Abstract
Background
The log odds of positive lymph nodes (LODDS) was considered a superior staging system to N stage in colon cancer, yet its value in determining the optimal duration of adjuvant chemotherapy for stage III colon cancer patients has not been evaluated. This study aims to assess the prognostic value of a model that combines LODDS with clinicopathological information for stage III colon cancer patients and aims to stratify these patients using the model, identifying individuals who could benefit from varying durations of adjuvant chemotherapy.
Method
A total of 663 consecutive patients diagnosed with stage III colon cancer, who underwent colon tumor resection between November 2007 and June 2020 at Sun Yat-sen University Cancer Center and Longyan First Affiliated Hospital of Fujian Medical University, were enrolled in this study. Survival outcomes were analyzed using Kaplan–Meier, Cox regression. Nomograms were developed to forecast patient DFS, with the Area Under the Curve (AUC) values of time-dependent Receiver Operating Characteristic (timeROC) and calibration plots utilized to assess the accuracy and reliability of the nomograms.
Results
Multivariate analysis revealed that perineural invasion (HR = 1.776, 95% CI: 1.052–3.003, P = 0.032), poor tumor differentiation (HR = 1.638, 95% CI: 1.084–2.475, P = 0.019), and LODDS groupings of 2 and 1 (HR = 1.920, 95% CI: 1.297–2.842, P = 0.001) were independent predictors of disease-free survival (DFS) in the training cohort. Nomograms constructed from LODDS, perineural invasion, and poor tumor differentiation demonstrated robust predictive performance for 3-year and 5-year DFS in both training (3-year AUC = 0.706, 5-year AUC = 0.678) and validation cohorts (3-year AUC = 0.744, 5-year AUC = 0.762). Stratification according to this model showed that patients in the high-risk group derived significant benefit from completing 8 cycles of chemotherapy (training cohort, 82.97% vs 67.17%, P = 0.013; validation cohort, 89.49% vs 63.97%, P = 0.030).
Conclusion
The prognostic model, integrating LODDS, pathological differentiation, and neural invasion, demonstrates strong predictive accuracy for stage III colon cancer prognosis. Moreover, stratification via this model offers valuable insights into optimal durations of postoperative adjuvant chemotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately 30% of colon cancer patients were identified with lymph node metastases at initial diagnosis, and the majority underwent direct curative surgical intervention [1, 2]. For patients whose lymph node metastases are confirmed by postoperative pathology, adjuvant chemotherapy can eliminate microscopic metastatic foci, thereby increasing the 5-year Disease-Free Survival (DFS) rate by 20% [3]. The consensus in both National Comprehensive Cancer Network (NCCN) and European Society for Medical Oncology (ESMO) guidelines for patients with colon cancer confirmed to have proficient mismatch repair (pMMR) is the administration of 3 to 6 months of capecitabine and oxaliplatin (CapOX) adjuvant chemotherapy [4, 5]. However, due to chemotherapy side effects, particularly oxaliplatin-induced neurotoxicity, approximately 20%-30% of patients are often unable to complete the full 6-month chemotherapy cycle [6, 7]. Additionally, 20%-40% of patients may not benefit from adjuvant chemotherapy, potentially leading to postoperative metastasis [8, 9]. Identifying stage III colon cancer patients who could benefit from adjuvant chemotherapy based on diverse clinicopathological features is crucial for developing personalized adjuvant chemotherapy regimens.
Despite the wide adoption of the TNM staging system for colon cancer, its efficacy in predicting DFS within the same stage is limited, as indicated by prior research [10, 11]. Significant survival disparities among stage III colon cancer patients and the lack of stratification based on clinicopathological characteristics pose substantial challenges for postoperative personalized treatment [12]. Introduced by Vincent et al. in 2004 for breast cancer staging, the concept of log odds of positive lymph nodes (LODDS) has shown superior predictive efficacy over traditional lymph node staging across various oncologic diseases [13,14,15]. Subsequent studies leveraging large cohort data have underscored the significant prognostic value of LODDS in colon cancer patients across stages II-IV [16,17,18,19]. However, to date, no study has assessed the guiding significance of LODDS on the duration of adjuvant chemotherapy in stage III colon cancer patients.
Leveraging data from the Sun Yat-sen University Cancer Center and the Longyan First Affiliated Hospital of Fujian Medical University, this study seeks to assess the prognostic value of a model that combines the log odds of positive lymph nodes (LODDS) with clinicopathological information for stage III colon cancer patients. Moreover, it aims to stratify these patients using the model to identify individuals who could benefit from different durations of adjuvant chemotherapy.
Method
Patient population
A retrospective analysis was conducted on all patients who underwent curative surgery for colon cancer at the Sun Yat-sen University Cancer Center from December 2007 to June 2020.The inclusion criteria were as follows: 1. Age between 18–80 years. 2. Postoperative pathology confirmed colon adenocarcinoma with pMMR. 3. Pathological confirmed pericolonic lymph node metastasis. 4. Radiological evidence without distant metastasis before surgery. 4. Receipt of at least 4 cycles of CapOX adjuvant chemotherapy postoperatively. 5. No preoperative neoadjuvant therapy. 6. A follow-up period of at least 12 months after the last chemotherapy cycle. The specific treatment regimen and method of administration for CapOX were as follows: Oxaliplatin at a dose of 130 mg/m2 was administered intravenously on the first day, and capecitabine at a dose of 1,000 mg/m^2 was administered orally twice daily on days 1–14 of a 3-week cycle. A total of 504 consecutive patients were selected, constituting the training cohort for the study. Additionally, 159 consecutive patients from Longyan First Affiliated Hospital of Fujian Medical University, who underwent curative surgery for colon cancer between January 2015 and December 2018, were included to form a validation cohort. Clinical and pathological information was obtained by four independent research assistants from the medical electronic record systems of the two centers. The use of clinical and pathological information was consented to by all patients. This study adhered to The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement Guidelines [20].
The calculation and categorization of the LODDS and risk score
The LODDS for each patient were calculated based on the number of dissected lymph nodes (NDLN) and the number of positive lymph nodes (NPLN). The formula used was \(log\frac{\text{NPLN }+0.050}{\text{NDLN }-\text{ NPLN }+ 0.050}\), which aimed to avoid undefined numbers by adding 0.050 to both the numerator and denominator. To standardize procedures and evaluations, we adopted the same cutoff points previously identified in large population studies as significantly impacting survival, categorizing patients into three groups based on LODDS values: LODDS0 (≤ − 1.36), LODDS1 (> − 1.36 and ≤ − 0.53), and LODDS2 (> − 0.53) [21, 22]. The risk score is derived by the method proposed by Cox et al. [23], involving the multiplication of the Cox model's coefficients (βi) by the individual's covariate values (xi) and the subsequent summation of these products. The calculation formula is expressed as follows: \(\mathrm{risk}\;\mathrm{score}\;={\mathrm\beta}_1{\mathrm x}_1+{\mathrm\beta}_2{\mathrm x}_2+\dots+{\mathrm\beta}_{\mathrm n}{\mathrm x}_{\mathrm n}\).
Follow up
Patients were followed up every 3 months during the initial 2 years post-surgery and thereafter semiannually for the next 3 years through clinical visits. The follow-up regimen encompassed physical examinations, evaluations of serum carcinoembryonic antigen (CEA) levels, endoscopic procedures, and Computed Tomography (CT) scans of the abdomen and pelvis. Disease-free survival (DFS) was defined as the period from the date of tumor removal to the occurrence of disease recurrence, death, or the date of the last follow-up, whichever came first. Overall survival (OS) spanned from the date of tumor resection to death from any cause or the last follow-up. The final follow-up dates were November 2023 for the training cohort and May 2022 for the validation cohort.
Statistical analysis
Descriptive analysis was employed to summarize the clinical features of the total patients. Baseline characteristics of the included population were described as medians (Interquartile Range, IQR) for continuous variables and numbers with percentages (n, %) for categorical variables. Statistical analysis and graph plotting were performed using R software (version 4.3.1) and Graphpad Prism 8. The "rms" package in R was utilized to construct nomograms, and the "timeROC" package was employed to draw time-dependent Receiver Operating Characteristic (ROC) curves at different time points and calculate the area under the ROC curve (AUC), with calibration curves assessing the consistency between predicted and actual survival times [24]. The Log-rank test was used to compare the survival of two groups of patients for statistical differences. Survival curves were plotted using the Kaplan–Meier method. To avoid overly optimistic results, all statistical analyses were repeated in the validation cohort to ensure the reliability of conclusions. All statistical tests were two-sided, with P < 0.05 considered statistically significant.
Result
Patient characteristics
Table 1 presents the demographic, clinical, and pathological characteristics of patients in the training cohort and validation cohort. The study encompassed a total of 663 patients, with 504 patients in the main cohort and 159 patients in the validation cohort. In the training cohort, the median age of patients was 61 years (IQR: 53–70 years). All participants received a minimum of four cycles of CapOX adjuvant chemotherapy, with 236 patients (46.83%) completing all eight cycles. After calculating the LODDS values, it was found that the median LODDS of patients was -0.85 (IQR: -1.07 to -0.56). Subsequently, stratification was performed: 38 patients were classified into the LODDS0 group (8.00%), 364 patients into the LODDS1 group (72.00%), and 102 patients into the LODDS2 group (20.00%). In the validation cohort, the median age of patients was 57 years (IQR: 47–65 years). All patients received more than four cycles of CapOX adjuvant chemotherapy, with 70 patients (44.03%) completing eight cycles. In this cohort, the median LODDS value for patients was -1.24 (IQR: -1.43 to -0.80). After stratification, there were 103 patients (65.00%) in the LODDS0 group, 35 patients (22.00%) in the LODDS1 group, and 21 patients (13.00%) in the LODDS2 group.
By the end of the follow-up period in training cohort, there were 95 patients (18.85%) who experienced recurrence or metastasis, and 45 patients (8.93%) succumbed to tumor-related causes. The 5-year survival rate and 5-year disease-free survival rate were 93.23% and 82.90%, respectively. In the validation cohort, 33 patients (20.75%) experienced recurrence or metastasis, and 22 patients (13.84%) died from tumor-related causes. The 5-year survival rate and 5-year disease-free survival rate were 85.51% and 78.28%, respectively. The median follow-up time for the training cohort was 62.74 months, while the median follow-up time for the validation cohort was 56.98 months.
Cox analysis in the training and validation cohorts
The results of univariate and multivariate Cox regression analyses, showing the factors influencing DFS of patients in the training cohort, are presented in Table 2. Univariate analysis revealed that tumors located in the right colon (HR = 1.550, 95% CI: 1.002–2.399, P = 0.049), perineural invasion (HR = 1.799, 95% CI: 1.053–3.012, P = 0.031), poor tumor differentiation (HR = 1.558, 95% CI: 1.034–2.348, P = 0.034), and LODDS grouping of 2 and 1 (HR = 1.155, 95% CI: 0.768–1.736, P < 0.001) were risk factors for DFS. The results of multivariate analysis indicated that perineural invasion (HR = 1.776, 95%CI: 1.052–3.003, P = 0.032), poor tumor differentiation (HR = 1.638, 95%CI: 1.084–2.475, P = 0.019), and LODDS grouping of 2 and 1 (HR = 1.920, 95%CI: 1.297–2.842, P = 0.001) were independent predictors for DFS. In the validation cohort, univariate analysis revealed that tumors located in the right colon (HR = 2.625, 95% CI: 1.103–6.250, P = 0.029), presence of perineural invasion (HR = 2.389, 95% CI: 1.034–5.516, P = 0.041), poor tumor differentiation (HR = 4.213, 95% CI: 1.647–10.78, P = 0.003), lympho-vascular invasion (HR = 2.438, 95% CI: 1.502–3.956, P < 0.001), and LODDS grouping of 2 and 1 (HR = 3.093, 95% CI: 1.318–7.255, P = 0.009) were identified as risk factors for DFS. Multivariate analysis revealed that the location of tumors in the right colon (HR = 2.667, 95% CI: 1.074–6.623, P = 0.035), poor tumor differentiation (HR = 3.618, 95% CI: 1.353–9.672, P = 0.010), and LODDS grouping of 2 and 1 (HR = 1.958, 95% CI: 1.086–3.532, P = 0.026) were identified as independent prognostic factors for DFS in the validation cohort (Table S1).
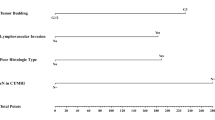
Development and validation of nomogram
A Cox regression model was fitted based on the independent predictors of DFS and a straightforward and intuitive nomogram (Fig. 1) was constructed, with the calculation of risk scores and the c-index based on the Cox model. The nomogram demonstrated that the LODDS contributed most significantly to the prognostic prediction. Furthermore, the same factors were included in a multivariate Cox regression model for the DFS of the validation cohort to verify the stability and reliability of the model. The c-index of 0.672 for the training cohort model indicated its predictive accuracy, while a c-index of 0.717 for the validation cohort further confirmed the model's reliability.
Subsequently, time-dependent ROC curves for 3-year and 5-year intervals were generated to assess the model's predictive efficacy. For the training cohort, the area under the curve (AUC) values at 3 years and 5 years were 0.706 and 0.678, respectively (Fig. 2A and B), whereas the validation cohort exhibited AUC values of 0.744 and 0.762 at the same time points (Fig. 2C and D). These findings demonstrated the model's capability to predict patient prognosis at different time intervals. Furthermore, the calibration curves for DFS at 3 years and 5 years, both in the training and validation cohorts, showcased a good agreement between the predicted probabilities and the actual occurrences (Fig. 3A-D). These results indicated that the Cox regression model is reliable in predicting patient DFS and can robustly support clinical decision-making.
Three-year calibration and five-year calibration diagram for assessment of the nomogram A 3-year calibration diagram for assessment of the nomogram in training cohort. B 3-year calibration diagram for assessment of the nomogram in validation cohort. C 5-year calibration diagram for assessment of the nomogram in training cohort. D 5-year calibration diagram for assessment of the nomogram in validation cohort
Prognostic analysis of different adjuvant chemotherapy duration with respect to nomogram model
By fitting Cox regression models separately for the training and validation cohorts, we calculated each patient's risk score using the model coefficients and covariate values. In the training cohort, the median risk score was 1.022 (IQR: 0.699–1.673); similarly, in the validation cohort, the median risk score was 1.062 (IQR: 0.561–2.009). To further demonstrate the model's utility in stratifying stage III colon cancer patients for postoperative chemotherapy, patients were divided into high-risk and low-risk groups based on their risk score, with a threshold set at 1. Survival analysis indicated that, in both the training and validation cohorts, grouping based on risk scores effectively differentiated the 5-year DFS rates between high-risk and low-risk groups (training cohort, 87.42% vs. 75.66%, P < 0.001; validation cohort, 93.17% vs. 74.98%, P = 0.001, Fig. 4A-B). Furthermore, the impact of receiving 8 cycles of CapOX chemotherapy compared to receiving 4–7 cycles of CapOX chemotherapy on the 5-year DFS rates in high-risk and low-risk patients was evaluated. The results showed that among patients in the high-risk group, in both the training and validation cohorts, there was a significant difference in the 5-year DFS rates between patients who received 8 cycles of CapOX chemotherapy and those who received 4–7 cycles (training cohort, 82.97% vs 67.17%, P = 0.013; validation cohort, 89.49% vs 63.97%, P = 0.030, Fig. 5A and B). However, among patients in the low-risk group, no difference in the 5-year DFS rates between the two treatment strategies was observed in either cohort (training cohort, 89.01% vs 86.48%, P = 0.314; validation cohort, 91.73% vs 94.22%, P = 0.681, Fig. 5C and D).
Kaplan–Meier survival analysis of DFS in stage III colon cancer patients between adjuvant chemotherapy 4–7 cycle and 8 cycle stratified by risk scores. A DFS for high-risk group in training cohort. B DFS for high-risk group in validation cohort. C DFS for low-risk group in training cohort. D DFS for low-risk group in validation cohort
Additionally, the guidance role of the American Joint Committee on Cancer (AJCC) Tumor, Node, Metastasis (TNM) staging in determining the duration of postoperative chemotherapy was also compared. Survival analysis was conducted in both the training and validation cohorts to evaluate the impact of the number of CapOX chemotherapy cycles on patient outcomes. After patients were divided into three groups based on TNM staging as IIIa, IIIb, and IIIc, the analysis was performed separately within these groups for both cohorts. There was no discernible difference in 5-year DFS between patients who received 8 cycles and those who received 4–7 cycles of CapOX chemotherapy within the three groups across both cohorts (Figures S1A-S1D).
To mitigate the confounding impact of other variables on survival outcomes, univariate Cox analyses were separately conducted for patients in the high-risk group of both the training and validation cohorts. The analysis results revealed that receiving 8 cycles of CapOX chemotherapy was an independent prognostic factor for DFS in patients, both in the training cohort (Table 3) and the validation cohort (Table S2). These findings further underscore the effectiveness and importance of the model in guiding the stratification of adjuvant chemotherapy regimens for patients with stage III colon cancer.
Discussion
In addition to TNM staging, this study constructed a Cox regression model by integrating the clinicopathological characteristics of stage III colon cancer patients, offering a refined risk stratification for this group. The research developed a prognostic model for predicting 5-year DFS in stage III colon cancer patients based on LODDS, tumor differentiation, and perineural invasion. Moreover, based on this model, patients were stratified to identify those who could benefit from six months of postoperative chemotherapy, thereby guiding the duration of adjuvant chemotherapy post-surgery.
Extensive research has demonstrated the value of LODDS in prognosticating outcomes for colon cancer across stages II-IV [16,17,18,19]. The study by Kuo et al. indicated that the number of negative lymph nodes was related to the prognosis of stage III colon cancer [25]. Both the lymph node ratio (LNR) and log odds of positive lymph nodes (LODDS) reflect the number of negative lymph nodes, highlighting their predictive value in stage III colon cancer. Compared to TNM staging or Lymph Node Ratio (LNR), LODDS has demonstrated superior predictive performance in colon cancer, according to previous reports [26]. Prior studies have constructed nomogram models utilizing LODDS to visually distinguish the prognostic outcomes of colon cancer patients, demonstrating significant predictive performance [27, 28]. Aligned with previous research, our study, which constructs a predictive model based on LODDS, showcases strong predictive power for the 3-year (training cohort AUC = 0.706, validation cohort AUC = 0.744) and 5-year DFS (training cohort AUC = 0.687, validation cohort AUC = 0.762) in stage III colon cancer patients. Moreover, within this model, LODDS is shown to carry the greatest weight, affirming its indispensable contribution to predicting DFS in this context.
It is noteworthy that most previous studies are based on the SEER database, inevitably lacking postoperative adjuvant chemotherapy information, including chemotherapy regimens and durations. This work represents the first evaluation of LODDS's guiding value on the duration of postoperative adjuvant chemotherapy in stage III colon cancer patients. Specifically, after stratifying patients into high-risk and low-risk groups through the predictive model, survival analysis confirmed that, in the high-risk group, patients receiving 8 cycles of CapOX regimen chemotherapy had significantly better 5-year DFS rates than those receiving fewer than 8 cycles, both in the training cohort (82.97% vs 67.17%, P = 0.013) and the validation cohort (89.49% vs 63.97%, P = 0.030). Subsequent univariate Cox analysis was conducted to exclude other potential baseline clinicopathological factors affecting survival, indicating that the number of Capox chemotherapy cycles is the only independent prognostic factor for the prognosis of high-risk group patients; however, no prognostic difference due to chemotherapy duration was observed when grouping patients according to TNM staging.
Compared to traditional models used for predicting prognosis in stage III colon cancer, our study integrates information from three postoperative pathological factors, providing a more comprehensive assessment and guidance for postoperative chemotherapy duration selection and prognosis evaluation for patients. In contrast to conventional N staging, LODDS is not influenced by the number of examined lymph nodes and can more accurately reflect the lymph node metastasis status. Integrating LODDS with factors such as the presence of perineural invasion and tumor differentiation allows for a comprehensive assessment of tumor biology based on pathological results, including local invasiveness, lymph node metastasis behavior, and microscopic morphology. Moreover, the pathological information this model utilizes is readily available, easy to obtain, and does not necessitate additional invasive procedures or tests, facilitating its clinical application.
This research is constrained by certain limitations. While it incorporates data from two centers, the presence of selection bias cannot be overlooked, highlighting the imperative for an expanded sample size to bolster the model’s credibility. Owing to the inclusion of cases from an earlier time period, it was not feasible to evaluate tumor deposit (TD) or tumor budding information. Furthermore, this study did not consider the role of molecular biomarkers in the recurrence of stage III colon cancer and in guiding adjuvant therapy. Minimal residual disease (MRD) has been proven to be a good predictor of early recurrence in colorectal cancer patients, and clinical studies have evaluated its guiding value for postoperative adjuvant therapy [29,30,31]. Additionally, KRAS and BRAF mutations have been thoroughly assessed for their prognostic value in stage II-III colon cancer [32]. Therefore, we believe that incorporating these molecular markers into future research could enhance the predictive performance of the model, enabling more precise postoperative adjuvant treatment for stage III colon cancer patients. In the future, the collection of prospective data strictly adhering to patient inclusion criteria, along with an increased number of external validation cohorts and the inclusion of a larger number of patients, as well as more factors related to prognosis, is expected to provide more robust and persuasive evidence for the model.
Conclusions
The study, drawing on data from two centers, confirms that a prognostic model incorporating LODDS, pathological differentiation, and the presence of neural invasion, demonstrates strong predictive performance for the prognosis of stage III colon cancer. Moreover, stratification of patients according to this model yields valuable predictions for the duration of postoperative adjuvant chemotherapy, highlighting the model's clinical utility.
Availability of data and materials
The authenticity of this article has been confirmed by uploading the key raw data to the Research Data Deposit public platform (www.researchdata.org.cn) under approval number RDDA2024841619. These data are available upon request from the corresponding author, Jianhong Peng.
References
Chagpar R, Xing Y, Chiang YJ, et al. Adherence to stage-specific treatment guidelines for patients with colon cancer. J Clin Oncol. 2012;30(9):972–9.
Gunderson LL, Jessup JM, Sargent DJ, Greene FL, Stewart AK. Revised TN categorization for colon cancer based on national survival outcomes data. J Clin Oncol. 2010;28(2):264–71.
Sobrero AF, Puccini A, Shi Q, et al. A new prognostic and predictive tool for shared decision making in stage III colon cancer. Eur J Cancer. 2020;138:182–8.
Argilés G, Tabernero J, Labianca R, et al. Localised colon cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2020;31(10):1291–305.
Benson AB, Venook AP, Al-Hawary MM, et al. Colon Cancer, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Cancer Netw. 2021;19(3):329–59.
André T, Vernerey D, Mineur L, et al. Three versus 6 months of oxaliplatin-based adjuvant chemotherapy for patients with stage iii colon cancer: disease-free survival results from a randomized, open-label, International Duration Evaluation of Adjuvant (IDEA) France, Phase III Trial. J Clin Oncol. 2018;36(15):1469–77.
Lonardi S, Sobrero A, Rosati G, et al. Phase III trial comparing 3–6 months of adjuvant FOLFOX4/XELOX in stage II-III colon cancer: safety and compliance in the TOSCA trial. Ann Oncol. 2017;28(12):3110.
Saltz LB, Niedzwiecki D, Hollis D, et al. Irinotecan fluorouracil plus leucovorin is not superior to fluorouracil plus leucovorin alone as adjuvant treatment for stage III colon cancer: results of CALGB 89803. J Clin Oncol. 2007;25(23):3456–61.
Taieb J, Tabernero J, Mini E, et al. Oxaliplatin, fluorouracil, and leucovorin with or without cetuximab in patients with resected stage III colon cancer (PETACC-8): an open-label, randomised phase 3 trial. Lancet Oncol. 2014;15(8):862–73.
Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17(6):1471–4.
Mo S, Zhou Z, Li Y, et al. Establishment and validation of a novel nomogram incorporating clinicopathological parameters into the TNM staging system to predict prognosis for stage II colorectal cancer. Cancer Cell Int. 2020;20:285.
Merkel S, Mansmann U, Papadopoulos T, Wittekind C, Hohenberger W, Hermanek P. The prognostic inhomogeneity of colorectal carcinomas Stage III: a proposal for subdivision of Stage III. Cancer. 2001;92(11):2754–9.
Vinh-Hung V, Verschraegen C, Promish DI, et al. Ratios of involved nodes in early breast cancer. Breast Cancer Res. 2004;6(6):R680–688.
Sun Z, Xu Y, de Li M, et al. Log odds of positive lymph nodes: a novel prognostic indicator superior to the number-based and the ratio-based N category for gastric cancer patients with R0 resection. Cancer. 2010;116(11):2571–80.
Salari A, Ghahari M, Nowroozi A, et al. Log Odds of Positive Lymph Nodes (LODDS) as an independent predictor of overall survival following radical cystectomy in urothelial bladder cancer: time to rethink conventional node staging. Clin Genitourin Cancer. 2023;21(3):e175–81.
Wang J, Hassett JM, Dayton MT, Kulaylat MN. The prognostic superiority of log odds of positive lymph nodes in stage III colon cancer.J Gastrointest Surg. 2008;12(10):1790–6.
Persiani R, Cananzi FC, Biondi A, et al. Log odds of positive lymph nodes in colon cancer: a meaningful ratio-based lymph node classification system. World J Surg. 2012;36(3):667–74.
Pei JP, Zhang CD, Fan YC, Dai DQ. Comparison of different lymph node staging systems in patients with resectable colorectal cancer. Front Oncol. 2018;8:671.
Scarinci A, Di Cesare T, Cavaniglia D, et al. The impact of log odds of positive lymph nodes (LODDS) in colon and rectal cancer patient stratification: a single-center analysis of 323 patients. Updat Surg. 2018;70(1):23–31.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573–7.
Arslan NC, Sokmen S, Canda AE, Terzi C, Sarioglu S. The prognostic impact of the log odds of positive lymph nodes in colon cancer. Colorectal Dis. 2014;16(11):O386–392.
Song YX, Gao P, Wang ZN, et al. Which is the most suitable classification for colorectal cancer, log odds, the number or the ratio of positive lymph nodes? PLoS One. 2011;6(12):e28937.
Cox DR. Regression models and life-tables. Journal of the Royal Statistical Society: Series B (Methodological). 1972;34(2):187–202. https://doi.org/10.1111/j.2517-6161.1972.tb00899.x.
Blanche P, Dartigues JF, Jacqmin-Gadda H. Estimating and comparing time-dependent areas under receiver operating characteristic curves for censored event times with competing risks. Stat Med. 2013;32(30):5381–97.
Kuo YH, You JF, Hung HY, Chin CC, Chiang JM, Chang CH. Number of negative lymph nodes with a positive impact on survival of stage III colon cancer; a retrospective observation study for right side and left side colon. BMC Cancer. 2022;22(1):126.
Baqar AR, Wilkins S, Wang W, Oliva K, McMurrick P. Log odds of positive lymph nodes is prognostically equivalent to lymph node ratio in non-metastatic colon cancer. BMC Cancer. 2020;20(1):762.
Zhu J, Hao J, Ma Q, et al. A novel prognostic model and practical nomogram for predicting the outcomes of colorectal cancer: based on tumor biomarkers and log odds of positive lymph node scheme. Front Oncol. 2021;11: 661040.
Cai H, Xu T, Zhuang Z, et al. Value of the log odds of positive lymph nodes for prognostic assessment of colon mucinous adenocarcinoma: Analysis and external validation. Cancer Med. 2021;10(23):8542–57.
Naidoo M, Gibbs P, Tie J. ctDNA and adjuvant therapy for colorectal cancer: time to reinvent our treatment paradigm. Cancers. 2021;13(2):346. https://doi.org/10.3390/cancers13020346.
Killock D. Early MRD predicts disease recurrence and benefit from adjuvant chemotherapy in CRC. Nat Rev Clin Oncol. 2023;20(3):137.
Wang DS, Yang H, Liu XY, et al. Dynamic monitoring of circulating tumor DNA to predict prognosis and efficacy of adjuvant chemotherapy after resection of colorectal liver metastases. Theranostics. 2021;11(14):7018–28.
Won DD, Lee JI, Lee IK, Oh ST, Jung ES, Lee SH. The prognostic significance of KRAS and BRAF mutation status in Korean colorectal cancer patients. BMC Cancer. 2017;17:1–12. https://doi.org/10.1186/s12885-017-3381-7.
Acknowledgements
We greatly appreciated the help from all of our colleagues in the Department of Colorectal Surgery at Sun Yat-sen University Cancer Center who were involved in administering the treatments in the current study.
Funding
The work was supported by the Science and Technology Projects in Guangzhou (No. 2023A04J1078) and Beijing Xisike Clinical Oncology Research Foundation (Y-Young2022—0023 and Y-Gilead2024-PT-0006).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by WL.Z, LJ.Z and JX.C. The first draft of the manuscript was finished by WL.Z and JH.P. ZL.H, XL.H, DB.X and WF. W coordinated and participated in the study. JH.P, ZH.L, and XJ.W commented and revised the previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study received approval from the Ethics Committees of Sun Yat-sen University Cancer Center (Approval number: B2023-272–01) and Longyan First Affiliated Hospital of Fujian Medical University (LYREC2024-k075-01). Informed consent was obtained from all patients whose clinical data were used.
Consent for publication
Approved for publication by all participants.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, W., Hou, Z., Zhang, L. et al. A log odds of positive lymph nodes-based predictive model effectively forecasts prognosis and guides postoperative adjuvant chemotherapy duration in stage III colon cancer: a multi-center retrospective cohort study. BMC Cancer 24, 1088 (2024). https://doi.org/10.1186/s12885-024-12875-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12875-6