Abstract
Background
Absolute lymphocyte count (ALC) is a predictive and prognostic factor for various tumor types, including breast cancer. Palbociclib is a CDK4/6 inhibitor widely used for the treatment of metastatic estrogen receptor (ER)-positive, HER2-negative breast cancer. However, predictive biomarkers of the efficacy of palbociclib remain unelucidated. We conducted a retrospective study to examine the predictive value of the baseline ALC in patients treated with palbociclib.
Methods
The medical records of patients with ER-positive, HER2-negative breast cancer treated with palbociclib plus hormonal therapy between December 2017 and December 2021 were analyzed retrospectively. The cutoff value of ALC was set at 1800 cells/μL at the initiation of palbociclib treatment. The clinical benefit rate (CBR) was defined as the rate of complete or partial response or stable disease for at least 6 months. Progression-free survival (PFS) rates were estimated using the Kaplan–Meier method and compared using the log-rank test. Univariate and multivariate analyses were performed using Cox proportional hazards regression.
Results
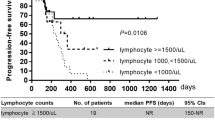
All of the 202 patients were women, with a median age of 59 years and a performance status (PS) of ≤ 2. The median numbers of lines of chemotherapy and endocrine therapy before palbociclib treatment were 0 (range, 0–9) and 1 (range, 0–7), respectively. Fifty-one patients had liver metastases. Forty-six patients tested negative for progesterone receptor (PgR) expression. The median follow-up time was 9.1 months. The CBR was significantly higher in the ALC-high group than in the ALC-low group (79% vs. 60%; P = 0.018). The median PFS was significantly longer in the ALC-high group than in the ALC-low group (26.8 months vs. 8.4 moths, respectively; P = 0.000013). ALC, age, PS, PgR status, prior chemotherapy, prior endocrine therapy, and liver metastasis were entered into the multivariate analysis. ALC was identified as an independent factor for PFS (P = 0.00085), along with liver metastasis (P = 0.0020), PS (P = 0.026), and prior endocrine therapy (P = 0.019).
Conclusion
ALC can serve as a predictor of palbociclib efficacy in patients with metastatic ER-positive, HER2-negative breast cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Breast cancer is the most common malignancy and leading cause of cancer-related mortality among women worldwide. In 2020, 2.26 million women were diagnosed with breast cancer and approximately 700,000 died from the disease [1]. Approximately 20–30% of patients with early breast cancer experience tumor recurrence in distant organs despite receiving curative surgery with adjuvant systemic therapy and radiotherapy, and this condition is still recognized as an incurable disease [2, 3]. Therefore, advancement in treatment strategies, such as the development of new drugs and biomarkers, is urgently required.
Peripheral absolute lymphocyte count (ALC) is recognized as a sensitive parameter reflecting the systemic immune status in various diseases, such as infections, trauma, respiratory disorders, autoimmune diseases, and malignant neoplasms [4, 5]. ALC has been widely evaluated as a predictive and prognostic biomarker of various malignant neoplasms, including breast cancer [6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22].
Palbociclib is a highly selective CDK4/6 inhibitor, which in combination with hormonal therapy, has been shown to be effective in treating metastatic estrogen receptor (ER)-positive, HER2-negative breast cancer, that is, metastatic luminal breast cancer (mLBC) [23, 24] and has now found widespread application in routine clinical practice. However, most patients eventually develop tumor progression, and some initially show resistance to palbociclib. Unfortunately, there is no practical or easy-to-use biomarker other than ER positivity for identifying patients who respond to palbociclib in clinical settings. This study aimed to examine the predictive value of ALC at baseline for patients with mLBC treated with palbociclib.
Methods
Patients
We retrospectively analyzed the data of registered patients with mLBC who were treated with palbociclib at the Cancer Institute Hospital of Japanese Foundation for Cancer Research (JFCR) between December 2017 and December 2021. This study was approved by the Institutional Review Board of the Cancer Institute Hospital of JFCR (2023-GB-051), which waived the requirement for informed consent.
Data collection
All patients underwent routine blood tests before starting palbociclib treatment in routine clinical practice, and complete blood counts, including ALC, were obtained using an automated hematology analyzer (Sysmex XN-9000; Sysmex Corporation, Kobe, Japan). Positivity for ER, progesterone receptor (PgR), and HER2 was defined according to the ASCO/CAP guidelines [25]. Briefly, the ER and PgR status was determined to be positive if the samples showed at least 1% positive invasive tumor nuclei on immunohistochemistry (IHC) staining. The HER2 status was defined as positive if the IHC assay score was 3 + and/or HER2-gene overexpression was confirmed by dual-color in situ hybridization. Baseline clinicopathological characteristics were extracted from the electronic medical records.
Statistical analysis
The cutoff value of ALC was determined according to receiver operating characteristic (ROC) curve analysis using the Youden index. Comparisons between the treatment groups were performed using the chi-squared and Fisher’s exact tests. The clinical benefit rate (CBR) was defined as the rate of complete (CR) or partial response (PR) or stable disease (SD) for at least 6 months, using RECIST ver1.1. Progression-free survival (PFS) was defined as the time from treatment initiation to the date of disease progression or the date of the last follow-up of patients who were alive at the last contact. PFS curves were generated using the Kaplan–Meier method and compared using the log-rank test. Univariate and multivariate Cox proportional hazard regression analyses were performed to examine the association between specific clinical variables and PFS. The multivariate analysis included all clinical variables that were considered clinically or statistically significant in the univariate analysis. For all tests, differences with P < 0.05 were considered statistically significant. All statistical analyses were performed using SPSS, version 27 (IBM Corp., Armonk, NY, USA).
Results
Patient characteristics and ALC status
This study included 202 consecutive patients with mLBC who were treated with palbociclib. The baseline clinicopathological characteristics of the patients, stratified by ALC status, are shown in Table 1. The cutoff value of ALC for PFS was set at 1800 cells/μL, per the ROC curve with the maximum Youden index (Fig. 1), based on which patients were divided into the ALC-high group (ALC ≥ 1800 cells/μL, n = 52) and ALC-low group (ALC < 1800 cells/μL, n = 150). The median follow-up duration was 9.1 months (range, 0.4–38.8 months).
All patients were women, with a median age of 59 years (range, 25–84 years) at the start of palbociclib treatment. Among them, 51 (25.2%) had liver metastases and 46 (22.8%) tested negative for PgR expression. The median numbers of lines of chemotherapy and endocrine therapy before palbociclib treatment were 0 (range, 0–9) and 1 (range, 0–7), respectively. All patients had a performance status (PS) of ≤ 2. The following hormonal therapies were used in conjunction with palbociclib: 110 (54.5%) patients received fulvestrant, 83 (41.1%) received an aromatase inhibitor (letrozole, n = 66; exemestane, n = 10; and anastrozole, n = 7), eight (4.0%) received tamoxifen, and 1 (0.5%) received medroxyprogesterone acetate. All premenopausal patients received a luteinizing hormone-releasing hormone agonist along with palbociclib and hormonal therapy. The ALC status was significantly associated with prior endocrine therapy and liver metastasis status (P = 0.037 and 0.026, respectively).
Predictive and prognostic value of ALC for the efficacy of palbociclib
The CBR was significantly higher in the ALC-high group (PR, 23%; long SD, 56%) than in the ALC-low group (PR, 10%; long SD, 50%) (79% vs. 60%, respectively; P = 0.018; Fig. 2). None of the patients achieved CR.
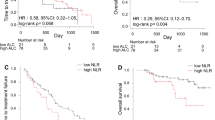
Overall, 202 patients experienced 136 disease progression events during the follow-up period. The median PFS was significantly longer in the ALC-high group than in the ALC-low group [26.8 months vs. 8.4 months; hazard ratio, 0.38; 95% confidence interval (CI), 0.46–0.72; P = 0.000013] (Fig. 3). To further examine the prognostic value of the ALC status, we performed multivariate analyses with the following clinically significant factors: age (≥ 60 vs. < 60 years), PS (0 vs. 1/2), PgR status (positive vs. negative), prior chemotherapy for metastatic disease (yes vs. no), prior endocrine therapy for metastatic disease (yes vs. no), liver metastasis (yes vs. no), and ALC. Multivariate analysis revealed that the ALC, as well as PS, previous endocrine therapy, and liver metastasis were independent prognostic factors for PFS (P = 0.00085, 0.026, 0.019, and 0.0020, respectively; Table 2).
Discussion
We found that the baseline ALC was a powerful and independent predictive biomarker of survival in patients treated with palbociclib. Although two randomized clinical trials have shown that the addition of palbociclib to endocrine therapy improves survival and increases the response rates of patients with mLBC [23, 24], there are no useful biomarkers other than ER expression for predicting the clinical efficacy of palbociclib. ALC is a noninvasive and easily available parameter that is evaluated in almost all patients at the start of palbociclib treatment in daily practice, making it a potential clinically useful predictive biomarker of the efficacy of palbociclib.
Recent studies have emphasized the importance of the tumor immune microenvironment in tumor progression [26, 27]. Systemic inflammatory markers such as ALC, neutrophil-to-lymphocyte ratio (NLR), lymphocyte-to-monocyte ratio, and platelet-to-lymphocyte ratio have been widely evaluated as prognostic and predictive biomarkers for various tumor types over the past few decades [28,29,30]. ALC has been shown to be associated with the prognosis of patients with breast cancer and other types of tumors [6, 11]. Furthermore, it has been found to predict drug efficacy in patients with various tumor types, including chemotherapy for breast, colorectal, and lung cancer [12,13,14,15,16]; trastuzumab for HER2-positive breast cancer [17]; immune checkpoint inhibitors (ICIs) for lung, head and neck cancer, and melanoma [18,19,20,21]; and immuno-radiotherapy for solid tumors [22]. These findings suggest that lymphocytes play an important role in eliciting the antitumor effects of various drugs. In light of the aforementioned observations, our study’s findings reinforce the role of lymphocytes in palbociclib treatment. Emile et al. also reported similar findings regarding the significant association between the baseline ALC and palbociclib efficacy [31]. However, the patient population analyzed in that study had undergone extensive prior treatments, with a median of four previous lines of therapy for metastases. In contrast, 49% of patients in our study received palbociclib as a first- or second-line treatment, consistent with the protocols of randomized trials [23, 24]. Therefore, our results may more accurately reflect the importance of ALC in current real-world clinical practice. Kanaoka et al. and Nakamoto et al. conducted similar studies evaluating the association of the baseline ALC with CDK4/6 inhibitors, including palbociclib and abemaciclib, but did not find any such association in the palbociclib cohort, possibly due to a smaller sample size and disparate ALC cutoff values [32, 33]. While both palbociclib and abemaciclib are selective CDK4/6 inhibitors, they exhibit different kinase activities and effects on survival [34, 35], suggesting that the role of lymphocytes in treatment with palbociclib may differ from that with abemaciclib.
We also evaluated the NLR in our study since it is another widely evaluated systemic inflammatory marker. However, the AUC of NLR was significantly lower than that of ALC (0.544 vs. 0.628, P = 0.024), indicating the latter’s superiority as a predictive indicator. This is not surprising, as neutropenia is one of the most common side effects of palbociclib, suggesting that neutrophils have little effect on its efficacy. Kim et al. also found that the baseline NLR did not exert an effect on the survival of patients treated with palbociclib [36].
Several studies have shown that CDK4/6 inhibitors alter the tumor immune microenvironment, and that ICI and CDK4/6 inhibitors have synergistic effects in mouse models [37,38,39]. Combined immunotherapy with CDK4/6 inhibitors and ICIs for the treatment of mLBC is currently under development [40, 41]. Yuan et al. conducted a phase 1/2 study and reported that the combination of palbociclib, pembrolizumab, and letrozole yielded a CR rate of 31% in patients with mLBC [41]. Further investigations on the development of combination immunotherapy with CDK 4/6 inhibitor are needed.
We found that patients with liver metastasis had a significantly lower ALC than those without, and liver metastasis was significantly associated with shorter PFS in the univariate and multivariate analyses. Yu et al. showed that liver metastases could siphon activated CD8 + T cells from systemic circulation and induce apoptosis following their interaction with monocyte-derived macrophages in mouse models [42]. They also found that patients with liver metastases had a lower peripheral ALC and diminished tumoral T cell diversity and function, suggesting that liver metastases suppress anti-tumor immunity in the clinical setting. Several recent meta-analyses have shown that the efficacy of ICI treatment is attenuated in patients with liver metastases [43,44,45]. Based on these findings, if CDK4/6 inhibitors exert their function in part through anti-tumor immunity, their efficacy may be attenuated in patients with liver metastases. Despite the potential influence of liver metastases on ALC and their generally poor prognostic implications, ALC retained significance as an independent factor in multivariate analyses, as did liver metastasis.
This study has several limitations. First, this was a retrospective, single-institutional, small-scale study, and these aspects may have resulted in unintentional biases. Second, the cutoff of ALC was not consistent across previous studies, whose results were unfortunately inconsistent [31,32,33]. In other words, a universally accepted cutoff of ALC has yet to be established. To further elucidate the significance of ALC in our cohort, we adopted a best cutoff of 1800 cells/µL based on the ROC analysis (Fig. 1). Third, the mechanism underlying our results is speculative. Lymphocytes comprise various cell types, including T cells, B cells, and NK cells, which interact with each other and with other leukocytes, such as neutrophils and monocytes. Dyikanov et al. conducted comprehensive peripheral blood immunoprofiling and demonstrated an association between immune subtypes and the efficacy of neoadjuvant chemotherapy in patients with breast cancer [46]. Similar further studies are warranted to elucidate the precise mechanism of palbociclib in the context of systemic immune status. Fourth, we did not analyze overall survival (OS), which is recognized as an important clinical endpoint, along with PFS. However, discrepancies between OS and PFS outcomes can complicate the assessment of a new treatment's efficacy. The duration of post-progression survival is influenced by various factors, including crossover treatments and subsequent administration of efficacious drugs [47]. Consequently, most recent randomized clinical trials for metastatic breast cancer tend to use PFS as the primary endpoint. Moreover, the objective of this study was to evaluate the predictive value of ALC as a biomarker, and not its prognostic value. From this perspective, we selected PFS and tumor response as endpoints, which facilitated a more direct assessment of the association between ALC and palbociclib efficacy, and we opine that the value of our study is not compromised by the lack of OS data. Finally, the patients in this study received various hormonal drugs in combination with palbociclib and the treatment lines varied. However, ALC was identified as an independent prognostic factor in the multivariate analysis, in addition to the prior endocrine therapy status.
Conclusions
Our study demonstrated that the baseline ALC is a strong prognostic indicator of the efficacy of palbociclib against mLBC. Further studies are needed to validate our findings in other cohorts and to fully elucidate the mechanism by which palbociclib alters the tumor immune microenvironment in the clinical setting.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ALC:
-
Absolute lymphocyte count
- CBR:
-
Clinical benefit rate
- ER:
-
Estrogen receptor
- ICI:
-
Immune checkpoint inhibitor
- mLBC:
-
Metastatic luminal breast cancer
- NLR:
-
Neutrophil-to–lymphocyte ratio
- PgR:
-
Progesterone receptor
- PFS:
-
Progression-free survival
- ROC:
-
Receiver operating characteristic
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–49.
Cardoso F, Paluch-Shimon S, Senkus E, Curigliano G, Aapro MS, André F, Barrios CH, Bergh J, Bhattacharyya GS, Biganzoli L, et al. 5th ESO-ESMO international consensus guidelines for advanced breast cancer (ABC 5). Ann Oncol. 2020;31(12):1623–49.
Harbeck N, Penault-Llorca F, Cortes J, Gnant M, Houssami N, Poortmans P, Ruddy K, Tsang J, Cardoso F. Breast cancer Nat Rev Dis Primers. 2019;5(1):66.
Andreu-Ballester JC, Pons-Castillo A, Gonzalez-Sanchez A, Llombart-Cussac A, Cano MJ, Cuellar C. Lymphopenia in hospitalized patients and its relationship with severity of illness and mortality. PLoS ONE. 2021;16(8): e0256205.
Zidar DA, Al-Kindi SG, Liu Y, Krieger NI, Perzynski AT, Osnard M, Nmai C, Anthony DD, Lederman MM, Freeman ML, et al. Association of Lymphopenia With Risk of Mortality Among Adults in the US General Population. JAMA Netw Open. 2019;2(12): e1916526.
Ray-Coquard I, Cropet C, Van Glabbeke M, Sebban C, Le Cesne A, Judson I, Tredan O, Verweij J, Biron P, Labidi I, et al. Lymphopenia as a prognostic factor for overall survival in advanced carcinomas, sarcomas, and lymphomas. Cancer Res. 2009;69(13):5383–91.
Cézé N, Thibault G, Goujon G, Viguier J, Watier H, Dorval E, Lecomte T. Pre-treatment lymphopenia as a prognostic biomarker in colorectal cancer patients receiving chemotherapy. Cancer Chemother Pharmacol. 2011;68(5):1305–13.
Milne K, Alexander C, Webb JR, Sun W, Dillon K, Kalloger SE, Gilks CB, Clarke B, Köbel M, Nelson BH. Absolute lymphocyte count is associated with survival in ovarian cancer independent of tumor-infiltrating lymphocytes. J Transl Med. 2012;10:33.
Lee YJ, Chung YS, Lee JY, Nam EJ, Kim SW, Kim S, Kim YT. Pretreatment lymphocytopenia is an adverse prognostic biomarker in advanced-stage ovarian cancer. Cancer Med. 2019;8(2):564–71.
Ménétrier-Caux C, Ray-Coquard I, Blay JY, Caux C. Lymphopenia in Cancer Patients and its Effects on Response to Immunotherapy: an opportunity for combination with Cytokines? J Immunother Cancer. 2019;7(1):85.
Lee KH, Kim EY, Yun JS, Park YL, Do SI, Chae SW, Park CH. The prognostic and predictive value of tumor-infiltrating lymphocytes and hematologic parameters in patients with breast cancer. BMC Cancer. 2018;18(1):938.
Liang L, Zhu J, Jia H, Huang L, Li D, Li Q, Li X. Predictive value of pretreatment lymphocyte count in stage II colorectal cancer and in high-risk patients treated with adjuvant chemotherapy. Oncotarget. 2016;7(1):1014–28.
Vicente Conesa MA, Garcia-Martinez E, Gonzalez Billalabeitia E, Chaves Benito A, Garcia Garcia T, Vicente Garcia V. Ayala de la Peña F: Predictive value of peripheral blood lymphocyte count in breast cancer patients treated with primary chemotherapy. Breast. 2012;21(4):468–74.
Lissoni P, Brivio F, Fumagalli L, Messina G, Ghezzi V, Frontini L, Giani L, Vaghi M, Ardizzoia A, Gardani GS. Efficacy of cancer chemotherapy in relation to the pretreatment number of lymphocytes in patients with metastatic solid tumors. Int J Biol Markers. 2004;19(2):135–40.
Araki K, Ito Y, Fukada I, Kobayashi K, Miyagawa Y, Imamura M, Kira A, Takatsuka Y, Egawa C, Suwa H, et al. Predictive impact of absolute lymphocyte counts for progression-free survival in human epidermal growth factor receptor 2-positive advanced breast cancer treated with pertuzumab and trastuzumab plus eribulin or nab-paclitaxel. BMC Cancer. 2018;18(1):982.
Miyoshi Y, Yoshimura Y, Saito K, Muramoto K, Sugawara M, Alexis K, Nomoto K, Nakamura S, Saeki T, Watanabe J, et al. High absolute lymphocyte counts are associated with longer overall survival in patients with metastatic breast cancer treated with eribulin-but not with treatment of physician’s choice-in the EMBRACE study. Breast Cancer. 2020;27(4):706–15.
Hong J, Chen X, Gao W, Zhu S, Wu J, Huang O, He J, Zhu L, Chen W, Li Y, et al. A high absolute lymphocyte count predicts a poor prognosis in HER-2- positive breast cancer patients treated with trastuzumab. Cancer Manag Res. 2019;11:3371–9.
Soyano AE, Dholaria B, Marin-Acevedo JA, Diehl N, Hodge D, Luo Y, Manochakian R, Chumsri S, Adjei A, Knutson KL, et al. Peripheral blood biomarkers correlate with outcomes in advanced non-small cell lung Cancer patients treated with anti-PD-1 antibodies. J Immunother Cancer. 2018;6(1):129.
Huemer F, Lang D, Westphal T, Gampenrieder SP, Hutarew G, Weiss L, et al. Baseline absolute lymphocyte count and ECOG performance score are associated with survival in advanced non-small cell lung cancer undergoing PD-1/PD-L1 blockade. J Clin Med. 2019;8(7):1014.
Ho WJ, Yarchoan M, Hopkins A, Mehra R, Grossman S, Kang H. Association between pretreatment lymphocyte count and response to PD1 inhibitors in head and neck squamous cell carcinomas. J Immunother Cancer. 2018;6(1):84.
Martens A, Wistuba-Hamprecht K, Geukes Foppen M, Yuan J, Postow MA, Wong P, Romano E, Khammari A, Dreno B, Capone M, et al. Baseline Peripheral Blood Biomarkers Associated with Clinical Outcome of Advanced Melanoma Patients Treated with Ipilimumab. Clin Cancer Res. 2016;22(12):2908–18.
Chen D, Verma V, Patel RR, Barsoumian HB, Cortez MA, Welsh JW. Absolute Lymphocyte Count Predicts Abscopal Responses and Outcomes in Patients Receiving Combined Immunotherapy and Radiation Therapy: Analysis of 3 Phase 1/2 Trials. Int J Radiat Oncol Biol Phys. 2020;108(1):196–203.
Finn RS, Martin M, Rugo HS, Jones S, Im SA, Gelmon K, Harbeck N, Lipatov ON, Walshe JM, Moulder S, et al. Palbociclib and Letrozole in Advanced Breast Cancer. N Engl J Med. 2016;375(20):1925–36.
Turner NC, Ro J, André F, Loi S, Verma S, Iwata H, Harbeck N, Loibl S, Huang Bartlett C, Zhang K, et al. Palbociclib in Hormone-Receptor-Positive Advanced Breast Cancer. N Engl J Med. 2015;373(3):209–19.
Wolff AC, Hammond MEH, Allison KH, Harvey BE, Mangu PB, Bartlett JMS, Bilous M, Ellis IO, Fitzgibbons P, Hanna W, et al. Human Epidermal Growth Factor Receptor 2 Testing in Breast Cancer: American Society of Clinical Oncology/College of American Pathologists Clinical Practice Guideline Focused Update. J Clin Oncol. 2018;36(20):2105–22.
Binnewies M, Roberts EW, Kersten K, Chan V, Fearon DF, Merad M, Coussens LM, Gabrilovich DI, Ostrand-Rosenberg S, Hedrick CC, et al. Understanding the tumor immune microenvironment (TIME) for effective therapy. Nat Med. 2018;24(5):541–50.
Teh JLF, Aplin AE. Arrested Developments: CDK4/6 Inhibitor Resistance and Alterations in the Tumor Immune Microenvironment. Clin Cancer Res. 2019;25(3):921–7.
Savioli F, Morrow ES, Dolan RD, Romics L, Lannigan A, Edwards J, McMillan DC. Prognostic role of preoperative circulating systemic inflammatory response markers in primary breast cancer: meta-analysis. Br J Surg. 2022;109(12):1206–15.
Cho U, Park HS, Im SY, Yoo CY, Jung JH, Suh YJ, Choi HJ. Prognostic value of systemic inflammatory markers and development of a nomogram in breast cancer. PLoS ONE. 2018;13(7): e0200936.
Batalha S, Ferreira S, Brito C. The peripheral immune landscape of breast cancer: clinical findings and in vitro models for biomarker discovery. Cancers (Basel). 2021;13(6):1305.
Emile G, Penager S, Levy C, Johnson A, Allouache D, Lequesne J, Hrab I, Segura C, Morel A, Gunzer K, et al. Baseline lymphopenia as prognostic factor in patients with metastatic breast cancer treated with palbociclib. Oncol Lett. 2022;23(1):25.
Kanaoka H, Nagahashi M, Atake Y, Hattori A, Bun A, Fukui R, Ozawa H, Fujimoto Y, Higuchi T, Natori K, et al. Absolute Lymphocyte Count Is an Independent Prognostic Factor for ER-positive HER2-negative Advanced Breast Cancer Patients Treated With CDK4/6 Inhibitors. Anticancer Res. 2022;42(10):4867–78.
Nakamoto S, Shien T, Iwamoto T, Kubo S, Yamamoto M, Yamashita T, Kuwahara C, Ikeda M. Absolute lymphocyte count and neutrophil-to-lymphocyte ratio as predictors of CDK 4/6 inhibitor efficacy in advanced breast cancer. Sci Rep. 2024;14(1):9869.
Hafner M, Mills CE, Subramanian K, Chen C, Chung M, Boswell SA, Everley RA, Liu C, Walmsley CS, Juric D, et al. Multiomics Profiling Establishes the Polypharmacology of FDA-Approved CDK4/6 Inhibitors and the Potential for Differential Clinical Activity. Cell Chem Biol. 2019;26(8):1067–1080.e1068.
Johnston S, Emde A, Barrios C, Srock S, Neven P, Martin M, et al. Cyclin-dependent kinase 4 and 6 (CDK4/6) inhibitors: existing and emerging differences. JNCI Cancer Spectr. 2023;7(4):pkad045.
Kim CG, Kim MH, Kim JH, Kim SG, Kim GM, Kim TY, Ryu WJ, Kim JY, Park HS, Park S, et al. On-treatment derived neutrophil-to-lymphocyte ratio and survival with palbociclib and endocrine treatment: analysis of a multicenter retrospective cohort and the PALOMA-2/3 study with immune correlates. Breast Cancer Res. 2023;25(1):4.
Zhang J, Bu X, Wang H, Zhu Y, Geng Y, Nihira NT, Tan Y, Ci Y, Wu F, Dai X, et al. Cyclin D-CDK4 kinase destabilizes PD-L1 via cullin 3-SPOP to control cancer immune surveillance. Nature. 2018;553(7686):91–5.
Goel S, DeCristo MJ, Watt AC, BrinJones H, Sceneay J, Li BB, Khan N, Ubellacker JM, Xie S, Metzger-Filho O, et al. CDK4/6 inhibition triggers anti-tumour immunity. Nature. 2017;548(7668):471–5.
Schaer DA, Beckmann RP, Dempsey JA, Huber L, Forest A, Amaladas N, Li Y, Wang YC, Rasmussen ER, Chin D, et al. The CDK4/6 Inhibitor Abemaciclib Induces a T Cell Inflamed Tumor Microenvironment and Enhances the Efficacy of PD-L1 Checkpoint Blockade. Cell Rep. 2018;22(11):2978–94.
Rugo HS, Kabos P, Beck JT, Jerusalem G, Wildiers H, Sevillano E, Paz-Ares L, Chisamore MJ, Chapman SC, Hossain AM, et al. Abemaciclib in combination with pembrolizumab for HR+, HER2- metastatic breast cancer: Phase 1b study. NPJ Breast Cancer. 2022;8(1):118.
Yuan Y, Lee JS, Yost SE, Frankel PH, Ruel C, Egelston CA, Guo W, Padam S, Tang A, Martinez N, et al. Phase I/II trial of palbociclib, pembrolizumab and letrozole in patients with hormone receptor-positive metastatic breast cancer. Eur J Cancer. 2021;154:11–20.
Yu J, Green MD, Li S, Sun Y, Journey SN, Choi JE, Rizvi SM, Qin A, Waninger JJ, Lang X, et al. Liver metastasis restrains immunotherapy efficacy via macrophage-mediated T cell elimination. Nat Med. 2021;27(1):152–64.
Tian BW, Han CL, Wang HC, Yan LJ, Ding ZN, Liu H, Mao XC, Tian JC, Xue JS, Yang LS, et al. Effect of liver metastasis on the efficacy of immune checkpoint inhibitors in cancer patients: a systemic review and meta-analysis. Clin Exp Metastasis. 2023;40(4):255–87.
Xia H, Zhang W, Zhang Y, Shang X, Liu Y, Wang X. Liver metastases and the efficacy of immune checkpoint inhibitors in advanced lung cancer: A systematic review and meta-analysis. Front Oncol. 2022;12: 978069.
Yin WJ, Ma SC, Dong ZY, Xu M, Mao W. Efficacy and Treatment Strategies in Advanced Cancers with Liver Metastasis Receiving Atezolizumab Therapy. Cancer Manag Res. 2021;13:4541–51.
Dyikanov D, Zaitsev A, Vasileva T, Wang I, Sokolov AA, Bolshakov ES, Frank A, Turova P, Golubeva O, Gantseva A, et al. Comprehensive peripheral blood immunoprofiling reveals five immunotypes with immunotherapy response characteristics in patients with cancer. Cancer Cell. 2024;42(5):759–779.e712.
Seidman AD, Maues J, Tomlin T, Bhatnagar V, Beaver JA. The Evolution of Clinical Trials in Metastatic Breast Cancer: Design Features and Endpoints That Matter. Am Soc Clin Oncol Educ Book. 2020;40:1–11.
Acknowledgements
We would like to thank Editage (www.editage.jp) for English language editing.
Funding
This work was supported by JSPS KAKENHI (Grant Number 21K08678).
Author information
Authors and Affiliations
Contributions
TK conceived and designed the study. TK, MN, MH, RK, SK, YA, YO, IF, FH, TT, TU collected the data. TK verified and analyzed the data. TK wrote the manuscript, and TU and MN edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol conformed to the ethical guidelines of the Declaration of Helsinki. This study was approved by the Institutional Review Board of the Cancer Institute Hospital of JFCR (2023-GB-051), which waived the requirement of informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kobayashi, T., Nishimura, M., Hosonaga, M. et al. Absolute lymphocyte count predicts efficacy of palbociclib in patients with metastatic luminal breast cancer. BMC Cancer 24, 1156 (2024). https://doi.org/10.1186/s12885-024-12941-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12941-z