Abstract
Background
Limited research has analyzed the association between diastolic blood pressure (DBP) and survival after pediatric cardiopulmonary resuscitation (CPR). This study aimed to explore the association between post-resuscitation diastolic blood pressure and survival in pediatric patients who underwent CPR.
Method
This retrospective single-center study included pediatric patients admitted to the pediatric intensive care unit of Asan Medical Center between January 2016 to November 2022. Patients undergoing extracorporeal CPR and those with unavailable data were excluded. The primary endpoint was survival to ICU discharge.
Results
A total of 106 patients were included, with 67 (63.2%) achieving survival to ICU discharge. Multivariate logistic regression analysis identified DBP within 1 h after ROSC as the sole significant variable (p = 0.002, aOR, 1.043; 95% CI, 1.016–1.070). Additionally, DBP within 1 h demonstrated an area under the ROC curve of 0.7 (0.592–0.809) for survival to ICU discharge, along with mean blood pressure within the same timeframe.
Conclusion
Our study highlights the importance of DBP within 1-hour post-ROSC as a significant prognostic factor for survival to ICU discharge. However, further validation through further prospective large-scale studies is warranted to confirm the appropriate post-resuscitation DBP of pediatric patients.
Similar content being viewed by others
Introduction
More than 300,000 pediatric patients experience out-of-hospital cardiac arrest (OHCA) or in-hospital cardiac arrest (IHCA) in the United States alone [1, 2]. However, despite improvements in post-cardiopulmonary resuscitation (CPR) over recent decades, there is a persistent high morbidity, accompanied by a mortality rate exceeding 65% [2, 3].
The lower limit of cerebral autoregulation should be adjusted higher for post-resuscitation patients. Theoretically, higher blood pressure can achieve better cerebral blood perfusion, which can lead to improved neurologic outcomes [4, 5]. A previous study reported that analyses of systolic blood pressure (SBP) and mean blood pressure (MBP) after CPR contributed to improving neurological outcomes or survival by high levels of SBP and MBP [6,7,8,9,10,11]. Some recent studies in adults have emphasized diastolic blood pressure (DBP) for better outcomes, with similar findings also observed in children [12,13,14]. In a recent prospective observational multicenter study for pediatric patients with IHCA, maintaining DBP 25 mmHg or higher in infants and 30 mmHg or higher in children over the age of 1 during the first 10 min of CPR was associated with survival to hospital discharge and favorable neurologic outcomes [12].
However, most published studies have measured DBP during CPR using an invasive arterial catheter. Moreover, most of the studies that analyzed DBP in post-CPR were conducted on adults and the number of studies was small.
We therefore aimed to investigate the relationship between post-resuscitation DBP and mortality in patients who underwent CPR. We hypothesized that a higher DBP after CPR would lead to lower mortality.
Methods
Study population
This was a single-center retrospective observational study. The study population was extracted from the medical records of all pediatric patients who experienced resuscitated cardiac arrest and were admitted to the 14-bed multidisciplinary pediatric intensive care unit (PICU) at Asan Medical Center, a tertiary academic referral hospital in Seoul, south Korea. The Institutional Review Board of the University of Ulsan College of Medicine reviewed and approved this study (No.2024-0033) and waived the need for parental consent given the retrospective nature of the study. We had access to information that could identify individual participants by electrical medical records between 8. Jan. 2024 and 25. Jan. 2024.
Both pediatric survivors of OHCA and IHCA from January 2016 to November 2022 were included in the study. These patients were managed in accordance with the current guidelines for pediatric basic and advanced life support [15]. Patients with insufficient data or who received ECMO support during resuscitation were excluded given the potential influence of extracorporeal circulation on hemodynamic monitoring.
Data collection
The demographics, underlying diseases, etiology of cardiac arrest, characteristics of cardiac arrest (bystander CPR, initial rhythm, duration of CPR, pharmacologic intervention), baseline Pediatric Cerebral Performance Category (PCPC) score, and baseline vasoactive inotropic score (VIS) of all patients were obtained. After the return of spontaneous circulation (ROSC), initial and worst blood pressure (systolic blood pressure, diastolic blood pressure, mean blood pressure) within 1 h were analyzed. The worst VIS within 24 h, ICU length of stay, use of CRRT or ventilator, and neurologic outcome calculated through PCPC score at ICU discharge were also assessed. PCPC 1 was defined as alert mentality with good cerebral performance, PCPC 2 as conscious, but with the possibility of mild neurologic deficit; PCPC 3 as conscious with cerebral disability; PCPC 4 as conscious with impaired brain function; PCPC 5 as coma or vegetative state; PCPC 6 as brain death or dead. Patients who were comatose after ROSC were managed with therapeutic hypothermia, performed with Blanketroll III (Genteherm Medical, Cincinnati, OH, USA) with the target temperature (34–35℃) maintained for 48 h. Patients with arrhythmia or lactic acidosis with poor circulation during therapeutic hypothermia were managed with a target temperature of 36℃. Hemodynamic status was recorded by non-invasive blood pressure (NIBP) monitoring in the emergency room (ER) or general ward. Mean blood pressure (MBP) was estimated using the following formula: MBP = DBP + 1/3 (SBP–DBP). When measuring blood pressure, it can be elevated if the child is crying or restless, so we measured blood pressure after the child had calmed down, usually during feeding or sleep. The blood pressure cuff size was chosen according to the following criteria: the cuff length was 40% of the distance from the elbow to the shoulder, and the width was approximately 40% of the arm circumference, measured at the midpoint between the olecranon and acromion. If the blood pressure reading was outside the normal range for the child’s age, measurements were repeated up to three times consecutively, and the final reading was recorded.
Initial blood pressure was defined as NIBP measured for the first time after ROSC. Then, we follow the blood pressure every 5 min and recorded the worst value within 1 h after recovery. The primary endpoint of this study was survival to ICU discharge.
Statistical analysis
The categorical variables or outcomes of enrolled patients were summarized using frequencies and percentages and were analyzed using the chi-squared test or two-tailed Fisher’s exact test, as appropriate. Continuous data were expressed as mean ± standard deviation (SD) or median with interquartile range (IQR) and compared using a two-tailed Student’s t-test. Measured blood pressure after ROSC with p-values of < 0.05 was included in a stepwise logistic regression for predicting independent variables by reporting an odds ratio (OR) with 95% confidence intervals (CI). To evaluate the discriminative ability of DBP, we analyzed initial blood pressure and the worst blood pressure within 1 h after ROSC using receiver operating characteristic (ROC) curves with the corresponding area under the curve (AUC) and related sensitivity and specificity. All p-values of < 0.05 were considered to be statistically significant. All data were analyzed using IBM SPSS Statistics for Windows, version 21.0 (IBM Corp, Armonk, NY, USA).
Results
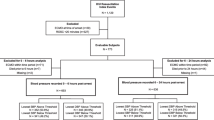
A total of 238 pediatric survivors of CPR, of which 106 were finally enrolled. Among the screened patients, patients not achieve ROSC (n = 76), patients who underwent extracorporeal CPR (n = 18), under 1 month or above 18 years (n = 15), or had insufficient data (n = 23) were excluded. Finally, a total of 67 patients (63.2%) were included in the survival of ICU discharge group and 39 (36.8%) were included in the non-survival of ICU discharge group (Fig. 1.)
The demographic and clinical characteristics are summarized in Table 1. No differences in age, sex, body weight, or ICU length of stay were noted between the two groups. The most common underlying disease in both groups was cardiac disease. Respiratory decompensation was the most common cause of cardiac arrest across the two groups; however, a greater proportion of cardiogenic and hypovolemic shock was observed in non-survivors compared to survivors. With the exception of pharmacological intervention, there were no statistically significant differences observed in the variables related to cardiac arrest between the two groups. After ROSC, all blood pressure, including the worst value within 1 h was significantly higher in the survival group than in the non-survival group.
Vasoactive inotropic drug score within 24 h and duration of using the vasoactive drug were higher in the non-survival group. However, the duration of the ventilator did not significantly differ (Table 2).
Based on the t-test analysis in Table 1, the univariate logistic regression analysis also revealed statistically significant differences across all blood pressure values. However, the results of the multivariate logistic regression analysis revealed that DBP within the first hour was a significant variable (p = 0.002, aOR, 1.043; 95% CI, 1.016–1.070) (Table 3).
Additionally, DBP within the first hour demonstrated an area under the ROC curve (AUROC) of 0.7 (0.592–0.809) for predicting survival to ICU discharge (Fig. 2). The cut point of the area under the curve and related sensitivity and specificity for SBP, DBP, and DBP within the first hour were 93, 60, and 48, respectively.
Discussion
In this study, during the initial post-ROSC hour, our findings indicate that diastolic blood pressure had the most influence on survival to ICU discharge following resuscitation. Despite MBP exhibiting a higher AUC value than DBP, with marginal differences in significance, our multivariate logistic regression analysis established DBP as the independent prognostic factor.
Numerous studies have explored the hemodynamic significance of DBP as a predictor of survival and favorable neurologic outcomes during CPR [16,17,18]. Additionally, many studies continue to identify various factors with hemodynamically significant implications in post-cardiac arrest. Our study has statistically demonstrated that within the first hour post-resuscitation, DBP can serve as an independent prognostic factor for survival to ICU discharge, in line with the findings of a recent adult study [19, 20]. With a greater influence than other blood pressure variables, DBP is a strong prognostic factor owing to its effects on peripheral vascular tone and coronary perfusion, whereas SBP has only a sensitive effect on cardiac contractility and volume change [21,22,23]. Relying solely on SBP targets in post-resuscitation management may effectively address circulatory shock, but there is an incurred risk of ischemic injury of the heart or end-organ damage, ultimately increasing morbidity and mortality. Maintaining an adequate DBP is crucial to reduce the mortality risk associated with post-cardiac arrest syndrome, which induces systemic ischemia and reperfusion injury by decreasing peripheral vascular tone [24,25,26]. Accordingly, our study revealed an association between DBP during the early post-resuscitation stage and the risk of mortality at ICU discharge.
In addition to DBP, MBP demonstrated a positive correlation with survival to ICU discharge in our study (Fig. 2). Previous studies have suggested that maintaining higher MBP levels is associated with improved outcomes. This observation can be ascribed to the pivotal role of DBP in the calculation of MBP compared with SBP. Consequently, given that raising and sustaining DBP ultimately increases MBP, we posit that DBP may be considered the more essential factor.
Our study can be distinguished from previous studies in several key ways. First, our study analyzed the lowest value within the first hour after ROSC, whereas previous studies evaluated the first NIBP or a mean value within 6 h post-ROSC. Given the importance of avoiding interference from inotropic agent effects and TTM in maintaining blood pressure during the first day after cardiac arrest, we contend that our study helped minimize the error range through consideration of the NIBP measurement.
Another differentiating factor is that the mean value of the worst DBP value within 1 h of enrollment exceeded 45 mmHg for most patients. This implies that, despite setting the cut-off value higher than the target DBP, our statistical analysis confirmed the significant influence of DBP on survival to ICU discharge. This correlation aligns with earlier studies, wherein setting the cut-off value of the lowest DBP as the 50th percentile for age-predicted survival and favorable neurologic outcomes for pediatric post-cardiac arrest patients. Post-ROSC diastolic hypertension was also associated with survival to discharge [20, 27].
Studies evaluating the efficacy of DBP during CPR have traditionally utilized invasive arterial catheters to monitor blood pressure. While invasive arterial catheters offer superior accuracy compared with NIBP measurements, a previous propensity-matched cohort study confirmed no association between the use of arterial catheters in critically ill patients with mechanical ventilators and hospital mortality [28]. In the pediatric population, particularly in infants, the technical challenges associated with inserting arterial catheters during CPR, coupled with the difficulties of performing this procedure in children with comprised vascular perfusion even after ROSC, pose substantial hurdles. Therefore, NIBP a more commonly employed clinical tool in pediatric medicine, can serve as a practical device for monitoring blood pressure instead of an arterial catheter. Despite a slightly lower accuracy, our study holds clinical significance in drawing conclusions that are more widely applicable.
Another distinguishing factor is that the primary outcome was survival to ICU discharge rather than survival to hospital discharge. Given the relatively extended average ICU stay of over 30 days, which is notably longer compared with other studies, we designated survival to ICU discharge as the primary outcome.
This study has several potential limitations. First, this study was a retrospective single-center study that included a relatively small number of pediatric patients who performed CPR compared with studies for adults. Due to the limited patient pool, and despite age-related variations in normal ranges, only simple values were compared without detailed subgroup analyses. While our study statistically established the influence of DBP on post-cardiac arrest mortality, large-scale prospective studies specifically focusing on pediatric patients are warranted to accurately determine the effectiveness of DBP. Second, certain prognostic factors, including inflammatory biomarkers reflecting neurological prognosis, lactate levels, and initial blood gas analysis, electroencephalographic findings, and echocardiography findings were not considered in the assessment of mortality. Third, a previous study included only pediatric patients who underwent IHCA, whereas this study included both IHCA and OHCA patients. Despite the relatively small proportion of OHCA cases (Table 1), the statistical insignificance between the two groups should be acknowledged.
In conclusion, within the initial hour post-ROSC, DBP emerged as the blood pressure parameter exerting the most influence on survival to ICU discharge after resuscitation. Further prospective and large-scale studies are warranted to validate the optimal DBP for post-resuscitation for pediatric patients.
Conclusion
This study identified diastolic blood pressure (DBP) within one-hour post-ROSC as the most significant hemodynamic determinant of survival to intensive care unit discharge among resuscitated pediatric patients. Multivariate analysis pinpointed DBP as the sole independent predictor, highlighting its prognostic relevance. The area under the receiver operating characteristic curve further substantiated DBP’s discriminative ability, comparable to mean arterial pressure.
These findings underscore the pivotal role of DBP in mitigating mortality risk associated with post-cardiac arrest syndrome. By modulating peripheral vascular resistance and coronary perfusion, optimizing DBP may attenuate systemic ischemia-reperfusion injury more effectively than targeting systolic pressures alone.
Nonetheless, prospective large-scale investigations are warranted to establish evidence based DBP thresholds specific to pediatric post resuscitation care. Such efforts could refine hemodynamic management protocols, ultimately translating to improved outcomes in this vulnerable population.
Data availability
The dataset analyzed during this study are available from the corresponding author on reasonable request.
Abbreviations
- CPR:
-
Cardiopulmonary Resuscitation
- CRRT:
-
Continuous Renal Replacement Therapy
- DBP:
-
Diastolic Blood Pressure
- ECMO:
-
Extracorporeal Membrane Oxygenation
- ICU:
-
Intensive Care Unit
- IHCA:
-
In-hospital Cardiac Arrest
- MBP:
-
Mean Blood Pressure
- NIBP:
-
Non-invasive Blood Pressure
- OHCA:
-
Out-of-hospital Cardiac Arrest
- PCPC:
-
Pediatric Cerebral Performance Category
- ROSC:
-
Return of Spontaneous Circulation
- SBP:
-
Systolic Blood Pressure
- TTM:
-
Target Temperature Management
- VIS:
-
Vasoactive Inotropic Score
References
McNally B, Robb R, Mehta M, Vellano K, Valderrama A, Yoon P, et al. Centers for disease control and prevention. Out-of-hospital cardiac arrest surveillance—cardiac arrest Registry to enhance survival (CARES), United States, October 1, 2005–December 31, 2010. MMWR Surveill Summ. 2011;60(8):1–19.
Morgan RW, Kirschen MP, Kilbaugh TJ, Sutton RM, Topjian AA. Pediatric in-hospital cardiac arrest and cardiopulmonary resuscitation in the United States: a review. JAMA Pediatr. 2021;175(3):293–302.
Nolan JP, Neumar RW, Adrie C, Aibiki M, Berg RA, Böttiger BW, the American Heart Association Emergency cardiovascular Care Committee. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication: a scientific statement from the international liaison Committee on Resuscitation. Resuscitation. 2008;79(3):350–79. the Council on Cardiovascular Surgery and Anesthesia; the Council on cardiopulmonary, Perioperative, and Critical Care; the Council on clinical cardiology; the Council on Stroke.
Skåre C, Karlsen H, Strand-Amundsen RJ, Eriksen M, Skulberg VM, Sunde K, et al. Cerebral perfusion and metabolism with mean arterial pressure 90 vs. 60 mmHg in a porcine post cardiac arrest model with and without targeted temperature management. Resuscitation. 2021;167:251–60.
Sundgreen C, Larsen FS, Herzog TM, Knudsen GM, Boesgaard S, Aldershvile J. Autoregulation of cerebral blood flow in patients resuscitated from cardiac arrest. Stroke. 2001;32(1):128–32.
Lautz AJ, Morgan RW, Karlsson M, Mavroudis CD, Ko TS, Licht DJ, et al. Hemodynamic-directed CPR improves neurologic outcomes and mitochondrial function in Heart and Brain. Crit Care Med. 2019;47(3):e241.
McGuigan PJ, Giallongo E, Blackwood B, Doidge J, Harrison DA, Nichol AD, et al. The effect of blood pressure on mortality following out-of-hospital cardiac arrest: a retrospective cohort study of the United Kingdom Intensive Care National Audit and Research Centre database. Crit Care. 2023;27(1):4.
Ushpol A, Je S, Niles D, Majmudar T, Kirschen M, Del Castillo J, et al. Association of blood pressure with neurologic outcome at hospital discharge after pediatric cardiac arrest resuscitation. Resuscitation. 2023;194:110066.
Topjian AA, Telford R, Holubkov R, Nadkarni VM, Berg RA, Dean JM, et al. Association of Early Postresuscitation Hypotension with Survival to Discharge after targeted temperature management for Pediatric out-of-hospital cardiac arrest: secondary analysis of a Randomized Clinical Trial. JAMA Pediatr. 2018;172(2):143–53.
Trzeciak S, Jones AE, Kilgannon JH, Milcarek B, Hunter K, Shapiro NI, et al. Significance of arterial hypotension after resuscitation from cardiac arrest. Crit Care Med. 2009;37(11):2895–903. quiz 904.
Topjian AA, French B, Sutton RM, Conlon T, Nadkarni VM, Moler FW, et al. Early post-resuscitation hypotension is associated with increased mortality following pediatric cardiac arrest. Crit Care Med. 2014;42(6):1518.
Berg RA, Sutton RM, Reeder RW, Berger JT, Newth CJ, Carcillo JA, et al. Association between diastolic blood pressure during pediatric in-hospital cardiopulmonary resuscitation and survival. Circulation. 2018;137(17):1784–95.
Morgan RW, French B, Kilbaugh TJ, Naim MY, Wolfe H, Bratinov G, et al. A quantitative comparison of physiologic indicators of cardiopulmonary resuscitation quality: diastolic blood pressure versus end-tidal carbon dioxide. Resuscitation. 2016;104:6–11.
O’Brien CE, Santos PT, Reyes M, Adams S, Hopkins CD, Kulikowicz E, et al. Association of diastolic blood pressure with survival during paediatric cardiopulmonary resuscitation. Resuscitation. 2019;143:50–6.
Wyckoff MH, Greif R, Morley PT, Ng K-C, Olasveengen TM, Singletary EM, et al. 2022 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations: Summary from the basic life support; advanced life support; pediatric life support; neonatal life support; education, implementation, and teams; and first aid task forces. Pediatrics. 2023;151(2):e2022060463.
Annoni F, Dell’Anna AM, Franchi F, Creteur J, Scolletta S, Vincent J-L, et al. The impact of diastolic blood pressure values on the neurological outcome of cardiac arrest patients. Resuscitation. 2018;130:167–73.
Wolfe HA, Sutton RM, Reeder RW, Meert KL, Pollack MM, Yates AR, et al. Functional outcomes among survivors of pediatric in-hospital cardiac arrest are associated with baseline neurologic and functional status, but not with diastolic blood pressure during CPR. Resuscitation. 2019;143:57–65.
Berg RA, Morgan RW, Reeder RW, Ahmed T, Bell MJ, Bishop R, et al. Diastolic blood pressure threshold during pediatric cardiopulmonary resuscitation and survival outcomes: a multicenter validation study. Crit Care Med. 2023;51(1):91–102.
Chi C-Y, Tsai M-S, Kuo L-K, Hsu H-H, Huang W-C, Lai C-H, et al. Post-resuscitation diastolic blood pressure is a prognostic factor for outcomes of cardiac arrest patients: a multicenter retrospective registry-based analysis. J Intensive Care. 2022;10(1):1–11.
Topjian AA, Sutton RM, Reeder RW, Telford R, Meert KL, Yates AR, et al. The association of immediate post cardiac arrest diastolic hypertension and survival following pediatric cardiac arrest. Resuscitation. 2019;141:88–95.
Rigamonti F, Graf G, Merlani P, Bendjelid K. The short-term prognosis of cardiogenic shock can be determined using hemodynamic variables: a retrospective cohort study. Crit Care Med. 2013;41(11):2484–91.
Feigl E. Coronary physiology. Physiol Rev. 1983;63(1):1–205.
Naim MY, Sutton RM, Friess SH, Bratinov G, Bhalala U, Kilbaugh TJ, et al. Blood pressure–and coronary perfusion pressure–targeted cardiopulmonary resuscitation improves 24-hour survival from ventricular fibrillation cardiac arrest. Crit Care Med. 2016;44(11):e1111–7.
Lamia B, Chemla D, Richard C, Teboul J-L. Clinical review: interpretation of arterial pressure wave in shock states. Crit Care. 2005;9(6):1–6.
Ospina-Tascón GA, Teboul J-L, Hernandez G, Alvarez I, Sánchez-Ortiz AI, Calderón-Tapia LE, et al. Diastolic shock index and clinical outcomes in patients with septic shock. Ann Intensiv Care. 2020;10:1–11.
Benchekroune S, Karpati PC, Berton C, Nathan C, Mateo J, Chaara M, et al. Diastolic arterial blood pressure: a reliable early predictor of survival in human septic shock. J Trauma Acute Care Surg. 2008;64(5):1188–95.
Gardner MM, Hehir DA, Reeder RW, Ahmed T, Bell MJ, Berg RA, et al. Identification of post-cardiac arrest blood pressure thresholds associated with outcomes in children: an ICU-Resuscitation study. Crit Care. 2023;27(1):1–12.
Gershengorn HB, Wunsch H, Scales DC, Zarychanski R, Rubenfeld G, Garland A. Association between arterial catheter use and hospital mortality in intensive care units. JAMA Intern Med. 2014;174(11):1746–54.
Acknowledgements
Not applicable.
Funding
This study was not supported by any funding or grants.
Author information
Authors and Affiliations
Contributions
MK.C and DH.K conceptualized the design of the study, contributed to the statical analysis and interpretation of the data, drafted the initial manuscript. JS.P, reviewed the initial and the revised draft of the manuscript. JH.H contributed the acquisition of the data. WK.J coordinated and supervised data collection. All authors read, provided feedback, and approved the final version of this article. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Asan Medical Center Ethics Committee, University of Ulsan College of Medicine (2024-0033) and waved the need for parental consent given the retrospective nature of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chun, M.K., Park, J.S., Han, J. et al. The association between initial post-resuscitation diastolic blood pressure and survival after pediatric cardiac arrest: a retrospective study. BMC Pediatr 24, 563 (2024). https://doi.org/10.1186/s12887-024-05037-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-024-05037-x