Abstract
Nocardia is widely distributed in the natural environment and typically cause opportunistic infections. However, it is important to note that the pathogenicity of different Nocardia species may vary significantly. Here we reported the first case of brain abscess caused by Nocardia beijingensis (N. beijingensis) infection in China. A 70-year-old male immunocompetent individual came to our hospital for treatment due to headache. After examination, it was found that he had a brain abscess caused by N. beijingensis. By utilizing a combination of surgical intervention and antibiotic therapy, the patient ultimately achieved full recovery. In addition, we isolated this strain and displayed its ultrastructure through scanning electron microscopy. The phylogenetic tree was analyzed by 16 S rRNA sequence. A literature review of N. beijingensis infections in all immunocompetent and immunocompromised patients was presented. It highlighted that abscess formation appears to be a common manifestation of N. beijingensis infection, and N. beijingensis has become an emerging pathogen in immunocompetent individuals.
Similar content being viewed by others
Introduction
Brain abscess is characterized as inflammatory lesions, and it is usually caused by pathogens encrust pus on the central nervous system [1, 2], with a mortality rate of approximately 50–55% [3, 4]. In all intracranial space-occupying lesions, the proportion of brain abscesses is nearly 1–2% in developed countries and about 8% in developing countries [4]. According to a survey in northern Europe, the incidence of brain abscesses is 9 cases per million people every year, and it has been rising continuously in recent years [5]. Although Nocardia brain abscess is uncommon and estimated about 1–2% of all intracranial space-occupying lesions, it has the highest mortality rates of all bacterial brain abscesses, which has gradually raised widespread concern [6].
Brain abscess caused by Nocardia infection is characterized by cerebritis and central focal necrosis. Nocardia are aerobic actinomycetes ubiquitous in water and soil, which can cause local or disseminated infections primarily affecting immunocompromised patients such as AIDS, malignant neoplasms, hematopoietic stem cells or organ transplantation, diabetes, COPD, flora imbalance, chronic kidney disease, trauma [7]. To date, nearly 92 Nocardia species have been identified, of which 54 have been identified as clinically significant pathogens [8,9,10].
Nocardia beijingensis (N. beijingensis) was initially isolated from sewage ditch soil in Beijing, the capital of China in 2001 by Wang et al. and was first reported as a human pathogenic pathogen primarily affecting immunocompromised patients in Thailand and Japan in 2004 [11, 12]. Here we reported the first case of brain abscess caused by N. beijingensis infection in China, which could raise the awareness of disseminated nocardiosis in immunocompetent individuals.
Case presentation
Clinical feature
A 70s male patient presented intermittent bilateral frontal headaches, swelling, fatigue, and unsteady gait, without any apparent causes 10 days ago. He had previously sought medical attention at a local hospital where a cranial Computed Tomography (CT) scan revealed extensive areas of low density in the left hemisphere of the cerebellum, as well as old lacunar infarcts in both basal ganglia and periventricular regions. Enhanced Magnetic Resonance Imaging (MRI) suggested a nodular lesion in the left cerebellar hemisphere, raising suspicion of a tumor with associated hemorrhage. The patient received treatment for a period of time but the efficacy was not good, so he came to our hospital for further treatment. Reviewing the medical records, a personal history of cerebral infarction was noted, without any other underlying conditions or medication use. After admission, the patient underwent a physical examination, with a body temperature of 36.8 ℃, blood pressure of 118/78 mmHg, clear consciousness, soft mind, and fluent language. Bilateral pupils were equally large and round, with a left to right ratio of 2.5:2.5 mm. He was sensitive to light reflection and had normal eye movements. Bilateral facial patterns were symmetrical, and the facial sensation was symmetrical on both sides. The pharyngeal reflex existed. The muscle strength of the limbs was at level V, with normal muscle tone and normal tendon reflexes. The superficial sensation of the limbs was symmetrical on both sides, and the deep sensation was basically normal. Due to concerns about intracranial infection, in addition to blood tests, we also extracted cerebrospinal fluid from the patient for testing. The laboratory results were shown in Table 1, where the patient’s blood infectivity indicators were elevated and abnormal cerebrospinal fluid indicators indicated the presence of intracranial infection.
Imaging examination
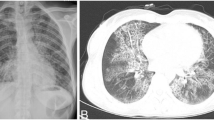
Upon admission, the patient underwent cranial MRI examination, which revealed bilaterally scattered patchy and focal abnormal signals in the frontal and parietal white matter, periventricular region, and basal ganglia. These signals appeared confluent in some localized areas. On T1-weighted imaging (T1WI), the signals were slightly decreased or isointense, while on T2-weighted imaging (T2WI) and FLAIR imaging, the signals were increased. No apparent diffusion restriction was observed on diffusion-weighted imaging (DWI). A lesion was observed in the left cerebellar hemisphere, characterized by indistinct borders. T1WI showed slightly decreased signals, while T2WI, FLAIR, and DWI showed high signals. Additionally, the surrounding area exhibited edema. In Fig. 1A, a distinct abscess lesion was seen, suggesting the possibility of an infection. Figure 1B and C depict postoperative MRI images acquired immediately after surgery and two weeks post-surgery, respectively. These images demonstrate the changes following the left cerebellar lesion resection, gradual resorption of pneumocephalus in the surgical area, and a reduced range of multiple enhancing lesions in the left cerebellum compared to the previous scan.
Etiological examination
During the excision of cerebellar lesion, a large abscess was identified in the left cerebellar hemisphere and promptly sent for examination. Histopathological analysis (Fig. 2A) revealed the presence of suppurative inflammation with abscess formation. Microscopic examination of the smears (Fig. 2B) revealed clusters of Gram-positive bacteria, while acid-fast staining (Fig. 2C) demonstrated red-colored bacterial filaments. Scanning electron microscopy (Fig. 2D) revealed rough, long, filamentous bacteria. After three days of incubation, blood agar plate culture exhibited white, dry, wrinkled colonies, which were identified as N. beijingensis by matrix-assisted laser desorption ionization-time of flight mass spectrometry (MALDI-TOF MS, Hangzhou YiDan biology technology co., ltd) (Fig. 2E). The antibiotic susceptibility results were summarized in Table 2.
Patient’s etiological results. (A) HE staining section of the patient’s abscess tissue showed inflammatory infiltration. (B) Gram staining of abscess tissue revealed purple bacterial clusters. (C) The abscess tissue was positive for acid fast staining, with visible red hyphae. (D) Under the electron microscope, slender bacterial bodies could be seen in N. beijingensis ZJSRMYY1. (E) Identification peak diagram of N. beijingensis ZJSRMYY1 by mass spectrometry
Treatment and outcome
During the patient’s hospitalization, continuous mannitol was administered to reduce intracranial pressure. On the second day of hospitalization, brain MRI revealed the presence of abscess. A single dose of vancomycin was administered for antimicrobial therapy. On the fifth day, the patient underwent cerebellar lesion resection. Following the incision of the left cerebellar hemisphere, purulent fluid was observed to discharge from a location approximately 2 cm deep to the left midline. After closure of the breach, the edematous area around the abscess was dissected, and a large abscess was completely excised for pathological and pathogen examinations. Based on the preoperative magnetic resonance images, the lateral part of the cerebellum was partially resected, and the remaining infected tissue was removed. The surgical field was thoroughly irrigated with a saline solution containing vancomycin, adequate hemostasis was achieved, and a gelatin sponge adhered to the surgical site was used to prevent further bleeding. After ensuring no active bleeding, dural defects were repaired with artificial dura mater, fascia was reconstructed, the bone flap was repositioned, and fixation was performed with titanium screws and plates. Layered closure was achieved with subcutaneous and skin sutures. Postoperatively, the patient received a combination of vancomycin, meropenem, linezolid, and trimethoprim-sulfamethoxazole (TMP-SMX) for antimicrobial therapy. After 24 days, the patient’s infection markers decreased to normal levels, the brain lesion on the MRI diminished, and the patient remained stable, allowing for discharge. Following discharge, the patient continued oral administration of linezolid and sulfamethoxazole/trimethoprim for 30 days. The treatment plan for the patient was presented in Fig. 3
Phylogenetic tree of N. beijingensis ZJPPH1
The nucleotide sequences of the1540-bp 16 S rRNA were verified and utilized to perform phylogenetic analysis by the Molecular Evolutionary Genetics Analysis (MEGA) software version 11 through the minimum-evolution method. A phylogenetic tree was constructed utilizing the sequence of N. beijingensis ZJPPH1 (GenBank number: PP267164) from the isolate of this study along with 29 available sequences with the highest homology retrieved from GenBank. The nucleic acid sequence of the present isolate revealed 99.37% similarity with N. beijingensis strain IFM 0841 (Fig. 4).
Discussion
Brain abscess is a life-threatening infection, and the mortality rate increases with prolonged illness [5]. Approximately 70% of surviving patients will experience sequelae such as epilepsy or neurological deficits [13]. Generally speaking, head trauma, chronic ear infections, dental infections, and immune dysfunction are the main risk factors for brain abscess, but the possibility of infection without obvious causes cannot be ruled out [14]. Oral bacteria such as Streptococcus anginosus, Fusobacterium species and Aggregatibacter species are the most common bacteria that cause brain abscess. Brain abscess caused by Staphylococcus aureus and other Gram-negative bacteria are relatively rare but have a poor prognosis for patients. Mycobacterium tuberculosis has regional prevalence, while brain abscesses caused by other fungi, parasites, and Nocardia are more common in immunocompromised patients [15].
Nocardia was first described as a saprophyte and innocuous species widely distributed in soil, water, and decaying plants. In recent years, more and more clinical data showed that some Nocardia species might cause life-threatening infections with varying pathogenicity, antibiotic resistance and prevalence. Nocardia abscessus, Nocardia cyriacigeorgica, Nocardia farcinica, and Nocardia nova commonly caused pulmonary infections, while Nocardia brasiliensis was often associated with cutaneous infections [16, 17]. Infections in other sites were typically caused by traumatic inoculation and hematogenous spread from primary foci [16]. Currently, there is extremely limited information on the epidemiology of N. beijingensis infection. According to the literature collected by N. beijingensis on Pubmed retrieval platform and the nucleic acid sequence source of N. beijingensis isolates published on Genbank, it has a global popularity with higher prevalence in Japan, USA, France, Mexico, Costa Rica, KSA, China, Thailand, Italy, Israel, Colombia, Australia. Worryingly, the number of immunocompetent patients with N. beijingensis is as high as 35.71% (10/28). A total of 28 cases of N. beijingensis infection were reported in the world, including 18 cases in immunocompromised patients (3 cases with diabetes, 1 case with smoking, 8 cases with HIV, 3 cases with solid organ transplantation, 6 cases with immunosuppressive drug, 2 cases with autoimmune diseases, and 1 case with malignant tumor), and 10 cases in immunocompetent individuals (Table 3). The average age of cases of N. beijingensis nocardiosis was 52-years-old, with a higher prevalence in males than females. Neurological infections accounted for 11 cases (39%), followed by pulmonary infections in 10 cases (36%), skin infections in 2 cases (7%), and 1 case each in other sites (including thoracic cavity, kidneys, heart, and the erector spinae muscle) (4%). Regarding N. beijingensis, based on existing case reports, despite variations in the site of infection, these cases share a common feature - the formation of abscesses at the lesion site [18, 19]. This appears to be a distinguishing characteristic of N. beijingensis infection.
The patient we report here had a previously healthy constitution and no smoking history. However, based on the pulmonary CT findings revealing inflammatory infiltrates and multiple small nodules, we suspected that the patient had a pulmonary infection that subsequently disseminated to the central nervous system, causing intracranial infection. Although diabetes, HIV, autoimmune diseases and smoking have been identified as risk factors for N. beijingensis infection, this patient had no documented risk factors, nor any history of immunosuppressive medication [20, 21]. Therefore, prevention of N. beijingensis infection should not be limited to immunocompromised or susceptible individuals. Once patients exhibit clinical manifestations of infection, the possibility of N. beijingensis infection should be considered. In 2014, Crozier et al. reported the first case of N. beijingensis infection in an immunocompetent patient in the United States [22]. Since then, an increasing number of reports have emerged in immunocompetent patients, predominantly involving the lungs and central nervous system [18]. Here we report the first case of brain abscess caused by Nocardia beijingensis infection in China, which develops an awareness of disseminated nocardiosis in immunocompetent individuals.
We reviewed all reported cases of N. beijingensis infection. Given that N. beijingensis infections often lead to the formation of abscesses at the site of infection, surgical intervention and antimicrobial therapy are necessary. Furthermore, susceptibility testing for N. beijingensis is indispensable. Currently, most reports indicate that N. beijingensis is susceptible to TMP-SMX, carbapenems, amikacin, and/or third-generation cephalosporins [22] but resistant to amoxicillin-clavulanic acid and ciprofloxacin according to the reported antimicrobial sensitivity results of N. beijingensis (Table 4), unlike N. transvaalensis is resistant to amikacin and N. abscessus is resistant to imipenem.
Our susceptibility results showed that the N. beijingensis ZJSRMYY1 strain was sensitive to TMP-SMX, linezolid and amoxicillin-clavulanate, intermediate to levofloxacin, but resistant to vancomycin, which explained the initial ineffectiveness of vancomycin treatment. Following the issuance of susceptibility results, we promptly switched to TMP-SMX and linezolid for treatment. Therefore, susceptibility testing played a crucial role in guiding the choice of antibiotics for Nocardia infections.
In conclusion, we report the first case of an immunocompetent individual who developed a brain abscess due to N. beijingensis infection in China. Abscess formation appears to be a common manifestation of N. beijingensis infection, and N. beijingensis has become an emerging pathogen in immunocompetent individuals. when patients present with symptoms such as headache, particular attention should be given to the possibility of intracranial infection of N. beijingensis. Susceptibility of N. beijingensis is uncertain to amoxicillin-clavulanic acid, ciprofloxacin and levofloxacin, therefore susceptibility testing is necessary in guiding the choice of antibiotics.
Data availability
Data available on request from the corresponding author.
References
Brouwer MC, Tunkel AR, McKhann GM 2nd, van de Beek D. Brain abscess. N Engl J Med. 2014;371(5):447–56. https://doi.org/10.1056/NEJMra1301635.
Brouwer MC, Coutinho JM, van de Beek D. Clinical characteristics and outcome of brain abscess: systematic review and meta-analysis. Neurology. 2014;82(9):806–13. https://doi.org/10.1212/wnl.0000000000000172.
Bodilsen J, Dalager-Pedersen M, van de Beek D, Brouwer MC, Nielsen H. Long-term mortality and Epilepsy in patients after Brain Abscess: a Nationwide Population-based Matched Cohort Study. Clin Infect Dis. 2020;71(11):2825–32. https://doi.org/10.1093/cid/ciz1153.
Nieves Perez CA, Sánchez Pérez MJ, Vargas AS, Franco MA, Molina Obana MC. Cerebral abscess due to Nocardia beijingensis Associated with HIV: Case Report and Mini Review. Cureus. 2023;15(10):e47571. https://doi.org/10.7759/cureus.47571.
Bodilsen J, Dalager-Pedersen M, van de Beek D, Brouwer MC, Nielsen H. Incidence and mortality of brain abscess in Denmark: a nationwide population-based study. Clin Microbiol Infect. 2020;26(1):95–100. https://doi.org/10.1016/j.cmi.2019.05.016.
Zhou C, Wang K, Li H, Zhang X. Idiopathic thrombocytopenic purpura with brain abscess caused by Nocardia farcinica diagnosed using metagenomics next-generation sequencing of the cerebrospinal fluid: a case report. BMC Infect Dis. 2021;21(1):380. https://doi.org/10.1186/s12879-021-06071-1.
Minero MV, Marín M, Cercenado E, Rabadán PM, Bouza E, Muñoz P. Nocardiosis at the turn of the century. Med (Baltim). 2009;88(4):250–61. https://doi.org/10.1097/MD.0b013e3181afa1c8.
Conville PS, Brown-Elliott BA, Smith T, Zelazny AM. The complexities of Nocardia Taxonomy and Identification. J Clin Microbiol. 2018;56(1). https://doi.org/10.1128/jcm.01419-17.
Fatahi-Bafghi M. Nocardiosis from 1888 to 2017. Microb Pathog. 2018;114:369–84. https://doi.org/10.1016/j.micpath.2017.11.012.
Wu J, Li X, Zhang T, Lin X, Chen YC. Disseminated Nocardia farcinica involves the spinal cord: a case report and review of the literature. BMC Infect Dis. 2021;21(1):1224. https://doi.org/10.1186/s12879-021-06905-y.
Wang L, Zhang Y, Lu Z, Shi Y, Liu Z, Maldonado L, et al. Nocardia beijingensis sp. nov., a novel isolate from soil. Int J Syst Evol Microbiol. 2001;51(Pt 5):1783–8. https://doi.org/10.1099/00207713-51-5-1783.
Kageyama A, Poonwan N, Yazawa K, Mikami Y, Nishimura K. Nocardia beijingensis, is a pathogenic bacterium to humans: the first infectious cases in Thailand and Japan. Mycopathologia. 2004;157(2):155–61. https://doi.org/10.1023/b:myco.0000020588.60081.37.
Bodilsen J, Duerlund LS, Mariager T, Brandt CT, Petersen PT, Larsen L, et al. Clinical features and prognostic factors in adults with brain abscess. Brain. 2023;146(4):1637–47. https://doi.org/10.1093/brain/awac312.
Bodilsen J, Dalager-Pedersen M, van de Beek D, Brouwer MC, Nielsen H. Risk factors for Brain Abscess: a Nationwide, Population-Based, nested case-control study. Clin Infect Dis. 2020;71(4):1040–6. https://doi.org/10.1093/cid/ciz890.
Bodilsen J, D’Alessandris QG, Humphreys H, Iro MA, Klein M, Last K, et al. European society of clinical Microbiology and Infectious diseases guidelines on diagnosis and treatment of brain abscess in children and adults. Clin Microbiol Infect. 2024;30(1):66–89. https://doi.org/10.1016/j.cmi.2023.08.016.
Brown-Elliott BA, Brown JM, Conville PS, Wallace RJ. Jr. Clinical and laboratory features of the Nocardia spp. based on current molecular taxonomy. Clin Microbiol Rev. 2006;19(2):259–82. https://doi.org/10.1128/cmr.19.2.259-282.2006.
Tan CK, Lai CC, Lin SH, Liao CH, Chou CH, Hsu HL, et al. Clinical and microbiological characteristics of Nocardiosis including those caused by emerging Nocardia species in Taiwan, 1998–2008. Clin Microbiol Infect. 2010;16(7):966–72. https://doi.org/10.1111/j.1469-0691.2009.02950.x.
Pender M, Mehta N, Hamilton BD, Swaminathan S. Nocardia beijingensis isolated from an adrenal abscess in a Diabetic host. Open Forum Infect Dis. 2022;9(7):ofac328. https://doi.org/10.1093/ofid/ofac328.
Martinaud C, Verdonk C, Bousquet A, Macnab C, Vaylet F, Soler C, et al. Isolation of Nocardia beijingensis from a pulmonary abscess reveals human immunodeficiency virus infection. J Clin Microbiol. 2011;49(7):2748–50. https://doi.org/10.1128/jcm.00613-11.
Steinbrink J, Leavens J, Kauffman CA, Miceli MH. Manifestations and outcomes of nocardia infections: comparison of immunocompromised and nonimmunocompromised adult patients. Med (Baltim). 2018;97(40):e12436. https://doi.org/10.1097/md.0000000000012436.
Paige EK, Spelman D. Nocardiosis: 7-year experience at an Australian tertiary hospital. Intern Med J. 2019;49(3):373–9. https://doi.org/10.1111/imj.14068.
Crozier JA, Andhavarapu S, Brumble LM, Sher T. First report of Nocardia beijingensis infection in an immunocompetent host in the United States. J Clin Microbiol. 2014;52(7):2730–2. https://doi.org/10.1128/jcm.00588-14.
Roy M, Martial A, Ahmad S. Disseminated Nocardia beijingensis infection in an Immunocompetent patient. Eur J Case Rep Intern Med. 2020;7(11):001904. https://doi.org/10.12890/2020_001904.
Raslan R, Bailey P, Sastry S. Nocardia beijingensis lung mass in an immunocompetent adult. BMJ Case Rep. 2021;14(1). https://doi.org/10.1136/bcr-2020-237454.
Qi L, Fan W, Li J, Cui H, Xu J, Gu D, et al. Persistent Nocardia beijingensis infection in a patient with postoperative abscess and misuse of antibiotics in China. Infect Med (Beijing). 2023;2(4):343–8. https://doi.org/10.1016/j.imj.2023.11.002.
Tanaka H, Kiko K, Watanabe Y, Yaguchi T, Oya S, Shiojiri T. Miliary cerebrospinal lesions caused by Nocardia beijingensis in an immunocompetent patient. IDCases. 2020;20:e00737. https://doi.org/10.1016/j.idcr.2020.e00737.
Rigotti S, Marocco S, Angheben A, Screpis D, Piovan G, Zorzi C. The first case of Nocardia beijingensis isolated infection to lumbar spine. J Neurosci Rural Pract. 2015;6(3):462–3. https://doi.org/10.4103/0976-3147.158767.
Abdel-Rahman N, Izhakian S, Wasser WG, Fruchter O, Kramer MR. Endobronchial Enigma: a clinically rare presentation of Nocardia beijingensis in an Immunocompetent patient. Case Rep Pulmonol. 2015;2015:970548. https://doi.org/10.1155/2015/970548.
Diioia A, Kalra L, Krop LC. Stroke like presentation of disseminated CNS Nocardia beijingensis infection in an immunocompetent patient: case report and review of the literature. IDCases. 2021;25:e01223. https://doi.org/10.1016/j.idcr.2021.e01223.
Solano-Varela DM, Barrios-Vidales EM, Plaza DF, Riveros WM, Guzmán J, Chica CE, et al. Immunocompetent patient with a brain abscess caused by Nocardia beijingensis in Latin America: a case report. Med (Baltim). 2019;98(11):e14879. https://doi.org/10.1097/md.0000000000014879.
Derancourt C, Theodose R, Deschamps L, Liautaud B, Briand E, Derancourt S, et al. Primary cutaneous nocardiosis caused by Nocardia beijingensis. Br J Dermatol. 2012;167(1):216–8. https://doi.org/10.1111/j.1365-2133.2012.10832.x.
Phoompoung P, Koomanachai P, NOCARDIA BEIJINGENSIS BRAIN, ABSCESS IN AN HIV INFECTED PATIENT: A FIRST CASE REPORT AND LITERATURE REVIEW. Southeast Asian J Trop Med Public Health. 2016;47(5):1020–5.
Laksananun N, Salee P, Kaewpoowat Q. Nocardia beijingensis pericarditis presenting with cardiac tamponade: a case report. Int J STD AIDS. 2018;29(5):515–9. https://doi.org/10.1177/0956462417736986.
Keenan JG, Mohapatra S. Nocardia beijingensis brain abscesses in an HIV-infected individual. IDCases. 2017;9:65–9. https://doi.org/10.1016/j.idcr.2017.03.006.
Leon-Tavares DM, Hernández-Silva G, Diaz-Lomeli P, Martínez-Gamboa A, Lopez-Luis BA. Multiple brain abscesses caused by Nocardia Beijingensis in a patient with HIV infection. Cureus. 2022;14(6):e25754. https://doi.org/10.7759/cureus.25754.
Bertrán-López J, Abbott A, Archibald LK, Benninger L, Lascano J, Kalyatanda G. Disseminated Nocardia beijingensis Masquerading as Pulmonary Tuberculosis in a patient with Human Immunodeficiency Virus/Acquired Immune Deficiency Syndrome. Open Forum Infect Dis. 2020;7(6):ofaa186. https://doi.org/10.1093/ofid/ofaa186.
Aragaki-Nakahodo A, Benzaquen S, Kirschner M. Coinfection by Nocardia beijingensis and Nocardia arthritidis in an immunocompromised patient diagnosed by endobronchial ultrasound guided transbronchial needle aspiration (EBUS-TBNA). Respir Med Case Rep. 2014;12:22–3. https://doi.org/10.1016/j.rmcr.2013.11.001.
Sheikh-Taha M, Corman LC. Pulmonary Nocardia beijingensis infection associated with the use of alemtuzumab in a patient with multiple sclerosis. Mult Scler. 2017;23(6):872–4. https://doi.org/10.1177/1352458517694431.
Ogawa T, Kasahara K, Yonekawa S, Nakagawa C, Maeda K, Konishi M, et al. Nocardia beijingensis pulmonary infection successfully treated with intravenous beta-lactam antibiotics and oral minocycline. J Infect Chemother. 2011;17(5):706–9. https://doi.org/10.1007/s10156-011-0233-2.
Gonzalez A, Jennings E, Vaziri S, Yachnis AT, Kubal A. Second report of a Nocardia beijingensis infection in the United States: nodular scleritis with in vitro imipenem resistance. Digit J Ophthalmol. 2016;22(3):62–6. https://doi.org/10.5693/djo.02.2016.01.003.
Richards AD, Stewart C, Karthik H, Lake SR. Bilateral subretinal abscesses: the first case of disseminated Nocardia beijingensis in Australia. Clin Exp Ophthalmol. 2015;43(9):843–5. https://doi.org/10.1111/ceo.12575.
Palavutitotai N, Chongtrakoo P, Ngamskulrungroj P, Chayakulkeeree M, Nocardia Beijingensis Psoas Abscess And Subcutaneous Phaeohyphomycosis Caused By, Phaeoacremonium Parasiticum In A Renal Transplant Recipient: The First Case Report In Thailand. Southeast Asian J Trop Med Public Health. 2015;46(6):1049–54.
Ohmori S, Kobayashi M, Yaguchi T, Nakamura M. Primary cutaneous nocardiosis caused by Nocardia beijingensis in an immunocompromised patient with chemotherapy for advanced prostate cancer. J Dermatol. 2012;39(8):740–1. https://doi.org/10.1111/j.1346-8138.2011.01411.x.
Chu RW, Lung D, Wong SN. Pulmonary abscess caused by Nocardia beijingensis: the second report of human infection. Pediatr Infect Dis J. 2008;27(6):572–3. https://doi.org/10.1097/INF.0b013e31816ffbfc.
Takayanagi K, Kimura Y, Kawakami K, Koyama K, Harada Y, Yamaryo T. [A case of pulmonary nocardiosis with Nocardia beijingensis]. Kansenshogaku Zasshi. 2008;82(1):43–6. https://doi.org/10.11150/kansenshogakuzasshi1970.82.43.
Kiatsuranon P, Suwanpimolkul G. Pulmonary nocardiosis with Superior Vena Cava Syndrome in a HIV-Infected patient: a Rare Case Report in the World. Jpn J Infect Dis. 2021;74(2):151–3. https://doi.org/10.7883/yoken.JJID.2019.470.
Acknowledgements
We thank all members of the microbiology laboratory of Zhejiang Provincial People’s Hospital for their help in the collection of clinical data.
Funding
This study was supported by the [New Project of Zhejiang Provincial People’s Hospital entitled “Construction of Rapid Nucleic Acid Detection Platform for Invasive Fungi”] under Grant [number 20211214].
Author information
Authors and Affiliations
Contributions
Lihong Jin and Weiqun Zhang analyzed data and draft articles. Fang Su collectd clinical data. Youqi J and Yumei Ge modified the article. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was supported by the Ethics Committee of Zhejiang People’s Hospital (Ethics Committee Approval of Biomedical Research Involving Humans, Approval No.: 2022JS008) and was carried out in accordance with the ethical standards of the Declaration of Helsinki.
Consent for publication
Written and informed consent was obtained from the patient for publication of this case report and any accompanying images.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jin, L., Zhang, W., Su, F. et al. Brain abscesses: the first report of disseminated Nocardia beijingensis infection in an immunocompetent individual in China. BMC Neurol 24, 341 (2024). https://doi.org/10.1186/s12883-024-03826-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-024-03826-6