Abstract
Background
This study aimed to establish a consensus on the delineation of target volumes for neoadjuvant radiation therapy (nRT) in esophageal squamous cell carcinoma (ESCC) within China.
Methods
From February 2020 to June 2021, nine ESCC patients who received nRT were retrospectively selected from Sun Yat-sen University Cancer Center and Shandong Cancer Hospital. A panel from eight cancer radiotherapy centers performed two rounds of nRT target volume delineation for these patients: the first round for cases 1–6 and the second for cases 7–9. Online meetings were held after each delineation round to discuss findings. The consistency of delineations across centers was compared using mean undirected Hausdorff distances (Hmean), dice similarity coefficients (DSC), and total volumes, analyzed with the Mann-Whitney U test.
Results
The second round of delineations showed improved consistency across centers (total clinical target volume (CTVtotal): mean DSC = 0.76–0.81; mean Hmean = 2.11–3.14 cm) compared to the first round (CTVtotal: mean DSC = 0.63–0.64; mean Hmean = 5.66–7.34 cm; DSC and Hmean: P < 0.050 between rounds), leading to the formation of a consensus and an atlas for ESCC nRT target volume delineation. A proposal was reached through evaluating target volume delineations, analyzing questionnaire survey outcomes, and reviewing pertinent literature.
Conclusions
We have developed guidelines and an atlas for target volume delineation in nRT therapy for ESCC in China. These resources are designed to facilitate more consistent delineation of target volumes in both clinical practice and clinical trials.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In the 2020 worldwide cancer statistics, esophageal cancer (EC) is identified as the seventh most prevalent cancer, registering 604,000 new cases, and emerges as the sixth leading cause of cancer mortality globally, with China accounting for nearly half of these cases and fatalities [1, 2]. EC displays notable geographical variations, with esophageal squamous cell carcinoma (ESCC) being the predominant histological subtype in China, comprising 85.79% of the cases [3]. Over 50% of EC patients are diagnosed at advanced stages, leading to a mere 25–36% five-year survival rate when treated with surgery alone [4].
The Dutch CROSS study and the Chinese NEOCRTEC5010 study have established the foundation for neoadjuvant chemoradiotherapy (nCRT) as the standard treatment for operable locally advanced ESCC [5, 6]. As nCRT is deployed, it introduces a series of challenges, particularly the debated topic of defining the radiation target area within nCRT. Radiation oncologists from five European centers firstly put forward a proposal for defining the radiation target volume in the neoadjuvant radiotherapy (nRT) for EC [7]. However, regional disparities in the pathology of EC are evident, with esophageal adenocarcinoma (EAC) is more prevalent in Western countries, including Europe and North America, while ESCC predominantly affecting Eastern Asia, Eastern and Southern Africa [8, 9]. It raises the question of whether this European consensus applies to the ESCC characteristic of China. Firstly, the lymphatic drainage patterns of ESCC and EAC are distinct and critically influence the delineation of radiation fields in the nRT; despite this, there is a paucity of research on the lymph node metastasis distribution specific to EAC, and the data concerning both tumor types are markedly heterogeneous; this variability presents challenges in formulating evidence-based protocols for both neoadjuvant treatments, specifically in radiation field optimization [10]. Secondly, ESCC and EAC exhibit differences in tumor location, predisposing factors, metastasis, and prognosis [11]. Thirdly, with the onset of the immunotherapy era, there has been a surge in clinical trials exploring the combination of radiotherapy and immunotherapy [12,13,14,15,16]; this integration of radioimmunotherapy introduces novel challenges in target volume delineation; moreover, to enable a fair comparison of treatment outcomes across various radiotherapy techniques and different centers, there is a pressing need for standardized guidelines on the delineation of radiation target volumes.
Through a comparative and analytical review of target volume delineation across eight cancer radiotherapy centers over two rounds, our goal was to achieve a consensus proposal and develop an atlas for the definition of target volumes in nRT for ESCC within China.
Materials and methods
Participating centers and cases selection
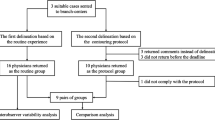
The study was conducted by eight premier cancer radiotherapy institutions across China, including Shandong Cancer Hospital, Anyang Cancer Hospital, the Fourth Hospital of Hebei Medical University, Sichuan Cancer Hospital, Shanghai Chest Hospital, Tianjin Cancer Hospital, Jiangsu Cancer Hospital, and Sun Yat-sen University Cancer Center. This team, comprising eight radiation oncologists and eight radiologists, selected nine ESCC cases that had received nRT from Shandong Cancer Hospital (cases 1–3, 7–9) and Sun Yat-sen University Cancer Center (cases 4–6). The delineation of nRT target volumes was carried out in two rounds, focusing on cases 1–6 in the first round and cases 7–9 in the second round. These cases were strategically chosen to cover a wide range of primary tumor locations and metastatic lymph node involvements within the thoracic esophagus—upper (cases 1, 4, 7), middle (cases 2, 5, 8), and lower (cases 3, 6, 9) segments. Patient demographics and tumor characteristics are detailed in Table 1, with computed tomography (CT) or positron emission tomography/CT (PET/CT) images provided when available, to depict the primary tumor and involved lymph nodes. Additionally, in this study, 18 radiation therapy centers in China participated in a survey questionnaire on the delineation of nRT target volumes.
Consensus process
-
Step 1: The first delineation round involved outlining target volumes for six cases, adhering to institutional guidelines.
-
Step 2: A questionnaire was conducted to gather information on nRT practices across 18 radiotherapy centers.
-
Step 3: A consensus meeting was held to review and discuss the findings from the initial questionnaire and the first delineation round, leading to the proposal of a preliminary target volume guideline.
-
Step 4: The proposed consensus, along with detailed delineation instructions and an atlas, was then distributed for feedback.
-
Step 5: In the second delineation phase, target volumes for three additional ESCC cases were outlined, incorporating feedback from the previous step.
-
Step 6: The final step culminated in the establishment of a consensus on the delineation guidelines, which was comprehensively documented in an atlas.
Statistical analysis
The delineated target volumes were centrally gathered in digital imaging and communications in medicine format and uploaded into Eclipse software (Version 15.3) for each case. The volumes, including the gross tumor volume of the primary tumor (GTVp), gross tumor volume of the lymph nodes (GTVn), and the total clinical target volume (CTVtotal), were compared and consolidated into a unified scan per case. Subsequently, these unified volumes were transferred to 3D Slicer software (Version 4.11.20200930) for quantitative analysis [17]. This analysis included measuring the mean undirected Hausdorff distances (Hmean), the dice similarity coefficient (DSC), and the total volume difference between the first and second delineation rounds. The Hmax/Hmean and DSC metrics quantitatively assessed the consistency across the contouring centers in defining the target volumes [18, 19]. The collected data underwent statistical analysis utilizing the Mann-Whitney U test for continuous variables, employing SPSS software (version 26.0). We evaluated differences in the DSC and Hmean across the eight centers that participated in both delineation rounds. Discrepancies were deemed statistically significant if the P-value was less than 0.05.
Results
First delineation round of cases 1–6
During our analysis, we found variability in delineation practices among eight centers. The DSC indicated moderate consistency, with values ranging from 0.67 to 0.90 for the GTVp and 0.44 to 0.78 for the CTVtotal. The Hmean further reflected this inconsistency, with ranges from 0.77 to 6.22 cm for GTVp and 2.84 to 13.12 cm for CTVtotal. The primary issues contributing to the variations were centered around three main areas: the first issue was the differing assessments of positive lymph nodes; the second issue concerned the cranio-caudal expansion from the GTVp to the clinical target volume of the primary tumor (CTVp), with some centers adopting a 2 cm expansion, while others opted for 3 cm; another significant area of dispute involved selective irradiation of specific lymphatic drainage areas, such as the supraclavicular region, with variations between centers in expanding the GTVn by 0.5–0.6 cm to form the clinical target volume of the lymph nodes (CTVn) versus including the entire lymph node drainage area.
Questionnaires
We collected feedback through questionnaires from 18 cancer radiotherapy centers across China, as summarized in Table 2. A majority of the centers, 83.33% (15 out of 18), opted for an involvement-based approach for radiation field selection. In terms of defining the CTVp from GTVp, 14 (77.78%) centers chose a radial expansion of 0.5 cm; uniformly, all centers concurred on a cranio-caudal expansion of 2–3 cm, with half (9 centers) specifically favoring a 3 cm expansion. For the expansion from the GTVn to the CTVn, 61.11% (11 out of 18) of centers applied a uniform expansion of 0.5 cm in all directions. Similarly, 61.11% (11 out of 18) of the centers expanded the CTV to form the planning target volume (PTV) by 0.5 cm. Additionally, 77.78% (14 out of 18), were amenable to including the surgical anastomosis within the radiation therapy field.
Meeting for preliminary consensus
In addition to radiologists and radiation oncologists who participated in the panel, a physicist and a thoracic surgeon specializing in esophageal therapy in each center also attended the meeting and gave constructive comments. A preliminary consensus on nRT target delineation has reached through discussion and analysis of the first round of target delineation.
All centers that participated in the working panel agreed to apply margins of an expansion of 0.5–0.6 cm radially and 2.0–3.0 cm cranio-caudally along the esophageal wall, including the paraoesophageal lymph nodes drainage area, from the GTVp to the CTVp. The importance of accurately distinguishing between benign and malignant lymph nodes was emphasized, highlighting the necessity for close collaboration with radiologists and the comprehensive use of multimodal imaging techniques, such as PET-CT and magnetic resonance imaging (MRI), to aid diagnosis [20].
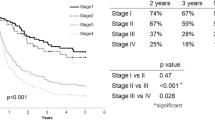
Second delineation round of cases 7–9
Due to inconsistencies in lymph node assessments between centers in the first round, we conducted preliminary discussions before the second round of delineation to pinpoint the locations of metastatic lymph nodes. We matched cases from the second delineation round with those from the first to assess consistency across rounds. The DSC, Hmean, and volumes for the GTVp and the CTVtotal in the second round from the eight centers participating in both rounds are detailed in Tables 3 and 4. In the second round of GTVp delineation, the DSC values were higher, and the Hmean values were lower, indicating greater overlap and higher consistency between the delineations. Similarly, the second round demonstrated enhanced consistency across centers for the CTVtotal, with mean DSC values between 0.76 and 0.81 and Hmean between 2.11 and 3.14 cm, an improvement from the first round (mean DSC: 0.63–0.64; Hmean: 5.66–7.34 cm; DSC and Hmean: P < 0.05). This increased uniformity was consistent for target volumes of upper, middle, and lower thoracic ESCC, across rounds (DSC and Hmean: P < 0.05). Additionally, the overall target volumes in the second delineation were smaller than those in the first for upper (P = 0.001), middle (P = 0.000), and lower (P = 0.002) thoracic ESCC.
Meeting for final consensus and atlas
The meeting after the second round of delineation focused on the delineation of CTVp and CTVn. A consensus was obtained for the delineation of the GTVp, GTVn, CTVp, CTVn, and CTVtotal in patients with ESCC undergoing nRT. This consensus was achieved through the analysis of target volume delineations, results from questionnaire surveys, and a review of relevant literature. After the meeting the atlas (Figs. 1, 2 and 3) for target volume delineation was generated.
Consensus atlas for cT3N0M0 upper thoracic esophagus cancer. Gross tumor volume (GTV) of the primary tumor is depicted in red, representing the actual tumor size. The clinical target volume (CTV) of the primary tumor, illustrated in blue, is achieved by expanding the GTV 2.0 cm in the cranio-caudal direction and 0.5 cm radially along the esophageal wall. The planning target volume (PTV), shown in green, is created by a uniform expansion of 0.5 cm around the entirety of the CTV
Consensus atlas for cT3N1M0 middle thoracic esophagus cancer. Gross tumor volume of the primary tumor or pathological lymph nodes (GTVp/n) is illustrated: GTVp is shown in red, representing the primary tumor mass, while GTVn, indicating pathological lymph nodes, is depicted in yellow. The clinical target volume for the primary tumor or lymph nodes (CTVp/n) involves strategic expansions from GTVp/n: CTVp is derived from GTVp with a 2.0 cm expansion cranio-caudally and a 0.5 cm expansion radially along the esophageal wall. CTVn is formulated by expanding GTVn by 0.5 cm in areas with paraoesophageal lymph node drainage. Additionally, for lymph nodes affected in the celiac area, CTVn incorporates a 1.0 cm margin cranio-caudally. The planning target volume (PTV), shown in green, is a uniform 0.5 cm expansion surrounding the total clinical target volume (CTVtotal), which is presented in blue and constitutes the combined volumes of CTVp and CTVn
Consensus atlas for cT3N1M0 lower thoracic esophagus cancer. GTVp/n represents the gross tumor volume of the primary tumor or pathological lymph nodes, with GTVp (shown in red) encompassing the primary tumor and expanded by 2.0 cm cranio-caudally and 0.5 cm radially along the esophageal wall to form the clinical target volume for the primary tumor (CTVp). GTVn (depicted in yellow) identifies pathological lymph nodes, expanded by 0.5 cm in paraoesophageal lymph node drainage areas to create CTVn. For the 106recR and celiac lymph nodes, CTVn includes a 1.0 cm cranio-caudal margin around the lymph node drainage area. The total clinical target volume (CTVtotal), illustrated in blue, aggregates CTVp and CTVn. Surrounding CTVtotal, the planning target volume (PTV) is visualized in green, marked by a uniform 0.5 cm expansion to ensure comprehensive coverage for radiation treatment planning
The CROSS trial highlighted that in 213 EC patients undergoing involved field irradiation (IFI), 11 instances (5.2%) encountered in-field recurrences, with merely 2 cases presenting isolated in-field recurrence without distant metastasis [21]. Concurrently, a retrospective analysis of 118 patients revealed no significant survival or local control benefits at the primary site for the 73 patients subjected to elective nodal irradiation (ENI) targeting either supraclavicular (n = 54) or abdominal (n = 19) lymph nodes [22]. Moreover, a comprehensive meta-analysis spanning 29 studies and encompassing 5,212 patients indicated no notable differences between IFI and ENI regarding loco-regional recurrence-free survival, overall survival (OS), R0 resection rates [23]. Additional research found comparable disease-free survival and OS rates between IFI and ENI groups, though ENI was associated with a heightened risk of radiation-induced adverse events [24]. In a retrospective study comparing clinicopathologic outcomes and lymphatic spread patterns among neoadjuvant chemotherapy, nCRT, and neoadjuvant immunochemotherapy in locally advanced ESCC, the nCRT group using the IFI model achieved a promising pCR rate and demonstrated superior therapeutic response in the primary lesion [25]. Hence, efforts to improve loco-regional control, such as expanding the irradiation field, may have a limited effect on enhancing OS rates in nCRT for EC. We acknowledge the follow-up results of a randomized phase 3 trial indicating that concurrent chemoradiotherapy with ENI improves long-term survival in locally advanced ESCC in the setting of definitive chemoradiotherapy [26]. However, we believe there are fundamental differences between definitive chemoradiotherapy and nCRT. NCRT is followed by surgery, which helps to clear high-risk lymph nodes in the cervical, thoracic, and abdominal regions, including the esophagus 5 cm above and below the primary lesion. Table 5 shows the comparison between the CROSS and NEOCRTEC5010 studies.While the CROSS [5] study included prophylactic irradiation for some high-risk lymph node regions, it did not show improved local control rates or survival compared to the NEOCRTEC5010 study [6], which did not use ENI. A meta-analysis by Kumagai et al. [27] showed that nCRT increases the incidence of postoperative adverse events in patients with ESCC with postoperative complications primarily involving cardiac and pulmonary-related adverse reactions. Prospective studies by the Radiation Therapy Oncology Group (RTOG) [28] have shown a significant association between V20 and the severity of radiation pneumonitis, and research by Wei et al. [29]. identified pericardial V30 as a major risk factor for pericardial effusion. IFI can reduce target volume, providing more reliable protection for the heart and lungs. Given the lower in-field recurrence rate and enhanced safety with neoadjuvant IFI, we suggest the use of IFI in neoadjuvant radiotherapy for ESCC.
-
GTVp includes the primary tumor, and should be determined by combining the results of multimodal image fusion (gastroenterography, enhanced CT, MRI, PET/CT, upper gastrointestinal endoscopy and endoscopic ultrasonography (EUS). GTVp includes the entire esophagus wall but not the fat surrounding the esophagus. If markers such as titanium clips are placed at tumor margins, they should be included in the GTVp [30].
-
GTVn includes metastatic lymph nodes. Similarly, multimodal image fusion (enhanced CT, MRI, PET/CT and EUS) are required. Lymph nodes with the following imaging characteristics should be considered suspicious for malignancy: short-axis diameter ≥ 10 mm on CT/MRI (≥ 5 mm for paratracheal and paraesophageal lymph nodes), eccentric calcification, ring enhancement similar to that of the primary tumor, and high standardized uptake values (SUV) on PET-CT (excluding inflammatory lymph nodes).We emphasize the importance of collaboration with radiologists. However, when in doubt that the lymph nodes can affect the patient’s treatment, it is recommended to use fine-needle aspiration cytology [31,32,33,34]. Considering that the position of abdominal lymph nodes is significantly influenced by the state of gastric filling, measures such as stabilizing the degree of gastric filling and enhancing image-guided interventions should be implemented during radiotherapy to ensure quality control.
-
CTVp expands from GTVp by 0.5 cm radially and 2.0–3.0 cm cranio-caudally, covering the esophageal wall and paraesophageal lymph nodes [35]. The feasibility for smaller expansions requires further research. Adjustments to CTVp should be made for surrounding anatomy like muscles, bones, and vessels, excluding areas without invasion.
-
CTVn includes the GTVn with an expansion of 0.5–1 cm in all directions [36]. CTVn should be corrected for anatomy (muscles, bones, large vessels, and organs at risk) if there is no invasion.
-
CTVtotal includes CTVp and CTVn. When skip metastasis is present (the distance between CTVn and CTVp exceeds 3 cm), it is permissible to delineate CTVn separately without connecting it to CTVp.
-
Internal target volume (ITV) is determined based on tumor motion assessed by 4D CT.
-
PTV is expanded by 5 mm in all directions from the ITV (CTV), with a longitudinal extension up to 8 mm (actual expansion can be decided based on quality control data from each center).
-
The consensus recommends a nRT dose of 40.0–50.4 Gy over 20–28 fractions, and for trials combining with immunotherapy, the advised dose is 40.0–41.4 Gy across 20–23 fractions [14, 15].
Discussion
Precise delineation of the tumor volume is crucial for the effective execution of nRT for ESCC patients. Despite this, there’s a lack of a universally accepted standard for defining irradiation volumes, leading to significant variability in tumor delineation. A prospective study investigating the precision of volume delineation in EC for nCRT found that in 35% of cases, the macroscopic tumor extended beyond the GTV, and in 14% of cases, beyond the CTV, among patients with macroscopic residual tumors [37]. The discrepancy between the delineated tumor volumes and the actual tumor location is associated with a marked decrease in OS, highlighting the urgent need for enhanced precision in mapping tumor volumes to improve therapeutic outcomes.
In the European target delineation guidelines [7], CTVn is defined by a 1.0 cm expansion around GTVn and a 3.0 cm superior-inferior extension from GTVp, covering lymphatic drainage zones such as the azygos vein, main pulmonary artery window, gastric coronary vein, subcarinal, paratracheal/pretracheal, pericardial, and supraclavicular regions. The consensus among most experts is that the European target delineation guidelines might be overly extensive, potentially elevating the risk of complications and diminishing the population of normal lymphatic cells, which could negatively impact the prognosis [38,39,40]. A study [41] on lung cancer also revealed that the effective radiation dose to immune cells is a critical independent risk factor for diminished OS and local progression-free survival in patients enrolled in the RTOG 0617 trial, underscoring radiation-induced immune suppression as a key determinant in tumor control efficacy.
In the era of immunotherapy, the merging of nRT and/or chemotherapy with immunotherapy for EC has emerged as a significant research focus, with increasing attention on the associated toxicities of such combinations. The PALACE-1 study [15], involving patients with ESCC undergoing surgery after preoperative pembrolizumab and concurrent chemoradiotherapy, affirmed the feasibility of this regimen for resectable ESCC. Notably, postoperative pulmonary complications such as pneumonia and atelectasis were reported in 22% of cases each. Meanwhile, in the PERFECT study [14], which examined 40 patients with resectable EC treated with nCRT combined with atezolizumab, 83% (33 patients) proceeded to surgery, experiencing predominantly pulmonary (30%, 10/33) and cardiac (21%, 7/33) perioperative complications. Additionally, a retrospective study [42] analyzed the impact of concurrent chemoradiotherapy combined with pembrolizumab on subsequent surgery, finding that although the pembrolizumab group did not experience an increase in surgical risks, the incidence of acute respiratory distress syndrome was higher than in the concurrent chemoradiotherapy alone group. This highlights the necessity of carefully balancing therapeutic efficacy against potential side effects in the context of combined treatments. Given the compounded toxicity observed with combined immunotherapy, particularly radiation or immune-related pulmonary toxicity, optimizing the target area of nRT is crucial. We recommend IFI and, for clinical trials combining radiotherapy with immunotherapy, suggest a dose of 40.0–41.4 Gy delivered over 20–23 fractions.
Through collaborative discussions and case-by-case analyses of the target volumes delineated by each center, we have achieved a consensus and subsequently developed an atlas for the delineation of target volumes for nRT in ESCC in China. Nevertheless, it’s important to recognize the limitations of these guidelines. A notable limitation is the lack of clinical validation or direct correlation with patient outcomes for our consensus, underlining the necessity for its effectiveness and safety to be assessed through future clinical trials. Furthermore, we acknowledge that these recommendations and the atlas may not be universally applicable to all individual patients. Consistent with contemporary radiation treatment planning techniques, the process of contouring and treatment planning should be personalized, with each plan meticulously tailored to the specific clinical circumstances of the patient.
Conclusions
This is the first report to define a consensus on the delineation of target volumes of nRT in ESCC in China. The establishment of this consensus significantly enhances the implementation of nRT for ESCC, ensuring precise target volume delineation. Moreover, it lays a solid groundwork for the design and execution of future clinical trials focusing on nRT in ESCC.
Availability of data and materials
The data underlying this article are available in the article and in its online supplementary material.
Abbreviations
- EC:
-
Esophageal cancer
- ESCC:
-
Esophageal squamous cell carcinoma
- nCRT:
-
Neoadjuvant radiotherapy
- EAC:
-
Esophageal adenocarcinoma
- CT:
-
Computed tomography
- PET/CT:
-
Positron emission tomography/computed tomography
- GTVp:
-
Gross tumor volume of the primary tumor
- GTVn:
-
Gross tumor volume of the lymph nodes
- CTVtotal:
-
Clinical target volume of the total volume
- Hmean:
-
mean undirected Hausdorff distances
- DSC:
-
Dice similarity coefficient
- CTVp:
-
Clinical target volume of the primary tumor
- CTVn:
-
Clinical target volume of the lymph nodes
- PTV:
-
Planning target volume
- MRI:
-
Magnetic resonance imaging
- IFI:
-
Involved field irradiation
- ENI:
-
Elective nodal irradiation
- OS:
-
Overall survival
- EUS:
-
Endoscopic ultrasonography
- ITV:
-
Internal target volume
References
Arnold M, Abnet CC, Neale RE, Vignat J, Giovannucci EL, McGlynn KA, Bray F. Global burden of 5 major types of gastrointestinal Cancer. Gastroenterology. 2020;159(1):335–e349315.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and Mortality Worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Chen R, Zheng R, Zhang S, Wang S, Sun K, Zeng H, Li L, Wei W, He J. Patterns and trends in esophageal cancer incidence and mortality in China: an analysis based on cancer registry data. J Natl Cancer Cent. 2023;3(1):21–7.
Shao-Bin Chen H-RW. Hao Zhang: prognostic factors and outcome for patients with esophageal squamous cell carcinoma underwent surgical resection alone: evaluation of the seventh edition of the American Joint Committee on Cancer staging system for esophageal squamous cell carcinoma. J Thorac Oncol. 2013;8(4):495–501.
van Hagen P, van Lanschot MCCMHJJB, Steyerberg EW, van Berge Henegouwen MI, Wijnhoven BPL, Richel,G DJ, A P Nieuwenhuijzen,G A P Hospers JJ, Bonenkamp MA, Cuesta RJB, Blaisse. O R C Busch,F J W ten Kate,G-J creemers: preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med. 2012;366(22):2074–84.
Yang H, Liu H, Chen Y, Zhu C, Fang W, Yu Z, Mao W, Xiang J, Han Y, Chen Z, et al. Neoadjuvant Chemoradiotherapy followed by surgery versus surgery alone for locally advanced squamous cell carcinoma of the Esophagus (NEOCRTEC5010): a phase III Multicenter, Randomized, open-label clinical trial. J Clin Oncol. 2018;36(27):2796–803.
Thomas M, Mortensen HR, Hoffmann L, Moller DS, Troost EGC, Muijs CT, Berbee M, Butof R, Nicholas O, Radhakrishna G, et al. Proposal for the delineation of neoadjuvant target volumes in oesophageal cancer. Radiother Oncol. 2021;156:102–12.
Arnold M, Ferlay J, van Berge Henegouwen MI, Soerjomataram I. Global burden of oesophageal and gastric cancer by histology and subsite in 2018. Gut. 2020;69(9):1564–71.
Morgan E, Soerjomataram I, Rumgay H, Coleman HG, Thrift AP, Vignat J, Laversanne M, Ferlay J, Arnold M. The Global Landscape of esophageal squamous cell carcinoma and esophageal adenocarcinoma incidence and mortality in 2020 and projections to 2040: new estimates from GLOBOCAN 2020. Gastroenterology. 2022;163(3):649–e658642.
Hagens ERC, van Berge Henegouwen MI, Gisbertz SS. Distribution of Lymph Node Metastases in Esophageal Carcinoma patients undergoing upfront surgery: a systematic review. Cancers (Basel). 2020;12(6):1592.
Cancer Genome Atlas Research N, Analysis Working Group, Asan U, Agency BCC, Brigham, Women’s H, Broad I, Brown U, Case Western Reserve U, Dana-Farber Cancer I, Duke U et al. Integrated genomic characterization of oesophageal carcinoma. Nature 2017, 541(7636):169–175.
Chen R, Liu Q, Li Q, Zhu Y, Zhao L, Liu S, Chen B, Liu M, Hu Y, Lin T, et al. A phase II clinical trial of toripalimab combined with neoadjuvant chemoradiotherapy in locally advanced esophageal squamous cell carcinoma (NEOCRTEC1901). EClinicalMedicine. 2023;62:102118.
Zheng Y, Li C, Yu B, Zhao S, Li J, Chen X, Li H. Preoperative pembrolizumab combined with chemoradiotherapy for esophageal squamous cell carcinoma: trial design. JTCVS Open. 2022;9:293–9.
van den Ende T, de Clercq NC, van Berge Henegouwen MI, Gisbertz SS, Geijsen ED, Verhoeven RHA, Meijer SL, Schokker S, Dings MPG, Bergman J, et al. Neoadjuvant Chemoradiotherapy Combined with Atezolizumab for Resectable Esophageal Adenocarcinoma: a single-arm phase II feasibility trial (PERFECT). Clin Cancer Res. 2021;27(12):3351–9.
Li C, Zhao S, Zheng Y, Han Y, Chen X, Cheng Z, Wu Y, Feng X, Qi W, Chen K, et al. Preoperative pembrolizumab combined with chemoradiotherapy for oesophageal squamous cell carcinoma (PALACE-1). Eur J Cancer. 2021;144:232–41.
Li M, Sun H, Yang W, Luo J, Lin H, Zhou T, Gong H, Zhao D, Niu Z, Wang Z, et al. A phase 1b clinical trial of Neoadjuvant Radio-immunotherapy for esophageal squamous cell Cancer. Int J Radiat Oncol Biol Phys. 2024;119(3):896–901.
Fedorov A, Beichel R, Kalpathy-Cramer J, Finet J, Fillion-Robin JC, Pujol S, Bauer C, Jennings D, Fennessy F, Sonka M, et al. 3D slicer as an image computing platform for the quantitative Imaging Network. Magn Reson Imaging. 2012;30(9):1323–41.
Rucklidge W. Efficient visual recognition using the Hausdorff distance. Lecture Notes in Computer Science (Springer Berlin Heidelberg). 1996;1173:1-120.
Dice LR. Measures of the amount of ecologic association between species. Ecology. 1945;26(3):297–302.
Garcia B, Goodman KA, Cambridge L, Dunphy M, Wu AJ. Distribution of FDG-avid nodes in esophageal cancer: implications for radiotherapy target delineation. Radiation Oncol (London England). 2016;11(1):156.
Oppedijk V, van der Gaast A, van Lanschot JJ, van Hagen P, van Os R, van Rij CM, van der Sangen MJ, Beukema JC, Rutten H, Spruit PH, et al. Patterns of recurrence after surgery alone versus preoperative chemoradiotherapy and surgery in the CROSS trials. J Clin Oncol. 2014;32(5):385–91.
Hsu FM, Lee JM, Huang PM, Lin CC, Hsu CH, Tsai YC, Lee YC, Chia-Hsien Cheng J. Retrospective analysis of outcome differences in preoperative concurrent chemoradiation with or without elective nodal irradiation for esophageal squamous cell carcinoma. Int J Radiat Oncol Biol Phys. 2011;81(4):e593–599.
Liu T, Ding S, Dang J, Wang H, Chen J, Li G. Elective nodal irradiation versus involved-field irradiation in patients with esophageal cancer receiving neoadjuvant chemoradiotherapy: a network meta-analysis. Radiat Oncol. 2019;14(1):176.
Chen X, Zhang Y, Zhou X, Wang M, Na F, Zhou L, Xu Y, Zou B, Xue J, Liu Y, et al. Involved-field irradiation or elective-nodal irradiation in neoadjuvant chemo-radiotherapy for locally-advanced esophageal cancer: comprehensive analysis for dosimetry, treatment-related complications, impact on lymphocyte, patterns of failure and survival. Front Oncol. 2023;13:1274924.
Tian Y, Shi Z, Wang C, Ke S, Qiu H, Zhao W, Wu Y, Chen J, Zhang Y, Chen Y. A comparison of clinicopathologic outcomes and patterns of Lymphatic Spread Across Neoadjuvant Chemotherapy, Neoadjuvant Chemoradiotherapy, and Neoadjuvant Immunochemotherapy in locally advanced esophageal squamous cell carcinoma. Ann Surg Oncol. 2024;31(2):860–71.
Xie C, Jing Z, Luo H, Jiang W, Ma L, Hu W, Zheng A, Li D, Ding L, Zhang H, et al. Chemoradiotherapy with extended nodal irradiation and/or erlotinib in locally advanced oesophageal squamous cell cancer: long-term update of a randomised phase 3 trial. Br J Cancer. 2020;123(11):1616–24.
Kumagai K, Rouvelas I, Tsai JA, Mariosa D, Klevebro F, Lindblad M, Ye W, Lundell L, Nilsson M. Meta-analysis of postoperative morbidity and perioperative mortality in patients receiving neoadjuvant chemotherapy or chemoradiotherapy for resectable oesophageal and gastro-oesophageal junctional cancers. Br J Surg. 2014;101(4):321–38.
Graham MVPJ, Emami B, Harms W, Bosch W, Lockett MA, Perez CA. Clinical dose-volume histogram analysis for pneumonitis after 3D treatment for non-small cell lung cancer (NSCLC). Int J Radiat Oncol Biol Phys. 1999;45(2):323–9.
Wei X, Liu HH, Tucker SL, Wang S, Mohan R, Cox JD, Komaki R, Liao Z. Risk factors for pericardial effusion in inoperable esophageal cancer patients treated with definitive chemoradiation therapy. Int J Radiat Oncol Biol Phys. 2008;70(3):707–14.
Guan Y, Wang J, Cao F, Chen X, Wang Y, Jiang S, Zhang D, Zhang W, Guo Z, Wang P, et al. Role of clip markers placed by endoscopic ultrasonography in contouring gross tumor volume for thoracic esophageal squamous cell carcinoma: one prospective study. Ann Transl Med. 2020;8(18):1144.
Min L, Qing Y, Chu Y, Liang C, Lv L, Liu D, Tan Y, Zhou Y. Role of endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) in the diagnosis of suspicious malignant esophageal strictures. J Clin Med. 2023;12(6):2153.
van der Bogt RD, van der Wilk BJ, Poley JW, Krishnadath KK, Schoon EJ, Oostenbrug LE, Siersema PD, Vleggaar FP, Bruno MJ, Biermann K, et al. Endoscopic ultrasound and fine-needle aspiration for the detection of residual nodal disease after neoadjuvant chemoradiotherapy for esophageal cancer. Endoscopy. 2020;52(3):186–92.
Chris Harrington LS, Jennifer Bisland. Elisabet López González,Neil Jamieson,Stuart Paterson,Adrian John Stanley: Mediastinal node staging by positron emission tomography-computed tomography and selective endoscopic ultrasound with fine needle aspiration for patients with upper gastrointestinal cancer: results from a regional centre. World J Gastrointest Endosc. 2018;10(1):37–44.
Hong G, Oki M. Transesophageal endoscopic ultrasound with bronchoscope-guided fine-needle aspiration for diagnostic and staging purposes: a narrative review. J Thorac Dis. 2023;15(9):5088–98.
Gao XS, Qiao X, Wu F, Cao L, Meng X, Dong Z, Wang X, Gao G, Wu TT, Komaki R, et al. Pathological analysis of clinical target volume margin for radiotherapy in patients with esophageal and gastroesophageal junction carcinoma. Int J Radiat Oncol Biol Phys. 2007;67(2):389–96.
Wang ZW, Zhang W, Dong W, Li BS, Mu DB, Huang W, Zhang J, Li HS, Zhang ZC, Lin HQ, et al. Pathological analysis of extracapsular extension of metastatic lymph node and its potential impact on nodal clinical target volume in the radiotherapy of esophageal squamous cell carcinoma. Neoplasma. 2014;61(3):324–30.
Muijs C, Smit J, Karrenbeld A, Beukema J, Mul V, van Dam G, Hospers G, Kluin P, Langendijk J, Plukker J. Residual tumor after neoadjuvant chemoradiation outside the radiation therapy target volume: a new prognostic factor for survival in esophageal cancer. Int J Radiation Oncol*Biol*Phys. 2014;88(4):845–52.
Boivin G, Kalambaden P, Faget J, Rusakiewicz S, Montay-Gruel P, Meylan E, Bourhis J, Lesec G, Vozenin MC. Cellular Composition and Contribution of Tertiary lymphoid structures to Tumor immune infiltration and modulation by radiation therapy. Front Oncol. 2018;8:256.
Shiraishi Y, Fang P, Xu C, Song J, Krishnan S, Koay EJ, Mehran RJ, Hofstetter WL, Blum-Murphy M, Ajani JA, et al. Severe lymphopenia during neoadjuvant chemoradiation for esophageal cancer: a propensity matched analysis of the relative risk of proton versus photon-based radiation therapy. Radiother Oncol. 2018;128(1):154–60.
So TH, Chan SK, Chan WL, Choi H, Chiang CL, Lee V, Lam TC, Wong I, Law S, Kwong D, et al. Lymphopenia and radiation dose to circulating lymphocytes with neoadjuvant chemoradiation in esophageal squamous cell carcinoma. Adv Radiat Oncol. 2020;5(5):880–8.
Jin JY, Hu C, Xiao Y, Zhang H, Paulus R, Ellsworth SG, Schild SE, Bogart JA, Dobelbower MC, Kavadi VS, et al. Higher radiation dose to the immune cells correlates with worse tumor control and overall survival in patients with stage III NSCLC: a secondary analysis of RTOG0617. Cancers (Basel). 2021;13(24):6193.
Park SY, Hong MH, Kim HR, Lee CG, Cho JH, Cho BC, Kim DJ. The feasibility and safety of radical esophagectomy in patients receiving neoadjuvant chemoradiotherapy with pembrolizumab for esophageal squamous cell carcinoma. J Thorac Dis. 2020;12(11):6426–34.
Acknowledgements
Not applicable.
Funding
This work was supported by the National Natural Science Foundation of China (grant number: 81773232); the Academic Promotion Program of Shandong First Medical University (grant number: 2020RC002); the Project of Young Taishan Scholars (grant number: Tsqn201909187), and the Wu Jieping Medical Foundation (grant number: 320.6750.2021-01-11).
Author information
Authors and Affiliations
Contributions
Han Dan and Jinling Dong contributed equally to this work. JLD, DH, QFW, BSL and WH conceived, designed, and supervised the project. JLD, LJ, HL, BQ, WCZ, YH, WBS, YWZ and XZZ contributed to the design of the study, writing the protocol, and data preparation, analysis, and interpretation. JLD, DH, FHS, YW and LW drafted the manuscript. BSL, WH, JLD and DH performed the quality assessment and revised the manuscript. All authors have read and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The conduct of this study was retrospectively reviewed and granted ethical approval by the Institutional Review Board (IRB) of the Shandong First Medical University Affiliated Cancer Hospital Ethics Committee (approval number: SDTHEC2022001005). Given the retrospective nature of the research, the requirement for patient consent was formally waived by the aforementioned IRB. All research procedures were executed in strict accordance with the ethical principles set forth in the Declaration of Helsinki, ensuring the protection of human subjects in biomedical research. To maintain patient confidentiality, all patient records were anonymized and de-identified prior to the data analysis phase.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Han, D., Dong, J., Wang, Q. et al. Neoadjuvant radiation target volume definition in esophageal squamous cell cancer: a multicenter recommendations from Chinese experts. BMC Cancer 24, 1086 (2024). https://doi.org/10.1186/s12885-024-12825-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12825-2