Abstract
Background
Given the critical role of immune cells and their responses in sepsis pathogenesis, this study aimed to evaluate the prognostic significance of various immune cell ratios in septic children through the collection and analysis of clinical data.
Methods
Clinical data were collected from septic children admitted to the pediatric intensive care unit (PICU) of Shenzhen Children’s Hospital between January 2019 and September 2021. The peripheral blood immune cell ratios included the neutrophil to lymphocyte ratio (NLR), the derived neutrophil to lymphocyte ratio (dNLR), the neutrophil to lymphocyte and platelet ratio (NLPR), the monocyte to lymphocyte ratio (MLR), and the platelet to lymphocyte ratio (PLR). To investigate the associations between these immune cell ratios and mortality, we utilized the locally weighted scatterplot smoothing (LOWESS) method, receiver operating characteristic (ROC) analysis, and Kaplan‒Meier (K‒M) analysis.
Results
A total of 230 septic children were enrolled in the study. When comparing the immune cell ratios between the deceased and surviving groups, all ratios except for the PLR were elevated in the deceased group. Using the LOWESS method, we observed that the MLR, NLR, dNLR, and NLPR exhibited an approximately linear association with in-hospital mortality. Among the various immune cell ratios, the NLPR exhibited the highest AUC of 0.748, which was statistically comparable to that of the Pediatric Critical Illness Score (PCIS) (0.748 vs. 0.738, P = 0.852). The NLR (0.652), MLR (0.638), and dNLR (0.615) followed in terms of AUC values. K‒M analysis revealed that children with elevated MLR, NLR, dNLR, and NLPR exhibited increased 30-day mortality.
Conclusion
The predictive capacity of the NLPR is comparable to that of the PCIS, suggesting that the NLPR has potential as a robust prognostic indicator for septic children.
Similar content being viewed by others
Introduction
Sepsis, resulting from a deregulated host response to infection, is a leading cause of systemic multiorgan dysfunction [1]. Despite a decreasing hospital mortality rate, sepsis still affects approximately 5.3 million people globally each year [2]. The condition of septic children is particularly complex, with often atypical symptoms that can rapidly change or progress, posing a significant threat to their lives. Early identification of high-risk children with sepsis and timely, appropriate intervention are thus paramount [3].
Despite significant research efforts, the identification of high-risk patients remains challenging [4]. Cytokines, including STREM-1, proenzymes, and interleukins, have garnered increasing attention for their potential in early sepsis recognition and prognosis prediction [5,6,7,8,9]. However, their clinical application is hindered by their high cost and complex operational techniques. Some critical scoring systems, such as the Paediatric Risk of Mortality (PRISM) III score and the Pediatric Critical Illness Score (PCIS), are widely used in paediatric intensive care units (PICUs) and have been used to accurately assess disease severity and prognosis in septic children [10]. These critical scoring systems involve many indicators, cumbersome operations, and unstable prediction accuracy, resulting in limited practical application, especially in some poor countries and regions.
Immune cells play a crucial role in the onset and progression of sepsis. They participate in both innate and adaptive immune responses through mechanisms such as phagocytosis, release of reactive oxygen species, and cytokine production [11, 12]. Existing evidence indicates that sepsis can alter the quantity and function of immune cells [13,14,15]. Notably, due to their immature immune development, limited regulatory and compensatory abilities, and significant individual differences, children are more prone to immune cell imbalances than are adults.
The complete blood count (CBC), a widely utilized and cost-effective testing method in pediatric clinical practice, serve as valuable biomarkers for systemic inflammation and immune responses. Recently, immune cell ratios, such as the neutrophil-to-lymphocyte ratio (NLR), derived neutrophil-to-lymphocyte ratio (dNLR), neutrophil-to-lymphocyte-to-platelet ratio (NLPR), monocyte-to-lymphocyte ratio (MLR), and platelet-to-lymphocyte ratio (PLR), have been associated with adverse outcomes in various diseases, including cancer [16, 17], critical illnesses [18, 19], cardiovascular diseases [20, 21], stroke [22], and COVID-19 [23]. These ratios, which are emerging as prognostic indicators, are gaining increasing attention from the medical community. Changes in immune cells are common in sepsis patients, yet limited research exists on the association between immune cell ratios and the prognosis of septic children in the PICU. Furthermore, there is a dearth of simple clinical indicators for assessing the prognosis of septic children. Therefore, the aim of this study was to investigate the predictive value of various immune cell ratios for the short-term prognosis of septic children, aiming to provide reliable clues for the early identification of high-risk patients.
Materials and methods
Source of patients
A retrospective analysis was conducted to gather clinical data from children with sepsis admitted to the PICU of Shenzhen Children’s Hospital between January 2019 and September 2021. Approval for the study was granted by the Ethics Committee of Shenzhen Children’s Hospital. As the retrospective nature of the study did not impact clinical decision-making, the informed consent was waived by the ethics committee.
Inclusion and exclusion criteria
The inclusion criteria for patients were as follows: (1) were children who were diagnosed with septicemia upon admission to the PICU; (2) were aged between 28 days and 18 years; and (3) had multiple hospitalizations in the PICU for whom only data from the initial hospitalization were available.
The exclusion criteria were as follows: (1) absence of routine blood test data within 24 h of PICU admission; (2) concurrent hematological malignancies or end-stage malignancies; (3) patients who received organ transplantation or used hormones, cytotoxic drugs, or immunosuppressive agents within the past 2 weeks; (4) PICU hospitalization duration less than 24 h; and (5) patients who elect to forgo treatment, opt for voluntary discharge, or who are referred to another medical facility.
Data collection
Clinical information for children with sepsis was gathered from the medical records management system and subsequently entered and managed using Epidata V.3.1 software (www.epidata.dk). The demographic data collected included age and sex. Routine blood examination data were retrieved from the Laboratory Department of Shenzhen Children’s Hospital, with the initial values recorded within 24 h of admission to the PICU.
The PCIS score, encompassing 10 indicators—including heart rate, systolic blood pressure, respiration, oxygen partial pressure, pH, serum sodium, serum potassium, serum creatinine or urea nitrogen, haemoglobin, and gastrointestinal manifestations—ranged from 0 to 100. Lower scores indicate more severe illness. The worst values of each PCIS were captured within 24 h of hospitalization in the PICU. Notably, missing values for all variables were limited to less than 10%, and thus, the missing values were replaced with the mean or median.
Regarding the immune cell ratios, the following calculation methods were applied in this study: (1) PLR = platelet count divided by lymphocyte count; (2) MLR = monocyte count divided by lymphocyte count; (3) NLR = neutrophil count divided by lymphocyte count; (4) dNLR = the ratio of neutrophils to (white blood cells - neutrophils); and (5) NLPR = neutrophil count multiplied by 100 divided by (lymphocyte count multiplied by platelet count). The primary outcome indicator was inpatient mortality, defined as death occurring during hospitalization.
Statistical analysis
Continuous variables with a normal distribution are expressed as the mean ± standard deviation. Differences between two groups were compared using Student’s t test. Variables with a skewed distribution are represented by the median (interquartile range) and were compared using the Mann‒Whitney U test. Categorical variables are presented as the number of cases (percentages) and were analysed using the chi-square test to assess differences between the groups.
Locally weighted scatterplot smoothing (LOWESS) was employed to elucidate the approximate relationship between various ratios of peripheral blood immune cells and inpatient mortality among children with sepsis. Receiver operating characteristic (ROC) curves were generated to assess the predictive utility of these immune cell ratios for inpatient mortality. The Youden index, which is the sum of the sensitivity and specificity minus 1, was computed to determine the optimal cut-off value based on the maximum Youden index. The Z test was utilized to compare the area under the curve (AUC) values among different indicators. Furthermore, we conducted a sensitivity analysis to investigate the predictive value of various immune cell ratios on mortality across different age subgroups and in subgroups stratified by the presence or absence of multi-system infection.
Children with sepsis were stratified based on the established cut-off values for different immune cell ratios. Kaplan‒Meier (K‒M) analysis was then conducted to generate 30-day survival curves for each stratum, and these curves were compared using the log-rank test. Statistical significance was set at P < 0.05. All the statistical analyses were performed using STATA V.16, R V.4.2.1 and MedCalc V.18.2.1.
Results
General information of the enrolled patients
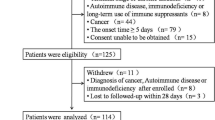
The flowchart depicting the selection of study subjects is presented in Fig. 1. Table 1 summarizes the baseline demographics of the children with sepsis. A total of 230 pediatric patients with sepsis were enrolled, with 131 (57.0%) being male and 99 (43.0%) being female, yielding a median age of 16 months. Regarding the sources of sepsis infection (multiple sites can be concurrently infected upon admission to the PICU), respiratory system involvement was observed in 150 patients (65.2%), followed by digestive system involvement in 74 patients (32.2%), blood system involvement in 75 patients (32.6%), and involvement of other sites in 87 patients (37.8%).
The median duration of ICU stay among the children with sepsis was 4.5 days, with 122 patients (53.0%) requiring mechanical ventilation support. A total of 51 patients (22.2%) died in the hospital.
Comparison of clinical data between septic patients in the survival group and those in the nonsurviving group
A comparison was conducted between septic children in the survival and death groups, and the results are summarized in Table 1. The death group exhibited significantly lower lymphocyte counts (1.44 vs. 2.05, P = 0.010), platelet counts (119 vs. 225, P < 0.001), and PCIS scores (78 vs. 86, P < 0.001) than did the survival group. Additionally, significant differences in immune cell ratios were observed between the two groups. Specifically, compared with the survival group, the death group had elevated MLR (0.43 vs. 0.26, P = 0.003), NLR (4.83 vs. 2.41, P < 0.001), dNLR (3.16 vs. 1.87, P = 0.012), and NLPR (5.22 vs. 1.06, P < 0.001) compared to the survival group, except for PLR.
Approximate association between immune cell ratios and in-hospital mortality in patients with pediatric sepsis
Using the LOWESS method, we examined the approximate relationship between immune cell ratios and in-hospital mortality among children with sepsis. Figure 2 illustrates that the PLR exhibits an inverted “U”-shaped association with hospital mortality. Notably, the lowest hospital mortality rate (11%) occurred when the PLR ranged between 150 and 250. Conversely, when the PLR was below 25 or above 550, the hospital mortality rates increased to 50% and 38%, respectively.
Relationship between the immune cell ratio and in-hospital mortality in children with sepsis. (A) Platelet-to-lymphocyte ratio (PLR); (B) monocyte-to-lymphocyte ratio (MLR); (C) neutrophil-to-lymphocyte ratio (NLR); (D) derived neutrophil-to-lymphocyte ratio (dNLR); (E) neutrophil-to-lymphocyte and platelet ratio (NLPR)
Threshold effect analysis and likelihood ratio tests were used to compare the difference between linear analysis (Model I) and non-linear analysis (Model II), and the bootstrap resampling method was used to analyze the threshold effect between PLR and the risk of hospital mortality. As depicted in Fig. 2A, the mortality rate was lower in the PLR range of 150–250 compared to other ranges. Consequently, we attempted to use 150 and 250 as two inflection points. The P-value for the likelihood ratio test of the models was less than 0.001, demonstrating a nonlinear relationship between PLR and risk of hospital mortality (Supplementary Table 1). When PLR was less than 150, the OR value was 0.983 (0.972–0.993) with a P-value of 0.001. For PLR values between 150 and 250, the OR value was 1.006 (0.983–1.029) with a P-value of 0.605. When PLR exceeded 250, the OR value was 1.000 (0.999–1.001) with a P-value of 0.887.
Furthermore, our analysis revealed an approximately linear growth relationship between the MLR, NLR, dNLR, and NLPR and in-hospital mortality. Specifically, hospital mortality rates reached 55% when the MLR ranged between 1.0 and 1.5, 44% when the NLR exceeded 15.0, 50% when the dNLR exceeded 15.0, and 55% when the NLPR exceeded 15.0. These findings suggest that specific immune cell ratios may serve as prognostic indicators for in-hospital mortality in patients with pediatric sepsis.
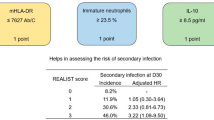
The ability of immune cell ratios to predict in-hospital mortality in patients with pediatric sepsis
The results of the ROC analysis, presented in Fig. 3A; Table 2, demonstrate the predictive value of the MLR, NLR, dNLR, and NLPR for in-hospital mortality in children with sepsis. All four ratios exhibited significant predictive ability (P < 0.05), with AUC values of 0.638, 0.652, 0.615, and 0.748, respectively.
Receiver operating characteristic (ROC) analysis. (A) ROC curves for predicting hospital mortality in children with sepsis using different immune cell ratios; (B) ROC curves for predicting hospital mortality in children with sepsis using the pediatric critical illness score (PCIS) score and the neutrophil-to-lymphocyte and platelet ratio (NLPR). dNLR, derived neutrophil-to-lymphocyte ratio; MLR, monocyte-to-lymphocyte ratio; NLR, neutrophil-to-lymphocyte ratio; PLR, platelet-to-lymphocyte ratio
For the MLR, the optimal cut-off value was 0.61, yielding a predictive sensitivity of 41.18% and specificity of 84.92% (P = 0.004). The NLR demonstrated an optimal cut-off value of 2.48, resulting in a predictive sensitivity of 74.51% and specificity of 51.96% (P < 0.001). Similarly, the dNLR had an optimal cut-off value of 1.59, achieving a predictive sensitivity of 78.43% and specificity of 45.25% (P = 0.008). The NLPR exhibited an optimal cut-off value of 2.34, with a predictive sensitivity of 68.63% and specificity of 71.51% (P < 0.001).
In the sensitivity analysis, we examined the predictive value of various immune cell ratios on mortality across different age subgroups and subgroups based on the presence or absence of multi-system infection. Initially, we stratified our study population into a younger age group (≤ 16 months) and an older age group (> 16 months) based on the median age. As shown in Supplementary Table 2, both the single indicator NLPR and the composite indicator PCIS demonstrated good predictive value in both age groups. Notably, in the younger age group, the AUC value of NLPR (0.796) was higher than that of PCIS (0.729). Similarly, in the subgroup analysis based on the presence or absence of multi-system infection, the results remained consistent across different subgroups (Supplementary Table 3).
As depicted in Fig. 3B; Table 3, among all the immune cell ratios, the NLPR had the highest predictive value for in-hospital mortality in septic children, even higher than that of the NLR, which ranked second (Z = 2.553, P = 0.011). The AUC for the PCIS was 0.738, with an optimal cut-off value of 84. The predictive sensitivity of the PCIS was 84.31%, while the specificity was 54.75% (P < 0.001). Notably, there was no statistically significant difference in the AUC between the NLPR and PCIS (Z = 0.187, P = 0.852).
Survival analysis of pediatric sepsis patients stratified by immune cell ratios
The K‒M curves depicted in Fig. 4A-E illustrate the associations between distinct immune cell ratios and 30-day mortality among children with sepsis. Notably, children in the high MLR, NLR, dNLR, and NLPR groups exhibited lower survival rates than those in the corresponding low groups at various time points (P < 0.05). This trend is mirrored in the survival curves for PCIS (Fig. 4F). Furthermore, the log-rank test yielded P-values less than 0.001 for both NLPR and PCIS.
Kaplan‒Meier analysis of the relationship between immune cell ratios and 30-day mortality in children with sepsis. (A) Platelet-to-lymphocyte ratio (PLR); (B) monocyte-to-lymphocyte ratio (MLR); (C) neutrophil-to-lymphocyte ratio (NLR); (D) derived neutrophil-to-lymphocyte ratio (dNLR); (E) neutrophil-to-lymphocyte and platelet ratio (NLPR); (F) Pediatric Critical Illness Score (PCIS)
Compared to those in the normal PLR group, children in the high PLR group had a lower survival rate (P = 0.046). No significant difference in survival rate was observed between the normal PLR group and the low PLR group (P = 0.133). However, this contradicts the findings obtained in our curve fitting section. There exists uncertainty regarding the use of PLR as a prognostic indicator in pediatric sepsis.
Discussion
Immune cells play a crucial role in the etiology and progression of sepsis, with alterations in their number and function significantly influencing the inflammatory and anti-inflammatory balance early in the disease course. The primary objective of this study was to assess the prognostic implications of various immune cell ratios in septic children admitted to the PICU. Specifically, we focused on the PLR, MLR, NLR, dNLR, and NLPR, integrating immune cells (neutrophils, lymphocytes, monocytes, and platelets) pertinent to sepsis pathogenesis and progression. This study highlighted the intricate immune-immune and immune-coagulation interactions underlying the inflammatory response in sepsis.
Our findings revealed that, except for the PLR, immune cell ratios were greater in the nonsurviving group than in the surviving group. The LOWESS method demonstrated a linear association between the MLR, NLR, dNLR, and NLPR and in-hospital mortality. Furthermore, we used ROC curves to assess the ability of these immune cell ratios to predict in-hospital mortality in septic children. The results indicated that the NLPR had predictive power comparable to that of the PCIS, followed by the NLR, MLR, and dNLR. K‒M analysis further revealed greater 30-day mortality rates among children with elevated MLR, NLR, dNLR, and NLPR. These findings offer valuable insights into the prognostic implications of immune cell ratios in pediatric sepsis patients, emphasizing the importance of immune cell monitoring in clinical practice.
Our study revealed no significant differences in white blood cell count, neutrophil count, or monocyte count between the nonsurviving and surviving groups upon admission. However, the lymphocyte count and platelet count were notably lower in the nonsurviving group. These observations align with previous research findings [24, 25]. White blood cells, a heterogeneous population encompassing lymphocytes, monocytes, and granulocytes, can exhibit elevated counts in sepsis patients but may also remain unchanged or decrease. Consequently, the specificity of the white blood cell (WBC) count as a biomarker of sepsis is limited. In this study, both groups exhibited relatively high neutrophil counts within the normal range, with a slight increase in the nonsurviving group; however, the difference was not statistically significant. Neutrophils, the most abundant leukocyte subpopulation, are influenced by numerous factors, including age, stress, hypoxia, endocrine function, medications, infection, and bone marrow haematopoiesis. Therefore, achieving a consistent trend in neutrophil count changes in complex disease environments remains challenging [25]. Monocytes, a heterogeneous cell population, exhibit diverse morphologies, functions, and phenotypic characteristics. Under physiological conditions, classical monocytes constitute approximately 85% of circulating monocytes, intermediate monocytes account for 5%, and nonclassical monocytes constitute 10% of the total [26]. During sepsis, monocytes transition from the classical subtype to intermediate and nonclassical subtypes [27]. Despite the pivotal role of monocytes in sepsis, the impact of monocyte count on sepsis patient prognosis remains controversial. Some studies have associated increased monocyte counts with increased mortality, while others have linked monocyte depletion to increased mortality [11, 28]. Consequently, the predictive value of a single monocyte count for the prognosis of patients with sepsis is limited.
Increasing evidence indicates that lymphocytopenia, which involves the depletion of T cells, B cells, and natural killer cells, frequently occurs during sepsis, ultimately leading to immune paralysis [29]. Clinical studies examining lymphocyte counts have revealed that this decrease not only occurs at sepsis onset but also persists at a low level for up to 28 days [30, 31]. Drewry et al. [30] conducted a single-center retrospective cohort study to assess whether sustained lymphocytopenia following sepsis diagnosis is a predictor of inpatient mortality. The findings demonstrated significantly lower lymphocyte counts on the 4th day postdiagnosis among nonsurvivors than among survivors. Multivariate logistic regression analysis revealed that the absolute lymphocyte count on the 4th day was independently correlated with 28-day mortality (adjusted OR 0.68, 95% CI 0.51–0.91) and 1-year mortality (adjusted OR 0.74, 95% CI 0.59–0.93). Inflammation and coagulation dysfunction are key contributors to organ damage in sepsis, with platelets playing a pivotal role in both processes [32]. Thrombocytopenia is common in PICU wards [33] and serves as a reliable predictor of poor prognosis in sepsis patients [34]. The emergence of thrombocytopenia in sepsis is linked to various factors, including decreased platelet production, blood dilution, platelet-leukocyte aggregation, immune-mediated platelet destruction, drug-induced thrombocytopenia, and disseminated intravascular coagulation [35, 36].
This study revealed significantly elevated values of MLR, NLR, dNLR, and NLPR in the septic death group compared to the survival group (P < 0.05), consistent with previous research [23, 24, 37]. However, no significant difference in the PLR was observed between the two groups. Few studies exist on the associations between the PLR or MLR and the prognosis of septic patients. A four-year prospective study encompassing 392 critically ill patients with sepsis showed no significant difference in the PLR between the death and survival groups, and logistic regression analysis did not establish a correlation between the PLR and mortality [24]. Our study employed LOWESS analysis to detect a putative “U”-shaped relationship between the PLR and in-hospital mortality among children with sepsis. Patients were subsequently categorized into three groups based on their PLR: low, normal, and high. After conducting a threshold effect analysis, it appears that a low PLR is associated with increased in-hospital mortality, whereas a high PLR seems unrelated. However, further survival analysis yielded contradictory results. The findings from our survival analysis align with those reported by Shen et al. [38]. It is widely recognized that low levels of lymphocytes and platelets correlate with poor prognosis. Nevertheless, it’s important to note that platelets and lymphocytes can trigger or exacerbate inflammatory processes by inducing the release of inflammatory cytokines and interacting with various bacteria and immune cells. Consequently, higher levels of platelets and lymphocytes may indicate a more severe inflammatory response. Therefore, the relationship between PLR and the prognosis of pediatric sepsis remains uncertain, requiring further validation with a larger sample size. Additionally, the association between PLR and outcomes varies considerably among different patient populations, and the heterogeneity among critically ill patients may also lead to deviations in results.
Monocytes constitute a crucial component of the innate immune system, presenting antigens to lymphocytes and serving as a bridge to the adaptive immune system. Current prognostic studies on the MLR primarily focus on malignant tumors, where it has been shown to predict mortality in patients with ovarian cancer, liver cancer, endometrial cancer, and colon cancer [39,40,41,42]. Given the established association between inflammation and malignant tumors, where inflammatory reactions play a pivotal role in tumor proliferation, invasion, and metastasis, this study aimed to investigate whether the MLR can serve as a predictor of inpatient mortality in children with sepsis. Our findings revealed that higher MLRs were associated with an elevated risk of inpatient mortality. However, this finding is not unanimous. A case‒control study evaluated the correlation between the MLR and various critical illness scores, including the Acute Physiology and Chronic Health Evaluation II, Simplified Acute Physiology Score II, and Sequential Organ Failure Assessment scores. The results did not demonstrate a linear correlation between the MLR and these scores (P > 0.05), and the MLR was not identified as an independent risk factor for inpatient mortality (OR 0.91, 95% CI 0.46–1.80) [43]. Given the physiological disparities between adults and children, further studies are imperative to elucidate the relationships between the PLR and MLR and their prognostic implications in children with sepsis.
The prognostic predictive role of the NLR in sepsis has been extensively studied, particularly in adults, but relatively few studies have focused on pediatric patients. In a separate study conducted by Fois et al. [23], a statistical analysis of the NLR and dNLR was performed among 119 adult patients with COVID-19 upon admission. Significantly elevated NLR and dNLR values were observed in the deceased group. K‒M survival curves demonstrated a significantly lower survival rate among patients with a higher NLR or dNLR. Although the difference in neutrophil counts between the surviving and deceased groups was not statistically significant in this study, the NLR and dNLR were significantly greater in the deceased group. This suggests that the difference in the NLR and dNLR between the two groups may be primarily attributed to differences in lymphocyte counts. The NLR and dNLR serve as markers of the balance between neutrophils and lymphocytes, providing a comprehensive indication of the immune status of the body. Given the association between the NLR and inflammatory response severity, it is speculated that an elevated NLR and dNLR may be associated with the severity of the inflammatory response in children with sepsis. Future studies are needed to further investigate the prognostic implications of the NLR and dNLR in pediatric sepsis patients.
With low AUC values, the NLR and dNLR possess limited predictive capacity for mortality in pediatric sepsis patients, rendering them unreliable prognostic indicators. In contrast, the NLPR, a novel prognostic marker, has garnered increasing attention from the medical community in recent years. Gameiro et al. [44] analyzed the prognostic relationship between NLPR and outcomes in a retrospective study involving 399 patients with sepsis complicated by acute kidney injury. The results indicated that the NLPR in the deceased group was significantly higher than that in the survival group (P = 0.028). When NLPR was analyzed as a continuous variable, the adjusted OR was 1.01 (95% CI 1.00-1.02). When treated as a categorical variable, the adjusted OR was 2.14 (95% CI 1.23–3.71). In another observational study, researchers evaluated the impact of NLR and NLPR on the 28-day in-hospital mortality rate of sepsis patients [45]. The results showed that the AUC for predicting 28-day mortality was 0.762 for NLR and 0.827 for NLPR. After grouping NLR and NLPR based on optimal cutoff values, both the high NLR and high NLPR groups had higher mortality rates and shorter survival times compared to the low NLR and low NLPR groups, respectively. These findings align with the results presented in our study.
By seamlessly integrating platelet counts into the traditional NLR, the NLPR aims to enhance its predictive capabilities. This study revealed that the NLPR exhibited the highest AUC among various immune cell ratios, highlighting its strong predictive power for inpatient mortality in children with sepsis. Notably, the NLPR demonstrated comparable predictive accuracy to that of the established PCIS. However, the clinical application of the PCIS is hindered by the requirement for numerous data inputs, encompassing blood pressure, blood gas, renal function, and other parameters. Conversely, the NLPR, an economically viable and easily accessible laboratory hematological parameter, may pave the way for its widespread clinical utilization.
This study has several noteworthy advantages. Firstly, we comprehensively explored the ability of various immune cell ratios to predict the prognosis of patients with pediatric sepsis, facilitating the identification of an indicator that rivals the predictive accuracy of the established PCIS. Secondly, the widespread availability and affordability of routine blood examination render it a practical tool for prognosis prediction in septic children, especially in low-income nations or regions with limited medical resources.
Certain limitations of this study should be acknowledged. Firstly, the single-center design may have introduced selection bias, affecting the representativeness of the study cohort. Secondly, its retrospective nature precluded the elucidation of a clear mechanism underlying the association between immune cell ratios and prognosis. Furthermore, retrospective studies inherently rely on existing data records, which may be incomplete or contain errors. Such issues could potentially introduce bias into the study results. In our future work, we plan to adopt a prospective study design, involving subjects from at least two centers and expanding the sample size. Our purpose is to construct a clinical prediction model based on NLPR combined with multiple indicators. Thirdly, due to the limitations of being a retrospective study and having a small sample size, we were unable to analyze some relatively important variables, such as the predictive value of immune cell composition for multidrug-resistant bacteria. Finally, the exclusion of dynamic immune cell data beyond the initial 24 h after admission to the PICU limited the scope of our findings.
Conclusion
Sepsis, a disease of significant concern among PICU practitioners, necessitates early identification of high-risk patients for improved prognosis. The present study investigated the association between various immune cell ratios and in-hospital mortality among septic children admitted to the PICU. Our findings revealed the limited ability of the MLR, NLR, and dNLR to predict in-hospital mortality. Conversely, the NLPR demonstrated robust predictive power comparable to that of the PCIS. Through this study, we have identified NLPR as a promising simple indicator. Integrating NLPR with other laboratory markers or scoring systems to construct a prognostic prediction model would be a highly worthwhile research avenue.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- AUC:
-
Area under curve
- CBC:
-
Complete blood count
- dNLR:
-
Derived neutrophil-to-lymphocyte ratio
- LOWESS:
-
Locally weighted scatterplot smoothing
- MLR:
-
Monocyte-to-lymphocyte ratio
- NLPR:
-
Neutrophil-to-lymphocyte and platelet ratio
- NLR:
-
Neutrophil-to-lymphocyte ratio
- PCIS:
-
Pediatric critical illness score
- PICU:
-
Pediatric intensive care unit
- PLR:
-
Platelet-to-lymphocyte ratio
- PRISM:
-
Paediatric risk of mortality
- ROC:
-
Receiver operating characteristic
- WBC:
-
White blood cell
References
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8). https://doi.org/10.1001/jama.2016.0287.
Fleischmann C, Scherag A, Adhikari NKJ, Hartog CS, Tsaganos T, Schlattmann P, et al. Assessment of global incidence and mortality of hospital-treated sepsis. Current estimates and limitations. Am J Respir Crit Care Med. 2016;193(3):259–72. https://doi.org/10.1164/rccm.201504-0781OC.
Vincent J-L, Pereira AJ, Gleeson J, Backer DD. Early management of sepsis. Clin Exp Emerg Med. 2014;1(1):3–7. https://doi.org/10.15441/ceem.14.005.
Opal SM, Wittebole X. Biomarkers of infection and sepsis. Crit Care Clin. 2020;36(1):11–22. https://doi.org/10.1016/j.ccc.2019.08.002.
Chen MK, Zhu Y. Utility of sTREM-1 and Presepsin (sCD14-ST) as diagnostic and prognostic markers of sepsis. Clin Lab. 2020;66(4):495–501. https://doi.org/10.7754/Clin.Lab.2019.190508.
Srisawat N, Kulvichit W, Tungsanga S, Peerapornratana S, Vorasitchai S, Tangkanakul C, et al. The role of neutrophil chemotaxis activity as an immunologic biomarker to predict mortality in critically-ill patients with severe sepsis. J Crit Care. 2020;56:215–21. https://doi.org/10.1016/j.jcrc.2020.01.020.
Jekarl DW, Kim JY, Lee S, Kim M, Kim Y, Han K, et al. Diagnosis and evaluation of severity of sepsis via the use of biomarkers and profiles of 13 cytokines: a multiplex analysis. Clin Chem Lab Med. 2015;53(4). https://doi.org/10.1515/cclm-2014-0607.
Sandquist M, Wong HR. Biomarkers of sepsis and their potential value in diagnosis, prognosis and treatment. Expert Rev Clin Immunol. 2014;10(10):1349–56. https://doi.org/10.1586/1744666x.2014.949675.
Huang Q, Xiong H, Yan P, Shuai T, Liu J, Zhu L, et al. The diagnostic and prognostic value of supar in patients with sepsis: a systematic review and meta-analysis. Shock. 2020;53(4):416–25. https://doi.org/10.1097/shk.0000000000001434.
Shen H, Qu D, Na W, Liu S, Huang S, Hui Y. Comparison of the OI and PaO2/Fio2 score in evaluating pards requiring mechanical ventilation. Pediatr Pulmonol. 2020;56(5):1182–8. https://doi.org/10.1002/ppul.25194.
Radzyukevich YV, Kosyakova NI, Prokhorenko IR, Mulens V. Participation of monocyte subpopulations in progression of experimental endotoxemia (EE) and systemic inflammation. J Immunol Res. 2021;2021(1–9). https://doi.org/10.1155/2021/1762584.
Jenne CN, Kubes P. Platelets in inflammation and infection. Platelets. 2015;26(4):286–92. https://doi.org/10.3109/09537104.2015.1010441.
Cao C, Yu M, Chai Y. Pathological alteration and therapeutic implications of sepsis-induced immune cell apoptosis. Cell Death Dis. 2019;10(10). https://doi.org/10.1038/s41419-019-2015-1.
Rimmelé T, Payen D, Cantaluppi V, Marshall J, Gomez H, Gomez A, et al. Immune cell phenotype and function in sepsis. Shock. 2016;45(3):282–91. https://doi.org/10.1097/shk.0000000000000495.
Delano MJ, Ward PA. The immune system’s role in sepsis progression, resolution, and long-term outcome. Immunol Rev. 2016;274(1):330–53. https://doi.org/10.1111/imr.12499.
Kim JH, Son NH, Lee JS, Mun JE, Kim JY, Park HS, et al. Time-sequencing of the neutrophil-to-lymphocyte ratio to predict prognosis of triple-negative breast cancer. Cancers (Basel). 2021;13(14). https://doi.org/10.3390/cancers13143472.
Basile D, Garattini SK, Corvaja C, Montico M, Cortiula F, Pelizzari G, et al. The MIMIC study: prognostic role and cutoff definition of monocyte-to-lymphocyte ratio and lactate dehydrogenase levels in metastatic colorectal cancer. Oncologist. 2020;25(8):661–8. https://doi.org/10.1634/theoncologist.2019-0780.
Wang X, Wang J, Wu S, Ni Q, Chen P. Association between the neutrophil percentage-to-albumin ratio and outcomes in cardiac intensive care unit patients. Int J Gen Med. 2021;14:4933–43. https://doi.org/10.2147/ijgm.S328882.
Zhai G, Liu Y, Wang J, Zhou Y. Association of monocyte-lymphocyte ratio with in-hospital mortality in cardiac intensive care unit patients. Int Immunopharmacol. 2021;96. https://doi.org/10.1016/j.intimp.2021.107736.
Li Z, Gao Q, Ren Z, Zhou H, Qian Z, Peng J. Nomogram based on neutrophil-to-platelet ratio to predict in-hospital mortality in infective endocarditis. Biomark Med. 2021;15(14):1233–43. https://doi.org/10.2217/bmm-2021-0085.
Li Y, Zou Z, Zhang Y, Zhu B, Ning Y, Shen B, et al. Dynamics in perioperative neutrophil-to-lymphocyte*platelet ratio as a predictor of early acute kidney injury following cardiovascular surgery. Ren Fail. 2021;43(1):1012–9. https://doi.org/10.1080/0886022x.2021.1937220.
He W, Ruan Y, Yuan C, Cheng Q, Cheng H, Zeng Y, et al. High neutrophil-to-platelet ratio is associated with hemorrhagic transformation in patients with acute ischemic stroke. Front Neurol. 2019;10. https://doi.org/10.3389/fneur.2019.01310.
Fois AG, Paliogiannis P, Scano V, Cau S, Babudieri S, Perra R, et al. The systemic inflammation index on admission predicts in-hospital mortality in covid-19 patients. Molecules. 2020;25(23). https://doi.org/10.3390/molecules25235725.
Djordjevic D, Rondovic G, Surbatovic M, Stanojevic I, Udovicic I, Andjelic T et al. Neutrophil-to-lymphocyte ratio, monocyte-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and mean platelet volume-to-platelet count ratio as biomarkers in critically ill and injured patients: Which ratio to choose to predict outcome and nature of bacteremia? Mediators Inflamm. 2018; 2018:1–15. https://doi.org/10.1155/2018/3758068
Liu S, Li Y, She F, Zhao X, Yao Y. Predictive value of immune cell counts and neutrophil-to-lymphocyte ratio for 28-day mortality in patients with sepsis caused by intra-abdominal infection. Burns Trauma. 2021;9. https://doi.org/10.1093/burnst/tkaa040.
Ożańska A, Szymczak D, Rybka J. Pattern of human monocyte subpopulations in health and disease. Scand J Immunol. 2020;92(1). https://doi.org/10.1111/sji.12883.
Ferreira da Mota NV, Brunialti MKC, Santos SS, Machado FR, Assuncao M, Azevedo LCP, et al. Immunophenotyping of monocytes during human sepsis shows impairment in antigen presentation: a shift toward nonclassical differentiation and upregulation of fcγri-receptor. Shock. 2018;50(3):293–300. https://doi.org/10.1097/shk.0000000000001078.
Chung H, Lee JH, Jo YH, Hwang JE, Kim J. Circulating monocyte counts and its impact on outcomes in patients with severe sepsis including septic shock. Shock. 2019;51(4):423–9. https://doi.org/10.1097/shk.0000000000001193.
Xue M, Zhang S, Xie J, Zhang X, Liu F, Huang Y, et al. Differential expression of genes associated with T lymphocytes function in septic patients with hypoxemia challenge. Ann Transl Med. 2019;7(24):810–810. https://doi.org/10.21037/atm.2019.12.63.
Drewry AM, Samra N, Skrupky LP, Fuller BM, Compton SM, Hotchkiss RS. Persistent lymphopenia after diagnosis of sepsis predicts mortality. Shock. 2014;42(5):383–91. https://doi.org/10.1097/shk.0000000000000234.
Monserrat J, de Pablo R, Diaz-Martín D, Rodríguez-Zapata M, de la Hera A, Prieto A, et al. Early alterations of b cells in patients with septic shock. Crit Care. 2013;17(3). https://doi.org/10.1186/cc12750.
Shannon O. The role of platelets in sepsis. Res Pract Thromb Hae. 2021;5(1):27–37. https://doi.org/10.1002/rth2.12465.
Kaur A. Thrombocytopenia in Paediatric ICU: incidence, transfusion requirement and role as prognostic indicator. J Clin Diagn Res. 2015. https://doi.org/10.7860/jcdr/2015/14590.6921.
Giustozzi M, Ehrlinder H, Bongiovanni D, Borovac JA, Guerreiro RA, Gąsecka A, et al. Coagulopathy and sepsis: pathophysiology, clinical manifestations and treatment. Blood Rev. 2021;50. https://doi.org/10.1016/j.blre.2021.100864.
McDonald B, Dunbar M. Platelets and intravascular immunity: guardians of the vascular space during bloodstream infections and sepsis. Front Immunol. 2019;10. https://doi.org/10.3389/fimmu.2019.02400.
Vardon-Bounes F, Ruiz S, Gratacap M-P, Garcia C, Payrastre B, Minville V. Platelets are critical key players in sepsis. Int J Mol Sci. 2019;20(14). https://doi.org/10.3390/ijms20143494.
Liu S, Wang X, She F, Zhang W, Liu H, Zhao X. Effects of neutrophil-to-lymphocyte ratio combined with interleukin-6 in predicting 28-day mortality in patients with sepsis. Front Immunol. 2021;12. https://doi.org/10.3389/fimmu.2021.639735.
Shen Y, Huang X, Zhang W. Platelet-to-lymphocyte ratio as a prognostic predictor of mortality for sepsis: Interaction effect with disease severity—a retrospective study. BMJ Open. 2019;9(1). https://doi.org/10.1136/bmjopen-2018-022896.
Xiang J, Zhou L, Li X, Bao W, Chen T, Xi X, et al. Preoperative monocyte-to-lymphocyte ratio in peripheral blood predicts stages, metastasis, and histological grades in patients with ovarian cancer. Transl Oncol. 2017;10(1):33–9. https://doi.org/10.1016/j.tranon.2016.10.006.
Nouri-Vaskeh M, Mirza-Aghazadeh-Attari M, Pashazadeh F, Azami-Aghdash S, Alizadeh H, Pouya P, et al. Prognostic impact of monocyte to lymphocyte ratio in clinical outcome for patients with hepatocellular carcinoma: a systematic review and meta-analysis. Galen Med J. 2020;9. https://doi.org/10.31661/gmj.v9i0.1948.
Song H, Jeong MJ, Cha J, Lee JS, Yoo JG, Song MJ, et al. Preoperative neutrophil-to-lymphocyte, platelet-to-lymphocyte and monocyte-to-lymphocyte ratio as a prognostic factor in non-endometrioid endometrial cancer. Int J Med Sci. 2021;18(16):3712–7. https://doi.org/10.7150/ijms.64658.
Jakubowska K, Koda M, Grudzińska M, Kańczuga-Koda L, Famulski W. Monocyte-to-lymphocyte ratio as a prognostic factor in peripheral whole blood samples of colorectal cancer patients. World J Gastroenterol. 2020;26(31):4639–55. https://doi.org/10.3748/wjg.v26.i31.4639.
Liberski PS, Szewczyk M, Krzych ŁJ. Haemogram-derived indices for screening and prognostication in critically ill septic shock patients: a case-control study. Diagnostics. 2020;10(9). https://doi.org/10.3390/diagnostics10090638.
Gameiro J, Fonseca JA, Jorge S, Gouveia J, Lopes JA. Neutrophil, lymphocyte and platelet ratio as a predictor of mortality in septic-acute kidney injury patients. Nefrologia. 2020;40(4):461–8. https://doi.org/10.1016/j.nefro.2019.11.006.
Liu D, Yu Z, Zhang D, Zhang J, Zhang Y, Wang X. Value of neutrophil to lymphocytes and platelets ratio for predicting 28-day mortality in sepsis patients. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2021;33(1):33–7. https://doi.org/10.3760/cma.j.cn121430-20200727-00545.
Acknowledgements
None.
Funding
This research was supported by Post-doctoral Innovative Talent Support Program of Shandong Province (grant number SDBX2022020), Shandong Provincial Natural Science Foundation (grant number ZR2023QH382), and Postdoctoral Program of Affiliated Hospital of Jining Medical University (grant number JYFY321211).
Author information
Authors and Affiliations
Contributions
HBW and XYR conceptualized and designed the study. HBW and YHW supervised the data collection, reviewed the analyses and wrote all versions of the manuscript. CG, YYW and CSL performed the imaging examinations and measurements. HBW, CG, YYW, CSL, YHW and XYR collected the data, performed the analysis, and interpreted the results. All authors reviewed and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was performed according to the guidelines of the Helsinki Declaration and was approved by the Ethics Committees of Shenzhen Children’s Hospital. Because this study was retrospective and did not affect clinical decision-making, the informed consent was waived by the ethics committee. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, H., Guo, C., Wang, Y. et al. Immune cell composition and its impact on prognosis in children with sepsis. BMC Pediatr 24, 611 (2024). https://doi.org/10.1186/s12887-024-05087-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-024-05087-1