Abstract
Objective
This scoping review sought to investigate the association between pregnancy-related complications and post-traumatic stress disorder (PTSD) among postpartum women, then summarize effective psychological interventions for pregnancy-related PTSD or sub-PTSD.
Method
Publications in English and Chinese were searched in PubMed, Embase, Cochrane, ISI Web of Science, China National Knowledge Infrastructure (CNKI), and WanFang databases using the subject headings of “Stress Disorders, Post-Traumatic”, “Pregnant Women”, and “psychotherapy”. To ensure that as many relevant studies are incorporated as possible, free terms such as prenatal, postnatal, perinatal and gestation were also used. Intervention studies and related cases published by July 1st, 2023, were also searched.
Results
Twenty-one articles (including 3,901 mothers) were included in this review. Evidence showed that typical psychological interventions exhibited great effect, and family support programs, peer support, online yoga, and music therapy were also effective in reducing risk and improving the psychological well-being of the studied population.
Conclusion
Fetal abnormalities, miscarriage, premature birth, infants with low birth weights, hypertension, pre-eclampsia, HELLP syndrome, and hyperemesis gravidarum are associated with an increased risk of PTSD. Moreover, high-risk pregnant women may benefit from psychological interventions such as cognitive behavioral therapy (CBT). It may also be feasible and well-accepted for music therapy and exposure therapy to lessen the intensity of PTSD in mothers.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
According to the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5), post-traumatic stress disorder (PTSD) is a psychiatric disorder that may occur in people who have experienced or witnessed a traumatic event, series of events or set of circumstances. It is commonly known that there are differences between genders in PTSD, with women suffering at a 2:1 ratio[1]. According to previous studies, pregnancy is recognized as a special period of immunological and physiological change [2], and it is also a period when the chance of PTSD increases and reaches a peak right before labor [3]. Approximately one-third of women in the general population have experienced a traumatic birth, and 3–6% of all postpartum women are diagnosed with PTSD. Furthermore, the prevalence of PTSD in high-risk groups is as high as 18.9%, but many of them remain undiagnosed [4, 5]. PTSD symptoms can affect mother–child interaction and may be responsible for the mothers’ social isolation [6, 7].
Pregnancy-related complications include physical and mental conditions that affect the health of pregnant or postpartum women and/or their babies. Physical and mental conditions that can lead to complications may start before, during, or after pregnancy [8]. Common complications include gestational hypertension, diabetes, nausea, vomiting and anemia, and serious complications include miscarriage, premature birth, premature rupture of membranes, stillbirth, low birth weight, birth defects, and infant and maternal morbidity or death [8]. Severe pregnancy-related complications such as pre-eclampsia (PE), HELLP syndrome, and hyperemesis gravidarum (HG) may increase the risk of PTSD and physical consequences. In the first trimester, pregnant women who experience miscarriage, stillbirth, and fetal abnormalities are found more likely to have emotional consequences such as depression, anxiety, and distress, which, however, are often overlooked [9]. In the second and third trimesters, pregnant women may face preterm birth, premature rupture of membranes, babies with very low birth weights, and others. Pregnancy-related complications have been found associated with PTSD as well as other injuries. In addition to raising the incidence of maternal PTSD, PE may also be linked to brain damage that impairs memory, and women with PE may frequently experience cognitive dysfunction [10, 11]. Nausea and vomiting during pregnancy can be persistent in 2% of pregnant women and worsen to develop into HG [12]. Post-traumatic stress (PTS) symptoms are common after HG [13]and may have long-term implications on a mother’s mental health. Symptoms of depression, anxiety, and PTSD may still be present through years after HG [14]. Among women who had experienced miscarriage, 28% may develop PTSD at 1 month after miscarriage, 0.6–5% may develop PTSD at 3 months after miscarriage, and 18% may develop PTSD at 9 months after miscarriage [15]. It was also found that approximately 50% of women who experienced abortion became pregnant again within 12 months after their abortion [16]; however, a prior abortion is also found to be a risk factor for anxiety, depression and PTS during subsequent pregnancies within one year [16]. Moreover, prior abortions have also been found associated with poor neuropsychiatric outcomes in offspring [17,18,19].
Early psychological intervention may help buffer parental influence on child outcomes [20], and it also plays a crucial role in reducing postpartum morbidity [21]. Early psychological intervention involves psychological, physical, and drug therapies. However, with regard to pharmacotherapy, doctors may hesitate to prescribe psychotropic medications due to potential side effects on mothers and their babies. There is also evidence that pregnant women prefer psychotherapy to pharmacotherapy or other types of psychiatric intervention [22]. Recurrent exposure to trauma may further sensitize underlying and latent illnesses, therefore, early psychological intervention may help avoid the buildup of unprocessed traumatic memories [23]. The National Institute for Health and Care Excellence (NICE) recommends that trauma-focused cognitive behavioral therapy (CBT) and extended exposure treatments be initiated within four weeks after the occurrence of traumatic events. For patients whose traumatic experience happened four weeks prior, eye movement desensitization and reprocessing (EMDR) is also a good option [24]. Previous studies have suggested that a variety of psychological interventions might be effective in perinatal pregnant women with PTSD, however, no conclusion has been reached regarding the effectiveness of different psychological interventions on this special population. Therefore, we conducted this scoping review to summarize the effective psychological interventions for patients with maternal PTSD resulting from pregnancy-related complications.
Methods
Research question/objective
Question 1. What are the main pregnancy-related complications that may precipitate PTSD or sub-clinical PTSD in affected mothers?
Question 2. What psychological interventions can be implemented for mothers experiencing PTSD or sub-clinical PTSD resulting from pregnancy-related complications?
Question 3. What is the efficacy of these psychological interventions in mitigating PTSD or sub-clinical PTSD among mothers affected by pregnancy-related complications?
Search strategy
Publications were searched in PubMed, Embase, Cochrane, Web of Science, CNKI, and WanFang databases, and only those published in English and Chinese were included in this study. See Supplementary Table 1 for details. We listed the keywords based on the topic of the study before literature search and then consulted a panel of professionals to finalize the keywords used in this scoping review. The following medical subject headings and terms (MESH) were used: “stress disorders, post-traumatic”, “pregnant women”, “psychotherapy”, “psychotherap*”, and “behavior therapy”; the terms “maternity,” “prenatal,” “postpartum,” and “perinatal” were also used. All the articles that had been retrieved were then screened according to the inclusion and exclusion criteria.
Selection of studies
Selection criteria
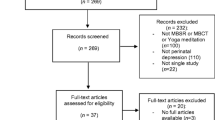
Studies that met the following criteria were included: (1) randomized controlled trials (RCTs), before-after (B-A) studies, prospective cohort studies, cross-sectional studies, and case reports published between January 1, 1996 and July 1, 2023; (2) studies involving women with PTSD caused by pregnancy-related complications; (3) received one or more psychological interventions to prevent and/or treat PTSD resulting from pregnancy-related complications; (4) PTSD or sub-PTSD is diagnosed by using a confirmed and standardized self-report or diagnostic interview as regulated by the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; 1995; or DSM-V, 2013, APA 2018) or the International Classification of Diseases (ICD-9, ICD-10 or ICD-11, WHO 1993, 2022); (5) publications in English or Chinese. Studies with insufficient information, articles published in other languages, case reports, conference abstracts, and studies on PTSD due to non-pregnancy related complications were excluded. The process of study selection is presented in a PRISMA flow diagram (Fig. 1) [25].
Screening process
The screening process consisted of three steps. First, studies were imported into the Rayyan web application (https://www.rayyan.ai/) for duplicate removal and screening. Second, following the inclusion and exclusion criteria, two reviewers (ZP and LZ) in the evidence review group screened the retrieved articles independently based on titles, abstracts, and then full texts. A third reviewer (JL) would be involved to resolve any disagreement through discussion or consultation. A total of 688 records were identified from the six databases. One hundred and fifty-two publications were removed as duplicate records, and 82 were removed due to irrelevance. Four hundred and twenty-six studies were excluded for not meeting the requirements (n = 134 for irrelevance, n = 58 for reviews and systematic reviews, n = 26 for incomplete information and conference articles, n = 198 for studies involving PTSD for non-pregnancy reasons, and n = 10 for articles published in other languages). We further evaluated the remaining 28 publications: 7 articles were excluded for not meeting the inclusion criteria (n = 1 for data duplication and n = 5 for missing key indicators) and one article was excluded for irrelevance. Finally, 21 publications were included in this scoping review.
Data collection
Data were extracted by two reviewers (ZP and LZ) using the established data extraction forms. The following data were collected: (a) authorship and publication year; (b) study design; (c) country; (d) number of participants; (e) pregnancy-related complications; (f) the questionnaire and timing of PTSD assessments; (g) type and time of interventions, and (h) severity of PTSD (Table 1). A meta-analysis of the included studies was not practical due to the heterogeneity of the patients and procedures (therapies, PTSD questionnaires, and timing of interventions and assessments).
Assessments of risk of bias
The criteria listed in the Cochrane Handbook for Systematic Reviews of Interventions were used to determine the risk of bias. For all the studies included, biases were rated as high, unsure, or low through discussion with the review panel (Figs. 2 and 3). The possibility of biased judgments was considered when evaluating the overall effectiveness of the treatments.
The criteria from the National Institutes of Health (NIH) Quality Assessment Tools for before-after (pre-post), observational cohort, cross-sectional, and case series studies with no control groups (available online at https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools) were used to evaluate the quality of the included studies. It contains 9–14 items with response options of “yes”, “no”, “cannot determine”, “not applicable”, and “not reported”, with the objective of directing reviewers’ attention to the essential ideas for assessing the study’s internal validity. Responses to the signaling questions and the relevance assigned to the major ideas represented in the signaling questions were used to determine the quality of the studies (available online at https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools).
Results
Overview of included studies
A total of 21 studies were included. There are ten RCT studies, three before-after studies, two cross-sectional studies, two prospective studies, three clinical studies, and one case report. Pregnancy-related complications included gestational hypertension (k = 1), pre-eclampsia and HELLP syndrome (k = 3), hyperemesis gravidarum (k = 1), fetal abnormalities (k = 10), and premature birth (k = 7). The conclusions of the studies are shown in Table 1.
Intervention
Cognitive Behavioral Therapy (CBT)
CBT is a first-line treatment for PTSD in adults and children. Among interventions for baby loss, short-term Internet-based CBT was found effective [26]. Furthermore, CBT can bring both short- and long-term influence. According to Koochaki et al., CBT has an outstanding effect on preterm mothers immediately and at 3 weeks after intervention, as compared to the control group.
Trauma-focused CBT (TF-CBT)
Trauma-focused CBT is an integrated CBT program that is strongly recommended by guidelines. Shaw et al. [27, 28] conducted two experiments on TF-CBT interventions for preterm mothers. The study using group TF-CBT, which involved one or two 90-min sessions per week for 3–6 weeks [27], revealed that individual intervention was more effective than group intervention in reducing symptoms. Furthermore, the results immediately after treatment and through the 6-month follow-up showed that participants in the group intervention had significant improvement in trauma symptoms, as compared to those receiving individual TF-CBT in their prior study. In another study combining TF-CBT with techniques developed to help increase parenting confidence and change negative parental perceptions of preterm infants, participants who received the intervention scored remarkably lower on the (Davidson Trauma Scale) DTS, as compared to participants in the control group [28]. Similarly, Simon et al. [29] found that the mean trauma score of participants was marginally below the PTSD cut-off level before follow-up and significantly below the cut-off level at the end of the 6-month follow-up. Interestingly, no significant change in trauma symptoms was found from baseline to 6 weeks after intervention, but significant improvement in symptoms was found at 6 months of follow-up compared to baseline and 6 weeks of follow-up.
Internet-based Cognitive Behavioral Therapy (iCBT)
Internet-based cognitive behavioral therapy consists of three phases. The first phase is self-confrontation, in which the traumatic loss and its circumstances are described, the second phase is cognitive reorganization, which aims to provide a new perspective on the loss, and the third phase is social sharing, which focuses on a symbolic farewell letter to the participants themselves, people involved in the loss, or their loved ones. Each writing session lasts for 45 min and is scheduled on a regular basis. In each session, the therapist provides feedback to individuals as well as instructions for the next writing task. Kersting et al. [26, 30] conducted studies on two iCBT interventions on people with miscarriage, termination of pregnancy due to fetal abnormalities, or stillbirth, which showed that the treatment group had significant improvement compared to the control group and that the improvement persisted through 3 months of follow-up. For participants receiving other interventions, 77.3% with a baseline diagnosis of PTSD improved and no longer met the diagnostic criteria for PTSD, while the percentage was only 31.7% for participants who did not receive the intervention.
Eye Movement Desensitization Reprocessing (EMDR)
EMDR improves patients’ symptoms using a series of eye movements at different times in sequence. By linking the patients’ traumatic memories to bilateral alternating stimuli, EMDR can help change the cognitive processes of memory, thereby relieving trauma-related distress. Appelman-Dijkstra [31] reported a 34-year-old woman with a history of hyperparathyroidism and gestational hypercalcemia who was diagnosed with hyperemesis gravidarum at 2 weeks of gestation, HELLP syndrome at 38 weeks, and PTS symptoms after delivery, which improved after EMDR intervention. Similar conclusions were reached by Stramrood [32], who reported a patient diagnosed with pre-eclampsia at 1 week after her first delivery and postpartum hemorrhage after her second delivery; the patient’s PTS symptoms improved significantly after four EMDR sessions.
Written exposure therapy
Expressive writing is based on inhibition theory, which links traumatic events to positive health outcomes. In this therapy, individuals are asked to write down their deepest thoughts and feelings from a painful or traumatic event they encountered. Generally, the writing session lasts for 15 min, is performed in a private space, and is scheduled for three consecutive days, with no feedback provided. Using a sample of preterm women, Horsch et al. [33], found a marked decrease in PTSD symptoms in the intervention group after 3 and 4 months of intervention, as compared to the control group, who only showed decreasing symptoms between 3 and 6 months after intervention. Taken together, evidence has shown that expressive writing is a simple, easily accessible, and cost-effective therapy that reduces maternal post-traumatic and depressive symptoms and improves the mental health of preterm infants after birth.
Acceptance and Commitment Therapy (ACT)
ACT is an acceptation-based intervention usually consisting of seven modules and lasting for 7 days. The modules include short readings explaining concepts of ACT, often using metaphors, and one to two exercises such as driving your life bus and loving mercy meditation. Through a study on women with PPROM, Tunnell et al. [34] found that those who participated in ACT had no deterioration, as assessed using PCL-5 (PTSD Checklist for DSM-5). Despite the limitations of this study, ACT has been widely accepted regarding its feasibility and acceptability as a transaction-based ACT.
Psychological grief counseling
Psychological grief counseling includes the understanding of stages of grief and the grief cycle, exposure to negative thoughts and practice of recovery writing, the thought-emotion cycle (involving cognitive reorganization and searching for meaning), and the practice of coping skills. It has shown a significant positive effect on reducing the severity of grief symptoms. Navidian et al. [35] found that for women with stillbirths, those who received psychological grief counseling had greater improvement in PTS symptoms than the control group.
Early intervention programs
The early intervention program consists of three main aspects, i.e., parental support, parent–child relationship support, and infant development support. In a study on women with preterm birth, Borghini et al. [36] conducted an early intervention program, which was based on a treatment model involving the conversion from a family system theory into a transactional preventive intervention; the program included three phases and was scheduled at 33 weeks and 42 weeks after conception as well as 4 months after the theoretical term of 40 weeks after conception (i.e., corrected age). In this program, parents were encouraged to comment on their babies’ behavior and their own emotions and participate in a 10-min mother-infant interactive game; the whole process was recorded for the instructor to provide feedback. Each session lasted 40–60 min and was designed to improve the quality of maternal care and sensitivity to the infant by providing directions on observing the infant’s responses, needs, abilities, and weaknesses. The study found that the PTSD symptoms of mothers of preterm infants were significantly more severe than those of mothers of full-term infants, and the difference persisted through 12 months after the birth of their children.
Family support program
The family support program focuses on emotions through real-time online counselling. In this program, the family function is evaluated after admission, and the family support plan is then formulated after communication with the patients and their families regarding the psychological characteristics of the pregnant women. Sun et al. [37] found that the family support program could improve PTSD symptoms in perinatal women, and another study of this group [38] indicated that the PTSD and hyperarousal symptoms of the participants who received family support intervention were significantly relieved, compared to those in the control group treated with routine care. In a study, Wang et al. [39] combined empathy nursing (focusing on active listening, understanding, respect, and acceptance) with a family support plan, which exhibited remarkable effects on pregnant women with fetal abnormalities. Sun et al. and Wu et al. [37, 40] conducted a family empowerment educational intervention for women with preeclampsia, which showed that the PCL-C (PTSD Checklist-Civilian Version) score of the participants was significantly reduced after intervention. Moreover, the severity of PTSD in patients with preeclampsia is closely related to family support. Dong et al. [41] found that the post-traumatic separation, depression and anxiety, and bereavement of patients were significantly reduced at 7 weeks after labor compared to 4 weeks after labor.
Peer support
The peer support group is usually formed by pregnant women admitted to hospital for labor. Zhang et al. [42] found that peer support could effectively reduce PTSD symptoms in pregnant women with fetal abnormalities, and the symptoms of intrusion and hyperarousal were also improved after intervention, However, the participants’ avoidance failed to improve significantly.
Mindfulness yoga
Yoga can help individuals maintain focused and calm and is suitable for women who refuse to take medications during pregnancy. For women who have experienced a stillbirth, yoga is an effective approach to reduce their mental and physical stress [43, 44]. Yoga can also improve sleep quality, reduce rumination and hyperarousal, and improve the ability to fall asleep and maintain sleep [45,46,47]. Using an online yoga intervention (60 min/week, 12 weeks) for women who had a stillbirth in the past 24 months, Huberty et al. found that PTS symptoms and associated sleep disturbances significantly improved [43].
Music therapy
Music therapy mainly involves listening to music, singing, or playing musical instruments. Kobus et al. [48] found that the perceived distress of preterm birth (measured by Impact of Event Scale-Revised score) was significantly decreased in participants who received music therapy, as compared to the control group; music therapy could also improve hyperarousal symptoms effectively.
Risk of bias
Data on the risk of bias for the included RCTs are shown in Figs. 2 and 3. All included studies were deemed to have a low risk of bias due to allocation concealment and low risk of bias in the selection of the reported outcome. The overall risk of bias was low for two of the 12 RCTs (studies 12, 20). Convenience sampling was used in three studies (studies 11, 13, 21), and six studies (studies 8, 11, 12, 14, 18, 21) had insufficient details about how the random sequence was generated. In the study by Zhang et al. (study 6), the trial design, by which participants were assigned to different groups based on their maternity unit rather than using a random numerical table, might have led to a higher risk of selection bias. A higher risk of follow-up bias was found in studies by Borghini and Kobus et al. In the study of Borghini et al. (study 15), the non-intervention group lacked follow-up data at 4 months, and in the study of Kobus et al. (study 18), up to 24% of participants dropped out during the course of the study. It should be noted that in the study of Kersting et al. (study 9), most of the participants were well-educated and did well in expressive writing; however, the result might be different for people with lower levels of education.
Information about the risk of bias in the three B-A studies (studies 2, 7, 17) is presented in Table 2. As we could not confirm that all subjects who met the entry requirements were enrolled, the sample size was insufficient to produce reliable results (studies 2, 17), and as the outcome measures were not evaluated before and after intervention, all the B-A studies were regarded as having a high risk of bias. The risk of bias for the observational cohort (study 5), cross-sectional (studies 1, 10) and case series (studies 3–4) studies is presented in Table 3 and Table 4.
Discussion
Pregnancy-related complications have been recognized as traumatic events that can result in PTSD, it has become a concern for clinicians.
Hypertensive Disorders of Pregnancy (HDP)
HDP mainly manifests as hypertension, edema, proteinuria, etc. In severe cases, patients can also experience nausea, vomiting, headache, convulsion, coma, and other symptoms, which is an important cause of maternal and fetal death [49]. Wang et al. found that the positive rate of PTSD in women with HDP was 13.04% as assessed using PCL-C. The incidence of postpartum depression, anxiety, and PTSD in women with HDP is also found higher than that in women without HDP. Women with a history of HDP are more likely to develop PTSD compared to those with normal labor, and the severity of HDP may be correlated with the seriousness of the symptoms [50]. However, a shortcoming is the absence of psychological interventions specifically for PTSD patients afflicted with HDP.
Pre-eclampsia (PE)
PE is a multisystem disorder of pregnancy characterized by concurrent hypertension (occurring after 20 weeks of gestation), proteinuria, and associated organ dysfunction [51]. Meanwhile, it is one of the major causes of maternal and perinatal mortality [52]. A large number of women who have experienced PE report their labor as a traumatic event [53]. Wu et al. [40] found that PTSD symptoms were significantly more severe at 1 day after childbirth than at admission among women with PE. It has been found that the prevalence of PTSD in women with PE ranges from 44 to 4% at 6 weeks to 5 years postpartum [54]. Moreover, compared to women with mild PE, those with severe PE are more likely to have PTSD, with a prevalence of 11% [55]. Stramrood et al. [32] reported that a 25-year-old woman with postpartum eclampsia who was diagnosed 1 week after her first delivery was found to have typical symptoms of PTSD, such as flashbacks of postpartum hospitalization, avoiding activities, places, and conversations related to childbirth. It was also found that PTSD symptoms were more severe in patients with PE than in those with HDP [50]. The most common symptom of PTSD was decrease in interest, which is present in approximately 56% of all cases [56].
HELLP syndrome
HELLP syndrome is usually defined as a severe form of PE and is also known as “atypical pre-eclampsia”. It is characterized by hemolysis, microangiopathic hemolytic anemia, elevated liver enzymes, and low platelet levels. Many studies have found that the incidence of mental health problems has increased in patients with PE/HELLP. In a study by Poel et al. [57], among the Caucasian primiparas with PE, eclampsia, and/or hemolysis, and HELLP syndrome, 5 subjects were diagnosed with PTSD, 15 reported hyperarousal symptoms, 10 reported anxiety and feelings of tension, and 9 reported re-experience of their problems/symptoms. Patients diagnosed with PE or HELLP syndrome who developed PTSD or PTSS were treated with distinct psychological interventions, including family-involved empowerment education and EMDR therapy. Patients with PTSD showed varying degrees of improvement when treated with different interventions.
Hyperemesis Gravidarum (HG)
HG refers to serious and persistent nausea and vomiting in early pregnancy, causing dehydration, ketosis, and even acidosis, which may require hospitalization. Kjeldgaard et al. [58] found that HG can also be a traumatic experience. Women with HG score had higher IES-R score at 8 weeks and 2 years postpartum than women with no, mild, or severe nausea. Women with HG are also at a higher risk of PTSD than those with premature childbirth. Unfortunately, studies on psychotherapy that aimed to effectively manage PTSD resulting from HG are still insufficient.
Fetal abnormalities and miscarriage
Fetal abnormalities include congenital malformations (birth defects) and stillbirths, which often require hospitalization for induction of labor. The sudden occurrence of such events may bring unimaginable pain to the pregnant woman physically and mentally as well as potential psychological trauma through years after the events. Several studies have found the baseline IES-R score of pregnant women with fetal abnormalities is generally above 19, suggesting that this population needs increasing clinical attention [37, 38, 42]. Compared to women giving birth to a live infant, those with stillbirths were found to have a 12-fold increased risk for PTSD [59], indicating that stillbirths can be traumatic events. It has also been reported the strong symptoms of sadness, poor coping, hopelessness, worthlessness, isolation, and guilt may persist for up to 10 years after the stillbirth [33]. The study by Huberty et al. [60] has shed more light on women who experienced stillbirth; it showed that the majority of participants (n = 38) reported high levels of PTSD symptoms (IES-R ≥ 35). This result is also supported by the findings of Navidian et al. [35]. A study found that among patients who experienced late fetal death, the prevalence of PTSD ranged from 0.6% to 39% [61]. Furthermore, evidence suggests that miscarriage can increase the risk of PTSD among pregnant women [26, 30, 39]. A study found that 44.7% of the subjects [62] were at a greater risk of PTS after miscarriage. Women who experienced induced labor after an adverse pregnancy are found more likely to develop dissociative symptoms, with 20% of women in the study showing acute stress symptoms [41]. Studies using the IES-R scale to measure the risk of PTSD showed that women with fetal abnormalities and miscarriages scored significantly higher, generally above 30 (with critical values set at 22 to 40). Most therapies for fetal abnormalities and mortal abortions are based on CBT, and 44% (4/9) of the trials included in the present study are Internet-based. This might be related to participants’ reluctance to receive in-person treatment due to their concerns about confidentiality or other people’s opinions on their help-seeking [63]. Internet-based psychotherapy allows more privacy and flexibility as well as avoids high costs and geographical limitations. For instance, participants in iCBT sessions can use the material at any time based on their progress, which is deemed as an advantage over traditional face-to-face CBT [64]. One-third of the studies included in the present review used family support therapy, highlighting the significant link between post-partum family support and PTSD [65]. Due to its organized structure and focus on problem-solving, family support therapy can help individuals make better decisions and reduce negative perceptions of stressful events, thereby improving their symptoms of PTSD [66].
Preterm, low birth-weight infants
Preterm birth can be a traumatic event for parents [67], and it may also impact mother-infant attachment and infant development [68]. Studies have found that parents can experience significant stress and even PTSD symptoms when their infants have to be separated from them and admitted to the NICU, as they worry that preterm birth will cause sequelae or even death to their infants [36]. Among the nine studies on preterm birth included in the present review, Borghini et al. [36] found that mothers of preterm infants (gestation age < 33 weeks) had significantly more severe PTSD symptoms than mothers of full-term infants. Preterm birth is often associated with low birth weight, both of which can bring traumatic effects and increased risk of PTSD to pregnant women [69]. Shaw et al. [27, 28] found that mothers of preterm infants (gestational age of 25–34 weeks; > 600 g) scored higher on scales of PTSD, and 90.3% of them were positive for acute stress reaction symptoms. Simon et al. [29] revealed that the mean trauma score of mothers of preterm infants (23–34 weeks of gestational age) at baseline was above the recommended clinical cut-off score for PTSD.
Studies on CBT have shown that this therapy could significantly reduce the severity of anxiety and PTSD in mothers of premature infants [70]. Furthermore, it can also reduce the symptoms of insomnia and depression as well as the risk of premature birth [71]. A study using group CBT showed a significant decrease in the severity of PTSD in participants after six months of intervention, with an average reduction of 22.26 points on the DTS scale. Studies have also found that therapies delivered in a time-limited, highly organized group style may bring persistent psychological benefits. Compared to individual TF-CBT, mothers participating in group CBT are more likely to feel more secure and supported and are more willing to share their experiences. Group CBT can also reduce the strain on mental health workers in the NICU setting. However, through the comparison of two studies, Shaw et al. suggested that both individual and group TF-CBT could significantly improve traumatic symptoms, but individual treatment showed a better effect.
For women who had experienced early childbirth, music therapy and expressive writing have been shown helpful. According to Kobus et al., music therapy showed a significantly better effect than conventional stress-reduction measures in the NICU for treating high awareness in preterm women; they also noticed that music therapy could be an additional stress-reducing approach in the NICU. The findings of Carr et al. revealed clinically significant improvement in the main symptoms of PTSD after music therapy, especially avoidance [72]. Another study found that music therapy performed by parents themselves could improve psychological outcomes [73]. Expressive writing is also helpful for mental health improvement, emotional ventilation, and rationalization of thoughts around abortion [44]. A study found that the subjects’ PTSD symptoms were significantly relieved through 3 to 4 months after they participated in expressive writing sessions. This is also supported by the study of Blasio et al., which found that subjects receiving expressive writing intervention for three months exhibited significantly decreased depression and posttraumatic symptoms [74].
Strengths and limitations
To our knowledge, the present review is the first one to address the impact of pregnancy-related complications on maternal PTSD. Furthermore, the thorough search of databases has also allowed for comprehensive analysis of different interventions and different populations.
Overall, the quality of the involved studies was mixed, particularly in terms of study design and measurement of exposure and outcome data. As different studies involved participants in different stages of their perinatal period and participants with different PTSD-related diagnoses, the studied population of this review can be heterogeneous. Furthermore, as the effect of intervention was not assessed in some studies (studies 3, 10) and the sample size was small for some studies (studies 3, 4, 6, 11, 17–19), our results might not be generalizable to other populations. Moreover, PTSD symptoms were evaluated using self-reported questionnaires (studies 1–2, 5–13, 15–21) in most studies, which might have reduced the accuracy of our findings due to participants’ propensity to provide socially acceptable answers. The tools used to assess or diagnose PTSD also varied across studies, which might have affected the accuracy of our results. The lack of long-term follow-up may be another limitation. Among all the included studies, only 3 trials (studies 5,9,15) included a post-intervention assessment at 12 or 24 months. As the B-A studies (studies 2, 7, 17, 19) do not have a control group, they could not determine whether the improvement in symptoms was caused by the intervention or other factors such as the normal healing process [29]. Articles published in languages other than English and Chinese might have been overlooked as we restricted the scope of this study to articles published in English and Chinese. In general, more RCTs are still needed to investigate the association between maternal PTSD and pregnancy problems.
Conclusion
In this scoping review, we evaluated studies on the effects of pregnancy-related complications on PTSD in women in the perinatal period and summarized the effective psychological treatment options. According to our analysis, a variety of pregnancy-related complications have been recognized as traumatic events that can cause short- or long-term consequences for women in the perinatal period. Therefore, more attention should be given to the mental health of this special population. More studies, especially high-quality RCTs, are still warranted to confirm the effects of different interventions on women with different pregnancy complications, as this may help maximize the effects, acceptability, and feasibility of the interventions.
Availability of data and materials
No datasets were generated or analysed during the current study.
References
Christiansen DM, Berke ET. Gender- and Sex-Based Contributors to Sex Differences in PTSD. Curr Psychiatry Rep. 2020;22(4):19. https://doi.org/10.1007/s11920-020-1140-y.
Wang Y, Chen L, Wu T, et al. Impact of Covid-19 in pregnancy on mother’s psychological status and infant’s neurobehavioral development: a longitudinal cohort study in China. BMC Med. 2020;18(1):347. https://doi.org/10.1186/s12916-020-01825-1.
Onoye JM, Shafer LA, Goebert DA, Morland LA, Matsu CR, Hamagami F. Changes in PTSD symptomatology and mental health during pregnancy and postpartum. Arch Womens Ment Health. 2013;16(6):453–63. https://doi.org/10.1007/s00737-013-0365-8.
Yildiz PD, Ayers S, Phillips L. The prevalence of posttraumatic stress disorder in pregnancy and after birth: A systematic review and meta-analysis. J Affect Disord. 2017;208:634–45. https://doi.org/10.1016/j.jad.2016.10.009.
Slade P, Murphy A, Hayden E. Identifying post-traumatic stress disorder after childbirth. BMJ. 2022;377:e067659. Published 2022 May 10. https://doi.org/10.1136/bmj-2021-067659
Beck CT. Birth trauma: in the eye of the beholder. Nurs Res. 2004;53(1):28–35. https://doi.org/10.1097/00006199-200401000-00005.
Ertan D, Hingray C, Burlacu E, Sterlé A, El-Hage W. Post-traumatic stress disorder following childbirth. BMC Psychiatry. 2021;21:155. https://doi.org/10.1186/s12888-021-03158-6.
Centers for Disease Control and Prevention: Pregnancy Complications. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pregnancy-complications.html (2023). Accessed 7 Sept 2023.
Lee C, Slade P. Miscarriage as a traumatic event: a review of the literature and new implications for intervention. J Psychosom Res. 1996;40(3):235–44. https://doi.org/10.1016/0022-3999(95)00579-x.
Brussé I, Duvekot J, Jongerling J, Steegers E, De Koning I. Impaired maternal cognitive functioning after pregnancies complicated by severe pre-eclampsia: a pilot case-control study. Acta Obstet Gynecol Scand. 2008;87(4):408–12. https://doi.org/10.1080/00016340801915127.
Baecke M, Spaanderman MEA, van der Werf SP. Cognitive function after pre-eclampsia: an explorative study. J Psychosom Obstet Gynecol. 2009;30(1):58–64. https://doi.org/10.1080/01674820802546212.
Lowe SA, Steinweg KE. Review article: Management of hyperemesis gravidarum and nausea and vomiting in pregnancy. Emerg Med Australas. 2022;34(1):9–15. https://doi.org/10.1111/1742-6723.13909.
Mullin P, Ching C, Shoenberg F, et al. Risk factors, treatments, and outcomes associated with prolonged hyperemesis gravidarum. J Matern Fetal Neonatal Med. 2012;25(6):632–6. https://doi.org/10.3109/14767058.2011.598588.
Nijsten K, van der Minnen LM, Dean C, et al. Depression, anxiety, and post-traumatic stress disorder symptoms after hyperemesis gravidarum: a prospective cohort study. J Matern Fetal Neonatal Med. 2022;35(25):10055–63. https://doi.org/10.1080/14767058.2022.2089550.
Jia L, Li W, Liu Y, Wang L. Psychologic Sequelae in Early Pregnancy Complications. IJWH. 2023;15:51–7. https://doi.org/10.2147/IJWH.S382677.
Forray A, Mayes LC, Magriples U, Epperson CN. Prevalence of post-traumatic stress disorder in pregnant women with prior pregnancy complications. J Matern Fetal Neonatal Med. 2009;22(6):522–7. https://doi.org/10.1080/14767050902801686.
Dubowitz H, Black MM, Kerr MA, et al. Type and timing of mothers’ victimization: effects on mothers and children. Pediatrics. 2001;107(4):728–35. https://doi.org/10.1542/peds.107.4.728.
Miranda JK, de la Osa N, Granero R, Ezpeleta L. Maternal experiences of childhood abuse and intimate partner violence: Psychopathology and functional impairment in clinical children and adolescents. Child Abuse Negl. 2011;35(9):700–11. https://doi.org/10.1016/j.chiabu.2011.05.008.
Yehuda R, Daskalakis NP, Bierer LM, et al. Holocaust Exposure Induced Intergenerational Effects on FKBP5 Methylation. Biol Psychiatry. 2016;80(5):372–80. https://doi.org/10.1016/j.biopsych.2015.08.005.
Ribaudo J, Lawler JM, Jester JM, et al. Maternal History of Adverse Experiences and Posttraumatic Stress Disorder Symptoms Impact Toddlers’ Early Socioemotional Wellbeing: The Benefits of Infant Mental Health-Home Visiting. Front Psychol. 2021;12: 792989. https://doi.org/10.3389/fpsyg.2021.792989.
Geller PA, Stasko EC. Effect of Previous Posttraumatic Stress in the Perinatal Period. J Obstet Gynecol Neonatal Nurs. 2017;46(6):912–22. https://doi.org/10.1016/j.jogn.2017.04.136.
Bacaro V, Benz F, Pappaccogli A, et al. Interventions for sleep problems during pregnancy: A systematic review. Sleep Med Rev. 2020;50: 101234. https://doi.org/10.1016/j.smrv.2019.101234.
Taylor Miller PG, Sinclair M, Gillen P, et al. Early psychological interventions for prevention and treatment of post-traumatic stress disorder (PTSD) and post-traumatic stress symptoms in post-partum women: A systematic review and meta-analysis. PLoS ONE. 2021;16(11): e0258170. https://doi.org/10.1371/journal.pone.0258170.
NICE: Post-traumatic stress disorder. 2018. https://www.nice.org.uk/guidance/ng116. Accessed 21 Aug 2023.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71. https://doi.org/10.1136/bmj.n71.
Kersting A, Kroker K, Schlicht S, Baust K, Wagner B. Efficacy of cognitive behavioral internet-based therapy in parents after the loss of a child during pregnancy: pilot data from a randomized controlled trial. Arch Womens Ment Health. 2011;14(6):465–77. https://doi.org/10.1007/s00737-011-0240-4.
Shaw RJ, St John N, Lilo E, et al. Prevention of Traumatic Stress in Mothers of Preterms: 6-Month Outcomes. Pediatrics. 2014;134(2):e481–8. https://doi.org/10.1542/peds.2014-0529.
Shaw RJ, Moreyra A, Simon S, et al. Group trauma focused cognitive behavior therapy for parents of premature infants compared to individual therapy intervention. Early Human Dev. 2023;181: 105773. https://doi.org/10.1016/j.earlhumdev.2023.105773.
Simon S, Moreyra A, Wharton E, et al. Prevention of posttraumatic stress disorder in mothers of preterm infants using trauma-focused group therapy: Manual development and evaluation. Early Human Dev. 2021;154: 105282. https://doi.org/10.1016/j.earlhumdev.2020.105282.
Kersting A, Dölemeyer R, Steinig J, et al. Brief Internet-based intervention reduces posttraumatic stress and prolonged grief in parents after the loss of a child during pregnancy: a randomized controlled trial. Psychother Psychosom. 2013;82(6):372–81. https://doi.org/10.1159/000348713.
Appelman-Dijkstra NM, Ertl DA, Zillikens MC, Rjenmark L, Winter EM. Hypercalcemia during pregnancy: management and outcomes for mother and child. Endocrine. 2021;71(3):604–10. https://doi.org/10.1007/s12020-021-02615-2.
Stramrood CAI, van der Velde J, Doornbos B, Marieke Paarlberg K, Weijmar Schultz WCM, van Pampus MG. The patient observer: eye-movement desensitization and reprocessing for the treatment of posttraumatic stress following childbirth. Birth. 2012;39(1):70–6. https://doi.org/10.1111/j.1523-536X.2011.00517.x.
Horsch A, Jacobs I, McKenzie-McHarg K. Cognitive predictors and risk factors of PTSD following stillbirth: a short-term longitudinal study. J Trauma Stress. 2015;28(2):110–7. https://doi.org/10.1002/jts.21997.
Tunnell N, Suterwala M, Meuret A. Brief acceptance-based therapy for women with high-risk pregnancies: Uncontrolled pilot of an intervention for inpatients. J Contextual Behav Sci. 2019;14:127–35. https://doi.org/10.1016/j.jcbs.2019.10.004.
Navidian A, Saravani Z, Shakiba M. Impact of Psychological Grief Counseling on the Severity of Post-Traumatic Stress Symptoms in Mothers after Stillbirths. Issues Ment Health Nurs. 2017;38(8):650–4. https://doi.org/10.1080/01612840.2017.1315623.
Borghini A, Habersaat S, Forcada-Guex M, et al. Effects of an early intervention on maternal post-traumatic stress symptoms and the quality of mother-infant interaction: the case of preterm birth. Infant Behav Dev. 2014;37(4):624–31. https://doi.org/10.1016/j.infbeh.2014.08.003.
Sun S, Li J, Ma Y, Bu H, Luo Q, Yu X. Effects of a family-support programme for pregnant women with foetal abnormalities requiring pregnancy termination: A randomized controlled trial in China. Int J Nurs Pract. 2018;24(1): e12614. https://doi.org/10.1111/ijn.12614.
Sun Shiwen. Family support status and intervention study of pregnant women with fetal abnormality requiring pregnancy termination. Zhejiang University. 2017; https://d.wanfangdata.com.cn/thesis/ChJUaGVzaXNOZXdTMjAyMzAxMTISCFkzMzc2MDE5Ggg5YXJ5M2Q3eQ%3D%3D. (in Chinese)
WANG Jingjing, Huanhuan SI. Impact of empathy combined family support program nursing on maternal mental health with fetal abnormalities. Practical J Med & Pharm. 2020;37(11):1030–3 (in Chinese).
WU Ying. Exploring the relationship between PTSD and family support in patients with preeclampsia. Journal of Aerospace Medicine. J Aerosp Med. 2023;34(4):486–489. (in Chinese)
DONG Ruan-zhen, ZHANG Qian-qian. Effect of adverse pregnancy on maternal mentality and evaluation of psychological intervention. Chinese Rural Health Service Administration. 2018;38(10):1355–1358. (in Chinese)
ZHANG Jieqiong. Implementation and evaluation of the peer support plan for pregnant women with fetal abnormalities. Shihezi University. 2018. https://kns.cnki.net/kcms2/article/abstract?v=3uoqIhG8C475KOm_zrgu4lQARvep2SAkZIGkvqfmUZglMdu7fCR482285FMhO8_MsYcxhPRfQcXnT4Q0mWM4oZMBBmRVaz&uniplatform=NZKPT (in Chinese).
Huberty J, Sullivan M, Green J, et al. Online yoga to reduce post traumatic stress in women who have experienced stillbirth: a randomized control feasibility trial. BMC Complement Med Ther. 2020;20:173. https://doi.org/10.1186/s12906-020-02926-3.
Traylor CS, Johnson JD, Kimmel MC, Manuck TA. Effects of psychological stress on adverse pregnancy outcomes and nonpharmacologic approaches for reduction: an expert review. Am J Obstet Gynecol MFM. 2020;2(4): 100229. https://doi.org/10.1016/j.ajogmf.2020.100229.
Khalsa SBS. Yoga as a therapeutic intervention: a bibliometric analysis of published research studies. Indian J Physiol Pharmacol. 2004;48(3):269–85.
Beddoe AE, Lee KA, Weiss SJ, Kennedy HP, Yang CPP. Effects of mindful yoga on sleep in pregnant women: a pilot study. Biol Res Nurs. 2010;11(4):363–70. https://doi.org/10.1177/1099800409356320.
Halpern J, Cohen M, Kennedy G, Reece J, Cahan C, Baharav A. Yoga for improving sleep quality and quality of life for older adults. Altern Ther Health Med. 2014;20(3):37–46.
Kobus S, Diezel M, Dewan MV, et al. Music Therapy in Preterm Infants Reduces Maternal Distress. IJERPH. 2022;20(1):731. https://doi.org/10.3390/ijerph20010731.
Liming WANG, Huixia WANG, Le YANG. Correlation between social support rating scale score and post - traumatic stress disorder in patients with hypertensive disorders of pregnancy after cesarean section. Henan Medical Research. 2022;31(19):3557–60 (in Chinese).
Roberts L, Davis GK, Homer CSE. Depression, Anxiety, and Post-traumatic Stress Disorder Following a Hypertensive Disorder of Pregnancy: A Narrative Literature Review. Frontiers in Cardiovascular Medicine. 2019. https://www.frontiersin.org/articles/https://doi.org/10.3389/fcvm.2019.00147. Accessed 27 June 2023.
McNestry C, Killeen SL, Crowley RK, McAuliffe FM. Pregnancy complications and later life women’s health. Acta Obstet Gynecol Scand. 2023;102(5):523–31. https://doi.org/10.1111/aogs.14523.
Steegers EAP, von Dadelszen P, Duvekot JJ, Pijnenborg R. Pre-eclampsia Lancet. 2010;376(9741):631–44. https://doi.org/10.1016/S0140-6736(10)60279-6.
Roberts L, Henry A, Harvey SB, Homer CSE, Davis GK. Depression, anxiety and posttraumatic stress disorder six months following preeclampsia and normotensive pregnancy: a P4 study. BMC Pregnancy Childbirth. 2022;22:108. https://doi.org/10.1186/s12884-022-04439-y.
Furuta M, Sandall J, Bick D. A systematic review of the relationship between severe maternal morbidity and post-traumatic stress disorder. BMC Pregnancy Childbirth. 2012;12:125. https://doi.org/10.1186/1471-2393-12-125.
Hoedjes M, Berks D, Vogel I, et al. Symptoms of post-traumatic stress after preeclampsia. J Psychosom Obstet Gynaecol. 2011;32(3):126–34. https://doi.org/10.3109/0167482X.2011.599460.
Engelhard IM, van Rij M, Boullart I, et al. Posttraumatic stress disorder after pre-eclampsia: an exploratory study. Gen Hosp Psychiatry. 2002;24(4):260–4. https://doi.org/10.1016/S0163-8343(02)00189-5.
Poel YHM, Swinkels P, de Vries JIP. Psychological treatment of women with psychological complaints after pre-eclampsia. J Psychosom Obstet Gynaecol. 2009;30(1):65–72. https://doi.org/10.1080/01674820802545990.
Kjeldgaard HK, Vikanes Å, Benth JŠ, Junge C, Garthus-Niegel S, Eberhard-Gran M. The association between the degree of nausea in pregnancy and subsequent posttraumatic stress. Arch Womens Ment Health. 2019;22(4):493–501. https://doi.org/10.1007/s00737-018-0909-z.
Huberty J, Matthews J, Leiferman J, Cacciatore J, Gold KJ. A study protocol of a three-group randomized feasibility trial of an online yoga intervention for mothers after stillbirth (The Mindful Health Study). Pilot Feasibility Stud. 2018;4(1):12. https://doi.org/10.1186/s40814-017-0162-7
Huberty J, Green J, Cacciatore J, Buman MP, Leiferman J. Relationship Between Mindfulness and Posttraumatic Stress in Women Who Experienced Stillbirth. J Obstet Gynecol Neonatal Nurs. 2018;47(6):760–70. https://doi.org/10.1016/j.jogn.2018.09.002.
Abiola L, Legendre G, Spiers A, et al. Late fetal demise, a risk factor for post-traumatic stress disorder. Sci Rep. 2022;12(1):12364. https://doi.org/10.1038/s41598-022-16683-5.
Kukulskienė M, Žemaitienė N. Postnatal Depression and Post-Traumatic Stress Risk Following Miscarriage. Int J Environ Res Public Health. 2022;19(11):6515. https://doi.org/10.3390/ijerph19116515.
Wang Z, Tang S, Wang J, Maercker A. Foundations and future application of internet-based interventions for PTSD in PR China. Int J Electron Healthc. 2012;7(1):19–35. https://doi.org/10.1504/IJEH.2012.048667.
Sjömark J, Parling T, Jonsson M, Larsson M, Skoog SA. A longitudinal, multi-centre, superiority, randomized controlled trial of internet-based cognitive behavioural therapy (iCBT) versus treatment-as-usual (TAU) for negative experiences and posttraumatic stress following childbirth: the JUNO study protocol. BMC Pregnancy Childbirth. 2018;18(1):387. https://doi.org/10.1186/s12884-018-1988-6.
Soltani N, Abedian Z, Mokhber N, Esmaily H. The Association of Family Support After Childbirth With Posttraumatic Stress Disorder in Women With Preeclampsia. Iran Red Crescent Med J. 2015;17(10): e17865. https://doi.org/10.5812/ircmj.17865.
Dai YT. The effects of family support, expectation of filial piety, and stress on health consequences of older adults with diabetes mellitus. 1995. https://digital.lib.washington.edu/researchworks/bitstream/handle/1773/7214/9609623.pdf?sequence=1&isAllowed=y.
Beck CT, Harrison L. Posttraumatic Stress in Mothers Related to Giving Birth Prematurely: A Mixed Research Synthesis. J Am Psychiatr Nurses Assoc. 2017;23(4):241–57. https://doi.org/10.1177/1078390317700979.
Anderson C, Cacola P. Implications of Preterm Birth for Maternal Mental Health and Infant Development. MCN Am J Matern Child Nurs. 2017;42(2):108–14. https://doi.org/10.1097/NMC.0000000000000311.
Koochaki M, Mahmoodi Z, Esmaelzadeh–Saeieh S, Kabir K, Dolatian M. Effects of Cognitive-Behavioral Counseling on Posttraumatic Stress Disorder in Mothers with Infants Hospitalized at Neonatal Intensive Care Units: A Randomized Controlled Trial. Iran J Psychiatry Behav Sci. 2018; In Press. https://doi.org/10.5812/ijpbs.65159
Seiiedi-Biarag L, Mirghafourvand M, Ghanbari-Homayi S. The effect of cognitive-behavioral therapy on psychological distress in the mothers of preterm infants: a systematic review and meta-analysis. J Psychosom Obstet Gynaecol. 2020;41(3):167–76. https://doi.org/10.1080/0167482X.2019.1678019.
MacKinnon AL, Madsen JW, Dhillon A, et al. Sleeping for two: study protocol for a randomized controlled trial of cognitive behavioral therapy for insomnia in pregnant women. Trials. 2021;22(1):532. https://doi.org/10.1186/s13063-021-05498-w.
Carr C, d’Ardenne P, Sloboda A, Scott C, Wang D, Priebe S. Group music therapy for patients with persistent post-traumatic stress disorder – an exploratory randomized controlled trial with mixed methods evaluation. Psychol Psychother Theory Res Pract. 2012;85(2):179–202. https://doi.org/10.1111/j.2044-8341.2011.02026.x.
Ghetti CM, Vederhus BJ, Gaden TS, et al. Longitudinal Study of Music Therapy’s Effectiveness for Premature Infants and Their Caregivers (LongSTEP): Feasibility Study With a Norwegian Cohort. J Music Ther. 2021;58(2):201–40. https://doi.org/10.1093/jmt/thaa023.
Blasio PD, Camisasca E, Caravita SCS, Ionio C, Milani L, Valtolina GG. THE EFFECTS OF EXPRESSIVE WRITING ON POSTPARTUM DEPRESSION AND POSTTRAUMATIC STRESS SYMPTOMS. Psychol Rep. 2015;117(3):856–82. https://doi.org/10.2466/02.13.PR0.117c29z3.
Acknowledgements
Not applicable.
Funding
The study was supported by the grant of National Natural Science Foundation of China (82171518, LZ, PI; 82001437, BL, PI), the Natural Science Foundation of Hunan Province, China (2020JJ5844, LZ, PI), STI2030-Major Projects (2021ZD0200702, JZ, PI), Key research and development plan of Hunan (2023SK2028, JZ, PI).
Author information
Authors and Affiliations
Contributions
Zhuo Peng drafted the manuscript, Li Zhang conceived the article and revised the manuscript, and Lin Liu, Bangshan Liu, Jiansong Zhou and Yan Zhang revised the manuscript. All authors endorsed the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Peng, Z., Liu, J., Liu, B. et al. Psychological interventions to pregnancy-related complications in patients with post-traumatic stress disorder: a scoping review. BMC Psychiatry 24, 478 (2024). https://doi.org/10.1186/s12888-024-05926-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-024-05926-6