Abstract
Background
Sexualised drug use, known as ‘chemsex’ or ‘chemfun,’ is the practice of intentionally using illicit drugs before or during sexual activates to enhance sexual arousal and pleasure. International and local data have both suggested that chemsex is common among men who have sex with men (MSM). Chemsex is generally seen with the engagement of risky sexual activities and therefore poses a threat regarding the potentially increased spread of human immunodeficiency virus and other sexually transmitted infections. However, little work has been done on the primary prevention of chemsex among MSM. Therefore, the aim of this study is to develop and evaluate an interactive internet-based intervention in reducing the sexual harms of chemsex among MSM in Hong Kong,
Methods
A two-armed, randomised, parallel-group trial with a three-month follow-up period will be conducted. 250 MSM aged 18 years or the above will be recruited through local non-governmental organisations, social media and by snowballing in Hong Kong. Participants will be randomly allocated into either the intervention (n = 125) or control group (n = 125). The interactive internet-based intervention will be developed based on the theory of planned behaviours. Participants in the control group will receive a web-based intervention without any sexual health information and without any interactive components. The primary outcomes will be self-efficacy in refusing risky sexual behaviours and chemsex, as measured by the Drug Avoidance Self-Efficacy Scale, the Self-Efficacy for Sexual Safety and the Condom Self-Efficacy Scale. Subjects in both groups will be evaluated at baseline and 3 months after baseline.
Discussion
To the best of our knowledge, this will be the first interactive internet-based intervention to specifically target chemsex among MSM. This project can help in the development and testing of culturally relevant health promotion programmes that reduce chemsex among MSM. Using an online delivery mode, the intervention is capable of reaching a large population of targets at a relatively low cost and thus has the potential to reduce the public health burden of chemsex and other risky sexual behaviours among MSM in a cost-effective manner.
Trial registration
International standard randomized controlled trial number (ISRCTN) registry: ISRCTN20134522 registered on 17 March 2021.
Similar content being viewed by others
Background
Chemsex: an emerging sexual health issue
Substance use is common among men who have sex with men (MSM). It is reported than MSM are three times more likely to use illicit substances than their heterosexual counterparts [1]. In Australia, about 60% of MSM used recreational drug in the past 6 months [2]. Another study in Melbourne, Australia found that 63.1% of MSM used at least one drug in the last 3 months and 36.6% used ≥2 drugs. Poppers (44.8%), marijuana (30.8%) and ecstasy (19.1%) were the three most common drugs used among MSM in the last 3 months [3]. Furthermore, the study found that 80.4% of ecstasy users and 74.3% of gamma-hydroxybutyrate (GHB) users reported the drug made them much more likely to kiss someone [3]. Another study in the United Kingdom found that one quarter of MSM had used three or more recreational drugs in the previous 3 months [4]. Recreational drug use is a global concern among MSM, particularly those who use drugs before or during sexual activities because it increases the likelihood of engaging in risky sexual behaviours [1].
Sexualised drug use, known as ‘chemsex’ or ‘chemfun,’ is the practice of intentionally using illicit drugs before or during sexual activates to enhance sexual arousal and pleasure. This practice, however, poses harmful risks to sexual health [1]. Chemsex is common among MSM [5]. One study in the Republic of Ireland found that 27% among 510 MSM reported engaging in chemsex within the previous 12 months [6], where a study in the Netherlands found that 41% of HIV-negative MSM and transgender persons who have sex with men (n = 330) had engaged in chemsex with casual partners in the previous 3 months [7].
Chemsex is also an emerging health issue in Hong Kong, where a report by the Hong Kong Jockey Club Drug Info Centre found that 17% of the surveyed MSM had ever engaged in chemsex, and more than half (58.18%) had engaged in their first chemsex experience between the ages of 16 and 25 [8]. A community-based organisation in Hong Kong also found that 9% of MSM respondents had ever engaged in chemsex [9], with those aged 31 to 35 being the most likely to engage in chemsex compared with other age groups. In Hong Kong, the most common drug used by MSM was methamphetamine (49%), followed by gamma-hydroxybutyrate (GHB)/ gamma-Butyrolactone (GBL) (27%), ecstasy (18%) and then ketamine (10%). Furthermore, 31% used methamphetamine and Viagra [9]. Additionally, an empirical study in Hong Kong found that that 8% of college students in Hong Kong had previously engaged in chemsex during their lifetime, and 73% of them were MSM [10]. Another study in Hong Kong reported that 12% of MSM had chemsex in the previous 6 months [11]. A qualitative study on 31 MSM in Hong Kong found that chemsex is also popular on dating apps [12]. The data suggest that there is a need to develop primary prevention programmes for chemsex among MSM.
Dangers associated with chemsex
Severe drug interactions with a range of drugs, including human immunodeficiency virus (HIV) medications, can be fatal [13]. This is particularly relevant to MSM populations, which are disproportionately affected by HIV infections. Moreover, the use of pre-exposure prophylaxis to prevent the acquisition of HIV has become increasingly common among MSM [14]. In addition to drug interactions, the anaesthetic nature of some drugs can prolong the duration of sexual activities, which in turn can lead to rectal and penile trauma, potentially further facilitating the spread of sexually transmitted infections (STIs) [13]. Furthermore, because of the sexual disinhibition and hypersexuality induced by the drugs, chemsex has been found to increase the likelihood of engaging in other risky sexual behaviours, such as condomless anal sex, injecting drug use and higher alcohol consumption, fisting, sharing sex toys, and group sex [15]. This might increase the spread of HIV and other STIs [13, 16]. Indeed, one systematic review conducted in 2019 found the rates of condomless anal sex range from 30 to 38% among MSM who practiced chemsex [1]. Besides, a study in the United Kingdom reported that engaging in chemsex was associated with a higher number of condomless anal male partners [15]. A recent study in Australia also reported an association between condomless anal sex and chemsex among MSM with an odds ratio: 1.54 [17].
Need of this trial
We propose this trial because chemsex, which is an emerging issue among MSM, substantially increases the risk of HIV and STIs infections. In spite of this, there have been very limited research evaluating the effectiveness of interventions or health promotion programmes which specifically aim to reduce the intention to engage in chemsex and the actual chemsex behaviours among MSM.
Aim and objectives
This study aims to evaluate the effectiveness of the interactive internet-based intervention in reducing the sexual harms of chemsex among MSM, with the following four objectives:
-
1.
To strengthen the self-efficacy in refusing risky sexual behaviours and chemsex.
-
2.
To reduce the intention to engage in chemsex and the actual chemsex behaviours.
-
3.
To enhance consistent condom use in both sober and drug-influenced sex.
-
4.
To increase motivation towards the practice of regular HIV/STIs testing.
Hypotheses
We hypothesise that, MSM receiving the internet-based intervention will be more likely to exhibit (i) better self-efficacy in refusing risky sexual behaviours and chemsex, (ii) lower intention to engage in chemsex and the actual chemsex behaviours, (iii) higher condom use consistency and (vi) more HIV and STI testing, compared to MSM in the control group.
Methods
Study design
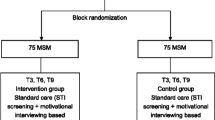
This is a two-armed, randomised, parallel-group trial with a three-month follow-up period.
Participants
The study inclusion criteria are (i) MSM, (ii) cis male, (iii) adult (aged 18 years or older), and (iv) having internet access. People who cannot read and understand Chinese will be not be eligible to the study.
Sample size justification
The sample size is determined based on G*Power, using an independent t-test, to detect a small-to-moderate between-group difference (Cohen’s d = 0.4) in the primary outcome. A minimum sample size of 200 MSM (100 in each group) will be needed to achieve a power of 80% at a 0.05 level of two-sided significance. We anticipate that 20% of the participants will drop out, we will recruit additional 50 (25 in each group) MSM. Therefore, a total of 250 MSM will be recruited.
Sampling frame
To ensure that we can recruit the required number of study participants with a diverse background, we will use multiple recruitment sources for participant recruitment. First, we will collaborate with local non-governmental organisations that target MSM populations in Hong Kong. They will recruit potential participants based on their existing network. Second, we will recruit participants by using social media (such as Instagram and Twitter) and other online platforms (such as forums) that target MSM. Third, we will use snowball sampling for recruitment. In other words, the enrolled participants will be asked to invite and refer potentially interested friends to participate the study. We have used these recruitment strategies to recruit MSM in previous studies, confirming the feasibility of these recruitment methods [18]. It is anticipated that it will require 6 months to recruit 250 MSM.
Online enrolment and consent
We will develop a website for study enrolment. A screening questionnaire will be used to determinate whether the potential participants meet the criteria to participate in the study. Eligible participants will be requested to sign an electronic consent form confirming the study details. They also need to provide contact information. After completing these steps, participants will be asked complete an online baseline questionnaire.
Randomisation and allocation concealment
After completing the baseline questionnaire, participants will be randomly assigned to either the intervention group or control group via a computer-generated block randomisation procedure (with a block size of four for two groups) with a 1:1 randomisation ratio. The computer-generated sequence will be generated by an independent researcher who is not involved in the trial. There will be no stratification. All participants and research team members are blind to allocation sequence. After randomisation, study participants will be automatically guided to the web content associated with their allocation. The participants will be blind.
Intervention group
A meta-analysis of HIV behavioural interventions aimed at reducing the sexual risk behaviour of MSM concluded that interventions using a theoretical basis such as the diffusion of innovations theory and the model of relapse prevention were associated with significantly greater reductions in condomless anal sex than interventions not reporting a theory with an odds ratio: 0.65 [19]. Thus, it is important to develop interventions and health promoting programmes based on theoretical frameworks.
The theory of planned behaviours (TPB) will be used in the current trial to guide the intervention development. According to the TPB, behaviours are primarily determined by intention and perceived control. It theorises that attitudes, perceived norms and behavioural control predict intention [20]. We will employ the TPB in our trial based on the evidence from past studies. First, one meta-analysis reported that the TPB is a strong and appropriate model for predicting sexual behaviours among MSM [21]. Another meta-analysis also supported the use of the TPB as a theoretical framework for designing interventions to reduce sexual risks [22]. Furthermore, a previous study in mainland China found that the TPB could be used to predict syringe sharing behaviours among female injecting-drug users who were also sex workers [23]. A more recent study among MSM in Hong Kong report that three constructs of the TPB measured at baseline were significantly associated with chemsex during the 6-month follow-up period. These constructs included: (i) positive attitudes toward chemsex (adjusted odds ratio: 1.19), (ii) perceived support for chemsex from significant others (adjusted odds ratio: 1.15), and (iii) perceived behavioural control of refraining from chemsex (adjusted odds ratio: 0.76) [24]. Therefore, the TPB is recommended for the present trial.
Rather than adopting a traditional anti-drug approach to combat drug use with sex, this project proposes to intervene from the perspective of harm reduction, primarily with regards to sexual harm. In fact, people engage in chemsex for multiple reasons. While it is difficult for current chemsex users to withdraw drug use in a short period, being empowered to carry out safer sex practices even in drug-influenced situations may be a more effective and realistic way to lower the risks regarding HIV/STI transmission from chemsex. Self-efficacy of such can be further extended to contexts of sober sex, which would also benefit sexual health at the community level. Based on the TPB, the intervention’s aims are:
-
To lower the desire to use drugs at sex by enhancing participants’ knowledge of chemsex, including negative health impacts, risks, social stigmas and legal consequences;
-
To foster a positive attitude towards consistent condom use;
-
To foster a positive attitude toward regular HIV/STI testing;
-
To increase the self-efficacy of refusing chemsex;
-
To improve participants’ perceived self-efficacy in making informed decisions on HIV/STI prevention in both sober and drug-influenced sex; and
-
To set expectations that consistent condom use and regular HIV/STI testing are normative.
We propose an interactive internet-based intervention for the following rationales. First, a Cochrane Review found that interactive computer-based interventions (ICBIs) are effective for sexual health promotion, while also having positive impacts on self-efficacy, intention and sexual behaviours [25]. The definition of ‘interactive intervention’ is that interventions comprise components that require user contributions (e.g. completing knowledge tests, entering personal data and making choices) to produce tailored feedback that is personally relevant to users [26]. Furthermore, the review also found that compared with face-to-face sexual health interventions, ICBIs are more effective [25]. Second, another systematic review and meta-analysis also reported that computer technology-based HIV prevention interventions are effective in reducing risky sexual behaviours [27]. The review also recommended computer technology-based HIV prevention interventions because of their low cost to deliver, the customisability of intervention content and the flexibility of dissemination channels [27]. Third, a systematic review also showed evidence that eHealth for HIV prevention in high-risk MSM has the potential to be effective in the short term for reducing HIV risk behaviours and increasing testing rates [28]. Fourth, a systematic review of mobile-based interventions (including web-based and smartphone application-based interventions) concluded that mobile-based technology is a promising method for addressing substance abuse because the interventions have been shown to reduce substance use among vulnerable individuals [29]. These four systematic reviews provide compelling evidence to support the use of internet-based interventions to prevent chemsex among MSM.
Internet-based interventions have several strengths. First, sexual health, homosexuality and chemsex are considered embarrassing topics in many cultures including the Chinese culture. Internet-based interventions can provide greater privacy and anonymity than traditional face-to-face interventions. Second, unlike traditional face-to-face interventions, participants can access internet-based interventions at their convenience. Third, web-based platforms facilitate data collection. Fourth, the dissemination of web-based interventions is fast and relatively cheap. Finally, and more importantly, in terms of empirical evidence, multiple systematic reviews support the effectiveness of eHealth interventions in promoting HIV-preventive behaviours among MSM [30,31,32]. Therefore, a web-based intervention is recommended for the proposed study.
The time spent on the web-based intervention is expected to be approximately 20 to 30 min for the intervention group. Reminders (via email or instant messaging such as WhatsApp) will be sent to the participants to ask them to access to the web-based intervention again at month 2 to enhance the intervention effect.
Control group
Participants in the control group will receive a web-based intervention without any sexual health information and without any interactive components. The contents for the control group will only include educational materials on general health information. Reminders (via email or instant messaging such as WhatsApp) will be sent to the participants to ask them to access to the web-based intervention again at month 2.
Access to the allocated web content
The study participants will have unlimited access to their allocated contents during the study period. However, the contents will only be available to participants with a registered email address and password to minimise contamination between intervention and control participants. In other words, if the participants need to gain access to their allocated web contents during the study period, they will need to use their registered email address and password to log in.
Study outcomes
The study outcomes in both groups will be measured at baseline (T0) and at 3 months (T1) after baseline. The primary outcomes will be self-efficacy in refusing risky sexual behaviours and chemsex. The secondary outcomes will be (i) intention to have chemsex, (ii) actual chemsex behaviours, (iii) condom use consistency in both sober and drug-influenced sex and (iv) having regular HIV/STI testing.
Study instruments
As there are no existing study instruments to specifically measure self-efficacy in refusing chemsex and risky sexual behaviours, we use (i) the Chinese version of Drug Avoidance Self-Efficacy Scale (DASES), (ii) the Self-Efficacy for Sexual Safety scale and (iii) the traditional Chinese version of the Condom Self-Efficacy Scale (CSES).
-
DASES was developed by Martin et al. [33] to measure drug avoidance self-efficacy. There are 16 items assessing abstinence self-efficacy across different high-risk situations. For each question, study participants are asked to imagine themselves in a particular situation and rate their perceived level of self-efficacy in resisting drug use in that situation. One example of the questions asked is: “Imagine that you are going to a party where you will meet new people. You feel that drug use will relax you and make you more confident. Could you avoid drug use?” A seven-point Likert scale (1 = certainly no to 7 = certainly yes) is used. The total score is obtained by summing across the 16 items, with a higher total score indicating a high level of self-efficacy to resist drug use [33].
-
Self-Efficacy for Sexual Safety consists of seven items. Participants are asked to rate on a five-point scale ranging from ‘strongly disagree’ to ‘strongly agree’ regarding a number of statements. Examples of the statements include: “When I am drunk or high, I can avoid situations that I consider sexually risky” and “When I am drunk or high, I can choose safer sex with a man I have never had sex with before” [34]. A higher score indicates a higher level of self-efficacy for safe sex.
-
CSES has 14 items, covering three subscales: (i) consistent condom use, (ii) correct condom use and (iii) communication. Participants will be asked to rate themselves on a five-point scale ranging from ‘very unsure’ to ‘very sure’ [35]. A higher score indicates a higher level of self-efficacy for condom use.
For the secondary outcomes, participants’ (i) intention to have chemsex, (ii) actual engagement in chemsex, (iii) practice of condomless sex both sober and drug-influenced, and (iv) the number of HIV/STI tests in the previous 3 months will be assessed.
Sociodemographic factors such as age and education level will be collected. Participants will be asked about their relationships and sexual behaviours to investigate elements such as preferred sexual position (top/bottom/versatile), frequency of condom use, number of sexual partners, relationship status, etc.
Table 1 shows the SPIRIT diagram for the schedule of enrolment, intervention and assessment.
Data analysis
All continuous outcomes will be analysed using the linear mixed-effects model, with the intervention group as the independent variable and adjusting for baseline characteristics as covariates. Similarly, a generalized linear mixed-effects model with logit link will be used to analyse the binary outcomes. The intention-to-treat principle will be adopted, and all study subjects will be randomised and included in the analysis. Missing values at the three-month follow-up will be handled by the model without the need of imputation.
Discussion
International and local data have both suggested that chemsex is not uncommon among MSM. The negative impacts of chemsex is multifaceted including mental health, increased risks of HIV and STIs, and social functioning [1]. Importantly, chemsex is in general carried out alongside other risky sexual activities and therefore poses a threat regarding the spread of HIV and other STIs in the community [1]. However, compared with other areas, such as promoting condom use among MSM and drug prevention among the general population, little work has been done on the primary prevention of chemsex among MSM, particularly in Hong Kong.
To the best of our knowledge, this will be the first interactive internet-based intervention specifically targeting chemsex among MSM. This project can help to develop and test culturally relevant health promotion programmes in reducing chemsex among MSM. This internet-based intervention, if found successful, will have important clinical and policy implications, as it could be adopted by governmental and non-governmental organisations targeting MSM. The programme will also raise the awareness of MSM regarding safe sex practices such as the consistent use of condoms and the importance of having regular HIV/STI check-ups. Eventually, they may be empowered to reduce their participation in risky sexual behaviours, leading to the decrease in HIV/STI transmission in the MSM community.
Using an online delivery mode, the intervention is capable of reaching a large population of targets at a relatively low cost. As such, it has the potential to reduce the public health burden of chemsex and other risky sexual behaviours among MSM in a cost-effective manner. Ultimately, we expect this intervention could be modified and implemented throughout the entire Hong Kong community.
Limitation
First, the study will be conducted in the Chinese population only. The applicability of the study findings in other populations is uncertain. Second, the follow-up period is relatively short. The long-term effectiveness of the intervention is therefore unknown. The acceptability of this internet-based intervention among people with low computer literacy is not sure.
Conclusion
This programme is the first attempt to develop an online intervention to reduce sexual harm related to chemsex among MSM. The study will provide evidence that is readily translatable to real-life practice through a territory-wide campaign promoting sexual health. If the online intervention is effective, it could be adopted as a relatively low-cost, sustainable community-based health promotion strategy by sexual health clinics, as well as community centres that target MSM. We expect the study to have a clinical impact on future development and implementation of online interventions for MSM both locally and globally.
Availability of data and materials
The data sharing plans for the current study are unknown and will be made available at a later date.
Abbreviations
- CSES:
-
Condom Self-Efficacy Scale
- DASES:
-
Drug Avoidance Self-Efficacy Scale
- HIV:
-
Human immunodeficiency virus
- ICBIs:
-
Interactive computer-based interventions
- ISRCTN:
-
International standard randomized controlled trial number
- MSM:
-
Men who have sex with men
- RCT:
-
Randomised control trial
- STIs:
-
Sexually transmitted infections
- TPB:
-
Theory of planned behaviour
References
Maxwell S, Shahmanesh M, Gafos M. Chemsex behaviours among men who have sex with men: a systematic review of the literature. Int J Drug Policy. 2019;63:74–89. https://doi.org/10.1016/j.drugpo.2018.11.014.
Chow EP, Grulich AE, Fairley CK. Epidemiology and prevention of sexually transmitted infections in men who have sex with men at risk of HIV. Lancet HIV. 2019;6(6):e396–405. https://doi.org/10.1016/S2352-3018(19)30043-8.
Chow EP, Ong JJ, Vodstrcil LA, Fairley CK. Drug use and the influence on kissing among men who have sex with men in Melbourne, Australia. Int J STD AIDS. 2020;31(1):16–21. https://doi.org/10.1177/0956462419878338.
Sewell J, Miltz A, Lampe FC, Cambiano V, Speakman A, Phillips AN, et al. Poly drug use, chemsex drug use, and associations with sexual risk behaviour in HIV-negative men who have sex with men attending sexual health clinics. Int J Drug Policy. 2017;43:33–43. https://doi.org/10.1016/j.drugpo.2017.01.001.
Evers YJ, Geraets JJ, Van Liere GA, Hoebe CJ, Dukers-Muijrers NH. Attitude and beliefs about the social environment associated with chemsex among MSM visiting STI clinics in the Netherlands: an observational study. PLoS One. 2020;15(7):e0235467. https://doi.org/10.1371/journal.pone.0235467.
Glynn RW, Byrne N, O’Dea S, Shanley A, Codd M, Keenan E, et al. Chemsex, risk behaviours and sexually transmitted infections among men who have sex with men in Dublin, Ireland. Int J Drug Policy. 2018;52:9–15. https://doi.org/10.1016/j.drugpo.2017.10.008.
Hoornenborg E, Coyer L, van Laarhoven A, Achterbergh R, de Vries H, Prins M, et al. Change in sexual risk behaviour after 6 months of pre-exposure prophylaxis use: results from the Amsterdam pre-exposure prophylaxis demonstration project. AIDS. 2018;32(11):1527–32. https://doi.org/10.1097/QAD.0000000000001874.
The Hong Kong Jockey Club Drug InfoCentre. https://www.druginfocentre.hk/bdf/Uploads/Files/150012/150012%20Research%20R.pdf. Accessed 20 Mar 2021.
Narcotics Division, Secruity Bureau, The Government of the Hong Kong Special Administrative Region of the People’s Republic of China. https://www.nd.gov.hk/pdf/BDF150026.pdf. Accessed 20 Mar 2021.
Choi EP, Wong JY, Lo HH, Wong W, Chio JH, Fong DY. Association between using smartphone dating applications and alcohol and recreational drug use in conjunction with sexual activities in college students. Subst Use Misuse. 2017;52(4):422–8. https://doi.org/10.1080/10826084.2016.1233566.
Wong NS, Kwan TH, Lee KCK, Lau JYC, Lee SS. Delineation of chemsex patterns of men who have sex with men in association with their sexual networks and linkage to HIV prevention. Int J Drug Policy. 2020;75:102591. https://doi.org/10.1016/j.drugpo.2019.10.015.
Choi KW, Choi EP, Chow EP, Wan EY, Wong WC, Wong JY, et al. The experience of using dating applications for sexual hook-ups: a qualitative exploration among HIV-negative men who have sex with men in Hong Kong. J Sex Res. 2021:1–10. https://doi.org/10.1080/00224499.2021.1886227.
Ma R, Perera S. Safer ‘chemsex’: GPs’ role in harm reduction for emerging forms of recreational drug use. In. Br J Gen Pract. 2016;66(642):4–5. https://doi.org/10.3399/bjgp16X683029.
McCormack S, Dunn DT, Desai M, Dolling DI, Gafos M, Gilson R, et al. Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. Lancet. 2016;387(10013):53–60. https://doi.org/10.1016/S0140-6736(15)00056-2.
Hibbert MP, Brett CE, Porcellato LA, Hope VD. Psychosocial and sexual characteristics associated with sexualised drug use and chemsex among men who have sex with men (MSM) in the UK. Sex Transm Infect. 2019;95(5):342–50. https://doi.org/10.1136/sextrans-2018-053933.
Kenyon C, Wouters K, Platteau T, Buyze J, Florence E. Increases in condomless chemsex associated with HIV acquisition in MSM but not heterosexuals attending a HIV testing center in Antwerp, Belgium. AIDS Res Ther. 2018;15(1):1–6.
Khaw C, Zablotska-Manos I, Boyd MA. Men who have sex with men and chemsex: a clinic-based cross-sectional study in South Australia. In: Sexuality research and social policy; 2020. p. 1–9.
Choi EP, Chow EP, Wan EY, Wong WC, Wong JY, Fong DY. The safe use of dating applications among men who have sex with men: a study protocol for a randomised controlled trial to evaluate an interactive web-based intervention to reduce risky sexual behaviours. BMC Public Health. 2020;20(1):1–7.
Herbst JH, Sherba RT, Crepaz N, DeLuca JB, Zohrabyan L, Stall RD, et al. A meta-analytic review of HIV behavioral interventions for reducing sexual risk behavior of men who have sex with men. J Acquir Immune Defic Syndr. 2005;39(2):228–41.
Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. https://doi.org/10.1016/0749-5978(91)90020-T.
Andrew BJ, Mullan BA, de Wit JB, Monds LA, Todd J, Kothe EJ. Does the theory of planned behaviour explain condom use behaviour among men who have sex with men? A meta-analytic review of the literature. AIDS Behav. 2016;20(12):2834–44. https://doi.org/10.1007/s10461-016-1314-0.
Tyson M, Covey J, Rosenthal HE. Theory of planned behavior interventions for reducing heterosexual risk behaviors: a meta-analysis. Health Psychol. 2014;33(12):1454–67. https://doi.org/10.1037/hea0000047.
Gu J, Lau JT, Chen H, Tsui H, Ling W. Prevalence and factors related to syringe sharing behaviours among female injecting drug users who are also sex workers in China. Int J Drug Policy. 2011;22(1):26–33. https://doi.org/10.1016/j.drugpo.2010.06.005.
Wang Z, Yang X, Mo PK, Fang Y, Ip TKM, Lau JT. Influence of social media on sexualized drug use and chemsex among Chinese men who have sex with men: observational prospective cohort study. J Med Internet Res. 2020;22(7):e17894. https://doi.org/10.2196/17894.
Bailey JV, Murray E, Rait G, Mercer CH, Morris RW, Peacock R, et al. Interactive computer-based interventions for sexual health promotion. Cochrane Database Syst Rev. 2010;(9). https://doi.org/10.1002/14651858.CD006483.pub2.
Bellis JM, Grimley DM, Alexander LR. Feasibility of a tailored intervention targeting STD-related behaviors. Am J Health Behav. 2002;26(5):378–85. https://doi.org/10.5993/AJHB.26.5.6.
Noar SM, Black HG, Pierce LB. Efficacy of computer technology-based HIV prevention interventions: a meta-analysis. AIDS. 2009;23(1):107–15. https://doi.org/10.1097/QAD.0b013e32831c5500.
Schnall R, Travers J, Rojas M, Carballo-Diéguez A. eHealth interventions for HIV prevention in high-risk men who have sex with men: a systematic review. J Med Internet Res. 2014;16(5):e134. https://doi.org/10.2196/jmir.3393.
Kazemi DM, Borsari B, Levine MJ, Li S, Lamberson KA, Matta LA. A systematic review of the mHealth interventions to prevent alcohol and substance abuse. J Health Commun. 2017;22(5):413–32. https://doi.org/10.1080/10810730.2017.1303556.
Xin M, Viswanath K, Li AY-C, Wangnan C, Yuhong H, Lau JT-F, et al. The effectiveness of electronic health interventions for promoting HIV-preventive behaviors among men who have sex with men: meta-analysis based on an integrative framework of design and implementation features. J Med Internet Res. 2020;22(5):e15977. https://doi.org/10.2196/15977.
Nguyen LH, Tran BX, Rocha LE, Nguyen HLT, Yang C, Latkin CA, et al. A systematic review of eHealth interventions addressing HIV/STI prevention among men who have sex with men. AIDS Behav. 2019;23(9):2253–72. https://doi.org/10.1007/s10461-019-02626-1.
Nelson KM, Perry NS, Horvath KJ, Smith LR. A systematic review of mHealth interventions for HIV prevention and treatment among gay, bisexual, and other men who have sex with men. Transl Behav Med. 2020;10(5):1211–20. https://doi.org/10.1093/tbm/ibaa007.
Martin GW, Wilkinson DA, Poulos CX. The drug avoidance self-efficacy scale. J Subst Abus. 1995;7(2):151–63. https://doi.org/10.1016/0899-3289(95)90001-2.
Alvy LM, McKirnan DJ, Mansergh G, Koblin B, Colfax GN, Flores SA, et al. Depression is associated with sexual risk among men who have sex with men, but is mediated by cognitive escape and self-efficacy. AIDS Behav. 2011;15(6):1171–9. https://doi.org/10.1007/s10461-010-9678-z.
Zhao Y, Wong CKH, Miu HYH, Yuen WWY, Chin WY, Luo T, et al. Translation and validation of a condom self-efficacy scale (CSES) Chinese version. AIDS Educ Prev. 2016;28(6):499–510. https://doi.org/10.1521/aeap.2016.28.6.499.
Acknowledgments
We would like to thank Dr. Garth Martin, the original author of the DASES and the Narcotics Division, Security Bureau, The Government of the Hong Kong Special Administration Region for the permission to use the tradition Chinese version of the DASES in the current study.
Funding
The study was sponsored by the Council for the AIDS Trust Fund, reference number: MSS 338 R.
This HIV/AIDS prevention part of project/ programme is sponsored by the AIDS Trust Fund. The content of this article represents the opinion of our organization only. It does not represent the position of the AIDS Trust Fund. AIDS Trust Fund is not responsible for any claims, demands or liabilities whatsoever arising from or in connection with the use of any information contained in this article or the participation of the sponsored project/ programme.
E.P.F.C. is supported by an Australian National Health and Medical Research Council (NHMRC) Emerging Leadership Investigator Grants (GNT1172873) outside the submitted work.
Author information
Authors and Affiliations
Contributions
EPHC is the principle investigator of the project. EPFC, PHC, WCWW, KWYC and JYYK are the collaborators of the project. All authors have been involved in revising the manuscript and read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (HKU/HA HKW IRB), reference number: UW 20–650. Electronic informed consent will be obtained for each study participant. We will strictly follow the Consolidated Standards of Reporting Trials (CONSORT) statement and the International Conference of Harmonisation Guidelines for Good Clinical Practice.
Consent for publication
Not applicable.
Competing interests
EPFC has received research funding and honoraria to his institute from Gilead Sciences SL on HIV/STI research outside of the submitted work. All other authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Choi, E.P.H., Chau, P.H., Wong, W.C.W. et al. Developing and testing of an interactive internet-based intervention to reduce sexual harm of sexualised drug use (‘chemsex’) among men who have sex with men in Hong Kong: a study protocol for a randomised controlled trial. BMC Public Health 21, 713 (2021). https://doi.org/10.1186/s12889-021-10742-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-021-10742-8