Abstract
Background
Obesity is characterized by excessive fat accumulation in the body. Physical activity (PA) is an effective intervention to combat obesity, but the effectiveness of different PA patterns on controlling obesity is unclear. Lipid accumulation product (LAP), derived from waist circumference and triglycerides, is a novel indicator for obesity evaluation. However, the association between PA patterns (i.e., weekend warriors and regularly active) and LAP remains unexplored. This study aims to elucidate the relationship between PA patterns and LAP in US adult population.
Methods
Adult individuals with complete data on LAP, PA patterns, and other covariates from the National Health and Nutrition Examination Survey (NHANES) database (2007–2018) were included in this study. Multivariate linear regression models were utilized to explore the association between PA patterns and LAP. Subgroup analyses, interaction tests, restricted cubic spline (RCS) regression analyses, and threshold and saturation effect analyses were also performed to investigate the stability and nonlinearity of PA-LAP association, respectively.
Results
A total of 11,212 participants were included in this study. After adjusting for all potential covariates, being regularly active (RA) (β=-8.85, P < 0.05) obtained significantly higher LAP reduction as opposed to being weekend warriors (WWs) (β=-4.70, P = 0.3841). Furthermore, subgroup analyses and interaction tests indicated that the PA-LAP association was more pronounced in individuals with higher education levels (P interaction = 0.0084) and diabetes (P interaction = 0.0062). Additionally, a significant, non-linear, and negative correlation between weekly total PA and LAP in non-inactive individuals was identified by RCS analysis (P for overall < 0.001, P for nonlinearity = 0.009). A threshold of 440 min in weekly total PA was found to arouse favorable LAP reduction.
Conclusions
Being regularly active obtained better LAP reduction as opposed to being WWs. For non-inactive adults, engaging in more than 440 min of PA per week helps to reduce LAP effectively.
Similar content being viewed by others
Introduction
Obesity is a multifactorial disease characterized by excess body fat accumulation, which is tightly linked to various unfavorable health outcomes, including hypertension [1], diabetes [2], cardiovascular diseases (CVD) [2], cancers [3], etc. Since 1980, the global obesity prevalence has surged significantly and continues to escalate rapidly [4], making it a serious public health problem worldwide. Therefore, studies concentrating on unraveling obesity pathogenesis, identifying evaluation biomarkers, or developing effective obesity management strategies are urgently needed now.
Since the harm of obesity is primarily derived from metabolic disturbance, including insulin resistance, dyslipidemia, glucose intolerance, etc [5]., a stable and reliable obesity reflective indicator is the pivotal prerequisite for developing obesity interventional strategies. Previous studies have indicated that obese individuals without metabolic abnormalities (namely metabolically healthy/normal obesity) do not get additional risks for suffering cardiometabolic diseases [6]. Therefore, metabolic indicators should be included in establishing obesity reflective indicators. Besides, significant changes in body anthropometrics usually occurred among obese individuals, such as waist circumference, sagittal abdominal diameter, BMI, and so on [7]. Given this, obesity indicators composed of metabolic and anthropometric indexes may be more reflective for the onset and progression of obesity.
Lipid accumulation products (LAP) is a sex-specific indicator calculated from waist circumference (WC) and triglycerides (TG), which is a pivotal index for various metabolic disorders, especially obesity [8]. Although BMI is an easily-accessible indicator for defining obesity, it fails to evaluate the underlying fat distribution and metabolic disorders of obesity. As opposed to BMI, LAP can provide a more precise evaluation of the extent of fat accumulation, and a higher LAP level usually indicates more severe fat accumulation [9,10,11]. Additionally, substantial evidences have proved that LAP plays critical roles in various aspects, including diagnosing metabolic syndrome, evaluating risks for diabetes and CVD, serving as key parameter to measure the efficacy of interventions targeted at improving metabolic syndrome [12]. Therefore, LAP can be utilized as a reliable and accurate indicator to detect dynamic alterations of fat accumulation and metabolic disorder in obese individuals.
In parallel with dietary, behavioral, and medication interventions, physical activity (PA) is acknowledged as a“pillar” in combating overweight and obesity [13]. Although a minimum of 150 min of moderate physical activity (MPA), or 75 min of vigorous physical activity (VPA), or equivalent combination of MPA and VPA per week was recommended by World Health Organization to improve cardiovascular health, such levels of weekly total PA are reported to be inadequate to arouse clinically significant weight loss or maintain weight without caloric restriction [14, 15]. Even worse, existing evidences have revealed that approximately 80% of adults and adolescents in the United States failed to meet the recommended minimal level of PA per week (i.e., being insufficiently active) [16]. With the increasing pace of global society, adhering to being regular active (RA) may become challenging for individuals with busy schedules. So, the recent years have witnessed a gradual increase of a new PA pattern, namely weekend warriors (WWs), which means individuals choose to complete at least 150 min of moderate-to-vigorous physical activity (MVPA) within 1 ~ 2 sessions per week [17]. Numerous studies have suggested that being WWs reaps similar health benefits in various aspects as being RA, such as reducing all-cause/ CVD/cancer mortality [18], lowering risks for diabetes [19], mitigating frailty levels [20], alleviating symptoms from depression or psychological distress [21, 22], and so on. However, there is study reporting conflicting results that being WWs (OR, 1.28; 95%CI, 1.02–1.65) obtained significantly higher risks for developing metabolic syndrome compared to being RA [23]. Therefore, even though the beneficial effects of PA has been acknowledged, whether WWs reap equivalent benefits in combating obesity and improving obesity-related metabolic disorders still remains unknown.
Given this, in this study, we mainly focused on exploring the association between different PA patterns and LAP (an obesity indicator) with the dataset from NHANES. Our results may provide PA reference for those obese individuals who are searching their suitable PA patterns.
Materials and methods
Study design and population
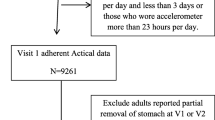
The NHANES survey, conducted by the CDC, has been an ongoing investigation of the population since 1999. This study utilizes a complex and stratified probability sampling method, releasing data every two years [24]. Prior to the interviews and examinations, informed consent was obtained from all participants [25]. For this research, we analyzed data from six consecutive NHANES cycles spanning from 2007 to 2008 to 2017–2018, including a total of 59,842 individuals. Adult participants (≥ 20 years old) with incomplete information on body measurements (height, weight, waist circumference, and hip circumference), serum total cholesterol and triglycerides, physical activity, demographic variables (age, gender, race, education, PIR, and marital status), as well as behavioral and health factors (smoking, drinking, CVD, and diabetes) were excluded from the analysis. Ultimately, a total of 11,212 participants was included in the study. The criteria for participants selection in the current study was presented in Fig. 1.
Lipid accumulation products (LAPs) assessment
Each participant underwent a household interview and completed a physical examination at the Mobile Examination Center [26]. The measurements of standing height (cm), weight (kg), waist circumference (cm), and hip circumference (cm) were measured using standardized protocols [27]. Blood samples were collected after a fasting period of at least 8 h overnight. Venous blood samples from the participants used for serum total cholesterol and triglycerides (TG) examinations were collected and processed according to the NHANES protocols [28]. The LAP was calculated by using sex-specific formula: LAP=[waist circumference (cm)-65] * TG (mmol/L) for male and [waist circumference (cm)-58] * TG (mmol/L) for female [29].
PA and other covariates
PA was assessed by using a PA questionnaire. Participants were asked about the frequency and duration of vigorous and moderate sports, fitness, and recreational activities that lasted for at least 10 continuous minutes in a typical week. PA was calculated by combining the frequency (sessions per week) and duration (duration per time) of these activities. Previous studies have revealed that 1 min of vigorous-intensity activity (VPA) was equivalent to 2 min of moderate physical activity (MPA) [16]. Therefore, total PA was calculated by using the following formula: 2 * vigorous PA + moderate PA. As previously described [18], the activity patterns can be divided into four groups according to self-reported leisure time PA: (1) inactive group (reporting no vigorous or moderate PA), (2) insufficiently active group (reporting less than 150 min per week of total PA), (3) weekend warriors group (reporting at least 150 min of total PA weekly in 1 or 2 sessions), and (4) regularly active group (reporting at least 150 min of total PA weekly in more than 2 sessions). The definition for different PA patterns was presented in Fig. 2.
Based on previous studies, some essential covariates were included in this study, including demographics data, behavioral risk factors, and chronic non-communicable diseases [21, 30, 31]. The demographic covariates included gender, age (≤ 45, 45–65, > 65 years), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, other), marital status (married/live with partner, divorced/separated/widowed, never married), educational level (less than 9th grade, high school or equivalent, some college or above), and poverty income ratio (PIR) (≤ 1.3, 1.3–3.5, > 3.5). Additional covariates included participants’ behavioral risk factors such as smoking and drinking [32, 33], as well as disease status including diabetes and cardiovascular disease (CVD) [34, 35]. Smoking status was evaluated by the answer to the question of “Have you smoked at least 100 cigarettes in your entire life?”, and those who answered “yes” were defined as smokers, otherwise defined as nonsmokers. Drinking was evaluated by the answer to the question of “Had at least 12 alcohol drinks in any one year?”, and those who answered “yes” were defined as drinkers, otherwise defined as nondrinkers. Body mass index (BMI) was determined using the standard formula (weight/height2) based on measured weight (kg) and height (m). Participants were further divided into three groups by BMI based on the criterion from World Health Organization (WHO) [13], including normal or low body weight (< 25 kg/m2), overweight (25–30 kg/m2), and obese (> 30 kg/m2).
Statistical analysis
The baseline characteristics of all participants were presented based on the grouping of different PA pattern groups. Variables which are not normally distributed were presented as median (Q1-Q3, interquartile), and categorical variables were presented as numbers and percentages. The differences in baseline characteristics were compared by using Rao-Scott chi-squared test or Kruskal-Wallis test. Multivariate linear regression models were utilized to explore the association between PA patterns and LAP. Additionally, subgroup analyses, interaction tests and restricted cubic spline regression analyses were employed to investigate the robustness and nonlinearity of PA-LAP association, respectively. Furthermore, when a non-linear association between total PA and LAP was determined, a recursive algorithm was employed to compute the inflection point for total PA, and a bi-segmented linear regression model was also established to evaluate the differences before and after the inflection point [36]. Statistical analyses were performed by using R software (version 4.3.1, https://www.r-project.org/). A two-sided P-values < 0.05 were considered statistically significant.
Results
Baseline characteristics of the study population
As is shown in Fig. 1, a total of 59,842 participants from 2007 to 2018 were preliminarily included in this study. Participants who had missing data on body measurements (height, weight, waist circumference, and hip circumference), serum total cholesterol and triglycerides, physical activity, demographic variables (age, gender, race, education, PIR, and marital status), as well as behavioral and health factors (smoking, drinking, CVD, and diabetes) were excluded from the analysis. Ultimately, a total of 11,212 participants was included in the study.
The baseline characteristics of participants in different PA pattern groups were presented in Table 1. The sample analyzed consisted of 11,212 participants, including 7,267 inactive individuals, 192 insufficiently active individuals, 122 weekend warriors, and 3,631 regularly active individuals. Participants in different PA pattern groups exhibited significant differences in variables of gender, age, race, educational level, marital status, PIR, diabetes, smoking, drinking, BMI and CVD. Specifically, compared those who in inactive group, participants belonged to WWs group were more likely to be male, aged under 45 years, non-Hispanic White, have higher level of education and PIR, be non-smokers and nondrinkers, and with no CVD or diabetes.
Differences in PA parameters among different PA pattern groups
The characteristics of PA among different PA pattern groups were presented in Supplementary Table 1. Except for sedentary time, regularly active group exhibited higher levels of PA parameters as opposed to WWs group, insufficiently active group and inactive group, including VPA/MPA sessions per week, VPA/MPA time per session, total VPA/MPA per week, total MVPA and total PA per week (all P values < 0.001).
Association between PA patterns and LAP
In order to clarify the relationship between PA patterns and LAP, the LAP levels between different PA groups were firstly compared. As is depicted in Fig. 3, regularly active individuals obtained significant reduced LAP level as opposed to other three PA pattern groups (P < 0.05). Although being insufficiently active or WWs got notable LAP reduction compared with being inactive (P < 0.05), no significant differences in LAP reduction were found between being insufficiently active and being WWs (P = 0.47).
Furthermore, multivariate linear regression models were subsequently performed to explore the PA-LAP association, and the results were presented in Tables 2 and Fig. 4. Compared with inactive group, only the regularly active group got significant LAP reduction in non-adjusted model (Model 1, β=-26.98, P < 0.0001), partially-adjusted model (Model 2, β=-21.96, P < 0.0001) and fully-adjusted model (Model 3, β=-8.85, P < 0.0001). Conversely, when the regularly active group was defined as the reference group, being inactive significantly associated with notable LAP increase in all models (Model 1, β = 26.98, P < 0.0001; Model 2, β = 21.96, P < 0.0001; Model 3, β = 8.85, P < 0.0001). Noteworthily, although WWs group didn’t obtain significant LAP reduction as regularly active group, WWs indeed achieve certain LAP reduction, which was reflected by the value of β in all models (β=-12.65, -16.11, -4.70 for model 1, 2 and 3, respectively).
Given that the reported mutual associations between PA and diabetes, BMI and CVD, and the correlations between LAP and diabetes, BMI and CVD in previous studies [37,38,39], potential multicollinearity or collider bias may existed among these variables. Therefore, multivariate linear regression models were further performed without adjusting for the variables of diabetes, BMI and CVD. Our results revealed a similar, consistent and significant trend in LAP reduction between the two regression models with or without adjusting for diabetes, BMI and CVD (Supplementary Table 2).
Subgroup analyses
To further confirm the robustness and stability of the association between PA pattern and LAP, subgroup analyses based on grouping of vital covariates were performed. As presented in Table 3, the correlations between PA patterns and LAP remained consistent across different subgroups stratified by the variables of gender, age, race, marital status, PIR, smoking, drinking, CVD and BMI. Additionally, interaction tests revealed that the associations between PA patterns and LAP were modified by the variables of education level and diabetes, individuals being regularly active obtained more pronounced LAP reduction in two subgroups, including individuals with higher education level (P interaction = 0.0084), and with diabetes (P interaction = 0.0062).
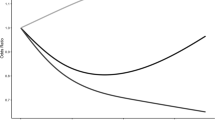
Dose-response relationships between total PA and LAP
RCS analyses were employed to explore the potential non-linear relationship between weekly total PA and LAP in non-inactive individuals. The results, as presented in Fig. 5, suggested a significant, non-linear, and negative correlation between weekly total PA and LAP (P < 0.001, P for nonlinearity = 0.009). Additionally, threshold effect and saturation effect analyses were conducted to identify the inflection point for total PA, with the results presented in Table 4. An inflection point of 440 min for weekly total PA was identified (Fig. 5) and significant differences were observed before and after the inflection point by using the bi-segmented linear regression model (effect size difference of 2 vs. 1, P < 0.0001). The entire group was subsequently divided into two subgroups based on the identified inflection point, individuals who performed over 440 min of PA weekly obtained significantly higher LAP reduction in all multivariate linear regression models (Table 5), with the β being − 21.516, -16.461 and − 7.759 in model 1, 2 and 3, respectively.
RCS analysis to explore the association between weekly total PA and LAP in all participants. Variables of age, gender, race, education, PIR, marital status, smoking, CVD, diabetes, drinking, and BMI were adjusted during RCS analyses. Abbreviations: RCS, restricted cubic spline; LAP, lipid accumulation product; CVD, cardiovascular disease; BMI, body mass index; PIR, ratio of family income to poverty
Except for the above-mentioned analyses, the non-linear relationship between weekly total PA and LAP in different subgroups were also performed by using RCS analyses, with the results being presented in Fig. 6. No significant and non-linear associations between weekly total PA and LAP were identified in insufficiently active group (P = 0.936, P for nonlinearity = 0.917; Fig. 6A) and WWs group (P = 0.477, P for nonlinearity = 0.227; Fig. 6B). In contrast, a negative and non-linear association between weekly total PA and LAP were found in the regularly active group (P = 0.001, P for nonlinearity = 0.033; Fig. 6C). As depicted in Fig. 7, the weekly sedentary time was found to be positively and linearly associated with LAP in the entire group as opposed to total PA in a week (P = 0.024, P for nonlinearity = 0.089).
Identification of the association between weekly total PA and LAP by RCS analyses. (A) Insufficiently active group; (B) Weekend warriors group; (C) Regularly active group. Variables of age, gender, race, education, PIR, marital status, smoking, CVD, diabetes, drinking, and BMI were adjusted during RCS analyses. Abbreviations: RCS, restricted cubic spline; LAP, lipid accumulation product; CVD, cardiovascular disease; BMI, body mass index; PIR, ratio of family income to poverty
RCS analysis illustrated the association between weekly sedentary time and LAP. Variables of age, gender, race, education, PIR, marital status, smoking, CVD, diabetes, drinking, and BMI were adjusted during RCS analyses. Abbreviations: RCS, restricted cubic spline; LAP, lipid accumulation product; CVD, cardiovascular disease; BMI, body mass index; PIR, ratio of family income to poverty
Discussion
In this study, we mainly focused on elucidating the association between PA patterns and LAP. Our results firstly revealed that only the PA pattern of RA was associated with significant LAP reduction as opposed to other PA patterns in the non-adjusted, partially-adjusted and fully-adjusted linear regression models. Noteworthily, being WWs didn’t harvest equivalent and significant LAP reduction as being RA. Furthermore, subgroup analyses demonstrated that the RA-LAP association remained consistent in all strata except for the variables of education and diabetes, which were proved to pose significant modification effects on the association, with the RA-LAP association being more pronounced in individuals with higher education level and diabetes. Besides, a significant, non-linear, and negative correlation between weekly total PA and LAP has been identified by RCS analysis, and an inflection point of 440 min for weekly total PA was determined by using threshold effect and saturation effect analyses, with significant differences being observed before and after the inflection point by using the bi-segmented linear regression model. Additionally, RCS analyses in subgroups suggested that significant, negative and non-linear association between weekly total PA and LAP were only found in RA group, but not in insufficiently active group or WWs group. In contrast with the weekly total PA, the weekly sedentary time was found to be significantly, positively and linearly associated with LAP in the entire group.
Previous studies have demonstrated that being WWs reaps similar healthy benefits in various aspects, including lowering the risk for incident cardiovascular events [40], reducing all-cause/CVD/cancer mortality risks [18], reducing the risk of depression symptoms [22, 30], decreasing visceral adiposity index [41], and so on. However, in this study, we discovered that only being RA got significantly LAP reduction, while being WWs did not obtain equivalent LAP reduction as expected, which is different from previous findings. Such discrepancy may be attributed to the following aspects. Since the health benefits from PA were principally depended on three PA parameters, namely frequency, duration and intensity, the differences in LAP reduction between RA group and WWs group can be analyzed from the three aspects. Firstly, previous studies have revealed that there was an minimal exercise threshold to bring about metabolic changes and thus controlling obesity. For example, exercise consuming approximately 1200 to 1600 kcal per week (i.e., performing MPA 3 to 5 times per week, equivalent to 7 ~ 14 miles) may be enough to result in favorable changes in HDL-C metabolism and thus reduced coronary heart disease mortality [42]. Therefore, although being WWs have reached total PA level of 150 min, which may be not enough to arouse changes in lipid metabolism. Actually, our findings suggested that the median of weekly total PA in WWs group was 300 min, which was obviously lower than the threshold (440 min) to reap significant LAP reduction and the median of weekly total PA in RA group (540 min). Furthermore, research conducted by Ryuki Hashida et al. demonstrated that completing exercise for a minimum of 40 ~ 45 min per session, three times a week for a duration of 12 weeks, regardless of aerobic or resistance exercise, can result in significant improvement in hepatic steatosis [43]. This suggests that engaging in exercise solely during two sessions (as WWs) may not be adequate to improve metabolic status. Additionally, an earlier study reported that the amount and frequency of PA, instead of mode and intensity of PA, was more important to affect glycaemic control in patients with type 2 diabetes [44]. Patients are advised to conduct more times of PA per week than increase the duration of per session or exercise intensity to maximize their glycaemic control. This implies that WWs may be not suitable for patients with metabolic disorders. Besides, a research performed by Suk-Yong Jang et al. suggested that being WWs (OR = 1.29, 95%CI:1.02–1.65) obtained significantly higher likelihood to develop metabolic syndrome than the RA group [23], which suggested that being WWs may arouse metabolic disorders and thus hindered the beneficial effects of PA. Finally, previous studies have suggested that continuous and long-term MPA is crucial for eliminating excess visceral fat in obese women [45], which also highlighted the importance of frequency and duration of PA in a week in reducing fat accumulation. Briefly, our results preliminary indicated that being regularly active and simultaneously reach a certain amount of PA can help to combat obesity and control LAP effectively.
In addition to the above-mentioned findings, we also found that the associations between PA patterns and LAP was modified by the variables of diabetes and education level. Participants included in the subgroup of higher education levels and complicated with diabetes showed more pronounced associations between PA pattern and LAP. Previously, amounting evidences have illustrated that patients with diabetes were usually significantly associated with higher LAP level [46], and LAP can be served as one of the effective discriminators for prediabetes and diabetes [47, 48]. Therefore, those who are obese and complicated with diabetes may obtain a higher LAP level than those who not. Given that regular exercise per se was one of the most effective interventional strategies to control diabetes and combating obesity, being RA may obtain more pronounced LAP reduction in obese individuals with diabetes. Besides, Diego Montano has reported that cardiometabolic risk was tightly associated with education differences, individuals with lower education levels got significantly higher cardiometabolic risk compared with those who were higher educated [49]. Education differences were found in multiple obesity-related indexes, including glycated haemoglobin, total cholesterol and BMI [49]. Education may modify the association between PA pattern and LAP in a rather complexed way, possibly via modulating the behavior, attitude and adaptation to PA.
According to the 2020 guidelines on PA from the World Health Organization, all adults are recommended to undertake 150 ~ 300 min of MPA, or 75–150 min of VPA, or the equivalent combination of MPA and VPA, per week [14]. The defined threshold of MVPA in 300 min for adults was based on the evidence that many of the benefits from PA began to occur when the average weekly PA volumes reach 300 min [14]. Previous studies have indicated a curvilinear dose-response association between PA volume and health outcomes, such as CVD mortality, diabetes, and so on [14]. As PA volume increases, additional benefits may be obtained, but such benefits may diminish at higher levels of PA, which is difficult to specify and it may vary in different health conditions [14]. Therefore, there is an interval between 300 min and a threshold level of PA to reap continuous improvement in health benefits. In this study, a threshold of 440 min for weekly total PA was identified by saturation and threshold effects analysis. A rapidly decreased trend in LAP levels was found as total PA increased before this inflection point (0 ~ 440), while the reduction rate of LAP remained relatively high and did not change significantly despite further increases in total PA. Therefore, it is recommended to do at least 440 minutes’ (approximately ≥ 62 min/daily) MVPA per week to achieve favorable LAP reduction. The results from our study, combined with the 2020 PA guidelines from the World Health Organization, have demonstrated that a minimal PA of 300 min per week is needed to keep one’s fundamental fitness, but additional PA is required in order to achieve a specific health goal (e.g., combating obesity or controlling LAP).
Our study possesses several advantages. It represents the first investigation to examine the correlation between the obesity-specific evaluation index LAP and various PA patterns. Stratified analyses, combined with the interaction tests were employed the robustness of PA-LAP association. Additionally, we innovatively employed RCS curves to illustrate the non-linear relationship between total PA and LAP. However, some limitations should be acknowledged in this study. Firstly, due to the cross-sectional analysis, causal relationships between different PA patterns and LAP cannot be deduced. Secondly, the self-reported measurement of PA may be not as accurate as the measurement of PA via accelerometry for the reason that self-reports may overestimate duration and intensity of PA, as reported in previous studies [50,51,52]. Thirdly, although various potential confounding factors have been adjusted in this study, the possibility of unmeasured confounding factors cannot be entirely eliminated. Finally, integrated analyses between PA parameters (including duration, session and intensity) and other indicators from high-throughput omics, such as metabolomics, microbiomics, proteomics, and so on, are recommended to get in-depth knowledge about the influences of PA on human fitness.
In summary, our findings from the current study highlighted the critical role of PA in combating obesity and controlling LAP. Being regularly active, in comparison with being weekend warriors throughout the week, was associated with significant and favorable LAP reduction. Moreover, engaging in more than 440 min of physical activity per week helped to yield optimal benefits in terms of reducing LAP.
Data availability
Publicly available datasets were analyzed in this study. This data can be accessible at: https://www.cdc.gov/nchs/nhanes/index.htm.
Abbreviations
- BMI:
-
body mass index
- CVD:
-
cardiovascular diseases
- LAP:
-
Lipid accumulation product
- MPA:
-
moderate physical activity
- MVPA:
-
moderate-to-vigorous physical activity
- PA:
-
physical activity
- PIR:
-
poverty income ratio
- RA:
-
regular active
- RCS:
-
restricted cubic spline
- TG:
-
triglycerides
- VPA:
-
vigorous physical activity
- WC:
-
waist circumference
- WWs:
-
weekend warriors
References
G S, G G. Obesity and hypertension. Pharmacol Res. 2017;122.
Obesity Phenotypes. Diabetes, and Cardiovascular Diseases | Circulation Research. https://doi.org/10.1161/CIRCRESAHA.120.316101?url_ver=Z39.882003&_id=ori:rid:crossref.org&_dat=cr_pub%20%200pubmed#. Accessed 28 Sep 2023.
Leikin JB. Foreword: obesity, obesities and gastrointestinal cancers. Dis–Mon DM. 2023;69:101591.
Elagizi A, Kachur S, Carbone S, Lavie CJ, Blair SN. A review of obesity, physical activity, and Cardiovascular Disease. Curr Obes Rep. 2020;9:571–81.
Stefan N, Schulze MB. Metabolic health and cardiometabolic risk clusters: implications for prediction, prevention, and treatment. Lancet Diabetes Endocrinol. 2023;11:426–40.
Karelis A, Brochu M, Rabasa-Lhoret R. Can we identify metabolically healthy but obese individuals (MHO)? Diabetes Metab. 2004;30:569–72.
Zamboni M, Turcato E, Armellini F, Kahn HS, Zivelonghi A, Santana H, et al. Sagittal abdominal diameter as a practical predictor of visceral fat. Int J Obes Relat Metab Disord J Int Assoc Study Obes. 1998;22:655–60.
Kahn HS. The lipid accumulation product performs better than the body mass index for recognizing cardiovascular risk: a population-based comparison. BMC Cardiovasc Disord. 2005;5:26.
Little P, Byrne CD. Abdominal obesity and the hypertriglyceridaemic waist phenotype. BMJ. 2001;322:687–9.
Underwood PM. Cardiovascular risk, the metabolic syndrome and the hypertriglyceridaemic waist. Curr Opin Lipidol. 2004;15:495–7.
Ebrahimi M, Seyedi SA, Nabipoorashrafi SA, Rabizadeh S, Sarzaeim M, Yadegar A, et al. Lipid accumulation product (LAP) index for the diagnosis of nonalcoholic fatty liver disease (NAFLD): a systematic review and meta-analysis. Lipids Health Dis. 2023;22:41.
Milla AMG, Chagas EBF, Miola VFB, Zanuso B, de O, Guiguer EL, Araújo AC, et al. Accuracy of visceral adiposity indices and lipid accumulation products in the identification of adults at high cardiovascular risk. Clínica E Investig En Arterioscler. 2023. https://doi.org/10.1016/j.arteri.2023.04.002
Mehta M, Istfan NW, Apovian CM. Obesity: overview of Weight Management. Endocr Pract. 2021;27:626–35.
Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54:1451–62.
Swift DL, McGee JE, Earnest CP, Carlisle E, Nygard M, Johannsen NM. The effects of Exercise and physical activity on weight loss and maintenance. Prog Cardiovasc Dis. 2018;61:206–13.
Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, et al. The physical activity guidelines for americans. JAMA. 2018;320:2020–8.
O’Donovan G, Sarmiento OL, Hamer M. The rise of the Weekend Warrior. J Orthop Sports Phys Ther. 2018;48:604–6.
O’Donovan G, Lee I-M, Hamer M, Stamatakis E. Association of Weekend Warrior and other Leisure Time physical activity patterns with risks for All-Cause, Cardiovascular Disease, and Cancer Mortality. JAMA Intern Med. 2017;177:335–42.
Zhao F, Wu W, Feng X, Li C, Han D, Guo X, et al. Physical activity levels and diabetes prevalence in US adults: findings from NHANES 2015–2016. Diabetes Ther Res Treat Educ Diabetes Relat Disord. 2020;11:1303–16.
Kehler DS, Theou O. The impact of physical activity and sedentary behaviors on frailty levels. Mech Ageing Dev. 2019;180:29–41.
Hamer M, Biddle SJH, Stamatakis E. Weekend warrior physical activity pattern and common mental disorder: a population wide study of 108,011 British adults. Int J Behav Nutr Phys Act. 2017;14:96.
Liang J, Huang S, Pu Y, Zhao Y, Chen Y, Jiang N, et al. Whether weekend warrior activity and other leisure-time physical activity pattern reduce the risk of depression symptom in the representative adults? A population-based analysis of NHANES 2007–2020. J Affect Disord. 2023;340:329–39.
Jang YS, Joo HJ, Jung YH, Park E-C, Jang S-Y. Association of the Weekend Warrior and other physical activity patterns with metabolic syndrome in the South Korean Population. Int J Environ Res Public Health. 2022;19:13434.
Iranpour S, Sabour S. Inverse association between caffeine intake and depressive symptoms in US adults: data from National Health and Nutrition Examination Survey (NHANES) 2005–2006. Psychiatry Res. 2019;271:732–9.
NHANES - NCHS Research Ethics Review Board Approval. 2022. https://www.cdc.gov/nchs/nhanes/irba98.htm. Accessed 30 Sep 2023.
Curtin LR, Mohadjer LK, Dohrmann SM, Montaquila JM, Kruszan-Moran D, Mirel LB et al. The National Health and Nutrition Examination Survey: Sample Design, 1999–2006. Vital Health Stat 2. 2012;:1–39.
Bawadi H, Abouwatfa M, Alsaeed S, Kerkadi A, Shi Z. Body shape index is a stronger predictor of diabetes. Nutrients. 2019;11:1018.
Carroll MD, Kruszon-Moran D, Tolliver E. Trends in Apolipoprotein B, non-high-density Lipoprotein Cholesterol, and low-density Lipoprotein Cholesterol for adults aged 20 and over, 2005–2016. Natl Health Stat Rep. 2019;:1–16.
Zhang X, Hong F, Liu L, Nie F, Du L, Guan H, et al. Lipid accumulation product is a reliable indicator for identifying metabolic syndrome: the China multi-ethnic cohort (CMEC) study. QJM Mon J Assoc Physicians. 2022;115:140–7.
Chen R, Wang K, Chen Q, Zhang M, Yang H, Zhang M, et al. Weekend warrior physical activity pattern is associated with lower depression risk: findings from NHANES 2007–2018. Gen Hosp Psychiatry. 2023;84:165–71.
Xiao J, Chu M, Shen H, Ren W, Li Z, Hua T, et al. Relationship of weekend warrior and regular physical activity patterns with metabolic syndrome and its associated diseases among Chinese rural adults. J Sports Sci. 2018;36:1963–71.
Batatinha HAP, Rosa Neto JC, Krüger K. Inflammatory features of obesity and smoke exposure and the immunologic effects of exercise. Exerc Immunol Rev. 2019;25:96–111.
Traversy G, Chaput J-P. Alcohol consumption and obesity: an update. Curr Obes Rep. 2015;4:122–30.
Powell-Wiley TM, Poirier CP, Burke VCLE, Després J-P, Gordon-Larsen P, Lavie CJ, et al. Obes Cardiovasc Disease Circulation. 2021;143:e984–1010.
Maggio CA, Pi-Sunyer FX. Obesity and type 2 diabetes. Endocrinol Metab Clin North Am. 2003;32:805–22. viii.
Hu S, Lan T, Wang S, Su L, Zou S, Ye J, et al. Serum chloride level is Associated with Abdominal aortic calcification. Front Cardiovasc Med. 2022;8:800458.
Gui J, Li Y, Liu H, Guo L-L, Li J, Lei Y, et al. Obesity- and lipid-related indices as a predictor of obesity metabolic syndrome in a national cohort study. Front Public Health. 2023;11:1073824.
Liu T, Lu W, Zhao X, Yao T, Song B, Fan H, et al. Relationship between lipid accumulation product and new-onset diabetes in the Japanese population: a retrospective cohort study. Front Endocrinol. 2023;14:1181941.
Chen S, Luo M, Sheng Z, Zhou R, Xiang W, Huang W et al. Association of lipid accumulation product with all-cause and cardiovascular disease mortality: result from NHANES database. Nutr Metab Cardiovasc Dis NMCD. 2023;:S0939-4753(23)00422-2.
Khurshid S, Al-Alusi MA, Churchill TW, Guseh JS, Ellinor PT. Accelerometer-derived Weekend Warrior Physical Activity and Incident Cardiovascular Disease. JAMA. 2023;330:247–52.
Wang K, Xia F, Li Q, Luo X, Wu J. The associations of Weekend Warrior activity patterns with the visceral Adiposity Index in US adults: repeated cross-sectional study. JMIR Public Health Surveill. 2023;9:e41973.
Kokkinos PF, Fernhall B. Physical activity and high density lipoprotein cholesterol levels: what is the relationship? Sports Med Auckl NZ. 1999;28:307–14.
Hashida R, Kawaguchi T, Bekki M, Omoto M, Matsuse H, Nago T, et al. Aerobic vs. resistance exercise in non-alcoholic fatty liver disease: a systematic review. J Hepatol. 2017;66:142–52.
Harmer AR, Elkins MR. Amount and frequency of exercise affect glycaemic control more than exercise mode or intensity. Br J Sports Med. 2015;49:1012–4.
Zhang H, Tong TK, Qiu W, Zhang X, Zhou S, Liu Y, et al. Comparable effects of high-intensity interval training and prolonged continuous Exercise training on Abdominal Visceral Fat reduction in obese Young women. J Diabetes Res. 2017;2017:5071740.
Qiao T, Luo T, Pei H, Yimingniyazi B, Aili D, Aimudula A, et al. Association between abdominal obesity indices and risk of cardiovascular events in Chinese populations with type 2 diabetes: a prospective cohort study. Cardiovasc Diabetol. 2022;21:225.
Ahn N, Baumeister SE, Amann U, Rathmann W, Peters A, Huth C, et al. Visceral adiposity index (VAI), lipid accumulation product (LAP), and product of triglycerides and glucose (TyG) to discriminate prediabetes and diabetes. Sci Rep. 2019;9:9693.
Wang Y, Zhang X, Li Y, Gui J, Mei Y, Yang X, et al. Obesity- and lipid-related indices as a predictor of type 2 diabetes in a national cohort study. Front Endocrinol. 2023;14:1331739.
Montano D. Education differences in cardiometabolic risk in England, Scotland and the United States between 1992 and 2019. BMC Cardiovasc Disord. 2022;22:247.
Schuna JM, Johnson WD, Tudor-Locke C. Adult self-reported and objectively monitored physical activity and sedentary behavior: NHANES 2005–2006. Int J Behav Nutr Phys Act. 2013;10:126.
Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181–8.
Fishman EI, Steeves JA, Zipunnikov V, Koster A, Berrigan D, Harris TA, et al. Association between objectively measured physical activity and mortality in NHANES. Med Sci Sports Exerc. 2016;48:1303–11.
Acknowledgements
We thank all the volunteers for the participation and personnel for their contribution to the NHANES study.
Funding
This study was supported by the outstanding talent pool key support object projects of Army Medical University (Number: XZ-2019-505-021), and the project of Military key clinical specialty (Number: 41561Z23711).
Author information
Authors and Affiliations
Contributions
All the authors have made significant contributions to this study. Fei Luo and Zhao Xie guided the whole research, from research design to data analysis and article writing. Wei Dai, DongYang Zhang and QianKun Yang wrote the main manuscript text for this research article and analysis data. Pan Liu and Chao Zhang helped to review and guide data analysis. Li Zhang and Jie Zhang revised the manuscript. Hao Xue and Jie Zhang provided data analysis advice. Li Zhang and Hao Xue helped in the collection and cleaning of data. Wei Dai, DongYang Zhang, ZhiYuan Wei, Chao Zhang and Zhao Xie were responsible for writing the response letter and making the additional statistical analyses. All authors gave final approval of the version to be published and agreed to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Ethics approval and consent to participant
The program was approved by the National Center for Health Statistics Ethics Review Board. All of the participants provided written informed consent. No additional ethical review board approval was required to analyze the anonymized NHANES data.
Consent for publication
Not applicable.
Competing interests
The authors declared that no potential conflicts of interests existed in this study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dai, W., Zhang, D., Wei, Z. et al. Whether weekend warriors (WWs) achieve equivalent benefits in lipid accumulation products (LAP) reduction as other leisure-time physical activity patterns? -Results from a population-based analysis of NHANES 2007–2018. BMC Public Health 24, 1550 (2024). https://doi.org/10.1186/s12889-024-19070-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19070-z