Abstract
Background
Epithelial ovarian cancer (EOC) is one of the deadliest gynaecological malignancies worldwide. The aim of this retrospective study was to create a predictive scoring model based on simple immunological and inflammatory parameters to predict overall survival (OS) and progression-free survival (PFS) in patients with EOC.
Methods
We obtained 576 EOC patients and randomly assigned them to the training set (n = 405) and the validation set (n = 171) in a ratio of 7:3. We retrospectively evaluated the association between PIV and OS and PFS using a novel immunoinflammatory marker, according to the optihmal treshold of PIV, we divided the patients into two different subgroups, high PIV (PIV > 254.9) and low PIV (PIV ≤ 254.9). Pan-immune Inflammatory Value (PIV) was computed as follows: neutrophil count (109/L) × platelet count (109/L) × monocyte count (109/L)/lymphocyte count (109/L). Then developed a simple score prediction model based on several independent prognostic parameters using Cox regression analysis. We used receiver operator characteristic (ROC) curves, calibration plots, and decision analysis (DCA) curves to evaluate the performance of the model. Finally, we used Kaplan-Meier curves to ensure that the model could distinguish well between low- and high-risk groups.
Results
There was a significant difference in survival outcomes between high PIV (PIV > 310.2) and low PIV (PIV ≤ PIV310.2) (3-year survival rates of 61.34% and 76.71%, respectively); 5-year OS, 25.21% and 51.14%, respectively; 3-year PFS, 40.90% and 65.30%; 5-year PFS, 19.33% and 39.73%, respectively). Column plots of OS and PFS were constructed using independent prognostic factors. In the training module, the 3-, 5-, and 10-year AUCs for OS and PFS column charts were 0.713, 0.796, 0.839, and 0.730, 0.799, 0.826, respectively.In the validation cohort, the 3-, 5-, and 10-year AUCs for OS and PFS column charts were 0.676, 0.803, 0.685, and 0.700, respectively, 0.754, 0.727. The calibration curves showed good agreement between predicted survival and actual observations. The decision analysis curves also showed that the current model has good accuracy and clinical applicability. 3-year OS was 61.34% and 76.71%, respectively; 5-year OS was 25.21% and 51.14%, respectively; 3-year PFS was 40.90% and 65.30%, respectively; 5-year PFS was 19.33% and 39.73%, respectively.
Conclusions
We constructed and validated a PIV-based nomogram to predict OS and PFS in EOC patients, with a view to helping gynaecologists converge on oncologists in their treatment and follow-up expertise in epithelial ovarian cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ovarian cancer (OC) is one of the deadliest gynaecological malignancies in women worldwide, with an estimated 19,710 new cases and 13,270 deaths in the United States by 2023 [1]. EOC is the major pathological subtype, accounting for more than 90% of OC cases and is most common in postmenopausal women [2]. The five-year survival rate for the EOC is less than 50% despite the application of advanced medical techniques and drugs [3, 4]. Therefore, it is important to define survival factors and establish survival prediction models to make better clinical decisions and accurately assess clinical survival for the benefit of elderly EOC patients.
Nomograms are comprehensive and easy-to-read models that are widely used tools to predict the prognosis of cancer patients [5,6,7]. Unlike the International Federation of Gynaecology and Obstetrics (FIGO) staging system, the column-diagram model can predict the survival of individual patients. Currently, several column-row diagrams have been created for younger EOC, postoperative metastasis, and distant metastasis patients, but these are publicly available data from the Surveillance, Epidemiology, and End Results (SEER) database, and studies using Chinese data are scarce [8,9,10]. Therefore, it is important to develop column-line diagrams specifically for Chinese EOC patients to improve accuracy and utility.
Many studies have shown that inflammatory factors such as IL-6 and TGF-β, the inflammatory response and the immune system are involved in the development and progression of a variety of cancers, such as cholangiocarcinoma and colitis-associated colorectal cancer [11, 12]. Studies have shown that macrophages are an important component of the immune-inflammatory response and may promote tumourigenesis in colorectal cancer through their involvement in inflammatory mechanisms [13]. Studies have also shown that haematological parameters, such as lymphocyte levels, are promising biomarkers of the body’s immune and inflammatory status [14]. Recently, significant progress has been made in the study of immune-inflammatory biomarkers (IIBs) that may influence the prognosis of ovarian cancer compared to traditional tumour-related biomarkers. Several IIBs readily available in blood, including neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR) and systemic immune inflammation index (SII), have been identified as potential independent prognostic factors for ovarian cancer [15,16,17].
Due to the complex interaction between tumour and host inflammatory immune response, the above-mentioned indicators based on simple calculations have limited prognostic value [18]. The level of pan-immune inflammation (PIV), a novel integrated biomarker including neutrophil, platelet, monocyte and lymphocyte counts, was found to be superior to other known IIBs as a powerful predictor of survival outcome in patients with metastatic colorectal cancer [19, 20]. Currently, only one study on PIV in ovarian cancer was retrieved, and the conclusions of that study were the first to find that high PIV was associated with an increased risk of death in patients with epithelial ovarian cancer, and that author had similar findings to those in this paper, although that study was based on the results of 158 patients in Europe [21]. Unlike that study, our study was based on 576 patients in China and constructed a nomogram for OS and PFS in epithelial ovarian cancer.
Methods
Patients
This retrospective study included a total of 576 EOC patients treated at Xijing Hospital from January 2010 to December 2019. Inclusion criteria were as follows Patients with epithelial ovarian cancer whose pathological diagnosis met the FIGO2014 ovarian tumour classification criteria; data including serum liver function, peripheral blood haematology, and relevant tumour marker tests measured at Xijing Hospital within 1 week before the first treatment; patients with epithelial ovarian cancer diagnosed and operated on for the first time at Xijing Hospital; age over 18 years; and complete clinical and follow-up data. Exclusion criteria: severe infection, blood diseases, autoimmune diseases, hepatocellular carcinoma, cirrhosis, hepatitis or other severe liver and kidney diseases, other concomitant malignancies, non-surgical systemic chemotherapy, patients who could not be further traced or died within 1 month after the first treatment. Due to the retrospective nature of this study, the ethics committee waived the requirement of written informed consent.
Data collection and definitions
The patient’s laboratory data were verified through the case history system and recorded in detail in excel. Laboratory data were collected one week prior to treatment, while clinicopathological data were collected from the patient’s medical record. The formula for each metric was as follows: PIV = neutrophil count (109/L) × platelet count (109/L) × monocyte count (109/L)/lymphocyte count (109/L); HALP = haemoglobin (g/L) × albumin(g/L) × lymphocyte count (109/L) / platelet count (109/L); SII = platelet count (109/L) × neutrophil count/lymphocyte count ( 109/L); NLR = neutrophil count (109/L)/ lymphocyte count (109/L); PLR = platelet count (109/L)/ lymphocyte count (g/L); PNI = albumin(g/L) + 5 × lymphocyte count(109/L); FAR = fibrinogen(g/L)/albumin(g/L); LMR = lymphocyte count(109/L)/monocyte count(109/L).
Follow up
Follow-up was conducted via telephone or routine outpatient monitoring systems to record the patient’s condition or cause and date of death (if the patient died). The endpoints of the study were OS, defined as the time between the start of treatment and death from any cause, and PFS, defined as the time between the start of treatment and the first progression of disease/death. The last date of follow-up for all surviving patients was considered the endpoint of the study. For patients who did not reach the endpoint, the last follow-up date was considered the study endpoint.
Statistical analysis
In this study, the optimal cut-off values for age, PIV, etc. were determined using X-tile software; based on previous literature and clinical work, CA125 levels were classified into three categories: ≤35 IU/mL, > 35 and ≤ 600 IU/mL, and > 600 IU/mL, and ascites volume was classified into two categories: <1000 mL and ≥ 1000 mL.
All statistical analyses in this study were conducted using R software (version 4.1.0) and SPSS 21.0. The chi-square test and Fisher’s exact test were used to compare the baseline characteristics of the training and validation groups. Correlations between clinicopathological variables and prognosis were analysed using one-way Cox regression analysis. Then, multifactor Cox regression analysis was performed to find independent prognostic factors in EOC patients (p < 0.05). Finally, we created a column chart based on these independent prognostic variables.
ROC, calibration curve, and DCA were calculated with R software. Among them, ROC and calibration curve were used to evaluate the discrimination power and predictive efficiency of the column line chart. DCA was also used to evaluate the predictive ability and validity of the columnar line chart compared with the traditional FIGO staging system. A new risk stratification was performed based on the total score of the columnar line chart, then patients were classified into low-risk and high-risk groups. The log-rank test and Kaplan-Meier plots were used to compare the survival differences between each risk stratification group.
Results
Clinicopathological characteristics of the patient of EOC
Based on the inclusion and exclusion criteria, a total of 576 EOC patients were finally enrolled and randomly assigned to the training set (n = 405) and validation set (n = 171) at a ratio of 7:3. The clinicopathological characteristics of the patients are shown in Table 1, with a mean age of 52 years, 92 with NACT and 484 without NACT, 109 laparoscopic and 467 open, 235 with lymph node metastasis, 304 without metastasis, 37 unknown, 454 with ovarian plasmacytoma, 107 without plasmacytoma, and 15 with mixed carcinoma; the International Federation of Gynecological and Obstetrics and Gynecology Using the 2014 FIGO staging criteria, there were 113 cases of stage I, 55 cases of stage II, 363 cases of stage III, and 45 cases of stage IV 491 patients underwent satisfactory tumour subtraction (residual lesion < 1 cm), and 85 cases of unsatisfactory resection (residual lesion ≥ 1 cm); there were 387 patients with ascites and 189 patients without ascites. During follow-up, 224 of 576 patients (38.9%, 224/576) relapsed and 24 patients were metastasis-free, and 24 patients with mixed ovarian plasmacytoma were metastasis-free. During follow-up, 224 (38.9%, 224/576) of the 576 patients relapsed and 249 (43.2%, 249/576) died, resulting in a median progression-free survival (PFS) of 36.7 months and a 3-year cumulative overall survival rate of 67.4%; 22 patients were treated with olaparib/nilaparib(parp inhibitors), 14 patients with two or more tumour-sparing operations, and 13 patients with radiotherapy; 398 patients were platinum-sensitive, 128 were platinum-resistant, and 50 cases were unknown. Among platinum-resistant patients, 80 patients were treated with platinum in combination with bevacizumab or with bevacizumab alone.
Independent prognostic factors in patients with EOC
Training set unidirectional multifactor Cox analysis identified independent prognostic factors associated with OS and PFS, with six variables identified as independent prognostic factors associated with OS (P < 0.05), including FIGO stage, positive lymph nodes, histological type, pre-treatment CA125 levels, PIV and ascites, and all these independent prognostic factors were incorporated into the construction of a nomogram predicting OS in patients with EOC. Five variables were identified as independent prognostic indicators of PFS (FIGO stage, histological type, pre-treatment CA125 value, PIV and surgical modality), Since laparoscopic surgery probably occurs mostly in FIGO stage I, which has a significantly better prognosis than patients in other stages, and the ultimate goal of surgery is to achieve maximum cytopenias through volume reduction surgery, which may have a large bias, the factor of surgical modality was deleted in this study. Details are provided in Tables 2 and 3.
Development and validation of column line diagrams
A nomogram was created to predict 3-, 5-, and 10-year OS and PFS in EOC patients based on the identified independent prognostic factors. The total score for all variables was calculated to derive the 3-, 5-, and 10-year probabilities of OS and PFS. Figures 1 and 2 are examples of using nomograms to predict overall survival and progression-free survival for specific patients.
Nomogram for predicting 3-year, 5-year,10-year overall survival. FIGO, International Federation of Gynecology and Obstetrics. LNM, Lymph Node Metastasis. Histological type, Non-serous incildes mucinous, endometrioid and clear cell carcinomas, Serous inciudes high-grade plasmacytoid carcinoma and low-grade plasmacytoid carcinoma, Other includes adenocarcinoma and plasma mucinous carcinoma. PIV Pan Immune Inflammation Value
The calibration curves for the training and validation cohorts showed that the actual observed survival was in good agreement with the survival predicted by the nomogram (Fig. 3). The ROC curves for predicting 3-, 5-, and 10-year OS in the training cohort showed AUC values of 0.713, 0.796, and 0.839, respectively, while in the validation cohort they were 0.676, 0.803, and 0.685. The AUC for predicting 3-, 5-, and 10-year PFS in the training and validation cohorts were 0.730, 0.799, 0.826, 0.700, 0.754, and 0.727, respectively (Fig. 4), indicating that thermography has good discriminatory ability.
Calibration curves for nomogram of the 3-(A), 5-(B), 10-year (C) overall survival in training set. Calibration plots for nomogram of the 3-(D), 5-(E)-, 10-year (F) overall survival in validation set. Calibration curves for nomogram of the 3-(G), 5-(H), 10-year (I) progression-free survival in training set. Calibration plots for nomogram of the 3-(J), 5-(K)-, 10-year (L) progression-free survival in validation set
Receiver operating characteristic curves for nomogram of the 3-, 5-, 10-year overall survival in training set (A). Receiver operating characteristic curves for nomogram of the 3-, 5-, 10-year overall survival in validation set (B). Receiver operating characteristic curves for nomogram of the 3-, 5-, 10-year progression-free survival in training set (C). Receiver operating characteristic curves for nomogram of the 3-, 5-, 10-year progression-free survival in validation set (D)
The horizontal dotted line in the DCA plot all samples did not receive any intervention, the slanted dotted line indicates that all samples received the intervention, and if the curves are very close to the two extreme curves, it suggests that they are ineffective. If all the benefits of a model are higher than the extreme curves, it suggests that the model has a high application value. As seen from the DCA plot, the proposed model curve is farther away from the two extreme curves than the FIGO stage curve, indicating that the positive net clinical benefit of this model is better than that of FIGO stage (Fig. 5).
Decision curve analysis for the nomogram and FIGO stage in prediction overall survival of patients at 3-(A), 5-(B), 10-year (C) point in the training cohort. Decision curve analysis for the nomogram and FIGO stage in prediction overall survival of patients at 3-(D), 5-(E), 10-year (F) point in the validation cohort. Decision curve analysis for the nomogram and FIGO stage in prediction progression-free survival of patients at 3-(G), 5-(H), 10-year (I) point in the training cohort. Decision curve analysis for the nomogram and FIGO stage in prediction progression-free survival of patients at 3-(J), 5-(K), 10-year (L) point in the validation cohort
Risk stratification of EOC patients
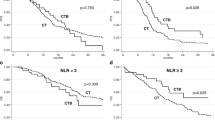
The Kaplan-Meier curves showed statistically significant discriminatory power in both the training and validation subgroups in predicting OS and PFS in patients with EOC, whereas the FIGO staging system was less able to discriminate between the risk of death, particularly between stage I and II also III and stage IV (Figs. 6 and 7).
Discussion
PIV is a new indicator of combined immuno-inflammatory nutrition that integrates four haematological markers (platelets, neutrophils, monocytes and lymphocytes) and may reflect systemic inflammatory status more comprehensively and yield high predictive accuracy, which has been explored in several studies [19, 22]. One study retrospectively analysed data from 49 patients with stage I-III Merkel cell carcinoma and found PIV to be a predictor of tumour recurrence [23]. With regard to antitumour therapy with ICIs, the predictive value of PIV in survivor cancers has been recognised, with a retrospective study analysing data from 163 patients with metastatic colorectal cancer receiving immunotherapy and finding that patients with high PIV levels had poorer survival [24]. One study showed that low PIV level values predicted better chemotherapy response and survival in breast cancer patients receiving neoadjuvant chemotherapy [25]. Another study found that PIV was a new effective predictor of OS in HER-2 positive advanced BC patients treated with first-line trastuzumab-patuzumab biochemotherapy [22]. Few studies have been reported on PIV levels to date, as it is a relatively new biomarker, and it has been studied more in colon and breast cancer and less in ovarian cancer, which was explored in this study in relation to the prognosis of epithelial ovaries.
Most studies have found age to be an independent prognostic factor for EOC [26]. Elderly patients are in poorer physical condition, often with comorbid respiratory and circulatory diseases, may not be able to tolerate surgery and subsequent adjuvant therapy, and are more prone to complications of surgery and chemotherapy; therefore, elderly patients are often treated conservatively and their survival rates are lower [27]. However, age was not found to be a prognostic correlate of EOC patients in this study, which may be due to the fact that older patients may have been excluded from this study without surgery or insufficient course of chemotherapy, and the age distribution was more concentrated, with a median age of 52 years old, a mean age of 52.1 years old, and only 22 cases of patients aged 70 and above, so the number of older patients in this study has yet to be further followed up with clinical data to be Supplementation.
HE4 is a relatively new cancer-related biomarker with better value than CA125 in predicting the prognosis of ovarian cancer patients as well as in early screening and monitoring of recurrence [28]. HE4 may provide a suitable method for the diagnosis of OC, but further large prospective cohort studies are needed to better elucidate the diagnostic and prognostic role of HE4 [29]. Due to the lack of information on HE4 in a significant proportion of cases (> 20%), HE4 has not been included in this study and needs to be supported by follow-up cases.
A number of studies have explored the significance of inflammatory indicators (NLR, PLR, SII, etc.) in guiding the prognosis of ovarian cancer patients [30]. It has also been found that PNR and LMR are better prognostic indicators for ovarian cancer patients compared to NLR, PLR and SII [17].
In this study, we found statistical differences in OS and PFS of ovarian cancer between high and low HALP, PLR, FAR, PNI, NLR, and SII groups, but because PIV is a better predictor and has been studied less in ovarian cancer, this study included PIV as a representative of immunoinflammatory indexes in the prediction of the column-line graph model, and the results also suggested that PIV has a better predictive value.
This study has several limitations. Firstly, there are inevitable limitations due to the nature of a retrospective observational design; secondly, the number of patients included in this study was relatively limited; thirdly, the patients included in this study were from a single cancer centre; therefore, potential selection bias may lead to data that do not reflect the true distribution of PIV values across the entire cohort.
In addition, it is important to note that although we built our model based on a randomised dichotomy (7:3), we used a training cohort to build the model and a test cohort to validate the model. We also made different efforts to validate our results: we tried to validate the results described in this study using different cohorts from publicly available databases. We tried to check publicly available databases such as the Surveillance, Epidemiology, and End Results (SEER) database and The Cancer Genome Atlas (TCGA), but none of these databases contain laboratory data (such as platelet counts). To our knowledge, there is no publicly available open database that contains routine preoperative laboratory data. Also, unfortunately, we have not been able to obtain sufficient external validation data to support our findings to date. However, we are actively seeking collaboration with other centres to confirm our results. These are limitations that must be taken into account.
Conclusion
We constructed a new PIV-based nomogram to predict OS and PFS in EOC patients, which can help clinicians accurately determine patients’ prognosis, answer patients’ consultations, and help patients make clinical judgements.
Data availability
Data supporting the results of this study is available upon request from the corresponding author. The data is not publicly available due to privacy and ethical constraints. These data also pertain to unpublished research. However, these data involve privacy issues for some patients and are not shared publicly.
References
Siegel RL, Miller KD, Wagle NS, et al. Cancer statistics, 2023. CA Cancer J Clin. 2023;73(1):17–48.
Sankaranarayanan R, Ferlay J. Worldwide burden of gynaecological cancer: the size of the problem. Best Pract Res Clin Obstet Gynaecol. 2006;20(2):207–25.
Kurnit KC, Fleming GF, Lengyel E. Updates and New options in Advanced Epithelial Ovarian Cancer Treatment. Obstet Gynecol. 2021;137(1):108–21.
Cress RD, Chen YS, Morris CR, et al. Characteristics of long-term survivors of epithelial ovarian Cancer. Obstet Gynecol. 2015;126(3):491–7.
Touijer K, Scardino PT. Nomograms for staging, prognosis, and predicting treatment outcomes. Cancer. 2009;115(13 Suppl):3107–11.
Balachandran VP, Gonen M, Smith JJ, et al. Nomograms in oncology: more than meets the eye. Lancet Oncol. 2015;16(4):e173–80.
Madsen LT. Cancer Prediction Nomograms for Advanced practitioners in Oncology. J Adv Pract Oncol. 2014;5(5):380–2.
Gao J, Wang S, Li F, et al. Nomograms for Predicting overall survival and Cancer-specific survival of young patients with epithelial ovarian Cancer: analysis based on SEER Program. Adv Ther. 2022;39(1):257–85.
Zhang T, Zhu L. Nomogram for predicting postoperative cancer-specific early death in patients with epithelial ovarian cancer based on the SEER database: a large cohort study. Arch Gynecol Obstet. 2022;305(6):1535–49.
Wang B, Wang S, Ren W. Development and validation of a nomogram to predict survival outcome among epithelial ovarian cancer patients with site-distant metastases: a population-based study. BMC Cancer. 2021;21(1):609.
Landskron G, De la Fuente M, Thuwajit P, et al. Chronic inflammation and cytokines in the tumor microenvironment. J Immunol Res. 2014;2014:149185.
Greten FR, Grivennikov SI. Inflammation and Cancer: triggers, mechanisms, and Consequences. Immunity. 2019;51(1):27–41.
Scheurlen KM, Billeter AT, O’Brien SJ, et al. Metabolic dysfunction and early-onset colorectal cancer - how macrophages build the bridge. Cancer Med. 2020;9(18):6679–93.
Ma X, Jia C, Fu D et al. Analysis of hematological traits in polled yak by Genome-Wide Association Studies using individual SNPs and Haplotypes. Genes (Basel), 2019,10(6).
Zhang CL, Jiang XC, Li Y, et al. Independent predictive value of blood inflammatory composite markers in ovarian cancer: recent clinical evidence and perspective focusing on NLR and PLR. J Ovarian Res. 2023;16(1):36.
Tian C, Song W, Tian X, et al. Prognostic significance of platelet-to-lymphocyte ratio in patients with ovarian cancer: a meta-analysis. Eur J Clin Invest. 2018;48(5):e12917.
Song Q, Xu SX, Wu JZ, et al. The preoperative platelet to neutrophil ratio and lymphocyte to monocyte ratio are superior prognostic indicators compared with other inflammatory biomarkers in ovarian cancer. Front Immunol. 2023;14:1177403.
Nikolaou K, Sarris M, Talianidis I. Molecular pathways: the complex roles of inflammation pathways in the development and treatment of liver cancer. Clin Cancer Res. 2013;19(11):2810–6.
Fuca G, Guarini V, Antoniotti C, et al. The Pan-immune-inflammation Value is a new prognostic biomarker in metastatic colorectal cancer: results from a pooled-analysis of the Valentino and TRIBE first-line trials. Br J Cancer. 2020;123(3):403–9.
Guven DC, Sahin TK, Erul E et al. The Association between the Pan-immune-inflammation Value and Cancer Prognosis: a systematic review and Meta-Analysis. Cancers (Basel), 2022,14(11).
El Bairi K, Kharmach I, Zaimi A et al. 49P first report on pan-immune-inflammation value as a new prognostic factor in ovarian cancer: a biomarker analysis of OVANORDEST-1 study. ESMO Open, 2023, 8(1).
Ligorio F, Fuca G, Zattarin E et al. The Pan-immune-inflammation-value predicts the survival of patients with human epidermal growth factor receptor 2 (HER2)-Positive advanced breast Cancer treated with first-line taxane-Trastuzumab-Pertuzumab. Cancers (Basel), 2021,13(8).
Gambichler T, Said S, Abu RN, et al. Pan-immune-inflammation value independently predicts disease recurrence in patients with Merkel cell carcinoma. J Cancer Res Clin Oncol. 2022;148(11):3183–9.
Corti F, Lonardi S, Intini R, et al. The Pan-immune-inflammation Value in microsatellite instability-high metastatic colorectal cancer patients treated with immune checkpoint inhibitors. Eur J Cancer. 2021;150:155–67.
Sahin AB, Cubukcu E, Ocak B, et al. Low pan-immune-inflammation-value predicts better chemotherapy response and survival in breast cancer patients treated with neoadjuvant chemotherapy. Sci Rep. 2021;11(1):14662.
Gong J, Jiang H, Shu C, et al. Prognostic value of lymphocyte-to-monocyte ratio in ovarian cancer: a meta-analysis. J Ovarian Res. 2019;12(1):51.
Aviki EM, Lavery JA, Roche KL, et al. Impact of provider volume on front-line chemotherapy guideline compliance and overall survival in elderly patients with advanced ovarian cancer. Gynecol Oncol. 2020;159(2):418–25.
Scaletta G, Plotti F, Luvero D, et al. The role of novel biomarker HE4 in the diagnosis, prognosis and follow-up of ovarian cancer: a systematic review. Expert Rev Anticancer Ther. 2017;17(9):827–39.
Sun ML, Yang ZY, Wu QJ, et al. The role of human epididymis protein 4 in the diagnosis and prognosis of diseases: an Umbrella Review of systematic reviews and Meta-analyses of Observational Studies. Front Med (Lausanne). 2022;9:842002.
Ceran MU, Tasdemir U, Colak E, et al. Can complete blood count inflammatory parameters in epithelial ovarian cancer contribute to prognosis? - a survival analysis. J Ovarian Res. 2019;12(1):16.
Acknowledgements
We thank the enrolled individuals, including ovarian patients, the medical staffs, and laboratory technicians in our study.
Funding
This study was funded by National Natural Science Foundation of China (contract/grant number: 82172993).
Author information
Authors and Affiliations
Contributions
WJ.L and WY.F conceived the project and wrote the manuscript. J.L, YJ.S, ZJ.C, WN.K managed data acquisition. WJ.L participated in the data analysis. WJ.L and H.Y participated in the discussion and language editing. H.Y and J.L reviewed the manuscript. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the Ethics Committee of the Xijing Hospital (Research No. KY20232001-F-1). Due to the retrospective nature of the study, the ethics committee waived the requirement of written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liao, W., Li, J., Feng, W. et al. Pan-immune-inflammation value: a new prognostic index in epithelial ovarian cancer. BMC Cancer 24, 1052 (2024). https://doi.org/10.1186/s12885-024-12809-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12809-2