Abstract
Background
An enduring challenge for women diagnosed with Turner syndrome (TS) is infertility. Oocyte donation (OD) offers a chance of pregnancy for these patients. However, current data on pregnancy outcomes are inadequate. Hence, this systematic review aims to explore the clinical outcomes of OD in patients with TS.
Methods
A systematic search was conducted in PubMed, Web of Sciences, Scopus, and Embase for relevant papers from 1 January 1990 to 30 November 2023. Our primary research objective is to determine the live birth rate among women with TS who have undergone in vitro fertilization (IVF) using OD for fertility purposes. Specifically, we aim to calculate the pooled live birth rates per patient and per embryo transfer (ET) cycle. For secondary outcomes, we have analyzed the rates of clinical pregnancy achievement per ET cycle and the incidence of gestational hypertensive complications per clinical pregnancy. Prevalence meta-analyses were performed using STATA 18.0 by utilizing a random-effects model and calculating the pooled rates of each outcome using a 95% confidence interval (CI).
Results
A total of 14 studies encompassing 417 patients were systematically reviewed. Except for one prospective clinical trial and one prospective cohort study, all other 12 studies had a retrospective cohort design. Our meta-analysis has yielded a pooled live birth rate per patient of 40% (95% CI: 29-51%; 14 studies included) and a pooled live birth rate per ET cycle of 17% (95% CI: 13-20%; 13 studies included). Also, the pooled clinical pregnancy achievement rate per ET cycle was estimated at 31% (95% CI: 25-36%; 12 studies included). Moreover, the pooled rate of pregnancy-induced hypertensive disorders per clinical pregnancy was estimated at 12% (95% CI: 1-31%; 8 studies included). No publication bias was found across all analyses.
Conclusions
This study demonstrated promising pregnancy outcomes for OD in patients with TS. Further studies are essential to address not only the preferred techniques, but also the psychological, ethical, and societal implications of these complex procedures for these vulnerable populations.
Trial registration
This systematic review was registered in the International Prospective Register of Systematic Reviews (PROSPERO) under the registration code CRD42023494273.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Turner syndrome (TS) is a genetic condition characterized by the complete or partial absence of one X chromosome in females [1, 2]. This condition affects about 1 in every 2000‒2500 females born alive [3]. The main karyotypes observed in patients with TS are 45, X (most common form), mosaic 45, X/46, XX, or isochromosome [4]. TS is characterized by a high incidence of early ovarian insufficiency, cardiovascular complications, short stature, renal abnormalities, hearing loss, osteoporosis, and neuropsychological deficits [1, 4,5,6]. The clinical manifestation varies significantly and shows differences in the various karyotypes [4, 7, 8]. Typically, women with a mosaic karyotype have a less severe phenotype [2, 4, 9].
An enduring challenge for women diagnosed with TS is delayed puberty and infertility [10, 11]. Most individuals with TS experience infertility due to gonadal dysgenesis [12, 13]. Oocyte loss occurs when oocytes are depleted from the ovaries after the 18th week of fetal development or within a few years after birth, typically before puberty [8, 14, 15]. Nevertheless, throughout adolescence, a small proportion of individuals, particularly those with mosaic karyotypes, may have ovaries containing a limited number of follicles. This can lead to spontaneous pubertal development and menarche [8]. Spontaneous puberty manifests in approximately 20–30% of individuals with TS, and their fertility rates range from 5 to 10% [15]. Although, most spontaneous pregnancies result in abortion, stillbirth, or delivery of newborns with congenital anomalies [8].
Reproductive medicine advancements provide fertility options for patients with TS through oocytes or ovarian tissue cryopreservation before the follicles start to disappear [16]. Furthermore, women with TS can become pregnant through emerging assisted reproductive technologies (ART), such as oocyte donation (OD) [17]. During this process, the donor undergoes ovarian stimulation to retrieve mature follicles, which are then fertilized with the sperm of the male partner (if applicable). Following endometrial preparation with hormone therapy, the resulting embryos are transferred into the uterus of the patient with TS [18, 19]. The pregnancy rate or live birth rate after OD in patients with TS varies across different studies [20, 21]. Furthermore, studies have demonstrated that the use of OD for the fertility of patients with TS may be linked to a higher occurrence of difficulties during pregnancy, such as pregnancy-induced hypertension, premature delivery, stillbirth, and abortion [22, 23].
Continuing investigation of strategies for improving fertility outcomes and decreasing pregnancy-induced complications in women with TS has been an area of interest [24,25,26,27]. To the best of our knowledge, this study is the first systematic review and meta-analysis to explore clinical outcomes of OD in patients with TS. Our primary objectives were to assess the live birth rate per patient receiving oocyte donation and per embryo transfer (ET) cycle. Additionally, we evaluated the clinical pregnancy rate per ET cycle and the occurrence rate of pregnancy-induced hypertensive disorders as secondary objectives. We hope the findings provide valuable insights into the success rates and adverse event rates associated with OD in patients with TS.
Materials and methods
This study was conducted by following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 checklist [28]. The review protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO) under the registration code CRD42023494273.
Research question
Our primary research objective is to determine the live birth rate among women with TS who have undergone in vitro fertilization (IVF) using OD for fertility purposes. Specifically, we aim to calculate the pooled live birth rates per patient (cumulative live birth rate) and live birth rate per ET cycle [29]. For secondary outcomes, we have analyzed the rates of clinical pregnancy achievement per ET cycle and the incidence of gestational hypertensive complications per clinical pregnancy.
Success rate definitions:
We defined a live birth as the delivery of a living baby beyond the 25th week of gestation, with the delivery of twins or other multiples considered a single event. Women with TS who underwent IVF using OD consisted of women who participated in at least one IVF using OD, whether they had successful intrauterine pregnancy or ectopic pregnancy or did not get implantation. Clinical pregnancy was defined by the detection of a gestational sac on the first ultrasound scan, conducted between 6 and 8 weeks of gestation. Pregnancy-induced hypertensive disorders were identified as the occurrence of at least one of the following complications in a successful clinical pregnancy: (1) gestational hypertension (2), mild or severe preeclampsia, or (3) eclampsia.
Search strategy
We conducted a systematic search on January 15, 2024, across four reputable online databases (PubMed, Scopus, Embase, and Web of Science) for papers published from January 1, 1990, to November 30, 2023, to identify relevant studies. No language restrictions were applied.
Given the aim of our review, descriptive, and observational studies conducted globally were included. Furthermore, non-observational studies which contained the data of our primary outcome were included. The search syntax contained variations of keywords related to [1] TS, and [2] OD. Supplementary Materials 1 provides a comprehensive description of the keywords and filters utilized in each database. Additionally, a precise citation screening was executed on the reference lists of the included studies to identify further relevant articles.
Inclusion and exclusion criteria
All peer-reviewed articles were considered if they explored the live birth rate among women with all variations of TS at any age, who underwent at least one IVF using OD for fertility purposes.
The exclusion criteria were defined as follows: (1) records that did not assess our primary outcome or lacked essential information; (2) animal studies; and (3) review articles, case reports, case series, brief reports, meeting abstracts, book chapters, letters, editorials, commentaries, correspondence, and study protocols.
Study selection
Two independent reviewers (ZS, TSSS) screened the identified studies based on title and abstract. Full-text assessments were performed to ensure the inclusion of relevant data. Any discrepancies in selection were resolved through discussion or consultation with a third reviewer (PR).
Data collection
Two individual reviewers performed data extraction independently (SK, PR). Any disagreement was resolved through discussion with a third reviewer (MP) and double-checking the extracted data. Data from each included article were systematically compiled across three key categories: general information (first author, publication year, country of origin, and study design), ART outcomes (women with TS who underwent IVF using OD, TS karyotypes, mean age, number of ET cycles, number of transferred embryos, clinical pregnancy achievement, live births, and ongoing pregnancies), and pregnancy-induced hypertensive complications.
Quality assessment
Two researchers (SK, PR) evaluated the methodological quality of each included study through a 10-questionary checklist developed by Hoy et al. [30]. This checklist was built to assess the risk of bias in studies measuring prevalence. The checklist comprises four inquiries concerning the external validity (e.g., sampling frame or random selection) and six inquiries concerning the internal validity (e.g., data collection or case definition) of the included studies. Each question has two standard answer options: Yes (low risk) or No (high risk). Subsequently, the studies will be divided into three levels of bias: (1) low risk of bias (2), moderate risk of bias (3), high risk of bias [30].
Meta-analysis
The data extracted from the included studies was transferred from a Microsoft Excel spreadsheet to the STATA version 18.0 statistical software (StataCorp LP, 4905 Lakeway Drive, College Station, TX 7854, USA) meta-analysis, which was conducted for four distinct purposes. Firstly, the meta-analysis explored the live birth rate per patient receiving OD (cumulative live birth rate). Secondly, it examined the live birth rate per ET cycle. Then, a meta-analysis was conducted to estimate the pooled clinical pregnancy rate per ET cycle. Lastly, a meta-analysis was performed to calculate the pooled hypertensive disorder occurrence rate per clinical pregnancy.
Each analysis presented the effect size as a proportion (and percentage), along with a 95% Confidence Interval (CI) around the summary estimate. To evaluate significant heterogeneity between studies, the Cochrane Q and I² statistics were employed. An I² value exceeding 50% was considered indicative of substantial heterogeneity among the studies. The existence of heterogeneity was graphically represented through a forest plot. Additionally, a Galbraith plot was generated to depict the presence or absence of each study within the 95% CI, indicating significant deviations from the majority of the analyzed studies. Pooled prevalences were estimated using a random-effect model with the restricted maximum likelihood method. Additionally, a sensitivity analysis was performed using a leave-one-out meta-analysis approach to assess the individual impact of each included study. Furthermore, when possible, we conducted two subgroup analyses for each meta-analysis for two separate groups of patients with monosomy (45, X) and mosaic TS karyotypes to examine the study outcomes in each group.
To examine potential publication bias across the analyzed studies after each meta-analysis, we utilized two objective methods: the nonparametric rank correlation (Begg) test [31] and the regression-based Egger test for small study effects [32]. A p-value below 0.05 was considered suggestive of potential publication bias. In cases where publication bias was identified, the nonparametric trim-and-fill method developed by Duval and Tweedie was planned to be applied [33]. Furthermore, in analyses that included more than 10 studies, we illustrated funnel plots to subjectively examine and illustrate the asymmetry of the analyzed studies [34].
Results
Search results
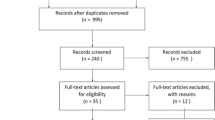
A comprehensive search of electronic databases identified 842 records. Following the elimination of 361 duplicated records, 481 unique records remained. Upon screening the titles and abstracts of these records, 413 were excluded, leaving 68 articles for thorough full-text screening. Subsequently, 14 articles met the inclusion criteria and were included in the meta-analysis [35,36,37,38,39,40,41,42,43,44,45,46,47,48]. Furthermore, manual screening of the reference lists of the included studies revealed no more eligible articles. The screening process is visually represented in the PRISMA 2020 flow chart, depicted in Fig. 1.
Study characteristics
The 14 included studies encompassed a total sample size of 417 women with TS who underwent IVF using OD. The sample size of these articles varied between 5 participants and 144 participants. These studies were conducted across diverse geographical regions and were published from 1990 to 2020. All of the included studies were published in English full-text. Except for one prospective clinical trial [46] and one prospective cohort study [44], all of the other 12 studies had a retrospective cohort design. Moreover, 3 studies were exclusively conducted on patients with a monosomy TS karyotype [35, 36, 39], 1 study only included patients with mosaic TS karyotypes [46], and 8 studies were conducted on combined populations of patients with monosomy and mosaic TS karyotypes [37, 38, 42,43,44,45, 47, 48]. However, 2 studies did not specify the karyotypes of their populations [40, 41]. Detailed characteristics of the included studies are provided in Table 1.
Quality assessment
Upon our examination, 5 studies were classified with an overall “moderate risk of bias” [35,36,37, 41, 48], while the remaining 9 studies were designated as having an overall “low risk of bias” [38,39,40, 42,43,44,45,46,47] (Table 1). Three inquiries examining the external validity of the included studies were consistently identified as the primary reasons for the elevated risk of bias. These inquiries specifically evaluate the target population of the studies, the sampling frame employed, and the methodology of case selection.
Meta-analysis
Live birth rate per patient (cumulative live birth rate)
A prevalence meta-analysis was performed on the pooled data from 14 studies encompassing a total of 417 patients [35,36,37,38,39,40,41,42,43,44,45,46,47,48]. The analysis revealed that the heterogeneity among the studies was considerable, as demonstrated by an I2 value of 74.43%. Employing a random-effect model, the estimated pooled live birth rate for each woman undergoing OD was 40% (95% CI: 29-51%). The Galbraith plot further illustrated that 3 studies fell outside the 95% CI range. The leave-one-out sensitivity analysis demonstrated that omitting each study resulted in pooled live birth rates per patient ranging from 39 to 45%, consistently falling within the initial estimated 95% CI, which highlights the robustness of our findings (Fig. 2).
Additionally, we conducted two separate subgroup analyses to calculate the pooled live birth rates per patient for both monosomy and mosaic TS karyotypes. Our findings indicated that the pooled live birth rate for the monosomy TS karyotype group was 31% (95% CI: 15-50%) based on data from five studies. In contrast, the pooled live birth rate for the mosaic TS karyotype group, derived from three studies, was estimated at 48% (95% CI: 31-66%). The forest plots of the subgroup analyses are provided in Supplementary Materials 2.
Regarding the assessment of publication bias, we calculated p-values of 0.900 and 0.868 for Egger’s and Begg’s tests, respectively, indicating no potential publication bias among the analyzed studies. The funnel plot is presented in Fig. 2.
Live birth rate per ET cycles
Pooling data from 13 studies [35,36,37,38,39,40, 42,43,44,45,46,47,48] with a total of 273 patients, the meta-analysis revealed very low heterogeneity among the included studies, evidenced by an I² value of 0%. Utilizing a random-effects model, the overall live birth rate per embryo transfer cycle was estimated at 17% (95% CI: 13-20%). Notably, the Galbraith plot indicated that two studies fell outside the 95% confidence interval range. Additionally, the leave-one-out sensitivity analysis yielded pooled live birth rates per embryo transfer cycle ranging from 16 to 18%, all of which fell within the initial estimated 95% CI, underscoring the consistency of our findings (Fig. 3).
Furthermore, we conducted two separate subgroup analyses to calculate the pooled live birth rates per embryo transfer cycle for both monosomy and mosaic TS karyotypes. Our results showed that the pooled live birth rate for the monosomy TS karyotype group was 15% (95% CI: 4-30%) based on data from five studies. In contrast, the pooled live birth rate for the mosaic TS karyotype group, derived from three studies, was estimated at 24% (95% CI: 12-37%). The forest plots for the subgroup analyses are provided in Supplementary Materials 2.
Regarding the assessment of publication bias, we calculated p-values of 0.103 and 0.160 for Egger’s and Begg’s tests, respectively, demonstrating no potential publication bias among the analyzed studies. The funnel plot is provided in Fig. 3.
Clinical pregnancy rate per ET cycles
After pooling data from 12 studies [35,36,37,38,39,40, 42,43,44,45,46,47] involving a total of 259 patients, the random-effects model indicated relatively low heterogeneity among the analyzed studies, as evidenced by an I² value of 33.64%. Our meta-analysis revealed a pooled clinical pregnancy rate per ET cycle of 31% (95% CI: 25-36%). Additionally, none of the 12 studies fell outside the 95% confidence interval range in the Galbraith plot. The leave-one-out sensitivity analysis produced consistent findings, with clinical pregnancy rates per ET cycle ranging from 29 to 32% (Fig. 4).
Further subgroup analyses demonstrated a pooled clinical pregnancy rate of 30% (95% CI: 20-41%) for patients with monosomy TS, based on data from five studies, and a pooled rate of 37% (95% CI: 24-51%) for patients with mosaic TS, derived from four studies. The forest plots for these subgroup analyses are provided in Supplementary Materials 2.
Our assessment of publication bias yielded p-values of 0.240 and 0.537 for Egger’s and Begg’s tests, respectively, indicating no potential publication bias among the analyzed studies. The funnel plot is presented in Fig. 4.
Pregnancy-induced hypertensive disorder rate per clinical pregnancy
A prevalence meta-analysis was performed on the pooled data from 8 studies [35, 40,41,42,43,44,45, 47] involving a total of 202 patients. The analysis revealed an I² value of 83.28%, indicating significant heterogeneity among the studies. Using a random-effects model, the estimated pooled rate of hypertensive disorders per confirmed clinical pregnancy was 12% (95% CI: 1-31%). In the Galbraith plot, 4 studies fell outside the 95% confidence interval, further demonstrating the high heterogeneity present. The leave-one-out sensitivity analysis produced a pooled rate of hypertensive disorders per clinical pregnancy ranging from 8 to 14%, all of which fell within the initially calculated 95% CI, suggesting the consistency of the findings despite the observed heterogeneity (Fig. 5).
Due to the limited number of studies, subgroup analysis for monosomy and mosaic TS karyotypes was not feasible.
Our assessment of publication bias yielded p-values of 0.963 and 0.901 for Egger’s and Begg’s tests, respectively, indicating no potential publication bias among the analyzed studies. A funnel plot was not included because the number of studies was less than 10.
Discussion
In this study, we identified a live birth rate per ET of 17% for OD in patients with TS, which increased to 40% when assessing the live birth rate per patient receiving OD (cumulative live birth rate). Considering that fewer than 10% of patients with TS can achieve spontaneous pregnancy [49], OD significantly enhances the fertility potential for these patients. However, our results highlight the necessity for further research to determine optimal approaches to improve pregnancy and live birth rates following OD in TS patients. Nonetheless, our findings suggest that OD can be a relatively effective method of ART for TS patients seeking to experience motherhood.
Infertility has always been one of the greatest obstacles faced by women with TS [13]. Since spontaneous conception in TS patients is rare, alternative methods are essential to help these patients become parents [13]. Currently, ART methods such as IVF, OD, embryo donation, and insemination, as well as alternative options like fostering and adoption, are viable solutions [13]. Among these methods, OD has been and continues to be the most commonly used procedure for TS women [50]. Over the past three decades, OD has significantly advanced and is now the preferred ART method for infertile women seeking to achieve motherhood [51]. OD is particularly beneficial for patients with complete primary ovarian insufficiency, especially those with TS [52]. However, societal beliefs can pose potential obstacles to OD [53]. For instance, in some Islamic societies, third-party reproduction may be considered forbidden under Islamic law [54]. Additionally, previous research suggested that OD may not be the most cost-effective ART method. For example, a study has shown that embryo donation is twice as cost-effective as OD following a single ET cycle [55]. This underscores that the current advancements are merely a starting point. Further research is imperative to enhance the outcomes of OD and to develop more optimal treatment methods for women with TS.
In a study conducted by Bryman et al. in Sweden, 30 women with TS became pregnant through OD [56]. The live birth rate among this cohort was 74%. Notably, the live birth percentage in the OD group was significantly higher than in the group of patients attempting spontaneous pregnancy, and combined groups of patients receiving IVF and insemination techniques [56]. While the live birth rates after OD in Bryman et al.‘s study were higher than those found in our meta-analysis, both sets of findings underscore the potential of OD as an effective fertility treatment for patients with TS [56].
It is noteworthy that live birth rates following OD in patients with different TS karyotypes are generally lower compared to those with normal karyotypes. In our study, we found a live birth rate per ET cycle of 17%, whereas prior research in women with normal karyotypes yielded a 53% live birth rate after the first ET cycle [57]. This discrepancy arises because the infertility issues in patients with TS extend beyond gonadogenesis failure. Patients with TS face several other challenges, including a higher risk of chromosomal abnormalities in their fetuses, autoimmune disorders, and ovarian and uterine insufficiencies, which can significantly increase the risk of early abortion and miscarriage in this population [12, 58]. The lower success rates of OD in patients with TS compared to those with normal karyotypes is a crucial topic that should be included in the pretreatment counseling process to ensure patients are adequately informed. However, it is important to note that, similar to normal-karyotype patients, our analysis demonstrated that increasing the number of ET cycles significantly enhances live birth rates following OD in patients with TS [57]. Therefore, the application of different modifications, such as increasing the prescribed ET cycles and the number of transferred embryos in each cycle, could potentially further improve the pregnancy outcomes after OD in patients with TS.
In addition to our primary analyses, we conducted subgroup analyses to assess live birth rates in patients with monosomy and mosaic TS karyotypes separately. Our findings indicate that both the live birth rate per patient (48% vs. 31%) and the live birth rate per ET cycle (24% vs. 15%) were significantly higher in patients with mosaic TS compared to those with monosomy TS. This aligns with previous research suggesting that mosaic karyotypes are associated with less severe outcomes, including reproductive outcomes [58]. Therefore, it is imperative for reproductive physicians to counsel patients with TS regarding their karyotypes prior to administering ovarian stimulation or other assisted reproductive technologies.
Moreover, patients with TS are at an increased risk for various cardiovascular diseases, which can worsen during pregnancy, including congenital cardiac defects and hypertensive disorders [26, 59, 60]. In this context, we conducted a meta-analysis to examine the incidence of pregnancy-induced hypertensive disorders following OD in patients with TS, finding a pooled occurrence rate of 12% per clinical pregnancy. This rate is lower than previously reported occurrences of hypertensive disorders in spontaneous pregnancies of patients with TS [61]. Two primary factors may explain this discrepancy: (a) Most studies included in our analysis performed cardiac assessments prior to OD and selected only patients without cardiac contraindications, likely reducing the estimated incidence of hypertensive disorders compared to those following spontaneous conception. (b) Due to varying data reporting methods, our analysis focused on the occurrence of hypertensive disorders per clinical pregnancy, primarily capturing data from the first trimester (6–8 weeks), whereas many hypertensive disorders arise after 20 weeks of gestation. Thus, further research is essential to assess the prevalence of hypertensive disorders in ongoing pregnancies during the later stages of pregnancy in patients with TS, which we hypothesize may exceed 12%. Nonetheless, due to the significant burden of cardiac disorders on both mothers and fetuses in patients with TS, it is essential for reproductive physicians to conduct thorough cardiac assessments before administering OD and to select only those patients without contraindications for pregnancy [58].
This study presents several notable strengths. First, all phases of the research, including the literature search, data extraction, and quality assessment, were conducted by two reviewers, minimizing the potential for reviewer bias. Second, we adhered to the PRISMA 2020 guidelines to enhance the reliability and validity of our results. Third, our literature search was rigorous and comprehensive, encompassing all relevant articles on the subject. Finally, we assessed publication bias using p-values obtained from Begg’s and Egger’s tests across all analysis groups, which indicated no evidence of publication bias among the included studies.
Nonetheless, there are certain limitations to this study. Primarily, the small sample sizes in most reviewed studies restrict the generalizability of our findings. Therefore, future investigations should aim to include larger and more representative populations of individuals with TS to yield more conclusive results regarding ART outcomes. Additionally, a significant proportion of the included studies utilized retrospective designs, which further limits the generalizability of their findings and highlights the need for additional research in this area. Also, many studies predate 2000, which may affect the accuracy of this review’s cumulative findings due to advancements in ART techniques. Lastly, it is important to note that most included studies did assess the potential effects of various confounding factors on the outcomes of OD. These factors may include the age of the donor and recipient of the oocytes, the number of transferred embryos per cycle, and embryo quality. Variations in these variables can significantly impact outcomes for patients undergoing OD, regardless of whether they have TS [62]. Therefore, it is imperative for future research to utilize larger sample sizes and longitudinal designs, adjusting analyses for the influence of these confounding factors to produce more generalizable findings in this field.
Conclusions
This systematic review and meta-analysis revealed a pooled live birth rate of 40% per patient and 17% per ET cycle in patients with TS undergoing ovarian stimulation for fertility purposes. Given that fewer than 10% of patients typically achieve spontaneous pregnancies, these rates are promising for those seeking to experience pregnancy and motherhood. However, as emerging ART methods offer new family planning options for TS patients, further investigation is necessary to explore not only the preferred techniques but also the psychological, ethical, and societal implications of these complex procedures for this vulnerable population. Therefore, there is a critical need for further research that utilizes larger sample sizes and longitudinal designs to evaluate the various outcomes of OD for fertility in patients with TS.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- ART:
-
Assisted reproductive technologies
- CI:
-
Confidence interval
- ET:
-
Embryo transfer
- IVF:
-
In vitro fertilization
- OD:
-
Oocyte donation
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PROSPERO:
-
International Prospective Register of Systematic Reviews
- TS:
-
Turner syndrome
References
Kesler SR. Turner syndrome. Child Adolesc Psychiatr Clin N Am. 2007;16(3):709–22.
Shankar Kikkeri N, Nagalli S, Turner Syndrome. StatPearls. Treasure Island (FL) with ineligible companies. Disclosure: Shivaraj Nagalli declares no relevant financial relationships with ineligible companies.: StatPearls Publishing Copyright © 2024. StatPearls Publishing LLC.; 2024.
McCarrison S, Carr A, Wong SC, Mason A. The prevalence of hypertension in paediatric Turner syndrome: a systematic review and meta-analysis. J Hum Hypertens. 2023;37(8):675–88.
Rosenberg AGW, Dingemans VDA, Bos-Roubos AG, Luijks S, Dessens AB, Dykgraaf R, et al. Associations between fatigue and endocrine and non-endocrine health problems in Turner Syndrome: Cohort Study and Review. J Clin Endocrinol Metab. 2023;108(12):e1649–59.
Yoon SH, Kim GY, Choi GT, Do JT. Organ abnormalities caused by Turner Syndrome. Cells. 2023;12(10).
Cui X, Cui Y, Shi L, Luan J, Zhou X, Han J. A basic understanding of Turner syndrome: incidence, complications, diagnosis, and treatment. Intractable Rare Dis Res. 2018;7(4):223–8.
Brezina P, Christianson M, Nguyen K-H, Siegel A, Benner A, Kearns W. Maternal XX/X chromosome mosaicism in donor oocyte in vitro fertilization (IVF). Middle East Fertility Soc J. 2012;17:129–33.
Bouchlariotou S, Tsikouras P, Dimitraki M, Athanasiadis A, Papoulidis I, Maroulis G, et al. Turner’s syndrome and pregnancy: has the 45,X/47,XXX mosaicism a different prognosis? Own clinical experience and literature review. J Matern Fetal Neonatal Med. 2011;24(5):668–72.
Kruszka P, Addissie YA, Tekendo-Ngongang C, Jones KL, Savage SK, Gupta N, et al. Turner syndrome in diverse populations. Am J Med Genet A. 2020;182(2):303–13.
Zhong Q, Layman LC. Genetic considerations in the patient with Turner syndrome–45,X with or without mosaicism. Fertil Steril. 2012;98(4):775–9.
Gonzalez L, Witchel SF. The patient with Turner syndrome: puberty and medical management concerns. Fertil Steril. 2012;98(4):780–6.
Doğer E, Çakıroğlu Y, Ceylan Y, Ulak E, Özdamar Ö, Çalışkan E. Reproductive and obstetric outcomes in mosaic Turner’s syndrome: a cross-sectional study and review of the literature. Reprod Biol Endocrinol. 2015;13:59.
Viuff M, Gravholt CH, editors. Turner syndrome and fertility. Annales d’Endocrinologie. Elsevier; 2022.
Hreinsson JG, Otala M, Fridström M, Borgström B, Rasmussen C, Lundqvist M, et al. Follicles are found in the ovaries of adolescent girls with Turner’s syndrome. J Clin Endocrinol Metab. 2002;87(8):3618–23.
Pienkowski C, Menendez M, Cartault A, Lorenzini F, Lesourd F, Tauber M. [Turner’s syndrome and procreation. Ovarian function and Turner’s syndrome]. Gynecol Obstet Fertil. 2008;36(10):1030–4.
Wang J, Lan T, Dai X, Yang L, Hu X, Yao H. The cut-off value of serum Anti-Müllerian hormone levels for the diagnosis of Turner Syndrome with spontaneous puberty. Int J Endocrinol. 2023;2023:6976389.
Borgström B, Hreinsson J, Rasmussen C, Sheikhi M, Fried G, Keros V, et al. Fertility preservation in girls with turner syndrome: prognostic signs of the presence of ovarian follicles. J Clin Endocrinol Metab. 2009;94(1):74–80.
Moomjy M, Cholst I, Mangieri R, Rosenwaks Z. Oocyte donation: insights into implantation. Fertil Steril. 1999;71(1):15–21.
Bistany G, Budinetz T, Benadiva C, Nulsen J, Bartolucci AF, DiLuigi A. Turner syndrome patients undergoing anonymous egg donation cycles have low clinical and ongoing pregnancy rates after single blastocyt transfer. Fertil Steril. 2013;100(3):S488.
Hadnott TN, Gould HN, Gharib AM, Bondy CA. Outcomes of spontaneous and assisted pregnancies in Turner syndrome: the U.S. National Institutes of Health experience. Fertil Steril. 2011;95(7):2251–6.
Giles J, Meseguer M, Mercader A, Rubio C, Alegre L, Vidal C, et al. Preimplantation genetic testing for aneuploidy in patients with partial X monosomy using their own oocytes: is this a suitable indication? Fertil Steril. 2020;114(2):346–53.
Söderström-Anttila V, Pinborg A, Karnis MF, Reindollar RH, Paulson RJ. Should women with Turner syndrome be allowed to carry their own pregnancies? Fertil Steril. 2019;112(2):220–5.
Delbaere A, Englert Y. Turner’s syndrome and oocyte donation. Gynecologie Obstetrique Fertil. 2002;30(12):970–8.
Brouillet S, Ranisavljevic N, Sonigo C, Haquet E, Bringer-Deutsch S, Loup-Cabaniols V, et al. Should we perform oocyte accumulation to preserve fertility in women with Turner syndrome? A multicenter study and systematic review of the literature. Hum Reprod. 2023;38(9):1733–45.
Bollig KJ, Mainigi M, Senapati S, Lin AE, Levitsky LL, Bamba V. Turner syndrome: fertility counselling in childhood and through the reproductive lifespan. Curr Opin Endocrinol Diabetes Obes. 2023;30(1):16–26.
Hynes JS, Kuller JA, Goldstein SA, Ward CC, Muasher SJ. Increased risk of aortic dissection Associated with pregnancy in Women with Turner Syndrome: a systematic review. Obstet Gynecol Surv. 2020;75(9):566–75.
Ye M, Yeh J, Kosteria I, Li L. Progress in Fertility Preservation Strategies in Turner Syndrome. Front Med (Lausanne). 2020;7:3.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. 2021;372:n71.
Gadalla MA, Wang R, van Wely M, Mol BWJ. How should we report outcomes in reproductive medicine? Ultrasound Obstet Gynecol. 2018;51(1):7–9.
Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65(9):934–9.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994:1088 – 101.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Duval S, Tweedie R. A nonparametric trim and fill method of accounting for publication bias in meta-analysis. J Am Stat Assoc. 2000;95(449):89–98.
Sterne JAC, Sutton AJ, Ioannidis JPA, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002.
Cornet D, Alvarez S, Antoine JM, Tibi C, Mandelbaum J, Plachot M, et al. Pregnancies following ovum donation in gonadal dysgenesis. Hum Reprod. 1990;5(3):291–3.
Press F, Shapiro HM, Cowell CA, Oliver GD. Outcome of ovum donation in Turner’s syndrome patients. Fertil Steril. 1995;64(5):995–8.
Yaron Y, Ochshorn Y, Amit A, Yovel I, Kogosowski A, Lessing JB. Patients with Turner’s syndrome may have an inherent endometrial abnormality affecting receptivity in oocyte donation. Fertil Steril. 1996;65(6):1249–52.
Khastgir G, Abdalla H, Thomas A, Korea L, Latarche L, Studd J. Oocyte donation in Turner’s syndrome: an analysis of the factors affecting the outcome. Hum Reprod. 1997;12(2):279–85.
Loutradis D, Drakakis P. Gonadal dysgenesis: Fertility options. 1997. pp. 389 – 94.
Foudila T, Söderström-Anttila V, Hovatta O. Turner’s syndrome and pregnancies after oocyte donation. Hum Reprod. 1999;14(2):532–5.
Karnis MF, Zimon AE, Lalwani SI, Timmreck LS, Klipstein S, Reindollar RH. Risk of death in pregnancy achieved through oocyte donation in patients with Turner syndrome: a national survey. Fertil Steril. 2003;80(3):498–501.
Bodri D, Vernaeve V, Figueras F, Vidal R, Guillén JJ, Coll O. Oocyte donation in patients with Turner’s syndrome: a successful technique but with an accompanying high risk of hypertensive disorders during pregnancy. Hum Reprod. 2006;21(3):829–32.
Bodri D, Guillén JJ, Schwenn K, Casadesus S, Vidal R, Coll O. Poor outcome in oocyte donation after elective transfer of a single cleavage-stage embryo in Turner syndrome patients. Fertil Steril. 2009;91(4 SUPPL):1489–92.
Boissonnas CC, Davy C, Marszalek A, Duranteau L, De Ziegler D, Wolf JP, et al. Cardiovascular findings in women suffering from Turner syndrome requesting oocyte donation. Hum Reprod. 2011;26(10):2754–62.
Mercadal BA, Imbert R, Demeestere I, Englert Y, Delbaere A. Pregnancy outcome after oocyte donation in patients with Turners syndrome and partial X monosomy. Hum Reprod. 2011;26(8):2061–8.
Brezina PR, Christianson MS, Nguyen KHD, Siegel A, Benner AT, Kearns WG. Maternal XX/X chromosome mosaicism in donor oocyte in vitro fertilization (IVF). Middle East Fertility Soc J. 2012;17(2):129–33.
Andre H, Pimentel C, Veau S, Domin-Bernhard M, Letur-Konirsch H, Priou G, et al. Pregnancies and obstetrical prognosis after oocyte donation in Turner Syndrome: a multicentric study. Eur J Obstet Gynecol Reproductive Biology. 2019;238:73–7.
Calanchini M, Aye CYL, Orchard E, Baker K, Child T, Fabbri A, et al. Fertility issues and pregnancy outcomes in Turner syndrome. Fertil Steril. 2020;114(1):144–54.
Saenger P, Wikland KA, Conway GS, Davenport M, Gravholt CH, Hintz R, et al. Recommendations for the diagnosis and management of Turner syndrome. J Clin Endocrinol Metab. 2001;86(7):3061–9.
Gravholt CH, Andersen NH, Conway GS, Dekkers OM, Geffner ME, Klein KO et al. Clinical practice guidelines for the care of girls and women with Turner syndrome: proceedings from the 2016 Cincinnati International Turner Syndrome Meeting. European journal of endocrinology. 2017;177(3):G1-G70.
Silvestris E, Petracca EA, Mongelli M, Arezzo F, Loizzi V, Gaetani M et al. Pregnancy by oocyte donation: reviewing fetal-maternal risks and complications. Int J Mol Sci. 2023;24(18).
Melnick AP, Rosenwaks Z. Oocyte donation: insights gleaned and future challenges. Fertil Steril. 2018;110(6):988–93.
Platts S, Bracewell-Milnes T, Saso S, Jones B, Parikh R, Thum M-Y. Investigating attitudes towards oocyte donation amongst potential donors and the general population: a systematic review. Hum Fertility. 2021;24(3):169–81.
Akyuz A, Sever N, Karasahin E, Guvenc G, Cek S. A Survey on Oocyte Donation: Turkish fertile and infertile women’s opinions. Int J Fertil Steril. 2014;8(3):289–98.
Finger R, Sommerfelt C, Freeman M, Wilson CK, Wade A, Daly D. A cost-effectiveness comparison of embryo donation with oocyte donation. Fertil Steril. 2010;93(2):379–81.
Bryman I, Sylvén L, Berntorp K, Innala E, Bergström I, Hanson C, et al. Pregnancy rate and outcome in Swedish women with Turner syndrome. Fertil Steril. 2011;95(8):2507–10.
Remohí J, Gartner B, Gallardo E, Yalil S, Simón C, Pellicer A. Pregnancy and birth rates after oocyte donation. Fertil Steril. 1997;67(4):717–23.
Whigham C-A, Vollenhoven B, Vincent AJ. Reproductive health in Turner syndrome: a narrative review. Prenat Diagn. 2023;43(2):261–71.
Bouet PE, Godbout A, El Hachem H, Lefebvre M, Bérubé L, Dionne MD, et al. Fertility and pregnancy in Turner Syndrome. J Obstet Gynaecol Can. 2016;38(8):712–8.
Chevalier N, Letur H, Lelannou D, Ohl J, Cornet D, Chalas-Boissonnas C, et al. Materno-fetal Cardiovascular complications in Turner Syndrome after Oocyte Donation: Insufficient Prepregnancy screening and pregnancy Follow-Up are Associated with Poor Outcome. J Clin Endocrinol Metabolism. 2011;96(2):E260–7.
Bernard V, Donadille B, Zenaty D, Courtillot C, Salenave S, de la Brac A, et al. Spontaneous fertility and pregnancy outcomes amongst 480 women with Turner syndrome. Hum Reprod. 2016;31(4):782–8.
Gupta P, Banker M, Patel P, Joshi B. A study of recipient related predictors of success in oocyte donation program. J Hum Reprod Sci. 2012;5(3):252–7.
Acknowledgements
Not applicable.
Funding
The authors declare that they have acquired no funding support for this study.
Author information
Authors and Affiliations
Contributions
P.R.: Conceptualization, Project administration, Protocol design, Systematic search, Data extraction, Quality assessment, Writing & Manuscript drafting, Critical revision. M.P.: Data Extraction, Statistical analysis, Writing & Manuscript drafting, Critical revision. S.K.: Protocol design, Data extraction, Quality assessment, Writing & Manuscript drafting. T.S.S.S.: Systematic search. Z.S.: Systematic search. S.A.S.: Writing & Manuscript drafting. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
: Utilized keywords and filters in each online dataset.
Supplementary Material 2
: Forrest plots for subgroup analyses. Supplementary Figs. 1–3.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Rashidian, P., Parsaei, M., Karami, S. et al. Live birth rate after oocyte donation in females diagnosed with turner syndrome: a systematic review and meta-analysis. BMC Pregnancy Childbirth 24, 605 (2024). https://doi.org/10.1186/s12884-024-06801-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-024-06801-8