Abstract
Background
Many studies have explored the clinicopathological features and prognosis between colorectal mucinous adenocarcinoma (MAC) and adenocarcinoma (AC) and have given different results. This meta-analysis summarizes previous evidence and evaluates the clinicopathological and prognostic features of MAC relative to AC in colorectal cancers (CRCs).
Methods
The meta-analysis was conducted by searching the databases of PubMed, China National Knowledge Infrastructure (CNKI), WANFANG data, Embase, and Web of Science. Pooled odds ratios (ORs) and hazard ratios (HRs) and corresponding 95% confidence intervals (CIs) were calculated to assess the clinicopathological and prognostic differences between MAC and AC.
Results
Fifty-six studies involving 803157 patients met the inclusion criteria and were included in this meta-analysis. The clinicopathological features of MAC were greatly different from AC, except for lymphatic invasion (OR = 1.07, 95% CI: 0.99–1.15, P = 0.09) and perineural invasion (OR = 0.92, 95% CI: 0.79–1.06, P = 0.09). Further investigation found that MAC predicted poor OS (HR = 1.04, 95% CI: 1.03–1.04, P < 0.01), but not DFS in CRCs (HR = 1.01,95% CI: 0.88- 1.17, P = 0.85). Subgroup analysis found that MAC was obviously correlated with OS in patients with different recruitment time, with tumor located in rectum, from different regions, with different sample sizes and with TNM stage in II, and calculated by different data types(P < 0.01).
Conclusions
This study shows that MAC displays obviously different clinicopathological features compared with AC. And MAC has a poor OS relative to AC but the DFS was comparable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is one of the leading causes of cancer-related death worldwide [1]. Different histological subtypes of CRC may exhibit quite different clinical characteristics and survival outcomes [2]. Most CRCs are classical adenocarcinomas (AC), and less frequent subtypes mainly include mucinous adenocarcinomas (MAC) and signet-ring cell carcinomas [3]. MAC, with extracellular mucin > 50% of the tumor, accounts for 10–15% of CRCs [4].
The results of previous studies investigating the clinicopathological and prognostic features are controversial [5]. Molecular and genetic analyses revealed significantly differences between MAC and AC, indicating a prominently different oncogenic development [6, 7]. MAC is more advanced at diagnosis, located mainly at the right side and has a poor prognosis compared with AC [8, 9]. In addition, MAC has a less firm consistency, which may cause symptoms to arise only when the tumor reaches an advanced stage [10]. Adjuvant chemotherapy should be routinely recommended for patients with MAC stage II, and special attention should be paid during their follow-up for chemoradiotherapy resistance [11]. Therefore, the prognosis and clinicopathological characteristics of MAC deserve further investigations. Previous studies quantitatively assessing the differences of clinicopathological features and prognosis in MAC and AC were systematically reviewed in this meta-analysis.
Methods
The reporting of this systematic review follows the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) statement [12].
Search strategy and study selection
The literature was searched using PubMed, China National Knowledge Infrastructure (CNKI), WANFANG data, Embase, and Web of Science in December, 2022. The search free-text terms used were (((((mucinous) OR (mucus OR colloid)) AND (cancer OR tumor OR neoplasm OR adenocarcinoma OR malign))) AND (rectal OR colon OR colorectal OR rectum)) AND (prognosis). The control terms used in PubMed were (colorectal neoplasms) OR (colonic neoplasms) OR (rectal neoplasms) and (adenocarcinoma, mucinous). Articles included should meet the following criteria: (1) sufficient information for calculating HR and 95% CI; (2) prognosis features presented in adenocarcinoma and mucinous adenocarcinoma patients; Articles were excluded if they were:(1)narrative reviews, case reports, congress abstracts; (2) studies without comparison of survival data; (3) neither English nor Chinese articles. In total, 56 studies were included in the final meta-analysis [5, 8,9,10,11, 13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63]. A flow diagram of the study selection and exclusion of duplicate articles process is presented in Fig. 1.
Data collection
Two authors reviewed all the involved articles and extracted the data independently. Disagreements between the 2 authors were resolved with consensus. We independently extracted the following data from each article: basic research information (name of the first author, publication time, region, number of patients included, survival analysis method); clinicopathological features of patients (gender, age, tumor location, CEA, tumor size, differentiation, metastasis location, lymphatic invasion, venous invasion, peritoneal metastasis, lymph node metastasis, distant metastasis, the mutation of KRAS and BRAF,MSI status, TNM stage and Duke’s stage); prognosis (the HRs of the ratio of MAC to AC for overall survival (OS), disease-free survival (DFS), as well as their 95% CIs and P values). If available, HRs and 95% CIs were preferentially obtained from multivariate results. Otherwise, they were extracted from univariable outcomes or calculated using Engauge Digitizer version 4.1 (free software down-loaded from http://sourceforge.net) to read the Kaplan–Meier survival curves to get the HRs and 95% CIs [64,65,66].
Quality assessment
We independently assessed the quality of all eligible studies using the Newcastle–Ottawa quality assessment scale (NOS). The NOS criteria evaluates the quality of articles from the following three aspects: (1) subject selection, (2) comparability of subject, (3) clinical outcome. We scored the included studies based on these three aspects. Based on the NOS standard score of 7–9, we defined high-quality quality research, 4–6 points for medium quality research, less than 4 points for low quality research.
Statistical analysis
We used Stata statistical software version 15.0 (Stata Corporation, College Station, Texas, USA) and Review Manager version 5 (Revman; The Nordic Cochrane Centre, Copenhagen, Denmark) to perform comprehensive meta-analysis. We used Odds ratios (ORs) and Hazard ratio with 95% confidence intervals (CIs) to evaluate the clinicopathological and prognostic differences between AC and MAC, respectively. The statistical significance of the pooled OR and HR was evaluated with the Z test and P values, and P < 0.05 was considered statistically significant. Subgroup analysis was conducted to analyze the sources of heterogeneity, which was assessed by means of Q and I2 statistic. Publication bias was assessed by the Begg’s rank correlation method and Egger’s weighted regression method and P value less than 0.05 was considered statistically significant. In addition, we used sensitivity analysis to assess the influence of a single study on pooled HR.
Results
Study selection and description of the included studies
A total of 8176 articles were obtained through database retrieval. After removing duplicated studies and irrelevant studies (included not related to CRC and not related to MAC) through screening title and abstract, 240 studies were remained. Then, we read the full texts of the articles carefully, articles without prognosis, incomplete and language restrictions were eliminated and 56 studies met our inclusion criteria were finally included in this meta-analysis. The main characteristics of the included studies are presented in Table 1. These studies were published between 1976 and 2022. A total of 803,157 patients (sample sizes ranged from 70 to 164,628) were included in this review. The relationship of OS between AC and MAC was described in 54 studies [5, 8,9,10,11, 13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43, 45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60, 62, 63] and DFS was compared in 13 studies [9, 11, 44, 46,47,48, 52, 53, 55, 59, 61,62,63]. Some included studies explored the relationship of OS and DFS between MAC and AC in colon and rectum and different TNM stages. The features of the included studies are listed in Table 1. All of the eligible studies scored more than five by NOS, revealing a high methodological quality across all studies.
Differences of clinicopathological features between MAC and AC
Differences of clinicopathological features between MAC and AC were presented in all included studies. MAC was significantly correlated with multiple clinicopathological features, including female(OR = 0.87, 95% CI: 0.86–0.88, P < 0.01), tumor located in colon(OR = 1.79, 95% CI: 1.76–1.83, P < 0.01), tumor size ≥ 5 cm(OR = 2.26, 95% CI: 2.17–2.36, P < 0.01), CEA ≥ 5 ng/mL (OR = 1.62, 95% CI:1.38–1.88,P < 0.01), advanced T,N,M stages(OR = 0.88, 95% CI: 0.87–0.90, P < 0.01), advanced Duke’s stage(OR = 0.57, 95% CI: 0.46–0.72, P < 0.01), moderate and well differentiation(OR = 0.84, 95% CI: 0.82–0.85, P < 0.01), non-vascular invasion(OR = 0.87, 95% CI: 0.78–0.98, P < 0.01), non- lymphovascular invasion(OR = 0.84, 95% CI: 0.74–0.95, P < 0.01), BRAF mutation(OR = 2.80, 95% CI: 1.99–3.94, P < 0.01), non-KRAS mutation(OR = 0.68, 95% CI: 0.55–0.85, P < 0.01), MSI-H status(OR = 2.80, 95% CI: 1.99–3.94, P < 0.01), lymph node metastasis (OR = 2.59, 95% CI: 2.17–3.11, P < 0.01), non-liver metastasis (OR = 0.51, 95% CI: 0.41–0.63, P < 0.01), non-lung metastasis (OR = 0.62, 95% CI: 0.40–0.95, P = 0.03), except for lymphatic invasion (OR = 1.07, 95% CI: 0.99–1.15, P = 0.09), and perineural invasion(OR = 0.92, 95% CI: 0.79–1.06, P = 0.25) (Table 2).
Prognostic value of MAC in CRCs
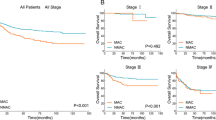
A total of 54 studies was enrolled to detect the prognostic value of MAC in OS. A random-effect model was used to calculate the pooled HR and 95% CI because excessive heterogeneity existed among studies (P < 0.01, I2 = 86%) (Fig. 2a). Overall, MAC predicted poor OS compared with AC (HR = 1.04, 95% CI: 1.03–1.04, P < 0.01), but the DFS was comparable between MAC and AC (HR = 1.01,95% CI: 0.88- 1.17, P = 0.85) (Fig. 2b). To detect potential heterogeneity, subgroup analyses were performed based on recruitment time, region, tumor location, TNM stage, sample size and data type used for calculating survival. As shown in Table 3, MAC was obviously correlated with OS in cohorts with different recruitment time (recruited before 2012 HR = 1.01, 95% CI: 1–1.03, P = 0.01; recruited after 2012 HR = 1.04, 95% CI: 1.04–1.05, P < 0.01), with tumor located in rectum (HR = 1.09, 95% CI: 1.07–1.11, P < 0.01), from different regions (from eastern Asia HR = 1.06, 95% CI: 1.05–1.06, P < 0.01; from other regions HR = 1.02, 95% CI: 1.02–1.03, P < 0.01), with different sample size (≥ 500 HR = 1.04, 95% CI: 1.03–1.04, P < 0.01; < 500 HR = 1.13, 95% CI: 1.08–1.19, P < 0.01), with different data types (analysed with multivariate method HR = 1.02, 95% CI: 1.02–1.03, P < 0.01; analysed with Univariate or K-M survival curves HR = 1.11, 95% CI: 1.1–1.13, P < 0.01), and with TNM stage II (HR = 1.39, 95% CI: 1.07–1.8, P < 0.01). However, the OS were not statistically different in MAC and AC patients with tumor located in colon (HR = 1.01, 95% CI: 1–1.02, P = 0.21), TNM stage III (HR = 1.02, 95% CI: 0.95–1.09, P = 0.64) and IV (HR = 1.13, 95% CI: 0.91–1.41, P = 0.27) (Table 3). As shown in Table 4, no significant difference was detected in DFS between MAC and AC.
Publication bias and sensitivity analysis
The funnel plots of publication bias of 54 studies for OS and 13 studies for DFS showed basic symmetry (Fig. 3A and B). Evaluation of publication bias using Begg’s and Egger’s tests also showed that no publication bias existed (P value of Begg’s test, 0.893 and 0.760 for OS and DFS, respectively; P value of Egger’s test, 0.065 and 0.373 for OS and DFS, respectively). Furthermore, to evaluate the results of meta-analysis, sensitivity analysis was conducted. No significant change was found in the results when any one study was excluded, confirming the robustness and reliability of meta-analysis results on both OS and DFS (Table 5).
Discussion
This systemic review and meta-analysis explore the differences of clinicopathological features and prognosis between MAC and AC, it covers a wide range of time from 1976—2022, 56 articles and 803,157 patients. Previous studies have confirmed that MAC often presents with advanced stages [36, 41, 52, 67]. This meta-analysis also showed that MAC was significantly associated with advanced TNM stage and lymph node metastasis. Besides, rate of lymphovascular invasion was also higher in MAC than in AC. These results indicate the essential role of mucin in local development and metastasis in MAC.
However, lymphatic invasion (OR = 1.07, 95%CI: 0.99–1.15, P = 0.09) and perineural invasion (OR = 0.92, 95%CI: 0.79–1.06, P = 0.25) were not correlated with MAC as revealed in this study. Compared with AC, MAC was reported to be associated with different molecular features, such as MSI and mutations in BRAF, KRAS [68]. This meta-analysis suggests that MAC has higher KRAS mutation and lower BRAF mutation tendency. MSI-H is a well-established prognostic biomarker for better survival [49]. Consistent with previous studies [9, 28, 29, 33, 69], MAC patients exhibited a higher rate of MSI-H, which might provide clues for using immunotherapy in MAC.
The prognosis of MAC patients is a pivotal topic but has always been in controverse, this meta-analysis suggests that MAC has a poor OS but comparable DFS compared with AC. Previous studies have suggested that the OS of MAC changes with tumor location and stage [9, 29, 41]. Subgroup analysis in this study found that MAC was correlated with OS in cohorts with TNM stage II and tumor located in rectum, but not with III or IV stage and tumor located in colon. So the prognosis of patients with MAC also varies and should be evaluated according to the localization of the tumor and TNM staging. We included 13 articles to explore the relationship of DFS between AC and MAC, however, no difference was found.
This meta-analysis has several limitations. First, heterogeneity in the meta-analysis is significant, although sensitivity analysis revealed the prognostic value of MAC by removing each study individually. Second, the number of patients recruited in some included studies was relatively small. Third, the included studies comprise a long time period and cover a diverse geographical origin, differences in treatment may affect survival analysis for MAC. Fortunately, publication bias was not detected for 54 studies for OS and 13 studies for DFS, and sensitivity analysis revealed that no significant change was found in the results when any 1 study was excluded. Finally, although we use Begg’s and Egger’s tests to assess the publication bias in our meta-analysis, some missing data were inevitable.
Conclusions
MAC has greatly different clinicopathological features compared with AC. And MAC indicated a poor OS relative to AC, though the DFS was comparable. This evidence suggests that MAC should be regarded as an unique cancer to treat, and further studies are needed to better define the mechanism of MAC initiation and development.
Availability of data and materials
The data that support the findings of this study are available upon request.
References
Haggar FA, Boushey RP. Colorectal cancer epidemiology: incidence, mortality, survival, and risk factors. Clin Colon Rectal Surg. 2009;22(4):191–7.
Zhu LL, Ling CR, Xu T, Zhang JL, Zhang YJ, Liu YJ, Fang C, Yang L, Zhuang W, Wang R, Ping J, Wang MJ. Clinicopathological features and survival of signet-ring cell carcinoma and mucinous adenocarcinoma of right colon, left colon, and rectum. Pathol Oncol Res. 2021;27:1609800.
Li ZH, You DY, Gao DP, Yang GJ, Dong XX, Zhang DF, Ding YY. Role of CT scan in differentiating the type of colorectal cancer. Onco Targets Ther. 2017;10:2297–303.
Hugen N, van Beek JJ, de Wilt JH, Nagtegaal ID. Insight into mucinous colorectal carcinoma: clues from etiology. Ann Surg Oncol. 2014;21(9):2963–70.
Wu S, Wu SJ, He YL, Cai SR, Zhang CH, Zhang XH, Zhan WH. Clinicopathologic features and survival of patients with colorectal mucinous, signet-ring cell or non-mucinous adenocarcinoma: experience at an institution in southern China. Chin Med J (Engl). 2009;122(13):1486–91.
Hanski C. Is mucinous carcinoma of the colorectum a distinct genetic entity? Br J Cancer. 1995;72(6):1350–6.
Song GA, Deng G, Bell I, Kakar S, Sleisenger MH, Kim YS. Mucinous carcinomas of the colorectum have distinct molecular genetic characteristics. Int J Oncol. 2005;26(3):745–50.
Mehrdad P, Masoud S, Edris S, Mehrnoush S. Mucinous and non-mucinous adenocarcinoma in colorectal cancer patients. Ann Oncol. 2017;28:iii83.
Park JS, Huh JW, Park YA, Cho YB, Yun SH, Kim HC, Lee WY, Chun HK. Prognostic comparison between mucinous and nonmucinous adenocarcinoma in colorectal cancer. Medicine (Baltimore). 2015;94(15):e658.
Lan YT, Chang SC, Lin PC, Lin CC, Lin HH, Huang SC, Lin CH, Liang WY, Chen WS, Jiang JK, Lin JK, Yang SH. Clinicopathological and molecular features of colorectal cancer patients with mucinous and non-mucinous adenocarcinoma. Front Oncol. 2021;11:620146.
Wang L, Hirano Y, Heng G, Ishii T, Kondo H, Hara K, Obara NA, Asari M, Kato T, Yamaguchi S. Mucinous adenocarcinoma as a high-risk factor in stage II colorectal cancer: a propensity score-matched Study from Japan. Anticancer Res. 2020;40(3):1651–9.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li TJ, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Symonds and Vickery. Mucinous carcinoma of the colon and rectum. Cancer. 1976;37(4):1891–900.
Umpleby HC, Ranson DL, Williamson RC. Peculiarities of mucinous colorectal carcinoma. Br J Surg. 1985;72(9):715–8.
Halvorsen TB, Seim E. Influence of mucinous components on survival in colorectal adenocarcinomas: a multivariate analysis. J Clin Pathol. 1988;41(10):1068–72.
Connelly JH, Robey-Cafferty SS, Cleary KR. Mucinous carcinomas of the colon and rectum. An analysis of 62 stage B and C lesions. Arch Pathol Lab Med. 1991;115(10):1022–5.
PonzdeLeon M, Sant M, Micheli A, Sacchetti C, Di Gregorio C, Fante R, Zanghieri G, Melotti G, Gatta G. Clinical and pathologic prognostic indicators in colorectal cancer. A population-based study. Cancer. 1992;69(3):626–35.
Green JB, Timmcke AE, Mitchell WT, Hicks TC, Gathright JB, Ray JE. Mucinous carcinoma–just another colon cancer? Dis Colon Rectum. 1993;36(1):49–54.
Yamamoto S, Mochizuki H, Hase K, Yamamoto T, Ohkusa Y, Yokoyama S, Ushitani Y, Tamakuma S. Assessment of clinicopathologic features of colorectal mucinous adenocarcinoma. Am J Surg. 1993;166(3):257–61.
Secco GB, Fardelli R, Campora E, Lapertosa G, Gentile R, Zoli S, Prior C. Primary mucinous adenocarcinomas and signet-ring cell carcinomas of colon and rectum. Oncology. 1994;51(1):30–4.
Cusack JC, Giacco GG, Cleary K, Davidson BS, Izzo F, Skibber J, Yen J, Curley SA. Survival factors in 186 patients younger than 40 years old with colorectal adenocarcinoma. J Am Coll Surg. 1996;183(2):105–12.
Wu CS, Tung SY, Chen PC, Kuo YC. Clinicopathological study of colorectal mucinous carcinoma in Taiwan: a multivariate analysis. J Gastroenterol Hepatol. 1996;11(1):77–81.
Cerottini JP, Caplin S, Pampallona S, Givel JC. Prognostic factors in colorectal cancer. Oncol Rep. 1999;6(2):409–14.
Consorti F, Lorenzotti A, Midiri G, Di Paola M. Prognostic significance of mucinous carcinoma of colon and rectum: a prospective case-control study. J Surg Oncol. 2000;73(2):70–4.
Nozoe T, Anai H, Nasu S, Sugimachi K. Clinicopathological characteristics of mucinous carcinoma of the colon and rectum. J Surg Oncol. 2000;75(2):103–7.
Purdie CA, Piris J. Histopathological grade, mucinous differentiation and DNA ploidy in relation to prognosis in colorectal carcinoma. Histopathology. 2000;36(2):121–6.
Kanemitsu Y, Kato T, Hirai T, Yasui K, Morimoto T, Shimizu Y, Kodera Y, Yamamura Y. Survival after curative resection for mucinous adenocarcinoma of the colorectum. Dis Colon Rectum. 2003;46(2):160–7.
Du W, Mah JT, Lee J, Sankila R, Sankaranarayanan R, Chia KS. Incidence and survival of mucinous adenocarcinoma of the colorectum: a population-based study from an Asian country. Dis Colon Rectum. 2004;47(1):78–85.
Kang H, O’Connell JB, Maggard MA, Sack J, Ko CY. A 10-year outcomes evaluation of mucinous and signet-ring cell carcinoma of the colon and rectum. Dis Colon Rectum. 2005;48(6):1161–8.
Negri FV, Wotherspoon A, Cunningham D, Norman AR, Chong G, Ross PJ. Mucinous histology predicts for reduced fluorouracil responsiveness and survival in advanced colorectal cancer. Ann Oncol. 2005;16(8):1305–10.
Grillo-Ruggieri F, Mantello G, Berardi R, Cardinali M, Fenu F, Iovini G, Montisci M, Fabbietti L, Marmorale C, Guerrieri M, Saba V, Bearzi I, Mattioli R, Bonsignori M, Cascinu S. Mucinous rectal adenocarcinoma can be associated to tumor downstaging after preoperative chemoradiotherapy. Dis Colon Rectum. 2007;50(10):1594–1603.
Hill DA, Furman WL, Billups CA, Riedley SE, Cain AM, Rao BN, Pratt CB, Spunt SL. Colorectal carcinoma in childhood and adolescence: a clinicopathologic review. J Clin Oncol. 2007;25(36):5808–14.
Lee WS, Chun HK, Lee WY, Yun SH, Cho YB, Yun HR, Park SH, Song SY. Treatment outcomes in patients with signet ring cell carcinoma of the colorectum. Am J Surg. 2007;194(3):294–8.
Farhat MH, Barada KA, Tawil AN, Itani DM, Hatoum HA, Shamseddine AI. Effect of mucin production on survival in colorectal cancer: a case-control study. World J Gastroenterol. 2008;14(45):6981–5.
Pande R, Sunga A, LeVea C, Wilding GE, Bshara W, Reid M, Fakih MG. Significance of signet-ring cells in patients with colorectal cancer. Dis Colon Rectum. 2008;51(1):50–5.
Catalano V, Loupakis F, Graziano F, Torresi U, Bisonni R, Mari D, Fornaro L, Baldelli AM, Giordani P, Rossi D, Alessandroni P, Giustini L, Silva RR, Falcone A, D'Emidio S and Fedeli SL. Mucinous histology predicts for poor response rate and overall survival of patients with colorectal cancer and treated with first-line oxaliplatin- and/or irinotecan-based chemotherapy. Br J Cancer. 2009;100(6):881–7.
Chew MH, Koh PK, Ng KH, Eu KW. Improved survival in an Asian cohort of young colorectal cancer patients: an analysis of 523 patients from a single institution. Int J Colorectal Dis. 2009;24(9):1075–83.
Sultan I, Rodriguez-Galindo C, El-Taani H, Pastore G, Casanova M, Gallino G, Ferrari A. Distinct features of colorectal cancer in children and adolescents: a population-based study of 159 cases. Cancer. 2010;116(3):758–65.
Catalano V, Loupakis F, Graziano F, Bisonni R, Torresi U, Vincenzi B, Mari D, Giordani P, Alessandroni P, Salvatore L, Fornaro L, Santini D, Baldelli AM, Rossi D, Giustini L, Silva RR, Falcone A, D'Emidio S, Rocchi M, Fedeli SL. Prognosis of mucinous histology for patients with radically resected stage II and III colon cancer. Ann Oncol. 2012;23(1):135–U111.
Hyngstrom JR, Hu CY, Xing Y, You YN, Feig BW, Skibber JM, Rodriguez-Bigas MA, Cormier JN, Chang GJ. Clinicopathology and outcomes for mucinous and signet ring colorectal adenocarcinoma: analysis from the National Cancer Data Base. Ann Surg Oncol. 2012;19(9):2814–21.
Numata M, Shiozawa M, Watanabe T, Tamagawa H, Yamamoto N, Morinaga S, Watanabe K, Godai T, Oshima T, Fujii S, Kunisaki C, Rino Y, Masuda M, Akaike M. The clinicopathological features of colorectal mucinous adenocarcinoma and a therapeutic strategy for the disease. World J Surg Oncol. 2012;10:109.
Hugen N, Verhoeven RH, Radema SA, De Hingh IH, Pruijt JF, Nagtegaal ID, Lemmens VE, De Wilt JH. Prognosis and value of adjuvant chemotherapy in stage III mucinous colorectal carcinoma. Ann Oncol. 2013;24(11):2819–24.
Imai Y, Yamagishi H, Fukuda K, Ono Y, Inoue T, Ueda Y. Differential mucin phenotypes and their significance in a variation of colorectal carcinoma. World J Gastroenterol. 2013;19(25):3957–68.
Kim SH, Shin SJ, Lee KY, Kim H, Kim TI, Kang DR, Hur H, Min BS, Kim NK, Chung HC, Roh JK, Ahn JB. Prognostic value of mucinous histology depends on microsatellite instability status in patients with stage III colon cancer treated with adjuvant FOLFOX chemotherapy: a retrospective cohort study. Ann Surg Oncol. 2013;20(11):3407–13.
Xu MM, WengZH, Lin Y, Wang WF, Lin JR, Zhuang YZ. Analyzing of the clinicopathological features and prognosis in mucinous colorectal cancer patients. Modern Med. 2013;21:21–3.
Hogan J, Burke JP, Samaha G, Condon E, Waldron D, Faul P, Coffey JC. Overall survival is improved in mucinous adenocarcinoma of the colon. Int J Colorectal Dis. 2014;29(5):563–9.
Ooki A, Akagi K, Yatsuoka T, Asayama M, Hara H, Yamamoto G, Nishimura Y, Yamaguchi K. Inverse effect of mucinous component on survival in stage III colorectal cancer. J Surg Oncol. 2014;110(7):851–7.
Foda AA, El-Hawary AK, Aziz AA. Colorectal adenocarcinoma with mucinous component: relation of MMP-13, EGFR, and E-cadherin expressions to clinicopathological features and prognosis. APMIS. 2015;123(6):502–8.
Inamura K, Yamauchi M, Nishihara R, Kim SA, Mima K, Sukawa Y, Li TT, Yasunari M, Zhang XH, Wu KN, Meyerhardt JA, Fuchs CS, Harris CC, Qian ZR, Ogino S. Prognostic significance and molecular features of signet-ring cell and mucinous components in colorectal carcinoma. Ann Surg Oncol. 2015;22(4):1226–35.
Nitsche U, Friess H, Agha A, Angele M, Eckel R, Heitland W, Jauch KW, Krenz D, Nüssler NC, Rau HG, Ruppert R, Schubert-Fritschle G, Wilhelm D, Werner J, Engel J. Mucinous and signet-ring cell colorectal cancer: results of a population based cohort. United Eur Gastroenterol J. 2016;4(5):A464.
Ott C, Gerken M, Hirsch D, Fest P,Fichtner-Feigl S, Munker S, Schnoy E, Stroszczynski C, Vogelhuber M, Herr W, Evert M, Reng M, Schlitt HJ, Klinkhammer-Schalke M, Teufel A. Advanced mucinous colorectal cancer -epidemiology, prognosis and efficacy of chemotherapeutic treatment. Z Gastroenterol. 2016;54:8.
Hosseini S, Bananzadeh AM, Salek R, Zare-Bandamiri M, Kermani AT, Mohammadianpanah M. Prognostic significance of mucinous histologic subtype on oncologic outcomes in patients with colorectal cancer. Ann Coloproctol. 2017;33(2):57–63.
Soliman BG, Karagkounis G, Church JM, Plesec T, Kalady MF. Mucinous histology signifies poor oncologic outcome in young patients with colorectal cancer. Dis Colon Rectum. 2018;61(5):547–53.
Dai D, Zhou B, Zhong Y, Jin H, Wang X. Survival of patients with resected primary colorectal mucinous adenocarcinoma: a competing risk nomogram analysis. Oncol Lett. 2019;18(6):6594–604.
Li C, Zheng H, Jia H, Huang D, Gu W, Cai S, Zhu J. Prognosis of three histological subtypes of colorectal adenocarcinoma: a retrospective analysis of 8005 Chinese patients. Cancer Med. 2019;8(7):3411–9.
Li ZP, Liu XY, Kao XM, Chen YT, Han SQ, Huang MX, Liu C, Tang XY, Chen YY, Xiang D, Huang YD, Lei ZJ, Chu XY. Clinicopathological characteristics and prognosis of colorectal mucinous adenocarcinoma and nonmucinous adenocarcinoma: a surveillance, epidemiology, and end results (SEER) population-based study. Ann Transl Med. 2020;8(5):205.
Tümay V, Guner OS. The association of mucinous histology with clinicopathological characteristics and long-term oncological outcome in patients with colorectal cancer. Ann Ital Chir. 2020;91:639–48.
Yu F, Huang L, Shen F, Wu S, Chen J. Prognostic implications of mucinous histology in stage III colon cancer with the receipt of adjuvant chemotherapy. J Gastrointest Oncol. 2020;11(5):858–69.
Awad Abd-Allah E, Zahir GM, Abd-Alhamid AA, El-Beshbishi WN. Prognostic comparison between mucinous and non-mucinous rectal adenocarcinoma. Middle East J Cancer. 2021;12(1):106–16.
Li J, Yang L, Bai F, Cai Y, Zhang J, Wu Z, Fu Y, Deng Y. Clinicopathological, molecular features and prognosis of colorectal cancer with mucinous component. Future Oncol. 2021;17(11):1351–62.
Zhang J, Xie X, Wu Z, Hu H, Cai Y, Li J, Ling J, Ding M, Li W, Deng Y. Mucinous adenocarcinoma predicts poor response and prognosis in patients with locally advanced rectal cancer: a pooled analysis of individual participant data from 3 prospective studies. Clin Colorectal Cancer. 2021;20(4):e240–8.
Huang L, Luo S, Lai S, Liu Z, Hu H, Chen M, Kang L. Survival after curative resection for stage I colorectal mucinous adenocarcinoma. BMC Gastroenterol. 2022;22(1):192.
Qwaider YZ, Sell NM, Stafford CE, Boudreau C, Kunitake H, Goldstone RN, Ricciardi R, Bordeianou LG, Cauley CE, Berger DL. Prognosis of different histological types in patients with stage II and III Colon Cancer. J Gastrointest Surg. 2022;26(2):476–8.
Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med. 1998;17(24):2815–34.
Williamson PR, Smith CT, Hutton JL, Marson AG. Aggregate data meta-analysis with time-to-event outcomes. Stat Med. 2002;21(22):3337–51.
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16.
Chen JX, Tang XD, Xiang DB, Dong XL, Peng FY, Sun GY. TNM stages and prognostic features of colorectal mucinous adenocarcinomas: a meta analysis. Asian Pac J Cancer Prev. 2012;13(7):3427–30.
Hugen N, Brown G, Glynne-Jones R, de Wilt JH, Nagtegaal ID. Advances in the care of patients with mucinous colorectal cancer. Nat Rev Clin Oncol. 2016;13(6):361–9.
Stewart SL, Wike JM, Kato I, Lewis DR, Michaud F. A population-based study of colorectal cancer histology in the United States, 1998–2001. Cancer. 2006;107(5 Suppl):1128–41.
Registration and protocol
This study was not registered.
Funding
The authors have no funding to declare.
Author information
Authors and Affiliations
Contributions
YH and CJB come up with the study, then all author collaborated on the design of the project. WX, WHR collated, screened and analyzed the data together, and drafted the manuscript. HHQ, LK and YWG reviewed the content, revised the manuscript and approved the final manuscript. With the joint efforts of all authors, this study was completed and completed. The author(s) read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, X., Wang, H., He, H. et al. Clinicopathological and prognostic features of colorectal mucinous adenocarcinomas: a systematic review and meta-analysis. BMC Cancer 24, 1161 (2024). https://doi.org/10.1186/s12885-024-12905-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12905-3