Abstract
Background
Socioeconomic status (SES) is associated with both depression and activities of daily living (ADL and IADL). However, the role of ADL as a biological mechanism in the relationship between SES and late-life depression, examined through longitudinal data, remains understudied. This study explored the longitudinal mediation effects of basic ADL or IADL on the SES-depression link in older adults.
Methods
Data from the China Health and Retirement Longitudinal Study (N = 4104) were utilized. Mediation analysis was performed using parallel process latent growth curve modeling.
Results
The average age of participants was 57.76 years, and 55.7% being females. Significant linear growth over time was observed in ADL, IADL, and depression. Adjusting for covariates, SES was positively linked to the initial levels (intercepts) of ADL (βiADL=-0.100[-0.143, -0.057]), IADL (βiIADL=-0.140[-0.185, -0.095]), and depression (βiDEP=-0.103[-0.158, -0.048]). However, SES showed no significant correlation with the rate of change (slopes) in ADL, IADL, or depression (P > 0.05). The intercepts of ADL (βiDEP = 0.566[0.503, 0.629]) and IADL (βiDEP = 0.607[0.544, 0.670]) were positively correlated with the depression intercept but negatively with the depression slope. Conversely, the slopes of ADL and IADL were positively associated with the depression slope. These results suggest a negative indirect relationship between SES and the initial level of depression, but a positive indirect relationship with the rate of increase in depression through ADL (or IADL) intercept.
Conclusions
Higher SES is associated with a lower initial risk of depression and ADL difficulties. However, this same higher SES may relate to a faster increase in ADL difficulties and depression among middle-aged and older adults. The findings underscore the need for increased governmental healthcare funding and improved healthcare accessibility. Additionally, maintaining adequate sleep and physical activity can help prevent disability and reduce depression risk later in life, particularly among older adults with lower SES.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Depression represents a significant public health issue globally, affecting 3.8% of the population, including 5.0% of adults and 5.7% of those over 60 years old [1, 2]. Approximately 280 million individuals worldwide suffer from depression [2]. Reports by the WHO indicate that China is now the second largest contributor to the global depression burden, with cases surpassing 54.8 million. Depression can manifest at any age, but is prevalent in later life [3]. Addressing risk factors to prevent depression is crucial. Similarly, functional disability poses a major public health challenge, with over 1 billion people globally experiencing one or more forms of disability [4]. Recent research in China showed that the functional disability rate among older adults reached 41.0% [5].
Previous studies have indicated that disability conditions are risk factors for depression among older adults [6,7,8,9]. Researchers have determined that disabilities in activities of daily living (ADL) can increase the risk of depression for middle-aged and older adults and their spouses [6]. Ahmad reported that older adults with limitations in both basic ADL and instrumental ADL are at a higher risk of depression [10]. Furthermore, Researcher Fan observed that severe ADL disabilities lead to an increased risk of depressive symptoms, as shown by a longitudinal trajectory model [11]. Wang noted a bi-directional relationship between ADL disabilities and depressive symptoms over time in this demographic [12]. According to cognitive theory models, negative emotions triggered by physical disabilities can cause cognitive dissonance [13]. The accumulation of such emotions tends to escalate, eventually resulting in depression. Functional disability is linked to unfavorable depressive symptom trajectories. Thus, understanding the longitudinal relationship between ADL disability and depression is essential to identify key interventions to prevent this detrimental progression. ADLs are commonly used to assess functional status in older adults [14], and are divided into basic ADL and IADL. Basic ADL encompasses essential daily activities necessary for basic survival and living, including self-care (such as eating, grooming, washing, bathing, toileting, dressing) and functional mobility (such as turning over, getting up from bed, transferring, walking, operating a wheelchair, and navigating stairs) [15]. IADL involves activities required for maintaining an independent life, such as using the telephone, shopping, cooking, doing housework, managing finances, taking medication, using transportation, handling emergencies, and participating in community leisure activities that require various tools [16]. The integration of ADL and IADL provides a comprehensive evaluation of an individual’s ability to perform daily life functions. Moreover, a decline in IADL is often a precursor to ADL disability, as IADL requires more complex cognitive and executive functions. Monitoring IADL can help in early detection of underlying health issues, including cognitive decline and symptoms of depression.
Previous studies have examined the connection between functional disabilities and the trajectory of depressive symptoms. However, the combined impact of functional disability and other factors on depression remains unclear. SES has been identified as a significant risk factor for both depression and ADL, respectively [17,18,19,20]. Research indicates that adults with low SES face restricted access to medical services, poor nutrition, and unhealthy behaviors, all of which contribute to a higher incidence of functional disabilities [21]. Liu noted that limited education, rural residence, unemployment and lower income are linked to functional disability among elderly Chinese individuals [22]. Eric found that socioeconomic status variables such as education and wealth at baseline were not related to disability, but the disability risk of individuals with lower socioeconomic status often increased over time [23]. SES is also an important factor influencing residents’ depression. Researchers found that SES variables were independently associated with the prevalence of depressive symptoms, with household wealth showing a more robust effect than education [24]. A Meta-Analysis of Lorant indicated compelling evidence for socioeconomic inequality in depression, but they think that socioeconomic inequality in depression varies according to the way mental disorder is measured, to the definition and measurement of SES, and to contextual features such as region and time [25]. Therefore, it is crucial to select appropriate indicators and construct the SES index in research.
These studies highlight the associations among socioeconomic factors, depression, and ADL in middle-aged and older adults, respectively. Nonetheless, the combined effects of functional disability and SES on the long-term trajectories of depressive symptoms in this demographic are not well-understood. Other research has shown that individuals from lower SES groups tend to exhibit more disabilities at similar depression levels [24]. Moreover, in countries with weaker welfare systems, these individuals receive substandard medical care and are less likely to utilize specialized psychiatric services, regardless of the available welfare benefits [25]. Despite these insights, there has been limited focus on the long-term interaction between SES and depression, including the potential mediating influence of ADL trajectories. Thus, there is a pressing need for interventions that address these disparities in depression, especially those associated with ADL limitations.
In this study, we are committed to filling current evidence gaps by testing the mediation effects of different dimensions of ADL (basic ADL and IADL) in the relationship between socioeconomic and depression trajectories. Firstly, we hypothesized that the development trajectory of ADL is positively correlated with depression among middle-aged and older adults Second, we hypothesized that SES has a direct correlation with both the initial levels and the rates of progression of ADL and depression. Thirdly, we hypothesize that the longitudinal association between SES and depression is mediated by ADL. We will also analyze the difference between basic ADL and IADL in the relationship between SES and depression.
Methods
Sample design and setting
The data we used from the China Health and Retirement Longitudinal Study (CHARLS), national representative survey on community-based population, conducted by the National School of Development in China [26]. The baseline survey was conducted in 2011, which utilized a multi-stage stratified probability proportional-to-size (PPS) sampling technique to select participants [27]. Three follow-up waves were conducted separately in 2013, 2015 and 2018. Demographic and socioeconomic characteristics and lifestyles variables were collected at wave 1, comprehensive information on the depression and ADL of middle-aged and older adults were collected at waves 1, 2, 3 and 4. In this study, participants aged under 45 years, had missing values in covariates, and missed visit in follow-up waves were excluded from the analysis. Finally, there were 4104 middle-aged and older adults were included in the analysis. Detail procedure of selection was shown in Additional file 1.
Measures
Depression
We defined depression using the Chinese version of the center for Epidemiological Studies Depressions scale (CES-D-10) [28]. The CES-D-10 includes 10 items with 4 response options, containing rarely, some days (1–2 days), occasionally (3–4 days) and most of the time (5–7 days) [29]. The scales for each of the 10 items were adjusted to 0, 1, 2 and 3. The total score ranges from 0 to 30, with a higher score indicating a higher level of depressive symptoms.
Basic or instrumental activity of daily living
Basic or physical ADLs (ADL) are the skills required to perform daily physical tasks, including dressing, bathing, feeding, moving from bed to chair, using the toilet, and maintaining continence. Instrumental ADLs (IADL) include more complex activities than basic ADLs, related to the ability to live independently, which constitute doing housework, cooking, shopping, managing money, and taking medication. Dependency in any items of ADLs and IADLs was recorded as “having any difficulty and needing help” (scored 1)versus “no difficulty” or “with difficulty but still can do it” (scored 0) [30]. The score of basic ADL ranged from 0–6, and the IADL ranged from 0–5 [11]. Higher score indicates worse performance in the basic ADL or IADL.
Socioeconomic status (SES)
Factors such as education level, occupation, income, wealth, and deprivation are often used to reflect SES [31]. This study selected educational level, household consumption expenditure, and hukou to measure the SES of older adults. Educational level is divided into the following four categories: no formal education, primary education, secondary education, and higher education. This study focuses on middle-aged and older adults, who are mostly retired. Therefore, we did not include occupational variables and instead incorporated household consumption expenditure to construct a socioeconomic status index. Within the China Health and Retirement Longitudinal Study (CHARLS), it is observed that income exhibits considerable volatility. In contrast, consumption patterns demonstrate higher stability and are more amenable to quantification. It is noteworthy that consumption data are associated with a lower incidence of measurement error when juxtaposed with transient income figures, thereby rendering consumption a more reliable proxy for assessing enduring economic resources [32]. The formula employed for calculating annual household consumption is as follows: annual household consumption = (weekly consumption × 52) + (monthly consumption × 12) + (annual consumption × 1). Due to China’s urban-rural dual structure, the nature of household registration (hukou) becomes an important identity characteristic for individuals. Having an urban household registration implies more opportunities to access higher-income occupations. Therefore, this study also includes hukou in constructing the socioeconomic status index.
This study utilized principal component analysis (PCA) to construct a SES index, based on three key indicators: household consumption expenditure, educational attainment, and household registration status. This composite index was created to assess SES comprehensively among middle-aged and older adults. Initially, the scores for household consumption expenditure, educational attainment, and household registration status were normalized, and integrated into the PCA model. Subsequently, the SES index was derived by summing the products of each principal component score and its corresponding weight.
Covariates
The covariates for this study included age, sex (male and female), and marital status (married and others). Following national guideline [33], the study also considered healthy lifestyle factors such as physical activity, drinking habits, sleep, and smoking.
According to Li, the total weekly physical activity, expressed in MET-minutes/week, is calculated by multiplying the frequency, duration, and MET value of activities. A threshold of at least 600 MET-minutes/week was set to define regular physical activity [34]. Drinking status was categorized into two groups: those who had consumed alcohol in the past 12 months (Yes) and those who had not (No). As defined by Healthy China, adequate sleep is considered 7–9 h per night, while inadequate sleep is less than 7 or more than 9 h [35]. Smoke was classified as current smoker and not a current smoker.
Statistical analyses
Latent Growth Curve modelling (LGCM) is a suitable tool for gerontological research, which can track the trajectories and changes of phenomena (e.g., physical health and psychological well-being) over time [36]. This study uses LGCM to analyze the longitudinal mediation model. The trajectories of ADL, IADL and depression were captured by two latent growth factors: the intercept (I) factor, reflecting the score of ADL, IADL and depression at baseline, and the slope (S) factor, reflecting the rate of change over the four waves of the observation period. First, we fit three unconditional model of ADL, IADL, and depression without risk factors, examine the development trends of each variable, separately. Secondly, we constructed two structural equation models, introduced the SES and all covariates (demographic characteristics, and lifestyle indicators) in the model, explore the relationship between the SES, depression and ADL, or IADL separately. Finally, the Bootstrap method was used to validate the significance of the mediating effect. All direct and indirect associations were calculated using bias corrected bootstrapped standard errors based on 1000 samples.
In addition, we calculated E-values for all statistically significant direct effects in order to explain the relationship between unmeasured confounder and all exposure and outcome [37]. Missing data on ADL, IADL and depression were estimated using multiple imputation by chained equations (MI). We created 10 imputed datasets, and the estimates from the LGCM mediation analysis were pooled used Rubin’s rules [27]. The significance level was set at P < 0.05. The LGCM were conducted by Mplus V.7.4.
Results
Descriptive statistics
The characteristics of the sample for both observed and imputed data are presented in Table 1. The study analyzed 4104 middle-aged and older adults. The mean age of the participants was 57.76 years, and 55.7% were females.
The growth trajectories of ADL, IADL, and depression
To investigate the temporal trends of variables, unconditional latent growth models for ADL, IADL, and depression were constructed sequentially (Table 2). The results showed that ADL (β = 0.493, P < 0.001), IADL (β = 0.517, P < 0.001), and depression (β = 0.279, P < 0.001) showed significant linear growth over time. Additionally, both the intercepts and slopes were positively correlated in the ADL (r = 0.521, P < 0.01) and IADL (r = 0.409, P < 0.01) dimensions, suggesting that higher initial levels are associated with increased growth rates.
Direct and indirect associations between SES, ADL and depression
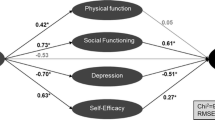
A structural equation model was established (Fig. 1) to explore the longitudinal mediating effects of ADL between SES and depression. The model testing confirmed a good fit (X2/df = 9.475, CFI = 0.944, TLI = 0.918, RMSEA = 0.045, SRMR = 0.028).
Direct associations between SES, ADL, and depression. Note: SES, Socioeconomic status; iADL, Basic activities of daily living Intercept; sADL, Basic activities of daily living Slope; iIADL, Instrumental activities of daily living Intercept; sIADL, Instrumental activities of daily living Slope; iDEP, Depression Intercept; sDEP, Depression Slope; PA, Regular physical activity. Model: adjusted for age, sex, marital status and lifestyle indicators (Regular physical activity, Sleep, Smoke, Drink)
The results of direct associations between SES, ADL, and depression are detailed in model 1 (Table 3). After adjusting for covariates, SES was found to be significantly and positively associated with the initial levels of both ADL (βiADL=-0.100[-0.143, -0.057]) and depression (βiDEP=-0.103[-0.158, -0.048]), indicating that older adults with higher SES exhibit lower initial levels of ADL and depression. However, SES was not significantly correlated with either the progression rates of ADL or depression (P > 0.05), suggesting that SES does not significantly influence the rates of progression for ADL and depression. Additionally, the initial level of ADL was positively correlated with the initial level of depression (βiDEP = 0.566[0.503, 0.629]), but negatively correlated with the rate of increase in depression (βsDEP=-0.509[-0.781, -0.237]). This implies that higher initial levels of ADL are associated with higher initial levels of depression, yet the rate of increase in depression is slower. The rate of progression in ADL was also found to be positively correlated with the rate of progression in depression(βsDEP = 0.868[0.462,1.274]), indicating a synchronous increase. Moreover, healthy sleep was negativity associated with ADL (β=-0.200[-0.259, -0.141]) (Fig. 1).
The mediating effects of the initial levels and progression rates of ADL were calculated using bias-corrected bootstrapped standard errors based on 1000 samples, as reported in model 1 (Table 4). The results revealed a negative indirect association between SES and the initial level of depression (β=-0.056[-0.081, -0.031]), and a positive indirect association with the rate of increase in depression (β=0.051 [0.014, 0.088]) through the initial level of ADL. These findings indicate that the initial level of ADL mediated 35.2% of the association between SES and the initial level of depression. Furthermore, the initial level of ADL mediated 100% of the association between SES and the rate of increase in depression.
Direct and indirect associations between SES, IADL and depression
A structural equation model was established (Fig. 2) to assess the longitudinal mediating effect of IADL between SES and depression. The model showed a good fit after evaluation (χ2/df = 11.456, CFI = 0.934, TLI = 0.903, RMSEA = 0.050, SRMR = 0.031).
Direct associations between SES, IADL and depression. Note: SES, Socioeconomic status; iADL, Basic activities of daily living Intercept; sADL, Basic activities of daily living Slope; iIADL, Instrumental activities of daily living Intercept; sIADL, Instrumental activities of daily living Slope; iDEP, Depression Intercept; sDEP, Depression Slope; PA, Regular physical activity. Model: adjusted for age, sex, marital status and lifestyle indicators (Regular physical activity, Sleep, Smoke, Drink)
The direct associations between SES, IADL, and depression are detailed in model 2 (Table 3). After adjusting for covariates, SES was significantly and positively associated with both the IADL (βiIADL=-0.140[-0.185, -0.095]) and depression intercepts (βiDEP=-0.075[-0.124, -0.026]), indicating that middle-aged and older adults with higher SES exhibit lower initial levels of IADL and depression.
However, SES was not correlated with the progression rates of either IADL or depression (P > 0.05). Additionally, the IADL intercept was positively correlated with the depression intercept (βiDEP = 0.607[0.544, 0.670]), but negatively correlated with the depression slope (βsDEP=-0.550[-0.803, -0.297]). This suggests that middle-aged and older adults with higher initial levels of IADL also exhibit higher initial levels of depression, but experience a slower increase in depression over time. The progression rate of IADL was also positively correlated with the progression rate of depression (βsDEP =1.076[0.674, 1.478]), indicating that faster increases in IADL are associated with faster increases in depression. Middle-aged and older adults engaging in regular physical activity (β=-0.186[-0.235, -0.137]) and maintaining healthy sleep patterns (β=-0.185[-0.236, -0.134]) are at a lower risk for IADL challenges (Fig. 2).
The indirect effects of the IADL intercept and slop are detailed in model 2 (Table 4). The results showed a negative indirect association between SES and the depression intercept (β=-0.085[-0.114, -0.056]), and a positive indirect association with the depression slope (β=0.077 [0.030, 0.124]) via the IADL intercept. These findings indicate that the IADL intercept mediated 46.9% of the association between SES and the depression intercept. Furthermore, the IADL intercept mediated 100% of the association between SES and the depression slope.
Sensitivity analyses
The models of SES, depression and ADL or IADL were reanalyzed in the sample of participants with no missing data (N = 3507). The direct and indirect associations between SES, depression and ADL or IADL were broadly similar to those found in the analyses with the imputed data (Additional file 2). The E-values for the imputed data analysis (Table 3) ranged between 1.17 (lower limit = 1.01) and 1.71(lower limit = 1.32). There is no special standard for E-value, this suggests that relatively modest confounder associations could explain the observed effects of SES, ADL, IADL and depression. Therefore, it is important to consider unmeasured confounding when interpreting these findings.
Discussion
This study employed Parallel Process Latent Growth Curve Modeling (PP-LGCM) to assess the mediating role of basic ADL or IADL in the relationship between SES and depression among middle-aged and older Chinese adults, using data from a large, nationally representative longitudinal cohort. The results indicated that SES had varying effects on the baseline levels of basic ADL and IADL. However, SES was not directly associated with the development rates of ADL and depression, which contradicted our hypothesis. Nonetheless, our findings suggested that the relationships between SES and depression were mediated by both the baseline and the development rates of basic ADL and IADL.
Consistent with prior evidence, our analysis confirmed socioeconomic inequalities in ADL, with individuals from higher socioeconomic backgrounds exhibiting lower basic ADL scores. Conversely, those with lower SES suffered more from functional disability (IADL) than their wealthier counterparts [38, 39]. This disparity may stem from the ability of wealthier individuals to invest more in health improvement. In contrast, those with lower incomes have limited resources for health care, as a significant portion of their income is allocated to basic needs [40, 41]. Diverging from previous research, our study differentiated the effects of SES on ADL at two levels: the baseline level and the development speed. Our findings showed that SES was negatively correlated with ADL and IADL at the baseline, yet no significant relationship was observed with the rate of ADL or IADL progression. Furthermore, SES had a more pronounced impact on the initial state of IADL compared to basic ADL among middle-aged and older adults.
Previous literature has highlighted the importance of wealth in decreasing the likelihood of IADL impairments among older adults [42, 43]. Ratna examined socioeconomic inequality in the prevalence of IADL among older adults in India, finding that educational status and wealth quintile were significant factors in this inequality [43]. Another study confirmed that income enables older adults to improve their living conditions, positively affecting IADL [39]. This suggests that SES is directly related to the occurrence of IADL, with lower SES associated with a higher likelihood and greater deterioration of IADL over time.
Moreover, our research identified a mediating role for basic ADL and IADL in the relationship between SES and depression among Chinese middle-aged and older adults. Previous studies have suggested that SES is a direct correlate of depression [44], with researchers like Gallo and Matthews noting that lower SES limits an individual’s capacity to manage stress, thereby increasing vulnerability to negative emotions and cognitions [45]. Additionally, as individuals age, accumulated social stress may make those from lower social strata more prone to depressive symptoms [46]. study discerned a direct association between SES and the initial presentation of depression. It was also observed that SES indirectly influenced the initial state and the development rate of depression through the status of basic ADL and IADL. Individuals with lower SES had higher scores for basic ADL and IADL, indicating a greater reliance on daily living activities, which subsequently impacted their level of depression. Interestingly, compared to basic ADL, IADL had a greater mediating effect on the relationship between SES and depression [47, 48]. This may be because IADL relates more closely to quality of life and is improvable through the use of tools. Therefore, public health services aimed primarily at improving IADL represent an important strategy for addressing depression in middle-aged and older adults with low socioeconomic status.
We observed more specific details in the relationships between basic ADL or IADL and depression. When baseline scores for ADL or IADL were higher, the rate of depression development was slower in middle-aged and older adults later in life. This finding aligns with the concept of post-traumatic growth, which refers to positive psychological changes following adverse experiences [49]. These changes may include improved relationships, enhanced self-perception, and a general positive shift in an individual’s life [50]. Previous research has indicated that adverse experiences can bolster an individual’s positive psychology, enhancing self-improvement efforts [51]. Individuals who experienced challenges with ADL were able to achieve post-traumatic growth and enhance self-worth through self-acceptance, subsequently lowering their depression risk. Additionally, we found that both sleep and physical activity could reduce disability incidence and slow the progression of disabilities while decreasing the risk of depression.
To our knowledge, this is the first study that to examine the longitudinal association between SES, and basic ADL or IADL, as well as depression in China. However, several potential limitations in our study should be acknowledged. First, ADL were use of self-reported measures, which may introduce recall bias into the data. Second, there are possibly environmental factor or genetic factors related to depression that is not included in the study. Future studies should consider a wider range of potential factors, including environmental factors and genetic factors.
Conclusion
This study clarifies the mediating roles of activities of daily living (basic ADL and IADL) in the longitudinal relationship between SES and depression among middle-aged and older adults. The findings reveal that higher initial levels of ADL and IADL were paradoxically associated with an increased risk of depression, but higher starting points for ADL or IADL were linked to a slower progression of depressive symptoms. Additionally, the more rapid the progression of basic ADL or IADL, the slower the progression of depression. SES was directly correlated with the initial levels of basic ADL, IADL, and depression. SES had no direct but an indirect relationship with the progression rate of depression, with initial levels of basic ADL and IADL serving as mediators. Specifically, higher SES is associated with better initial functional capabilities in basic ADL and IADL, and a lower initial prevalence of depression. However, this same higher SES may correlate with a more rapid development of depression among middle-aged and older adults, underscoring the complex relationship between SES and mental health outcomes in later life. Collectively, these findings underscore the important policy implication that increasing financial resources and improving to health care services, especially for the lower socioeconomic strata, could enhance ADL levels and potentially prevent depression in the future. Moreover, maintaining adequate sleep and PA can prevent the onset of disabilities and may reduce the risk of depression in later life, particularly among those in lower social classes.
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request. http://charls.pku.edu.cn/.
References
Malhi GS, Mann JJ, Depression. Lancet. 2018;392(10161):2299–312.
World Health Organization. Depressive disorder (depression) 2023 [ https://www.who.int/news-room/fact-sheets/detail/depression. Accessed July, 2024.
Lian Y, Yang L, Gao M, Jia CX. Relationship of Frailty markers and socioeconomic status to incidence of depressive symptoms in a community cohort. J Am Med Dir Assoc. 2021;22(3):570–e61.
Chauhan S, Kumar S, Bharti R, Patel R. Prevalence and determinants of activity of daily living and instrumental activity of daily living among elderly in India. BMC Geriatr. 2022;22(1):64.
Zhang Y, Xiong Y, Yu Q, Shen S, Chen L, Lei X. The activity of daily living (ADL) subgroups and health impairment among Chinese elderly: a latent profile analysis. BMC Geriatr. 2021;21(1):30.
He MF, Ma J, Ren Z, Zhou G, Gong P, Liu MT, et al. Association between activities of daily living disability and depression symptoms of middle-aged and older Chinese adults and their spouses: a community based study. J Affect Disorders. 2019;242:135–42.
Mendes-Chiloff CL, Ramos-Cerqueira ATA, Lima MCP, Torres AR. Depressive symptoms among elderly inpatients of a Brazilian university hospital: prevalence and associated factors. Int Psychogeriatr. 2008;20(5):1028–40.
Liu AH, Peng YJ, Zhu WL, Zhang YL, Ge SH, Zhou Y et al. Analysis of factors Associated with Depression in Community-Dwelling older adults in Wuhan, China. Front Aging Neurosci. 2021;13.
Zhou L, Wang W, Ma X. The bidirectional association between the disability in activities of daily living and depression: a longitudinal study in Chinese middle-aged and older adults. BMC Public Health. 2024;24(1).
Ahmad NA, Abd Razak MA, Kassim MS, Sahril N, Ahmad FH, Harith AA, et al. Association between functional limitations and depression among community-dwelling older adults in Malaysia. Geriatr Gerontol Int. 2020;20:21–5.
Tian F, Yang H, Pan J. Association between functional disability and long-term trajectories of depressive symptoms: evidence from the China Health and Retirement Longitudinal Study. J Affect Disord. 2022;310:10–6.
Wang J, Luo N, Sun Y, Bai R, Li X, Liu L et al. Exploring the reciprocal relationship between activities of daily living disability and depressive symptoms among middle-aged and older Chinese people: a four-wave, cross-lagged model. BMC Public Health. 2023;23(1).
Furukawa TA, Suganuma A, Ostinelli EG, Andersson G, Beevers CG, Shumake J, et al. Dismantling, optimising, and personalising internet cognitive behavioural therapy for depression: a systematic review and component network meta-analysis using individual participant data. Lancet Psychiatry. 2021;8(6):500–11.
Dey AB. World report on ageing and health. Indian J Med Res. 2017;145(1).
Zhang YC, Xiong Y, Yu QH, Shen SS, Chen L, Lei X. The activity of daily living (ADL) subgroups and health impairment among Chinese elderly: a latent profile analysis. BMC Geriatr. 2021;21(1).
Pashmdarfard M, Azad A. Assessment tools to evaluate activities of Daily Living (ADL) and instrumental activities of Daily Living (IADL) in older adults: a systematic review. Med J Islam Repub Iran. 2020;34:33.
Brunner EJ, Shipley MJ, Ahmadi-Abhari S, Valencia Hernandez C, Abell JG, Singh-Manoux A, et al. Midlife contributors to socioeconomic differences in frailty during later life: a prospective cohort study. Lancet Public Health. 2018;3(7):e313–22.
Wang JL, Schmitz N, Dewa CS. Socioeconomic status and the risk of major depression: the Canadian National Population Health Survey. J Epidemiol Community Health. 2010;64(5):447–52.
Domenech-Abella J, Mundo J, Leonardi M, Chatterji S, Tobiasz-Adamczyk B, Koskinen S, et al. The association between socioeconomic status and depression among older adults in Finland, Poland and Spain: a comparative cross-sectional study of distinct measures and pathways. J Affect Disord. 2018;241:311–8.
Yang L, Konttinen H, Martikainen P, Silventoinen K. Socioeconomic status and physical functioning: a longitudinal study of older Chinese people. J Gerontol B Psychol Sci Soc Sci. 2018;73(7):1315–29.
Liu H, Wang M. Socioeconomic status and ADL disability of the older adults: cumulative health effects, social outcomes and impact mechanisms. PLoS ONE. 2022;17(2):e0262808.
Liu J, Chi I, Chen G, Song X, Zheng X. Prevalence and correlates of functional disability in Chinese older adults. Geriatr Gerontol Int. 2009;9(3):253–61.
Lai ETC, Ho HC, Ho SC, Woo J, Socioeconomic, Status. Physical functioning and mortality: results from a Cohort Study of older adults in Hong Kong. J Am Med Dir Assoc. 2022;23(5):858–e645.
Hinata A, Kabasawa K, Watanabe Y, Kitamura K, Ito Y, Takachi R et al. Education, household income, and depressive symptoms in middle-aged and older Japanese adults. BMC Public Health. 2021;21(1).
Lorant V, Deliege D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol. 2003;157(2):98–112.
Zhao Y, Atun R, Oldenburg B, McPake B, Tang S, Mercer SW, et al. Physical multimorbidity, health service use, and catastrophic health expenditure by socioeconomic groups in China: an analysis of population-based panel data. Lancet Global Health. 2020;8(6):e840–9.
Zheng X, Cui YH, Xue YQ, Shi L, Guo Y, Dong F, et al. Adverse childhood experiences in depression and the mediating role of multimorbidity in mid-late life: a nationwide longitudinal study. J Affect Disorders. 2022;301:217–24.
Jin Y, Luo Y, He P. Hypertension, socioeconomic status and depressive symptoms in Chinese middle-aged and older adults: findings from the China health and retirement longitudinal study. J Affect Disord. 2019;252:237–44.
Jing R, Xu T, Rong H, Lai X, Fang H. Longitudinal Association between Sleep Duration and depressive symptoms in Chinese Elderly. Nat Sci Sleep. 2020;12:737–47.
Gong J, Wang G, Wang Y, Chen X, Chen Y, Meng Q, et al. Nowcasting and forecasting the care needs of the older population in China: analysis of data from the China Health and Retirement Longitudinal Study (CHARLS). Lancet Public Health. 2022;7(12):e1005–13.
Xue BL, Xue YQ, Dong F, Zheng X, Shi L, Xiao SJ et al. The impact of socioeconomic status and sleep quality on the prevalence of multimorbidity in older adults. Front Public Health. 2022;10.
Gong J, Wang G, Wang Y, Zhao Y. Consumption and poverty of older Chinese: 2011–2020. J Econ Ageing. 2022;23.
Chudasama YV, Khunti K, Gillies CL, Dhalwani NN, Davies MJ, Yates T, et al. Healthy lifestyle and life expectancy in people with multimorbidity in the UK Biobank: a longitudinal cohort study. PLoS Med. 2020;17(9):e1003332.
Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol. 2014;43(1):61–8.
McCrann S, Loughman J, Butler JS, Paudel N, Flitcroft DI. Smartphone use as a possible risk factor for myopia. Clin Exp Optom. 2020;104(1):35–41.
Burant CJ. Latent growth curve models: Tracking Changes over Time. Int J Aging Hum Dev. 2016;82(4):336–50.
VanderWeele TJ, Ding P. Sensitivity analysis in Observational Research: introducing the E-Value. Ann Intern Med. 2017;167(4):268–.
Zhang T, Liu C, Lu B, Wang X. Changes of inequality in functional disability of older populations in China from 2008 to 2018: a decomposition analysis. BMC Geriatr. 2022;22(1):308.
Guerra RO, Alvarado BE, Zunzunegui MV. Life course, gender and ethnic inequalities in functional disability in a Brazilian urban elderly population. Aging Clin Exp Res. 2008;20(1):53–61.
Zhang L, Liu N. Health reform and out-of-pocket payments: lessons from China. Health Policy Plan. 2014;29(2):217–26.
Noronha KV, Andrade MV. [Social inequality in health and the utilization of health services among the elderly in Latin America]. Rev Panam Salud Publica. 2005;17(5–6):410–8.
Connolly D, Garvey J, McKee G. Factors associated with ADL/IADL disability in community dwelling older adults in the Irish longitudinal study on ageing (TILDA). Disabil Rehabil. 2017;39(8):809–16.
Patel R, Srivastava S, Kumar P, Chauhan S, Govindu MD, Jean Simon D. Socio-economic inequality in functional disability and impairments with focus on instrumental activity of daily living: a study on older adults in India. BMC Public Health. 2021;21(1):1541.
Roozenbeek J, Schneider CR, Dryhurst S, Kerr J, Freeman ALJ, Recchia G, et al. Susceptibility to misinformation about COVID-19 around the world. R Soc Open Sci. 2020;7(10):201199.
Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: do negative emotions play a role? Psychol Bull. 2003;129(1):10–51.
Turner RJ, Wheaton B, Lloyd DA. The epidemiology of social stress. Am Sociol Rev. 1995;60(1).
Gobbens RJ. Associations of ADL and IADL disability with physical and mental dimensions of quality of life in people aged 75 years and older. Peerj. 2018;6.
Ran LY, Jiang XD, Li BG, Kong HQ, Du MQ, Wang XL et al. Association among activities of daily living, instrumental activities of daily living and health-related quality of life in elderly Yi ethnic minority. BMC Geriatr. 2017;17.
Calhoun LG, Tedeschi RG. Handbook of Posttraumatic Growth. 2006.
Tedeschi RG, Calhoun LG. The Posttraumatic Growth Inventory: measuring the positive legacy of trauma. J Trauma Stress. 1996;9(3):455–71.
Affleck G, Tennen H. Construing benefits from adversity: adaptational significance and dispositional underpinnings. J Pers. 1996;64(4):899–922.
Acknowledgements
We are grateful to all volunteers and staff who participated in China Health and Retirement Longitudinal Study for collecting and providing data.
Funding
This work was supported by the Guangdong Basic and Applied Basic Research Foundation (No.2022A1515110295, 2022A1515011591), National Nature Science Foundation of China (No.72274091), China Postdoctoral Science Foundation (No. 2022M721539), Guangdong Philosophy and Social Science Foundation (No. GD23CGL06).
Author information
Authors and Affiliations
Contributions
ZCC was responsible for the conception and design of the study. ZX, YY were major contributors in writing the manuscript. YLL, ZXY, XSJ, and LXY analyzed and interpreted the data. LJX, LXR and ZMJ processed the data statistically. ZCC, ZX and TF reviewed and finalized the manuscript. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The CHARLS survey project was approved by the Biomedical Ethics Committee of Peking University, and all participants were required to sign informed consent. The ethical approval number was IRB00001052-11015.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zheng, X., Yin, Y., Yang, L. et al. Socioeconomic status and depression in later life: longitudinal mediation effects of activities of daily living. BMC Psychiatry 24, 625 (2024). https://doi.org/10.1186/s12888-024-06077-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-024-06077-4