Abstract
Background
Influenza is a contagious respiratory disease posing a huge burden of disease for children around the world. The purpose of this study was to investigate the epidemiologic changes in childhood influenza in Zhengzhou, China, before, during, and after the COVID-19 outbreak. The aim of this study was to determine the impact of the COVID-19 outbreak and related prevention and control policies on the children’s influenza epidemiological trend.
Methods
All influenza report card data from the Children’s Hospital Affiliated with Zhengzhou University’s Disease Surveillance Reporting Management System were collected and analyzed monthly from January 2018 to December 2023. The period of the study was divided into three phases for comparison: the pre-pandemic period, the pandemic period, and the post-pandemic period.
Results
Between January 2018 and December 2023, a total of 82,030 children with influenza were diagnosed at our hospital, including 46,453 males and 35,577 females. A total of 11,833 of them had to be hospitalized for influenza, and 321 of them were brought to the ICU. Influenza showed low-level epidemiologic status during the COVID-19 pandemic, and there was a substantial rise in influenza and a surge in the number of cases after the COVID-19 pandemic period. The year 2023 will had the most influenza cases (40,785). The peak incidence of influenza changes in 2022, from July to October, and in 2023, from February to April and from October to December. During the post-pandemic period, the proportion of new-borns and young children among influenza patients decreased, while the proportion of school-age children increased significantly, and the proportion of influenza patients hospitalized and the proportion of ICU admissions decreased.
Conclusion
Influenza showed low-level epidemiologic status during the COVID-19 pandemic. In the post-pandemic period, there is a large increase in influenza incidence, with a double peak in influenza incidence. The proportion of school-age children with influenza has also increased. As a result, we recommend that influenza vaccination for key populations, particularly school-age children, be completed by October of each year in Henan Province, and that the government and schools increase education about nonpharmacological influenza prevention approaches.
Similar content being viewed by others
Background
Influenza is a contagious respiratory disease caused by influenza A and influenza B viruses, which are seasonally prevalent each year. Annual influenza epidemics, according to the World Health Organization (WHO), result in 1 billion infections, 3–5 million cases of severe disease, and 300,000–500,000 deaths [1]. China has included the influenza virus in the national catalog of legally recognized infectious diseases as a Category C infectious disease, which are also known as monitoring and management infectious diseases, patients with such infectious diseases, suspected patients and carriers of infectious diseases required to report should be reported online within 24 h after diagnosis. The population is generally susceptible to influenza viruses, and infants, young children, elderly people, and people with chronic illnesses are at high risk of serious illness and death from influenza [2]. Globally, the incidence of influenza in children under 5 years of age is estimated to be 90 million cases per year [3]. In China, the annual influenza incidence rate among children is 20%-30% during the epidemic season, and the annual infection rate can reach 50% during certain high epidemic seasons [2]. Influenza poses an enormous burden of disease for children around the world. The influenza vaccine is the most effective measure for preventing influenza, and the WHO recommends influenza vaccination for high-risk groups such as children, elderly individuals and medical personnel [4]. The influenza vaccine is a nonimmunization program in China, and residents are vaccinated voluntarily [5]. Therefore, understanding the epidemiological trend of influenza in children can provide a scientific foundation for the creation of efficient preventive and control measures, which are extremely important for the management of epidemics, the reduction of influenza morbidity in children, and the prevention and treatment of epidemics.
In December 2019, COVID-19 began a worldwide pandemic, and in January 2020, China initiated a national blockade in response to the outbreak with emergency measures. Since February 2020, the spread of many respiratory viruses, including influenza viruses, has been significantly suppressed (or decreased), and the incidence of influenza has decreased substantially [6,7,8]. Between 2020 and 2022, China adopted dynamic zeroing measures for COVID-19 outbreaks which does not require complete “zero infection”, but for each outbreak that occurs, it is required to contain it within a relatively short period of time, before abandoning its three-year zero new crown policy in December 2022 [9]. Subsequently, China lifted preventative and control measures against COVID-19 as a Category A infectious disease on January 8, 2023, with no additional large-scale interventions beginning in January 2023. With the liberalization of the embargo, the population is experiencing mass infections with SARS-CoV-2 Omicron, while cases of other types of infectious diseases are also increasing [9, 10]. Most of the current studies have focused on the decline in the incidence of a wide range of diseases following the COVID-19 outbreak, with fewer studies on the impact on the incidence of a wide range of diseases following the lifting of control measures for the COVID-19 outbreak. The purpose of this study was to investigate the epidemiologic changes in childhood influenza in Zhengzhou, China, before, during, and after the COVID-19 pandemic; to analyze the impact of the COVID-19 pandemic and related prevention and control policies on the epidemiological trend of childhood influenza; and to provide a theoretical basis for the prevention and control of childhood influenza in the future.
Methods
Data collection
Our hospital is a large tertiary-level A pediatric specialty hospital with 1810 beds, and a nationally designated sentinel hospital for the surveillance of influenza-like illness in children. Tertiary-level A hospitals are the highest level in the “three levels, six grades” classification of hospitals in mainland China, and are hospitals above the regional level that provide high-level specialized medical and healthcare services and perform higher education and scientific research tasks to several regions. We collected all influenza report card data from the Disease Surveillance Reporting Management System of the hospital from January 2018 to December 2023 and analyzed the data on a monthly basis. The throat swab influenza viral nucleic acid test or influenza antigen test were given to all clinically diagnosed cases with influenza symptoms in our hospital. The Influenza Surveillance Reporting Management System counted all cases of clinically diagnosed influenza in the outpatient and inpatient departments of the hospital with one or more of the following positive pathogenicity tests: [1] positive influenza viral nucleic acid test; (2) positive influenza antigen test.
Statistical analysis
According to the changes in the COVID-19 pandemic and preventive and control measures, our study period was divided into three main phases, from January 2018 to January 2020 for the pre-pandemic period, from February 2020 to January 2023 for the pandemic period, and from February 2023 to December 2023 for the post-pandemic period. The epidemiologic characteristics of influenza patients in the three periods were then compared. Excel was utilized for data summary processing, while SPSS 26.0 and Excel were used for data analysis and graphing.
Results
Characteristics of the study subjects
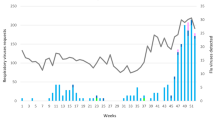
Between January 2018 and December 2023, a total of 82,030 children with influenza were diagnosed at our hospital, including 46,453 males and 35,577 females, and the sex ratio was approximately the same every year, at approximately 1.3:1, with the age ranging from 1 day to 18 years old. Among them, 11,833 children with influenza were in serious condition and required hospitalization, and 321 children were admitted to intensive care units (ICUs) due to critical conditions. The highest number of influenza cases is in 2023 (40,785). (Table 1) Monthly trends in the number of influenza cases over the years are shown in Fig. 1.
Seasonal variation in the number of influenza cases
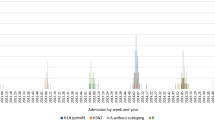
As shown in Fig. 1 and Fig. 2, in the pre-pandemic period, the peak incidence of influenza was mainly concentrated between November and January. During the pandemic period, after the COVID-19 outbreak and the emergence of state control measures, 2020 saw a significant decrease in the number of influenza cases throughout the year, with no significant peak in the number of influenza cases. In 2021, the number of influenza cases began to increase with the relaxation of state controls and peaked from November through January. In 2022, the number of influenza cases will continue to increase, but the peak incidence will occur from July to October. In the post-pandemic period, there was a substantial increase in the number of influenza cases in 2023 and a change in the peak incidence to February-April and October- December.
Changes in the age composition of influenza patients
Based on the growth and development of the children, we stratified the patients according to age and divided them into four groups: infancy (less than or equal to 1 year old), early childhood (2–3 years old), preschool (4–5 years old), and school-age (greater than or equal to 6 years old). As shown in Table 1 and Fig. 3, the trend in the number of children with influenza in different age groups was more or less the same as the overall trend. It is interesting to note, however, that following the COVID-19 pandemic, the age distribution of influenza patients shifted. (Fig. 4) In the pre-pandemic period, the majority of influenza cases were in infants under 1 year old and 2–3 years old, with 23.36% and 28.84%, respectively. After the outbreak, there was a decline in the proportion of infants and young children among influenza cases and a significant increase in the proportion of school-age children (6 years and older), which peaked at 46.60%. The trend in age of influenza hospitalizations was consistent with the overall number of cases. (Fig. 5).
Changes in the proportion of severe and critical influenza cases and deaths
Comparing the pre-pandemic period to the post-pandemic period, we can observe a decrease in the proportion of influenza patients hospitalized and the proportion of ICU admissions. The highest percentage of hospitalized children with influenza was in 2019 (28.91%), and the lowest percentage was in 2023 (9.07%). The proportion of deaths due to influenza did not vary much between the years. (Table 1).
Discussion
Influenza is a seasonal epidemic that occurs every year. The COVID-19 outbreak and the implementation of national control measures have had an impact on the epidemiological trends of a wide range of diseases [11]. Numerous studies have shown a significant decrease in influenza incidence following the COVID-19 pandemic across various regions of the world [8, 12, 13]. This study analyzed the number of influenza cases in the Children’s Hospital Affiliated with Zhengzhou University between January 2018 and December 2023, and the findings revealed a significant decrease in influenza cases in the first pandemic year following the February 2020 COVID-19 pandemic, followed by a modest increase in the second and third pandemic years. After China’s zero-tolerance policy for COVID-19 was fully lifted in January 2023, there was a surge in the number of influenza cases, which is in general agreement with the findings of Liu P et al. in Shanghai, China [10, 14]. Previously, studies have identified variable increases in influenza, respiratory syncytial virus, and enterovirus during the COVID-19 pandemic (2021–2022) as SARS-CoV-2 infections declined and nonpharmacological interventions were relaxed [15]. Our study similarly confirmed this finding and revealed a more severe backlash against the flu virus in 2023.
This phenomenon may be due to a combination of factors. First, during the pandemic, most children were homebound due to public health control measures and had reduced exposure to influenza viruses, which triggered influenza “immune debt” after prolonged minimal exposure to influenza viruses and decreased immunity in the population [16, 17]. Second, annual influenza vaccination is the most effective means of preventing influenza and significantly reduces the risk of influenza and serious complications for those who are vaccinated [18]. However, due to prolonged home control, most children were not vaccinated against influenza during the pandemic, resulting in the loss of vaccine protection. Moreover, after the lifting of the ZERO-COVID policy in China in December 2022, China experienced a mass infection of the population with the Omicron virus, and although the symptoms of the infection in children were relatively mild, the viral infection was detrimental to the overall immunity of the children; as a result, there was a wave of influenza infections that occurred very soon after the wave of Omicron infections. In addition, this may also be related to changes in patients’ medical treatment behavior during the COVID-19 pandemic. Due to lockdown measures and other reasons, some patients with mild influenza may reduce their visits to hospitals.
Our study similarly revealed that not only did the number of influenza cases change but also the seasonal peaks in the number of influenza cases changed equally during and after the pandemic. The peak number of influenza cases in 2022 and 2023 appears to shift forward and backward to varying degrees. In China, influenza A has a winter epidemic pattern in the northern provinces north of 33 degrees north latitude, a single annual peak in spring in the southernmost provinces south of 27 degrees north latitude, and a double-cycle peak in mid-latitude areas every winter and summer [2]. Henan Province is located in northern China, and the peak season for influenza is from November to January each year. However, in 2022, the peak of the number of influenza cases was changed to July to October, and 2023 showed a double peak epidemic trend, from February to April and from October to December. Meanwhile, it is interesting to note that according to the monthly influenza surveillance report from our Disease control department, influenza A and B were co-prevalent during the peak monthly period of October-December 2023, with influenza B accounting for about one-fourth of the overall total. This was similarly found in a study by Boqiang Chen et al. [19]. This is obviously connected to COVID-19 nonintervention measures. Zhengzhou’s prevention and control measures have gradually loosened since June 2022 due to a decrease in SARS-CoV-2 viral infection, and since October 2022, Zhengzhou has taken highly rigorous control measures due to the large-scale transmission of SARS-CoV-2. This finding reaffirms the impact of nondrug interventions on respiratory transmission diseases and reminds us that in addition to promoting vaccination, nondrug interventions are essential for influenza prevention and control. Therefore, we recommend that children complete their influenza vaccination before October each year in order to provide immune protection.
Another important and interesting finding is that the age composition of influenza cases in children changed during and after the pandemic. In this study, we observed an increasing trend in the prevalence of influenza in school-aged and preschool-aged children. We speculate that this phenomenon may be related to the following: 1. School-aged children are more likely to be exposed to influenza viruses after the pandemic due to school attendance, whereas children under 3 years of age are less likely to be out of the house, and caregivers are more attentive to respiratory viral precautions in the later stages of the pandemic than in the pre-pandemic period, with a decreased likelihood of contracting the virus. 2. A greater proportion of school-aged children are likely to have infections in the January 2023 wave of Omicron infections, and these children may be more susceptible to the influenza virus than are uninfected children for a period of time after infection with Omicron. Dynamic observations are still needed regarding how the age composition ratio of childhood influenza patients changes in the future. Based on the above findings, we suggest that school-age children should be more active in completing influenza vaccination. The government and schools should strengthen the promotion of nonpharmacological interventions for the prevention of respiratory viral infections, such as maintaining good personal hygiene, washing hands frequently, avoiding going to crowded places, and avoiding contact with respiratory infections to maintain good respiratory hygiene practices.
In this study, we also found that there was a decrease in the proportion of hospitalized children and ICU admissions among children with influenza admitted to our hospital. During the pandemic, this may be because nonpharmacologic interventions not only reduce the spread of influenza but also reduce the likelihood of severe illness. In the post-pandemic, even we think that children’s immunity to influenza generally declines, but we found that although the number of children with influenza increased, the proportion of children hospitalized with influenza declined. The decrease in the proportion may be attributed to the fact that more parents refused to be hospitalized in the aftermath of the pandemic due to concerns such as cross-infection. Another reason may be that the number of cases soared due to the limited number of beds in hospitals, preventing some of the children who needed to be hospitalized from being admitted to the hospitals. This may also be because after the COVID-19 pandemic, people’s awareness and attention to infectious diseases increased, so treatment of the disease in the early stage was more active, preventing the development of severe disease. However, the current observation period is relatively short, and long-term observation is still needed for future changes in the proportion of severe childhood influenza cases.
In summary, our study revealed that the COVID-19 pandemic and nonpharmacological interventions had dramatic impacts on influenza epidemics in terms of the number of influenza cases, peak, age composition, and proportion of critical illnesses. In the post-pandemic period, there was an outbreak and a forward shift in the peak incidence of influenza cases due to several factors, including immunization debt, which reminds us to pay attention not only to the spread of SARS-CoV-2 after the deregulation of COVID-19 but also to the pandemics of other types of respiratory transmissible diseases.
Our study has some limitations. We examined the medical files from only one hospital. And due to the absence of records in the case system, we do not have access to the immunization coverage of the catchment population and the immunization coverage of the patient population over the study period. However, the number of cases is representative of China’s largest tertiary-level A pediatric specialty hospital and a nationally designated sentinel hospital for the surveillance of influenza-like illness. Our observation of changes in the number of influenza cases in the post-pandemic period was short-lived, and longer monitoring will be needed in the future. Since we did not have access to influenza type information, we analyzed only the overall cases of influenza without grouping them according to the type of influenza virus, but the seasonal epidemics of influenza are mainly dominated by influenza A; therefore, the results of this study are still informative. Meanwhile, according to the 2023 influenza detection report of the Department of Disease Control and Prevention of our hospital, the influenza epidemic in the peak period from February to April of 2023 was dominated by influenza A, and the incidence of influenza B was less. The peak period from October to December in 2023 showed a common epidemic trend of influenza A and influenza B, and influenza B accounted for about 1/4 of the total, which showed an increasing trend compared with February-April.
Conclusion
In conclusion, the epidemiologic pattern of influenza in China changed both during the COVID-19 pandemic and in the latter part of the pandemic. There was a surge in the number of influenza cases in the latter part of the pandemic, along with an earlier peak of influenza onset and an increase in the proportion of school-aged children with influenza. Therefore, we recommend that influenza vaccination for key populations, especially school-age children, be completed by October each year, and that the government and schools increase education on nonpharmacological interventions to prevent influenza.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ICU:
-
Intensive care units
- WHO:
-
World Health Organization
References
Krammer F, Smith GJD, Fouchier RAM, Peiris M, Kedzierska K, Doherty PC, et al. Influenza. Nat Rev Dis Primers. 2018;4(1):3.
Group of Respirology,Chinese Pediatric Society, Chinese Medical Association. China National Clinical Research Center for Respiratory Diseases Group of Respirology CPS, Association CM, Expert consensus on diagnosis and treatment of influenza in children. (2020 Edition). Chin J Appl Clin Pediatrs. 2020;2020(17):1281–8.
Nayak J, Hoy G, Gordon A. Influenza in Children. Cold Spring Harb Perspect Med. 2021;11(1):a038430.
World Health O. Global influenza strategy 2019–2030. Geneva: World Health Organization; 2019. p. 2019.
Prevention CCfDCa. Technical guidelines for seasonal influenza vaccination in China (2022–2023). Chin J Viral Dis. 2023;13(1):1–19.
Sun J, Shi Z, Xu H. Non-pharmaceutical interventions used for COVID-19 had a major impact on reducing influenza in China in 2020. J Travel Med. 2020;27(8):taaa064.
Chen B, Wang M, Huang X, Xie M, Pan L, Liu H, et al. Changes in incidence of notifiable infectious diseases in china under the prevention and control measures of COVID-19. Front Public Health. 2021;9:728768.
Fricke LM, Glöckner S, Dreier M, Lange B. Impact of non-pharmaceutical interventions targeted at COVID-19 pandemic on influenza burden - a systematic review. J Infect. 2021;82(1):1–35.
Ioannidis JPA, Zonta F, Levitt M. What really happened during the massive SARS-CoV-2 omicron wave in China? JAMA Intern Med. 2023;183(7):633–4.
Liu P, Cheng F, Su L, Ye Z, Xu M, Lu L, et al. An outbreak of influenza A in Shanghai after ending the zero-COVID policy in February-March 2023. J Infect. 2023;87(2):e33–5.
Zhao X, Li M, Haihambo N, Jin J, Zeng Y, Qiu J, et al. Changes in temporal properties of notifiable infectious disease epidemics in china during the COVID-19 pandemic: population-based surveillance study. JMIR Public Health Surveill. 2022;8(6):e35343.
Huang QM, Song WQ, Liang F, Ye BL, Li ZH, Zhang XR, et al. Non-pharmaceutical interventions implemented to control the COVID-19 were associated with reduction of influenza incidence. Front Public Health. 2022;10:773271.
Feng L, Zhang T, Wang Q, Xie Y, Peng Z, Zheng J, et al. Impact of COVID-19 outbreaks and interventions on influenza in China and the United States. Nat Commun. 2021;12(1):3249.
Liu P, Xu J. Resurgence of influenza virus activity during COVID-19 pandemic in Shanghai, China. J Infect. 2023;86(1):66–117.
Yang MC, Su YT, Chen PH, Tsai CC, Lin TI, Wu JR. Changing patterns of infectious diseases in children during the COVID-19 pandemic. Front Cell Infect Microbiol. 2023;13:1200617.
Hatter L, Eathorne A, Hills T, Bruce P, Beasley R. Respiratory syncytial virus: paying the immunity debt with interest. Lancet Child Adolesc Health. 2021;5(12):e44–5.
Billard MN, Bont LJ. Quantifying the RSV immunity debt following COVID-19: a public health matter. Lancet Infect Dis. 2023;23(1):3–5.
Tanner AR, Dorey RB, Brendish NJ, Clark TW. Influenza vaccination: protecting the most vulnerable. Eur Respir Rev. 2021;30(159):200258.
Chen B, Zhu Z, Li Q, He D. Resurgence of different influenza types in China and the US in 2021. Math Biosci Eng. 2023;20(4):6327–33.
Acknowledgements
Not Applicable.
Funding
This study was supported by the 2023 Open Subjects of Henan Provincial Engineering Research Center for Diagnosis and Treatment of Pediatric Infections and Critical Illnesses [China] under [grant number ERC202304].
Author information
Authors and Affiliations
Contributions
Wanyu Jia, Xue Zhang and Ruiyang Sun were responsible for the data curation methodology. Xinggang Zhen were responsible for providing the raw data. Wanyu Jia was responsible for writing the original draft. Peng Li, Yu Li, Daobin Wang, Changqing Li and Chunlan Song revised the article critically for important intellectual content. Peng Li, Daobin Wang, Changqing Li and Chunlan Song final approval of the version to be submitted.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not Applicable.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jia, W., Zhang, X., Sun, R. et al. Changes in the epidemiological characteristics of influenza in children in Zhengzhou, China, in the post-COVID-19 era. BMC Public Health 24, 1938 (2024). https://doi.org/10.1186/s12889-024-19460-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19460-3