Abstract
Background
Despite routine iron supplementation for pregnant women in South Africa, anaemia and iron deficiency (ID) in pregnancy remain a public health concern.
Objective
To determine the associations between iron status and birth outcomes of pregnant women attending antenatal clinic at a regional hospital in Bloemfontein.
Methods
In this cross-sectional study of 427 pregnant women, blood was taken to analyze biomarkers of anaemia (haemoglobin), iron status (ferritin and soluble transferrin receptor) and inflammation (C-reactive protein and α-1-acid glycoprotein). A questionnaire was used to collect information about birth outcomes (birth weight and gestational age at birth), HIV exposure, sociodemographics, iron supplement intake, and maternal dietary iron intake using a validated quantified food frequency questionnaire.
Results
The median (Q1, Q3) weeks of gestation of participants was 32 (26, 36) at enrolment. Anaemia, iron deficiency (ID), ID anaemia (IDA) and ID erythropoiesis (IDE) were present in 42%, 31%, 19% and 9.8% of participants, respectively. Median (Q1, Q3) dietary and supplemental iron intake during pregnancy was 16.8 (12.7, 20.5) mg/d and 65 (65, 65) mg/d, respectively. The median (max-min) total iron intake (diet and supplements) was 81 (8.8-101.8) mg/d, with 88% of participants having a daily intake above the tolerable upper intake level of 45 mg/d. No significant associations of anaemia and iron status with low birth weight and prematurity were observed. However, infants born to participants in the third hemoglobin (Hb) quartile (Hb > 11.3–12.2 g/dL) had a shorter gestation by 1 week than those in the fourth Hb quartile (Hb > 12.2 g/dL) (p = 0.009). Compared to pregnant women without HIV, women with HIV had increased odds of being anaemic (OR:2.14, 95%CI: 1.41, 3.247), having ID (OR:2.19, 95%CI: 1.42, 3.37), IDA (OR:2.23, 95%CI: 1.36, 3.67), IDE (OR:2.22, 95%CI: 1.16, 4.22) and delivering prematurely (OR:2.39, 95%CI: 1.01, 5.64).
Conclusion
In conclusion, anaemia, ID, and IDA were prevalent in this sample of pregnant women, despite the reported intake of prescribed iron supplements, with HIV-infected participants more likely to be iron deficient and anaemic. Research focusing on the best formulation and dosage of iron supplementation to enhance iron absorption and status, and compliance to supplementation is recommended, especially for those living with HIV infection.
Graphical Abstract

Highlights
-
• Only 19% of the pregnant women met the daily estimated average requirement for iron through dietary intake, highlighting the need for iron supplementation.
-
• Despite the intake of routine 65 mg of elemental iron as a single micronutrient, anaemia and iron deficiency was prevalent in 42% and 31% of pregnant women respectively.
-
•In the total sample, anaemia, iron deficiency, iron deficiency anaemia (IDA), and iron deficiency erythropoiesis (IDE) were not associated with low birth weight and premature birth.
-
• Women living with HIV had over two times increased odds of being anaemic, iron deficient, having IDA and IDE, and delivering prematurely compared to those without HIV.
Similar content being viewed by others
Introduction
Iron is an essential element responsible for oxygen transport, energy production, DNA synthesis and muscle metabolism [1, 2]. Iron deficiency (ID) is the leading cause of anaemia, which is the most common nutritional deficiency in the world, affecting one-third of all women of reproductive age, 37% of pregnant women, and 40% of children [3]. During pregnancy, there is an increased physiological requirement for iron due to the transfer of iron to both the growing fetus and placental structures, and the expansion of the red blood cell mass [4]. However, iron requirements vary with each trimester. During the first trimester, iron requirement is lower due to the cessation of blood loss from menstruation, while in the second trimester, it starts to steadily increase through to the third trimester [4]. Anaemia in pregnancy, especially in the second trimester has been associated with increased prematurity, low birth weight (LBW), fetal death, and impaired cognitive and neuro-behavioral development [5]. Additionally, ID can adversely affect the general well-being of pregnant women by causing breathing difficulties, fainting, tiredness, palpitations, and sleep difficulties as well as increased risk of perinatal infection, pre-eclampsia, and bleeding [5].
It is estimated that 31% of pregnant women and 30.5% of non-pregnant women of reproductive age (i.e., 15–49 years) in South Africa are anaemic [3]. Similarly, data from a prospective cohort of pregnant women in Johannesburg showed that at 18 weeks of gestation, 29%, 15% and 15% of participants had anaemia, ID and ID erythropoiesis (IDE), respectively, and the prevalence of ID and IDE increased significantly through pregnancy week 22 and 36 [6]. Considering the high iron requirement in pregnancy, dietary intake alone may not be adequate to meet requirements, especially during the second and third trimesters. In developing countries where the staple food is predominantly cereal, with limited meat, vegetable and fruit intake, the amount of iron obtained from dietary sources is much lower [4]. In South Africa, the Government has implemented a number of policies to curb ID. One such policy is the mandatory fortification of maize meal and wheat flour with micronutrients including iron [7] to improve iron status of the entire population. Additionally, in South Africa, all pregnant women in the public health sector are routinely supplemented with single micronutrients in the form of 60 to 65 mg of ferrous iron and 5 mg of folic acid [8], beginning as early as possible after conception throughout pregnancy, irrespective of iron status, to prevent and/or treat iron deficiency anaemia and ID. Nonetheless, anaemia remains persistent, and is associated with nearly half of South African maternal deaths [9]. Factors such as poor dietary iron intake, poor compliance to prenatal iron supplementation, Human Immunodeficiency Virus (HIV) infection, obesity, and infection-induced inflammation (which impedes iron absorption) increase the risk of anaemia [10, 11]. Despite the importance of iron supplementation in preventing the detrimental effects of anaemia and ID in pregnancy, it should also be noted that routine iron supplementation in replete individuals can be harmful. Unabsorbed iron in the intestines favor the growth of iron-dependent enteropathogens, causing alterations in the gut microbiome, resulting in gut irritation and inflammation [12, 13]. These complications lead to non-compliance to the iron supplementation regimen and thus, persistence of anaemia and ID [10].
Although daily iron supplements are prescribed for pregnant women in the South African public health sector to prevent anaemia and ID, only haemoglobin is routinely assessed as part of the supplementation monitoring plan, while iron status is not. Therefore, data on the iron status of pregnant women and associations with birth outcomes in South Africa are limited. Considering this background, we hypothesized that the iron status of pregnant women in Bloemfontein is poor and is associated with adverse birth outcomes. Thus, the current study aimed to assess iron status, and associations with birth weight and prematurity among pregnant women in Bloemfontein, Free State Province.
Methods
Study design and participants
This was designed as a quantitative analytical cross-sectional study and was nested within the larger Nutritional status of Expectant Mothers and their newborn Infants (NuEMI) study. Pregnant women attending their routine antenatal visits at a Regional Hospital in Bloemfontein, South Africa were conveniently recruited between May 2018 and April 2019. About 700 women visit the antenatal clinic at this regional hospital monthly. To be included, pregnant women of any gestational age, had to provide informed consent and be older than 18 years and understand either English, Afrikaans, or SeSotho. Women expecting multiple babies were excluded in this sub-study.
Data collection
Sociodemographic and health data
At enrolment, sociodemographic data such as employment status, level of education, and marital status were collected from participants during a structured interview conducted by trained fieldworkers using a questionnaire adapted from the “Assuring Health in the Free State” (AHA-FS) study [14]. Health data such as smoking/tobacco use, previous pregnancies, HIV status, and medication use were also collected. HIV exposure status of babies was determined based on the details on HIV exposure noted in the Road to Health booklet of the baby.
Anthropometry
Weight and height of participants were measured using standard anthropometric techniques to determine gestational body mass index (GBMI), as described elsewhere [15]. To calculate GBMI, an algorithm developed by the Argentinian Ministry of Health [16], and used by Davies et al. [17] and Cruz et al. [18] in the EpiNut program was applied. The algorithm modified BMI to adjust for gestational age [17]. GBMI was categorized as: underweight (GBMI ≥ 10 to < 19.8 kg/m2), normal weight (GBMI ≥ 19.8 to < 26.1 kg/m2), overweight (GBMI ≥ 26.1 to < 29 kg/m2), and obese (GBMI ≥ 29 kg/m2) [18].
Dietary and supplemental iron intake
A validated quantified food frequency questionnaire (QFFQ) [19] was used to obtain data on maternal dietary iron intake during pregnancy. The QFFQ has proven reproducibility in similar study populations in South Africa [20,21,22]. For the current study, minor adaptions were made to the QFFQ to ensure participants understood the terminology used as described by Robb et al. [23]. The QFFQ was administered by trained fieldworkers in the form of structured interviews, in the preferred language of the participant.
Calculation of total daily dietary iron intake was performed by the South African Medical Research Council (SAMRC). This was done by combining dietary intake data with the most recent food composition database, which contains the iron content values of fortified foods as per the national food fortification program. The proportion of participants with consumption below the Estimated Average Requirement (EAR) of the Institute of Medicine was classified as having inadequate iron intake in this cohort [24]. To determine supplemental iron intake, participants had to indicate if they were taking any supplements, where they received them, and how often they took them. This information was used to calculate the daily average intake of iron from the supplements. The vast majority of women reported only taking the supplements provided at the antenatal clinic (iron, folic acid and calcium). The routinely provided iron supplement contains 65 mg elemental iron per day in the form of 200 mg dried ferrous sulphate [8].
Household food security
The household food security of participants was assessed using the Household Food Insecurity Access Scale (HFIAS), which included nine questions that ascertained whether members of the household have access to sufficient food or have had to alter their food due to resource limitation during the past four-week period. Household food security was interpreted as ‘secure’, ‘mildly insecure’, ‘moderately insecure’, and ‘severely insecure’ [25].
Hematological biomarkers and laboratory analysis
Capillary blood (approximately 70–100 µL) was collected from the pregnant women using a finger prick into labelled heparin tubes. Immediately after pricking the finger, haemoglobin (Hb) concentrations were measured in the blood sample using the HemoCue Hb 201 + System. Hb concentrations were adjusted for altitude (Bloemfontein is 1300 m above sea level) [26, 27], and anaemia was defined as Hb < 11 g/dL based on the WHO Hb cut-off for pregnancy [27]. Severe anaemia was defined as Hb < 7 g/dL [28], and in such cases, the participants were referred to the nurses at the antenatal clinic for appropriate treatment. Within 30 min of capillary blood collection, plasma aliquots were prepared and stored at 4 °C. The samples were transported daily from the study site in cooler bags with refrigerant gel ice packs to be stored at The University of the Free State, firstly at -20 °C for at most 4 days and then transferred to the − 80 °C freezer at the end of the week for storage until analysis.
The iron status indicators, ferritin and soluble transferrin receptor (sTfR) were analyzed using the Q-Plex™ Human Micronutrient Array (Quansys Bioscience, Utah, USA) at the micronutrient laboratory of the Centre of Excellence for Nutrition at the North-West University [29]. The Q-Plex™ Human Micronutrient Array (7-plex) as previously described by Ngounda et al. is a fully quantitative chemiluminescent assay allowing concurrent measurement of biomarkers used in nutritional assessment [15]. Markers of inflammation, i.e., C-reactive protein (CRP) and alpha-1-acid glycoprotein (AGP) were also analysed. CRP and AGP are acute-phase proteins that act as markers of inflammation, with AGP being a more reliable indicator of chronic inflammation [30]. Inflammatory status was grouped as; (1) healthy (both CRP concentration ≤ 5 mg/L and AGP concentration ≤ 1 g/L); (2) incubation (CRP concentration > 5 mg/L and AGP concentration ≤ 1 g/L); (3) early convalescence (both CRP concentration > 5 mg/L and AGP concentration > 1 g/L); and (4) late convalescence (CRP concentration ≤ 5 mg/L and AGP concentration > 1 g/L) [30, 31]. Elevated inflammation was defined as CRP concentration > 5 mg/L and AGP concentration > 1 g/L [30].
ID was defined as adjusted ferritin concentration < 15 µg/L [32]. Ferritin is an intracellular protein that stores iron, and is influenced by inflammation. Therefore, ferritin concentration was adjusted for inflammation using the correction factors recommended by Thurnham, Northrop-Clewes [30], taking into account CRP > 5 mg/L and AGP > 1 g/L. sTfR is a carrier protein for transferrin, which facilitates the uptake of iron into cells. sTfR increases in ID and indicates the demand for iron and the intensity of erythropoiesis [33]. Iron-deficiency erythropoiesis (IDE) was defined as sTfR > 8.3 µg mg/L [6, 34]. Iron deficiency anaemia (IDA) was defined as ferritin < 15 µg/L and Hb < 11 g/dL [35].
Birth outcomes
Participants were requested to present the Road to Health booklet of the baby to the dietitians at the hospital after delivery for assessment of birth outcomes. Birth outcome information such as gestational age and birth weight were obtained from the booklet. Exposure to HIV at birth was also recorded. Babies born at 37 weeks of gestation or later were classified as term, and those born at < 37 + 0 weeks of gestation (259 days) were classified as premature [36]. Birth weight was classified according to the WHO criteria. Newborns with birth weights < 2500 g were defined LBW [37]. The neonates were further classified according to small, adequate and large for gestational age according to their gestational age and birth weight using the INTERGROWTH 21st programme. Mothers who failed to provide the birth outcome information after delivery were followed up via short message service to remind them of the birth outcome assessment.
Statistical analyses
All data processing and statistical analyses were performed using Statistical Package for Social Sciences software, Version 27. Data were tested for outliers and normality using Q-Q plots, histograms, and the Shapiro-Wilk test. Descriptive statistics, namely frequencies and percentages for categorical data, and medians and 25th (Q1) and 75th (Q3) percentiles for numerical data, were calculated and reported by groups (i.e., preterm vs. term or LBW vs. healthy birth weight or anaemic vs. non-anaemic). Associations were determined by using the Chi-square or Fisher’s exact test for categorical data, and the Mann-Whitney U test and Kruskal-Wallis test for numerical data. P-values of < 0.05 were considered significant. Logistic and linear regression models were used to determine the association of anaemia and iron status and other exposure variables with preterm birth and LBW.
Ethical statement
This study was approved by the Health Sciences Research Ethics Committee of the University of the Free State (Ethics No. UFS-HSD2017/0969) and the Free State Department of Health. All study procedures were in accordance with the guidelines of the Declaration of Helsinki. Participation in the research was voluntary and written informed consent was obtained from all participants.
Results
Characteristics of study participants and birth outcomes
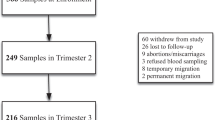
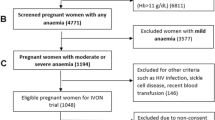
A total of 618 eligible pregnant women were recruited and enrolled for baseline assessment, of which 427 had blood samples available for iron status assessment. Of these, only 205 and 197 participants provided the birth weight and gestational age of their newborn infants. Hence, 53.8% of participants were lost to follow up with missing birth outcome data. The women who had the weight and length outcome data for their babies were significantly older (i.e. 32 (Q1, Q3): 28, 37) years) than those without (i.e. 31 (Q1, Q3): 26, 36) years, p < 0.050. There was no significant difference in anaemia and iron status between the women who had birth outcome data and those who did not.
The characteristics of the study participants by birth outcomes are described in (Table 1). The median (Q1, Q3) age of the pregnant women was 32 (27, 37) years. The median (Q1, Q3) weeks of gestation at enrolment was 32 (26, 36) weeks. At enrolment, pregnant women in their first, second, and third trimesters constituted 3 (0.7%), 114 (26.7%), and 310 (72.6%), respectively. Additionally, 56% of the pregnant women had completed high school and about 62% were unmarried. The median (Q1, Q3) GBMI of the women was 31.3 (24.6, 37.7) kg/m2 and about 55% and 11% of them were obese and overweight, respectively. Meanwhile, over 70% of the pregnant women were food insecure, out of which about 29% were severely food insecure. Over 30% of participants were living with HIV and were taking anti-retroviral treatment.
Out of the neonates with birth outcome data, 22 (10.7%) had LBW (< 2.5 kg) and 27 (13.7%) were born pre-term (< 37 weeks of gestation). Additionally, 26 (13.3%) were born small for gestational age, 145 (74.0%) were born appropriate for gestational age, while 25 (12.8%) were born large for gestational age (Table 2). The median (Q1, Q3) birth weight was 3000 g (2720, 3400), and the median (Q1, Q3) gestational age at birth was 39 (38, 40) weeks. No babies were born before 28 weeks of gestation. Neonates born with LBW were born significantly earlier than those born with healthy birth weight i.e., 36 (Q1, Q3): 34, 37) vs. 39 (Q1, Q3): 38, 40) weeks; p < 0.001. There were no statistical differences in the demographic characteristics between women who delivered preterm and term babies or LBW and healthy birth weight. Nonetheless, mothers of babies born with LBW had a significantly lower GBMI of 25 (Q1, Q3): 22, 32) kg/m2 compared to those who had babies with healthy birth weight i.e., 32 (Q1, Q3): 25.0, 38.2); p = 0.005. There was no difference in the inflammatory, anaemia, and iron status between mothers who delivered preterm or term, or LBW or healthy birth weight. Moreover, no significant differences in anaemia and iron status were found between mothers who delivered neonates born small, appropriate, or large for gestational age (Supplementary table). A significantly higher proportion of babies who were HIV exposed were born preterm (48.2%) than those born at term (25.4%), p = 0.020.
Maternal anaemia, iron and inflammatory status
Approximately 42% of participants were anaemic, 19% had IDA, and 31% were iron deficient (Table 1). Additionally, the median Hb (Q1, Q3) concentration of the mothers was 11.3 (10.2, 12.2) g/dL, and the median (Q1, Q3) ferritin concentration was 22.4 (13.1, 39.5) µg/L (Table 3). As expected, mothers in their first trimester had significantly higher iron stores compared to those in their second and third trimester (p = 0.020). Similarly, mothers in their second trimester recorded significantly higher iron stores than those in their third (p = 0.010) (Table 3). In effect, mothers in their third trimester had a significantly higher plasma sTfR concentration compared to those in their second trimester (p = 0.043). A large proportion of participants (68.6%) presented with elevated CRP (> 5 mg/L). The median (Q1, Q3) plasma CRP concentration was 8.8 (4.0, 18.2) mg/L, with those in the second trimester having a significantly higher CRP concentration compared to those in the third trimester (p < 0.001). Nonetheless, only 2.3% of participants had elevated chronic inflammation (AGP > 1 g/L). Pregnant women living with HIV had increased odds of being anaemic (OR: 2.14; 95%CI: 1.41, 3.247, p < 0.001), iron deficient (OR: 2.19; 95%CI: 1.42, 3.37, p < 0.001) and having IDA (OR: 2.23; 95%CI: 1.36, 3.67, p = 0.002) and IDE (OR: 2.22; 95%CI: 1.16, 4.22; p = 0.015) compared to those living without HIV.
Maternal dietary and supplemental iron intake and anaemia and iron status
Table 4 shows the reported dietary and supplemental intake of iron of the mothers. Majority of participants only consumed the supplements that were routinely provided by the clinic as part of the general antenatal care. In the less than 3% of participants that did report using additional supplements, the iron content of these was added to total intake. The median (minimum-maximum) intake of dietary iron was 16.8 (12.7–20.5) mg/d, which is below the estimated average requirement (EAR) of 22 mg/d [24]. Only 19% of the mothers met the daily EAR for iron through dietary intake. There was no significant difference in the dietary intake of iron between the mothers who were anaemic and non-anaemic, and those who were iron deficient versus those who were not. The median (min-max) daily intake of iron from supplements was 65 (0–65) mg/d, and this was similar across the anaemic, non-anaemic, iron deficient and iron sufficient mothers. On average, the total median (min-max) daily iron intake from both diet and supplements was 81 (8.8-101.8) mg, and the majority (88%) of participants had a total daily iron intake above the Tolerable Upper Intake Level of 45 mg/d for pregnant and lactating women [24]. The proportion who consumed iron above the daily tolerable upper intake was similar across the anaemic, non-anaemic, iron-deficient and iron sufficient groups. A significantly higher proportion of participants who had a history of snuffing, were anaemic (p = 0.006) (Table 4).
Association of maternal anaemia and iron status and other exposure factors with birth outcomes
Table 5 shows the results of the logistic regression analysis of the associations of maternal iron and anaemia status with preterm delivery and LBW. In this sample, no significant association of anaemia and iron status with preterm birth as well as LBW was observed. Furthermore, anaemia, ID and IDE in the second or third trimesters were not associated with preterm delivery or LBW. After adjusting for maternal age, HIV exposure and GBMI, we observed that mothers in the third Hb quartile (Hb between 11.3 and 12.2 g/dL) had a significantly shorter gestation by one week (β-coefficient = -1.15 (95% CI: -2.01, -0.29, p = 0.009), compared to mothers in the highest Hb quartile (Table 6). Additionally, HIV exposure was associated with over two times increased odds for preterm birth (OR: 2.39 (95% CI: 1.01, 5.64), p = 0.047). In the adjusted model, there was a trend for women presenting with inflammation (i.e., CRP > 5 mg/L) to have increased odds for preterm delivery (OR: 2.64 (95%CI: 0.91, 7.62), p = 0.073).
Discussion
In this cross-sectional study of the iron status of pregnant women in Bloemfontein, South Africa, a high prevalence of anaemia and ID of severe and moderate public health significance, respectively, were identified [28, 38], despite the reported intake of iron supplements, thus demonstrating our initial hypothesis that the iron status of pregnant women in Bloemfontein is poor. However, no associations between iron status and preterm delivery or LBW were found, which rejects our initial hypothesis that iron status is linked with poor birth outcomes.
In the current study, which involved pregnant women predominantly in their second and third trimesters, the 42% anaemia prevalence observed was similar to the 44% and 45% anaemia prevalence observed among generally healthy (women living with HIV were excluded), non-smoking pregnant women in their second and third trimesters, respectively, in a study by Symington et al. [6] in Johannesburg, South Africa. Moreover, the median Hb concentration of 11.3 g/dL observed in our study was similar to that of 11.2 g/dL reported in the second and third trimesters in the Johannesburg study [6]. In a systematic review involving 26 studies that investigated the prevalence and risk factors of anaemia in pregnant women in South Africa, a pooled anaemia prevalence of 31% was identified, and ID was reported as the primary risk factor for anaemia, despite the routine intake of iron and folate supplements [11]. In the current study, at an average of 32 weeks of gestation, more than 31% of participants were iron deficient, while 19% had IDA, even though a high intake of iron from supplementation was reported. The Johannesburg study by Symington et al. found a comparable ID prevalence of 19% at 22 weeks of gestation, which increased to 33% by 36 weeks of pregnancy amidst iron supplementation [6].
According to the WHO, daily supplementation of 30 mg to 60 mg of elemental iron is recommended for pregnant women, with the higher dose preferred in settings with anaemia prevalence above 40% to prevent anaemia and the risk of LBW and ID [39]. In accordance with this recommendation, all pregnant women in South Africa are required to receive daily supplementation of oral 200 mg of ferrous sulphate (65 mg of elemental iron) together with 5 mg of folic acid throughout pregnancy for the prevention of anaemia as stipulated in the Basic Antenatal Care Guidelines [8].
During pregnancy, serum ferritin declines, reaching its lowest in the third trimester. This decline in serum ferritin leads to a suppression in hepcidin production for efficient mobilization of maternal iron stores for placental transfer [40]. However, supplementation of iron should attenuate the decline in maternal iron stores in the third trimester [40]. Despite the reportedly high intake of iron from supplements observed in the current study (88% of participants exceeding the Tolerable Upper Intake Level), a high prevalence of anaemia and ID persisted, with participants in their third trimester having a significantly lower plasma ferritin concentration compared to those in their second trimester. Similarly, Symington et al. [6] found that even though there was a 100% compliance (self-reported) to the routine supplementation of 55 mg of iron in their setting, anaemia and ID prevalence doubled over the course of pregnancy. A Ghanaian study observed a similar decline in iron status during pregnancy, despite 82–90% of their participants taking routine iron supplements [41]. This observation of persistent anaemia and ID amidst high iron intake raises concerns about the effectiveness of routine iron supplementation. Several factors such as heightened inflammation and infection which are common in developing countries can lead to poor iron absorption; poor dietary bioavailability, as well as non-compliance to supplementation due to commonly experienced gastrointestinal side effects or stigma associated with taking tablets may contribute to the ineffectiveness of the iron supplementation regime [42, 43]. A high proportion (68.9%) of our participants had elevated acute inflammation (CRP > 5 m/L), which could be evidence of sub-clinical or active infection or obesity-related inflammation. Elevated inflammation caused by infection or obesity increases the production of hepcidin, which causes a restriction in iron absorption and a block of iron release into circulation, resulting in a higher risk of developing anaemia [44]. In the current study, almost 31% of participants were living with HIV, which concurs with the national antenatal HIV prevalence of 30% in South Africa [45]. As observed in this study, the pregnant women who were living with HIV were at more than two times increased odds of having anaemia, ID, IDA and IDE. Several studies have reported a high prevalence of anaemia and ID prevalence in HIV-positive pregnant women [46,47,48]. Aside from inflammation, the absorption of iron can also be inhibited by calcium. In addition to iron and folic acid, 1000 mg of calcium is provided as part of the routine prenatal supplementation, and if taken together with iron, can impede iron absorption [49]. Hence, it is recommended that calcium supplements be taken four hours before or after iron supplements [8], but the possibility of non-adherence to this recommendation is high.
In the present study, anaemia, ID, IDA, IDE were not associated with LBW or preterm birth, although, Hb concentration between 11.3 and 12.2 mg/L was associated with a significantly shorter gestation by one week. Quite similar to our findings, the Johannesburg study reported that anaemia, ID and IDA were not associated with LBW or preterm delivery [6]. However, anaemia and ID at mid-pregnancy were associated with a 207 g and 205 g higher birth weight, while infants born to mothers who had IDE in late pregnancy had a higher birth weight by 178 g [6]. IDE in mid-pregnancy was associated with a higher risk for prematurity (OR: 3.57, 95% CI: 1.24, 10.34) [6]. Furthermore, a study conducted in Moshi Municipality in Tanzania showed no association between maternal anaemia and LBW, preterm birth, and still birth [50]. Additionally, according to a multinational RCT conducted in Benin, Gabon, Mozambique, and Tanzania, maternal anaemia did not appear to be associated with LBW. However, maternal age of less than 19 years and malnutrition were both associated with LBW [51]. In contrast, multiple studies have associated maternal anaemia with LBW and preterm delivery [52,53,54,55]. The inconsistent observations made from various studies could be due to the fact that some studies only supplement iron deficient pregnant women, while others provide supplements to all pregnant women, including those that are iron replete.
There are a number of plausible biological mechanisms that have linked maternal anaemia with LBW. Anaemia (low Hb concentration) during pregnancy restricts oxygen circulation in the body, creating an environment of oxidative stress or chronic hypoxia which may predispose the foetus to intrauterine growth restriction, and consequently LBW [56]. Additionally, ID triggers an increase in the production of norepinephrine, which induces maternal and foetal stress, which in turn activates the release of corticotropin-releasing hormone (CRH), which could increase foetal cortisol production, limiting the growth and length of the foetus [56]. High CRH concentration is a significant risk factor for preterm birth, pregnancy-induced hypertension and eclampsia, and premature rupture of the membranes [56].
The predominant risk factor of LBW is preterm delivery [57, 58]. It is widely known that preterm delivery may be caused by medical conditions such as hypertension, as well as infections including malaria, and HIV [55, 59, 60]. In the current study, HIV infection was associated with an increased risk of preterm birth, similar to the findings of a systematic review and meta-analysis, which showed a significant association between maternal HIV infection, prematurity and LBW, irrespective of antiretroviral drug usage [61]. It is known that HIV infection causes severe immune dysregulation, characterised by altered CD4:CD8 T cell ratios, chronic inflammation and eventually, failure of the immune system [62,63,64]. The human placenta is made up of several immune cells including decidual natural killer cells, CD4 + T, CD8 + T cells, regulatory T cells, and macrophages, some of which play an important role in the inflammatory processes that accompany labour [65]. It is therefore likely that HIV-associated immune dysregulation, co-infections, acute and chronic inflammation, and vascular malperfusion within the placenta and poor placental development and function are reasons for the increased risk of preterm birth and poor intrauterine fetal growth resulting in LBW in pregnant women with HIV [66,67,68]. As observed in this study, elevated inflammation (CRP > 5 mg/L) showed a trend of increased odds of preterm birth. A study conducted in China reported that elevated CRP concentration (> 16 mg/L) in the first trimester was associated with increased odds of preterm birth in their participants (OR = 2.53, 95% CI: 1.14–5.64, p = 0.023) [69].
Our study was limited by the cross-sectional design; hence, we could not investigate the effect of iron status at different time points during the course of pregnancy on birth outcomes. Nonetheless, the current study has some strengths. The findings of this study provide insights into the factors associated with the understudied birth outcomes in the study population, and highlights direction for future research. Another limitation of the study was the high proportion of mothers lost to follow up, and the relatively high percentage of missing birth outcome data. Furthermore, the study was conducted at a specialized antenatal clinic which may not be representative of the general population. Information on the intake of iron supplements was self-reported and could be subject to over-reporting.
Conclusion
In conclusion, anaemia, ID, and IDA prevalence were high in our sample of pregnant women, despite the high intake of supplemental iron. Anaemia and iron status at a median gestational age of 32 weeks were not associated with LBW or preterm birth. However, HIV infection was significantly associated with increased risk of anaemia, ID and IDA, and two times increased odds of preterm birth. The results highlight the need for an evaluation of the current prenatal iron supplementation program, suggesting that research focused on strategies to augment iron absorption and compliance would be important in improving the effectiveness of the supplementation regimen.
Data availability
The dataset will be made available by the corresponding authors upon reasonable request.
Abbreviations
- AGP:
-
α1-acid glycoprotein
- CRP:
-
C-reactive protein
- EAR:
-
Estimated average requirement
- GBMI:
-
Gestational body mass index
- Hb:
-
Haemoglobin
- HFIAS:
-
Household food insecurity access scale
- HIV:
-
Human immunodeficiency virus
- ID:
-
Iron deficiency
- IDA:
-
Iron deficiency anaemia
- IDE:
-
Iron deficiency erythropoiesis
- LBW:
-
Low birth weight
- QFFQ:
-
Quantified food frequency questionnaire
- sTfR:
-
Soluble transferrin receptor
- WHO:
-
World Health Organization
References
Pantopoulos K, Porwal SK, Tartakoff A, Devireddy L. Mechanisms of mammalian iron homeostasis. Biochemistry. 2012;51(29):5705–24.
Yiannikourides A, Latunde-Dada GO. A short review of Iron Metabolism and Pathophysiology of Iron disorders. Med (Basel). 2019;6(3):85.
WHO. The global health observatory, WHO global anaemia estimates, 2021 edition 2023. 2021. Available from: https://www.who.int/data/gho/data/themes/topics/anaemia_in_women_and_children
Bothwell TH. Iron requirements in pregnancy and strategies to meet them123. Am J Clin Nutr. 2000;72(1):S257–64.
Abu-Ouf NM, Jan MM. The impact of maternal iron deficiency and iron deficiency anemia on child’s health. Saudi Med J. 2015;36(2):146–9.
Symington EA, Baumgartner J, Malan L, Wise AJ, Ricci C, Zandberg L, et al. Maternal iron-deficiency is associated with premature birth and higher birth weight despite routine antenatal iron supplementation in an urban South African setting: the NuPED prospective study. PLoS ONE. 2019;14(9):e0221299.
Steyn NP, Wolmarans P, Nel JH, Bourne LT. National fortification of staple foods can make a significant contribution to micronutrient intake of South African adults. Public Health Nutr. 2008;11(3):307–13.
National Department of Health. Guidelines for maternity care in South Africa 2015. Available from: https://health-e.org.za/wp-content/uploads/2015/11/Maternal-Care-Guidelines-2015_FINAL-21.7.15.pdf
National Committee on Confidential Enquiries into Maternal Deaths. Saving mothers 2005–2007: fourth report on confidential enquiries into maternal deaths in South Africa. South Africa: NCCEMD.: Expanded Executive Summary Pretoria; 2007.
Mkhize PZ, Naicker T, Onyangunga OA, Moodley J. Adherence to iron prophylactic therapy during pregnancy in an urban regional hospital in South Africa. South Afr Family Pract. 2019;61(5):203–8.
Dorsamy V, Bagwandeen C, Moodley J. The prevalence, risk factors and outcomes of anaemia in South African pregnant women: a systematic review and meta-analysis. Syst Reviews. 2022;11(1):16.
Stoffel NU, von Siebenthal HK, Moretti D, Zimmermann MB. Oral iron supplementation in iron-deficient women: how much and how often? Mol Aspects Med. 2020;75:100865.
Bullen J, Griffiths E, Rogers H, Ward G. Sepsis: the critical role of iron. Microbes Infect. 2000;2(4):409–15.
Walsh CM, van Rooyen FC. Household food security and hunger in rural and urban communities in the Free State Province, South Africa. Ecol Food Nutr. 2015;54(2):118–37.
Ngounda J, Baumgartner J, Nel M, Walsh CM. Iodine status of pregnant women residing in the urban Free State Province of South Africa is borderline adequate: the NuEMI study. Nutr Res. 2022;98:18–26.
National Directorate of Maternal and Infant Health, Maternal and Infant Program of the Buenos Aires Province and the Directorate of Information of the Province of Neuquén. Programa Nutri Desarrollado en EpiInfo [Nutri Program, Developed in EpiInfo Directorate of Information of the Province of Neuquén]. 2012. Available from: https://www.msal.gov.ar/htm/Site/promin/UCMISALUD/Software/nutri13.ziphttps://www.msal.gov.ar/htm/Site/promin/UCMISALUD/utilidades/util.htm
Davies H, Visser J, Tomlinson M, Rotheram-Borus M, Gissane C, Harwood J, et al. An investigation into utilising gestational body mass index as a screening tool for adverse birth outcomes and maternal morbidities in a group of pregnant women in Khayelitsha. South Afr J Clin Nutr. 2013;26(3):116–22.
Cruz ML, Harris DR, Read JS, Mussi-Pinhata MM, Succi RC. Association of Body Mass Index of HIV-1-Infected pregnant women and infant weight, body Mass Index, length, and Head Circumference: the NISDI Perinatal Study. Nutr Res. 2007;27(11):685–91.
MacIntyre UE, Venter CS, Vorster HH, Steyn HS. A combination of statistical methods for the analysis of the relative validation data of the quantitative food frequency questionnaire used in the THUSA study. Transition, Health and Urbanisation in South Africa. Public Health Nutr. 2001;4(1):45–51.
Wentzel-Viljoen ELR, Kruger A. Using different approaches to assess the reproducibility of a culturally sensitive quantified food frequency questionnaire. South Afr J Clin Nutr. 2011;24:143–8.
MacIntyre U, Kruger H, Venter C, Vorster H. Dietary intakes of an African population in different stages of transition in the North West Province, South Africa: the THUSA study. Nutr Res. 2002;22(3):239–56.
Hattingh Z, Le Roux M, Nel M, Walsh C. Assessment of the physical activity, body mass index and energy intake of HIV-uninfected and HIV-infected women in Mangaung, Free State province. South Afr Family Pract. 2014;56(3):196–200.
Robb L, Joubert G, Jordaan EM, Ngounda J, Walsh CM. Choline intake and associations with egg and dairy consumption among pregnant women attending a high-risk antenatal clinic in South Africa: the NuEMI study. BMC Pregnancy Childbirth. 2021;21(1):833.
Institute of Medicine. In: Otten JJ, Hellwig JP, Meyers LD, editors. Dietary reference intakes: the essential guide to nutrient requirements. Washington, DC: National Academies; 2006. p. 1344.
Coates J, Swindale A, Bilinsky P. Household Food Insecurity Access Scale (HFIAS) for measurement of Household Food Access: Indicator Guide. Washington, D.C.: Food and Nutrition Technical Assistance Project, Academy for Educational Development; 2007.
Silubonde TM, Baumgartner J, Ware LJ, Malan L, Smuts CM, Norris S. Adjusting haemoglobin values for Altitude maximizes combined sensitivity and specificity to Detect Iron Deficiency among women of Reproductive Age in Johannesburg, South Africa. Nutrients. 2020;12(3).
WHO. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity: Vitamin and mineral nutrition information system 2011. Available from: https://apps.who.int/iris/bitstream/handle/10665/85839/WHO_NMH_NHD_MNM_11.1_eng.pdf
WHO. Guideline on haemoglobin cutoffs to define anaemia in individuals and populations. Geneva: World Health Organisation; 2024.
Brindle E, Fujita M, Shofer J, O’Connor KA. Serum, plasma, and dried blood spot high-sensitivity C-reactive protein enzyme immunoassay for population research. J Immunol Methods. 2010;362(1–2):112–20.
Thurnham DI, Northrop-Clewes CA, Knowles J. The use of adjustment factors to address the impact of inflammation on vitamin A and iron status in humans. J Nutr. 2015;145(5):s1137–43.
Namaste SM, Rohner F, Huang J, Bhushan NL, Flores-Ayala R, Kupka R, et al. Adjusting ferritin concentrations for inflammation: biomarkers reflecting inflammation and nutritional determinants of Anemia (BRINDA) project. Am J Clin Nutr. 2017;106(Suppl 1):s359–71.
WHO. Serum ferritin concentrations for the assessment of iron status and iron deficiency in populations. Vitamin and mineral nutrition information system Geneva: WHO. 2011. Available from: http://www.who.int/vmnis/indicators/serum_ferritin.pdf
Northrop-Clewes CA, Thurnham DI. Biomarkers for the differentiation of anemia and their clinical usefulness. J Blood Med. 2013;4:11–22.
Erhardt JG, Estes JE, Pfeiffer CM, Biesalski HK, Craft NE. Combined Measurement of Ferritin, Soluble Transferrin Receptor, Retinol binding protein, and C-Reactive protein by an Inexpensive, Sensitive, and simple sandwich enzyme-linked immunosorbent assay technique. J Nutr. 2004;134(11):3127–32.
WHO. Nutritional Anaemias: Tools for Effective Prevention. Geneva, Switzerland: World Health Organization; 2017.
March of Dimes P. Save the children,. Born too soon: The Global Action Report on Preterm Birth. Geneva,Switzerland: Geneva: World Health Organization; 2012.
UNICEF, WHO. Low birthweight: Country, Regional and Global estimates. New York: UNICEF; 2004.
WHO. WHO guideline on use of ferritin concentrations to assess iron status in individuals and populations. Geneva: World Health Organisation; 2020.
WHO. Antenatal iron supplementation Geneva2023 Available from: https://www.who.int/data/nutrition/nlis/info/antenatal-iron-supplementation#:~:text=The%20suggested%20dose%20is%20120,early%20as%20possible%20after%20conception
Fisher AL, Nemeth E. Iron homeostasis during pregnancy†‡. Am J Clin Nutr. 2017;106:S1567–74.
Pobee RA, Setorglo J, Klevor M, Murray-Kolb LE. The prevalence of anemia and iron deficiency among pregnant Ghanaian women, a longitudinal study. PLoS ONE. 2021;16(3):e0248754.
Silubonde TM, Draper CE, Baumgartner J, Ware LJ, Smuts CM, Norris SA. Barriers and facilitators of micronutrient supplementation among non-pregnant women of reproductive age in Johannesburg, South Africa. PLOS Glob Public Health. 2022;2(11):e0001310.
Hurrell RF. Influence of inflammatory disorders and infection on iron absorption and efficacy of iron-fortified foods. Nestle Nutr Inst Workshop Ser. 2012;70:107–16.
Ganz T. Anemia of inflammation. N Engl J Med. 2019;381(12):1148–57.
Woldesenbet SA, Lombard C, Manda S, Kufa T, Ayalew K. M. C, The 2019 National Antenatal Sentinel HIV Survey, South Africa, National Department of Health. South Africa: National Department of Health. 2021.
Tunkyi K, Moodley J. Prevalence of anaemia in pregnancy in a regional health facility in South Africa: research. South African Medical Journal. 2016;106(1):101 – 4.
Msuya SE, Hussein TH, Uriyo J, Sam NE, Stray-Pedersen B. Anaemia among pregnant women in northern Tanzania: prevalence, risk factors and effect on perinatal outcomes.Tanzania Journal of Health Research. 2011;13(1):33 – 9.
Friis H, Gomo E, Kæstel P, Ndhlovu P, Nyazema N, Krarup H, et al. HIV and other predictors of serum folate, serum ferritin, and hemoglobin in pregnancy: a cross-sectional study in Zimbabwe. The American journal of clinical nutrition. 2001;73(6):1066 – 73.
Lönnerdal B. Calcium and iron absorption–mechanisms and public health relevance.Int J Vitam Nutr Res. 2010;80(4–5):293–9.
Stephen G, Mgongo M, Hussein Hashim T, Katanga J, Stray-Pedersen B, Msuya SE.Anaemia in Pregnancy: Prevalence, Risk Factors, and Adverse Perinatal Outcomes in Northern Tanzania. Anemia. 2018;2018:1846280.
Ghyslain M-N, Jean Rodolphe M, Raquel G, Smaila O, Mwaka AK, Rella Zoleko M, et al. Young adolescent girls are at high risk for adverse pregnancy outcomes in sub-Saharan Africa: an observational multicountry study. BMJ Open. 2016;6(6):e011783.
Engidaw MT, Eyayu T, Tiruneh T. The effect of maternal anaemia on low birth weight among newborns in Northwest Ethiopia. Scientific Reports. 2022;12(1):15280.
Lone FW, Qureshi RN, Emmanuel F. Maternal anaemia and its impact on perinatal outcome in a tertiary care hospital in Pakistan. East Mediterr Health J. 2004;10(6):801–7.
Figueiredo A, Gomes-Filho IS, Silva RB, Pereira PPS, Mata F, Lyrio AO, et al.Maternal Anemia and Low Birth Weight: A Systematic Review and Meta-Analysis. Nutrients. 2018;10(5).
van den Broek NR, Jean-Baptiste R, Neilson JP. Factors Associated with Preterm,Early Preterm and Late Preterm Birth in Malawi. PLOS ONE. 2014;9(3):e90128.
Allen LH. Biological Mechanisms That Might Underlie Iron’s Effects on Fetal Growth and Preterm Birth. The Journal of Nutrition. 2001;131(2):581S – 9S.
Tshotetsi L, Dzikiti L, Hajison P, Feresu S. Maternal factors contributing to low birth weight deliveries in Tshwane District, South Africa. PLOS ONE. 2019;14(3):e0213058.
Anil K, C., Basel PL, Singh S. Low birth weight and its associated risk factors:Health facility-based case-control study. PLoS One. 2020;15(6):e0234907.
Yingjuan L, Peng J, Liu Y, Xia W, Chen S, Yongcheng S, et al. Association between maternal HIV infection and the risks of preterm birth and low birth weight in Chengdu,China: a propensity score matching approach. BMJ Open. 2023;13(9):e071205.
An H, Jin M, Li Z, Zhang L, Li H, Zhang Y, et al. Impact of gestational hypertension and pre-eclampsia on preterm birth in China: a large prospective cohort study. BMJ Open. 2022;12(9):e058068.
Xiao P-L, Zhou Y-B, Chen Y, Yang M-X, Song X-X, Shi Y, et al. Association between maternal HIV infection and low birth weight and prematurity: a meta-analysis of cohort studies. BMC Pregnancy and Childbirth. 2015;15(1):246.
Okoye AA, Picker LJ. CD4(+) T-cell depletion in HIV infection: mechanisms of immunological failure. Immunol Rev. 2013;254(1):54–64.
Hileman CO, Funderburg NT. Inflammation, Immune Activation, and Antiretroviral Therapy in HIV. Curr HIV/AIDS Rep. 2017;14(3):93–100.
Demers KR, Makedonas G, Buggert M, Eller MA, Ratcliffe SJ, Goonetilleke N, et al. Temporal Dynamics of CD8 + T Cell Effector Responses during Primary HIV Infection.PLoS Pathog. 2016;12(8):e1005805.
Gomez-Lopez N, StLouis D, Lehr MA, Sanchez-Rodriguez EN, Arenas-Hernandez M. Immune cells in term and preterm labor. Cell Mol Immunol. 2014;11(6):571 – 81.
Ikumi NM, Matjila M, Gray CM, Anumba D, Pillay K. Placental pathology in women with HIV. Placenta. 2021;115:27–36.
Ikumi NM, Malaba TR, Pillay K, Cohen MC, Madlala HP, Matjila M, et al. Differential impact of antiretroviral therapy initiated before or during pregnancy on placenta pathology in HIV-positive women. Aids. 2021;35(5):717 – 26.
Visser L, van Buggenum H, van der Voorn JP, Heestermans L, Hollander KWP, Wouters M, et al. Maternal vascular malperfusion in spontaneous preterm birth placentas related to clinical outcome of subsequent pregnancy. J Matern Fetal Neonatal Med. 2021;34(17):2759 – 64.
Huang S, Tian J, Liu C, Long Y, Cao D, Wei L, et al. Elevated C-reactive protein and complement C3 levels are associated with preterm birth: a nested case–control study in Chinese women. BMC Pregnancy and Childbirth. 2020;20(1):131.
Acknowledgements
We appreciate the contribution of all the fieldworkers, Michelle Du Plooy, Desiré Brand, and Khanyi Khumalo for their hard work and dedication during data collection. We also thank the staff of the antenatal clinic at Pelonomi Regional Hospital and the participants for their support.
Funding
This project was financially supported by The Department of Nutrition and Dietetics, University of the Free State, Bloemfontein, South Africa.
Author information
Authors and Affiliations
Contributions
J. A. C.: conceptualization, data analysis, interpretation of results and manuscript preparation. J. N.: conceptualization, methodology, data collection, assistance with draft manuscript preparation. J. B.: laboratory analysis, interpretation of results. L. R.: coding and interpretation of dietary data. M. J.: coding and interpretation of dietary data and birth outcome data. C. M. W.: conceptualization, methodology, Principal Investigator All authors read and edited the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval for the study was obtained from the Health Sciences Research Ethics Committee of the University of the Free State (Ethics No. UFS-HSD2017/0969) and the Free State Department Health. Participation in the research was voluntary and written informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Carboo, J.A., Ngounda, J., Baumgartner, J. et al. Iron status, anemia, and birth outcomes among pregnant women in urban Bloemfontein, South Africa: the NuEMI study. BMC Pregnancy Childbirth 24, 650 (2024). https://doi.org/10.1186/s12884-024-06845-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-024-06845-w