice [7]. The use of ULT remains controversial, although most of clinical studies main criteria are based on reaching a target value of serum uric acid [8, 9].
Without clear guidelines regarding the management of hemodialysis patients, the purpose of this study was to investigate whether gout flare incidence was reduced on this population treated with urate lowering therapy.
Materials and methods
Data source and patient selection
We performed a retrospective cohort study on two hemodialysis centers in France: in the nephrology unit of Reims University Hospital and in the hemodialysis unit of Local Association for Home dialysis promotion in Reims.
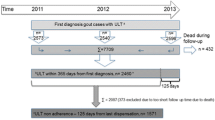
We selected patients over 18 years old with a gout history and started hemodialysis between January 2005 and September 2015. Once hemodialysis started, patients should have been monitored through a minimum six months follow-up in the nephrology centers.
Patients’ selection was performed using a medical software “Hemadialyse®” containing medical records from both centers. Specific queries were performed using this software retaining the following criteria: “hemodialysis initiation between 01/01/2005 and 09/01/2015” AND “gout history (CIM-10 code M10.3)” OR “treatment by colchicine OR Colchimax® OR Allopurinol OR Zyloric ® OR Febuxostat OR Adenuric ®». The same query was addressed to Reims University hospital’s Medical Informations Department (MID). After removing duplicates, each medical file was analyzed.
All the patients were included with the agreement of the National Commission for Informatics and Freedoms. According to the French legislation, no ethics committee approval was required for such a retrospective study.
Variables of interest
Demographics and epidemiological data selected was comprised of: age, sex, ethnical origin, BMI, nephropathy type, hemodialysis initiations date, comorbidities through Charlson comorbidity index, cardiovascular comorbidities (history of hypertension, dyslipidemia and cardiopathy without cardiac failure).
We monitored through a five-year period each gout flares since hemodialysis initiation for all patients included in the study. The period was shortened in case of decease, dialysis center and/or technic change (peritoneal dialysis) or renal transplantation before the five years of follow-up.
Gout flares was defined as presence of sodium urate crystal in articular fluid after punction or medical gout flares diagnostic with colchicine prescription associated. We recorded number and the dates of each flare for each patient.
Hemodialysis efficiency was evaluated by recording urea reduction ratio (URR) three times a year and KT/V ratio only during each gout flare occurrences. Similarly, serum urate levels have been recorded for each patient three times a year during follow-up at fixed intervals. All patients underwent hemodialysis sessions three times a week.
The ULT prescription such as allopurinol or febuxostat, as well as their dosages and prescription duration were identified. Patients were considered as long-term ULT exposures when they were on ULT for more than 6 weeks following hemodialysis initiation.
We registered use and duration of hyperuricemic treatments such as angiotensin—converting enzyme inhibitors, angiotensin II receptor blockers, diuretics and platelet antiaggregants. Exposition to urate lowering therapy was analyzed by their type, duration and dosage.
Statistical analysis
Depending on tests validity conditions, descriptive analyses were performed using Fischer’s test and/or Chi-squared test Student t-test or Mann-Whitney test have been used for quantitative data. Bilateral analysis has been performed for each test with significative p-value < 0.05.
Kaplan-Meier curve have been conducted to assess gout flares and a Cox proportional hazards regression to study their association with clinicals factors. For each patient, we have calculated percent of serum urate level inferior of 360 µmol/L and a Mann-Whitney U test has been performed to compare these values between patients with and without long term urate lowering therapy.
All statistical analyses were performed in SAS® version 9.4 (SAS Institute Inc., Cary, NC).
Results
Patients’ characteristics
One hundred eighty-one gouty patients have started hemodialysis between 2005 and 2015 and met study eligibility criteria. Within observation period, 97 patients (54%) were treated by long-term ULT (allopurinol or febuxostat) and 84 (46%) had no ULT after initiating hemodialysis.
In the no ULT group, 14/84 (17%) patients had a history of treatment by ULT: 13 were treated by allopurinol and one by adenuric. ULT were stopped for all patients before the hemodialysis beginning.
Figure 1 shows patient flow chart and exclusion criteria.
Patients’ characteristics at baseline are shown in Table 1.
The mean age of the population was 68.6 years (± 12.4 years). Patients treated with ULT were more often men (81.4% vs 63.1%; p = 0.007) and had a significantly higher BMI (27.87 kg/m2 vs 25.24 kg/m2; p = 0.005).
Patients from ULT and no ULT groups were similar regarding the initial nephropathy; these were mainly hypertensive, diabetic or mixed etiologies. Furthermore, there were no differences for cardiovascular comorbidities or for Charlson comorbidity index. There were no significant differences concerning treatment influencing serum urate level except for Angiotensin II receptor blockers: 13.4% of patients in no ULT group versus 30.9% in ULT group (p = 0.004).
In the ULT group, 87/97 patients (89.7%) received Allopurinol and 9/97 patients (9.3%) were treated with Febuxostat. One patient received both treatments successively. Allopurinol daily dose was 100 mg for 77 patients: 200 mg for 10 patients and 300 mg for two patients. Febuxostat daily dose was 80 mg for eight patients and 120 mg for one patient. The patient who received both was successively treated by Allopurinol 100 mg then Febuxostat 80 mg.
Survival analysis of gout flares occurrence
Survival analysis was performed to compare gout flares occurrence between groups (Fig. 2). Hemodialysis patients who received ULT had significantly fewer gout flares compared to the group without ULT (p = 0.0009).
After hemodialysis initiation, 35.36% patients (64/181) had experienced at least one gout flare. The appearance of at least one gout flare concerned 50% of patients (42/84) in no ULT group and 22.68% patients (22/97) in ULT group (p = 0.0002). Repartition of gout flare through the five years of follow-up is described in Table 2.
Dialysis efficiency was measured at regular interval during follow-up and was similar in both groups: 80% of ULT group patients had URR > 60% versus 85% of no ULT group patients (p = 0.457). Among patients who had at least one gout flare, the mean number of gout flares was 1.27 (± 0.63) in ULT group with an average KT/V at the time of the gout flares of 0.91 (± 0.26) and 1.16 (± 0.38) in no ULT group with an average KT/V at the time of gout flares of 1.1 (± 0.21).
KT/V comparison between patients who experience at least one gout flare during follow-up versus those who did not in ULT group were similar (p = 0.7). Same results were found in the no ULT group (p = 0.355).
Factors associated with gout flare
To study the strength of association between clinicals factors and gout flares occurrences, a Cox model has been performed (Fig. 3). ULT is a protector factor of gout flare (HR:0,42, CI 95: 0,25-0,71). By using propensity score weighting, ULT decrease significantly gout flares occurrences (HR: 0,423, CI95: 0,235-0,762).
Serum urate level variation analysis
To analyze serum urate level variation on this population, 1691 serum values from 177/181 patients were collected with a median number of values of nine (2-15) per patient. The median number of values collected per patient was the same in both groups.
For each patient, the percentage of serum urate values under 360 μmol/L, the target value, was calculated.
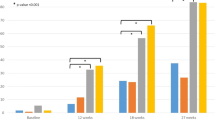
Groups of patients were performed according to the mean percentage of serum uric acid values under 360 μmol/L (Fig. 4).
Patients were grouped according to the mean percentage of serum uric acid values below 360 μmol/L as such: ≤ 25%, 26–50%, 51–75% and 76–100%.
Thirty-one % of patients had less than 25% of serum urate measurements within target and 23% of patients had serum urate within target on 76–100% of measurements (Fig. 5A). There was a significant difference between patients treated with and without urate-lowering agents after distribution by range of percentages of serum urate values below 360 μmol/L (p = 0.0003) (Fig. 5B). Forty-seven % of patients not treated with ULT had less than 25% of values below 360 μmol/L while 18% of patients treated with urate-lowering agents had less than 25% of values below 360 μmol/L. Furthermore, 29% of patients treated with ULT had more than 75% of values below 360 μmol/L, while 15% of patients without ULT had more than 75% of values below 360 μmol/L.
The proportion of serum urate values within the target (median 53% vs 29.3%, p < 0.0001) was significantly higher in ULT group compared to no ULT group.
Discussion
We had hypothesized that hemodialysis was not sufficient to control clinical gout. To our knowledge, it is the first real-life cohort study with selective criteria showing the positive effect of urate lowering therapy on gout flares in patients starting hemodialysis.
Regarding gout clinical aspect, there are only few published studies: in a large German analysis of 601 patients from five dialysis centers, the incidence of gout flares in hemodialysis patients was only 3.6% versus 13.5% in a US dialysis cohort patients [5, 10]. However, in our study, gout flares affected a third of the patients within five years after the start of dialysis, provided that our population corresponded to patients with a history of gout flares before the start of dialysis.
Another study evaluated 216 patients on hemodialysis and peritoneal dialysis, almost 25% of whom experienced gout, suggesting that hemodialysis alone is insufficient [8].
Yeo and al, showed that among adults treated with long-term dialysis, a minority have serum urate level at a target sufficient to prevent gout [8]. Forty-six percent of participants had a rate of less than 360 μmol/L on less than 25% of measurements. However, it was a cross-sectional retrospective study with no clinical data on long term for their population. In our study, its concerns 47% of hemodialysis patients in the no ULT group with five years data.
Most studies have assessed the effect of urate lowering therapy on serum urate level in hemodialysis patients [9, 11,12,13]. In our study, patients with ULT had a significant higher percentage of serum urate values within the target (< 360 μmol/L) than patients without ULT. Difference concerning rate of target serum urate values does not seem to be linked to a difference in dialysis efficiency between the two groups. We collected parameters evaluating the effectiveness of dialysis such as URR, which was comparable between the two groups. However, analysis did not take into account parameters evaluating long term effectiveness of dialysis by KT/V. These parameters were not collected and analyzed in this study due to the multitude of data that their collection would generate and because of their great variability over time. At the time of gout flares occurrences, the mean KT/V ratio seemed lower in patients on ULT while they had significantly fewer gout flares compared to the group without treatment. Thus, gout flares occurrences were less frequent despite dialysis appearing less effective at the time of gout flares in patients on ULT.
In literature, there are currently only case reports regarding the effectiveness of these treatments on gout flares in hemodialysis patients. Most studies focus on the influence of allopurinol or febuxostat on serum urate level in hemodialysis patients. A retrospective study carried out in New Zealand found a percentage of serum urate values was within the target below 360 μmol/L which is not different between groups treated or not with Allopurinol in patients on hemodialysis and on peritoneal dialysis [8]. This study included smaller numbers and the two extra-renal purification techniques, which could explain the differences observed with our results. In addition, in our study, serum urate values were recorded reproducibly and over the entire duration of follow-up.
With respect to febuxostat, a prospective Japanese placebo-controlled study analyzed its effect on serum urate level in 57 hemodialysis patients and found a significant decrease after two months of treatment in the Febuxostat group and not in the placebo group [13]. These results are consistent with our results.
Regarding urate lowering therapy efficiency on gout flares, there are only a few case reports showing the efficiency of the treatment for patients suffering from severe gout [14,15,16].
Our study confirms these results and that urate lowering therapy should be considered for patient with a history of gout starting dialysis. There are no sufficient tolerance studies of allopurinol or febuxostat in patients undergoing dialysis. Only four reports exists on the use of Febuxostat or Allopurinol in patients on hemodialysis, each showing these treatments as well-tolerated in gout patients undergoing dialysis [17,18,19,20]. No safety data has been collected in our study.
This retrospective and observational study has some limitations. Our data come from a single site, which may affect generalizability. Our inclusion criteria may have missed some eligible subjects, and we did not include patients on peritoneal dialysis. We identified gout flares but excluded corticosteroid intake, although we checked the absence of gout flares during corticoid intake.
In conclusion, when considering gout patients starting hemodialysis, urate lowering therapy limited the occurrence of new gout flares compared to patients not treated. To our knowledge, this is the first study analyzing long term effect of urate lowering therapy in hemodialysis patients on gout flares.
Results from this analysis may have implications in managing dialysis patients with history of gout. Further research on this topic and collaboration between rheumatologists and nephrologists may help to inform updated guidelines specifically for urate-lowering therapy in patients on dialysis.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- BMI:
-
Body Mass Index
- CKD:
-
Chronic Kidney Disease
- ESRD:
-
End Stage Renal Disease
- ULT:
-
Urate Lowering Therapy
- URR:
-
Urea Reduction Ratio
References
Wang W, Bhole VM, Krishnan E. Chronic kidney disease as a risk factor for incident gout among men and women: retrospective cohort study using data from the Framingham Heart Study. BMJ Open. 2015;5(4):e006843.
Mei Y, Dong B, Geng Z, Xu L. Excess uric acid induces gouty nephropathy through crystal formation: a review of recent insights. Front Endocrinol (Lausanne). 2022;13:911968.
Ohno I, Ichida K, Okabe H, Hikita M, Uetake D, Kimura H, et al. Frequency of gouty arthritis in patients with end-stage renal disease in Japan. Intern Med. 2005;44(7):706–9.
Andrés M, Soriano R, Oliveira E, Trigo C, Arenas M, Pascual E. THU0406 Serum uric acid lowering treatment appears unnecessary during hemodialysis. In: Poster Presentations. BMJ Publishing Group Ltd and European League Against Rheumatism; 2017. p. 361.1-361. Disponible sur: https://ard.bmj.com/lookup/doi/10.1136/annrheumdis-2017-eular.2392. Cité 5 juill 2023.
Zhang Y, Kshirsagar O, Marder BA, Cohen AR, LaMoreaux B, Bleyer AJ. Gout among patients with dialysis: prevalence, associated factors, treatment patterns, and outcomes-population-based retrospective cohort study. Kidney360. 2023;4(2):177–87.
Cohen SD, Kimmel PL, Neff R, Agodoa L, Abbott KC. Association of incident gout and mortality in dialysis patients. J Am Soc Nephrol. 2008;19(11):2204–10.
Jing J, Kielstein JT, Schultheiss UT, Sitter T, Titze SI, Schaeffner ES, et al. Prevalence and correlates of gout in a large cohort of patients with chronic kidney disease: the German Chronic Kidney Disease (GCKD) study. Nephrol Dial Transplant. 2015;30(4):613–21.
Yeo E, Palmer SC, Chapman PT, Frampton C, Stamp LK. Serum urate levels and therapy in adults treated with long-term dialysis: a retrospective cross-sectional study. Intern Med J. 2019;49(7):838–42.
Kang SH, Kim BY, Son EJ, Kim GO, Do JY. Comparison between the Effects of Allopurinol and Febuxostat on the Survival of Patients on Maintenance Hemodialysis. Am J Nephrol. 2023;54(3–4):117–25.
Rohn B, Jansing W, Seibert FS, Pfab T, Cinkilic O, Paßfall J, et al. Association of hyperuricemia and serum uric acid lowering therapy with mortality in hemodialysis patients. Ren Fail. 2020;42(1):1067–75.
Rutherford E, Stewart G, Houston JG, Jardine AG, Mark PB, Struthers AD. An open-label dose-finding study of allopurinol to target defined reduction in urate levels in hemodialysis patients. J Clin Pharmacol. 2017;57(11):1409–14.
Mitsuboshi S, Yamada H, Nagai K, Okajima H. Switching from allopurinol to febuxostat: efficacy and tolerability in hemodialysis patients. J Pharm Health Care Sci. 2015;1:28.
Horikoshi R, Akimoto T, Inoue M, Morishita Y, Kusano E. Febuxostat for hyperuricemia: experience with patients on chronic hemodialysis treatment. Clin Exp Nephrol. 2013;17(1):149–50.
Day RO, Kannangara DRW, Hayes JM, Furlong TJ. Successful use of allopurinol in a patient on dialysis. BMJ Case Rep. 2012;2012:bcr0220125814.
Amine HM. Tophi as the initial manifestation of gout in a normouricemic hemodialysis patient: an unusual case of a common disorder. Saudi J Kidney Dis Transpl. 2017;28(1):194–5.
Frassetto LA, Gibson S. Febuxostat and increased dialysis as a treatment for severe tophaceous gout in a hemodialysis patient. Case Rep Nephrol. 2016;2016:9106935.
Choi SY, Choi SW, Lee S, So MW, Oh JS, Lim DH. Efficacy and tolerability of febuxostat in gout patients on dialysis. Intern Med J mars. 2021;51(3):348–54.
Hayes CP, Metz EN, Robinson RR, Rundles RW. The use of allopurinol (HPP) to control hyperuricemia in patients on chronic intermittent hemodialysis. Trans Am Soc Artif Intern Organs. 1965;11:247–54.
Johnson WJ, O’Duffy JD. Chronic gouty nephropathy treated by long-term hemodialysis and allopurinol. Mayo Clin Proc. 1979;54(9):618–20.
Ma J, Huang J, Bao S, Zhang A, Dai L, Yu Q, et al. The safety and urate-lowering efficacy of febuxostat in patients undergoing peritoneal dialysis: a retrospective single-arm cohort study of 84 patients. Ann Palliat Med. 2022;11(7):2443–50.
Acknowledgements
Not applicable.
Author information
Authors and Affiliations
Contributions
A.S.: conceptualization, data curation, formal analysis, investigation, methodology, software, original draft, and writing A.H.: conceptualization, data curation, formal analysis, investigation, methodology, project administration, supervision, validation, writing L.K.: data curation, methodology, formal analysis I.K.: data curation, methodology, resources, software, validation P.C.: data curation, methodology, resources, validation, L.B.: formal analysis, methodology, supervision, validation, writing P.R.: conceptualization, data curation, formal analysis, methodology, project administration, resources, software, supervision, validation, visualization, JH.S.: conceptualization, data curation, formal analysis, investigation, methodology, project administration, resources, supervision, validation, visualization, writing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
According to current French law for non-interventional retrospective studies, no ethical approval or consent to participate was required.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Steelandt, A., Hittinger, A., Kanagaratnam, L. et al. Urate lowering therapy in patients starting hemodialysis limit gout flares occurrence: ten years retrospective study. BMC Nephrol 25, 266 (2024). https://doi.org/10.1186/s12882-024-03712-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12882-024-03712-w