Abstract
Background
Breast cancer remains a pervasive threat to women worldwide, with increasing incidence rates necessitating effective screening strategies. Timely detection with mammography has emerged as the primary tool for mass screening. This retrospective study, which is part of the Chiraiya Project, aimed to evaluate breast lesion patients identified during opportunistic mammography screening camps in Jammu Province, India.
Methods
A total of 1505 women aged 40 years and older were screened using a mobile mammographic unit over a five-year period, excluding 2020 and 2021 due to the COVID-19 pandemic. The inclusion criterion was women in the specified age group, while the exclusion criterion was women with open breast wounds, history of breast cancer or a history of breast surgery. The screening process involved comprehensive data collection using a detailed Proforma, followed by mammographic assessments conducted within strategically stationed mobile units. Radiological interpretations utilizing the BI-RADS system were performed, accompanied by meticulous documentation of patient demographics, habits, literacy, medical history, and breastfeeding practices. Participants were recruited through collaborations with NGOs, army camps, village panchayats, and urban cooperatives. Screening camps were scheduled periodically, with each camp accommodating 90 patients or fewer.
Results
Among the 1505 patients, most were aged 45–50 years. The number of screenings increased yearly, peaking at 441 in 2022. The BI-RADS II was the most common finding (48.77%), indicating the presence of benign lesions, while the BI-RADS 0 (32.96%) required further evaluation. Higher-risk categories (BI-RADS III, IV, V) were less common, with BI-RADS V being the rarest. Follow-up adherence was highest in the BI-RADS III, IV, and V categories, with BI-RADS V achieving 100% follow-up. However, only 320 of 496 BI-RADS 0 patients were followed up, indicating a gap in continuity of care. The overall follow-up rate was 66.89%. Compared to urban areas, rural areas demonstrated greater screening uptake but lower follow-up rates, highlighting the need for tailored interventions to improve follow-up care access, especially in rural contexts.
Conclusion
This study underscores the efficacy of a mobile mammographic unit in reaching marginalized populations. Adherence to screening protocols has emerged as a linchpin for early detection, improved prognosis, and holistic public health enhancement. Addressing misconceptions surrounding mammographic screenings, especially in rural settings, is crucial. These findings call for intensified efforts in advocacy and education to promote the benefits of breast cancer screening initiatives. Future interventions should prioritize improving access to follow-up care and addressing screening to enhance breast cancer management in Jammu Province.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Breast cancer is the most prevalent malignancy among women, affecting both urban and rural populations, and surpassed lung cancer as the primary global cancer in 2020, with an alarming 2.3 million new cases accounting for 11.7% of all cancer cases [1]. Projections from epidemiological studies indicate a looming global burden of almost 2 million cases by the year 2030 [2]. Within India, there was a substantial 50% increase in the incidence of breast cancer between 1965 and 1985 [3]. Over the last 26 years, the age-standardized incidence rate of breast cancer in females surged by 39.1% from 1990 to 2016, manifesting as an upwards trend in every state across the country [4].
Breast cancer burdens are most common in Jammu Province, which is located in northern India, and breast cancer is the most common malignancy among females, followed by cervical cancer [5]. Recognizing the critical importance of early detection in improving survival rates, comprehensive breast cancer screening initiatives are imperative. Mammography has emerged as the cornerstone of mass screening programs due to its proven efficacy in detecting early-stage breast cancer [6]. However, the widespread lack of awareness about available screening programs contributes to late-stage diagnoses and high mortality rates [7]. A heightened understanding of the significance of early detection plays a pivotal role not only in treatment efficacy but also in the overall management of cancer.
The inception of the ‘Chiraiya’ initiative, symbolizing the graceful bird in Hindi, embodies our profound mission to detect breast cancer in its nascent stages, thereby maximizing benefits for women. Like the nurturing wings of a bird, our mobile mammography unit serves as a beacon of hope, extending aid to those in need. With this transformative vision, our study embarked upon its journey in 2019, driven by the noble pursuit of early detection and unwavering support for women’s health.
Rationale
Breast cancer, a major health concern, requires targeted screening efforts, especially in regions where awareness may be limited. The deployment of a mobile mammographic unit is aimed at overcoming accessibility barriers and reaching populations in both peripheral and urban areas. This study sought to identify individuals with breast lesions, offering insights into the prevalence, distribution, and characteristics of breast cancer cases in Jammu Province. These findings are anticipated to contribute to the development of region-specific strategies for early detection, treatment, and awareness campaigns, ultimately reducing the burden of breast cancer in the studied population.
Aim of the study
The primary aim of this study was to identify and categorize patients with breast lesions within the population screened and recruited from mammography camps in Jammu Province via a mobile mammographic unit strategically designed to reach both peripheral rural and urban populations across diverse regions.
Objectives
-
1.
To employ a mobile mammographic unit for comprehensive breast cancer screening in Jammu Province.
-
2.
To assess and categorize patients with breast lesions based on mammographic findings.
-
3.
To determine the prevalence of breast lesions among the screened population.
-
4.
To analyse the distribution of breast lesions in different regions, rural and urban areas were differentiated.
-
5.
To evaluate the effectiveness of the opportunistic screening program in terms of reach and participation among diverse demographic groups.
-
6.
To contribute data that can inform future interventions, policies, and awareness campaigns for breast cancer in Jammu Province.
Materials and methods
Study design
This retrospective observational study was conducted over five years, from January 2016 to December 2023, excluding the years 2020 and 2021 due to the COVID-19 pandemic. The primary data was collected and analysed. The study utilized a mobile mammographic unit for data collection. All female patients aged 40 years and older attending the screening camps were eligible for inclusion in the study. The exclusion criteria were patients who had open wounds on their breasts, a history of breast cancer or past breast surgery. Participants were recruited through the abovementioned collaborations, ensuring broad community involvement.
Sample size and duration
A total of 1505 patients aged 40 years and older were screened over a 5-year period spanning from 2016 to 2023, excluding the years 2020 and 2021 due to the COVID-19 epidemic. This is an observational data acquired during an opportunistic screening program, where the number of participants (1505) reflects the feasibility of screening within the available resources over the study period. Quantitative variables such as age were categorized into groups (e.g., 40–45 years, 46–50 years) for analysis.
Mobile mammographic unit
The mobile mammographic unit (Fig. 1) utilized in this study was equipped with state-of-the-art mammography equipment, featuring high-resolution digital imaging systems (Figs. 2 and 3) capable of capturing both craniocaudal and mediolateral views of the breasts. The unit was operated by a team of five professionals, comprising a medical officer, a nurse, trained technologists specializing in breast imaging, a driver, and a helper.
Operational logistics
Screening camps were strategically organized in collaboration with various stakeholders, including non-governmental organizations (NGOs), army camps, village panchayats, and urban cooperatives. Information regarding forthcoming screening camps was disseminated 15 days prior through a multichannel approach, including community announcements, posters, and local media outlets. Each screening camp accommodated 90 patients or fewer to ensure personalized attention and an efficient workflow.
Screening process
The screening process commenced with the administration of a structured questionnaire (Questionnaire 1) designed to elicit a specific patient history relevant to breast cancer risk and symptoms. This questionnaire aimed to collect comprehensive personal health information from participants, beginning with basic demographic details such as age, sex, and marital status. Subsequent sections of the questionnaire delved into personal health history, encompassing aspects such as prior cancer diagnoses, occupational exposures, and lifestyle behaviors including caffeine, alcohol, tobacco, and recreational drug use. Furthermore, participants were queried about psychiatric comorbidities, current medications, allergies, past surgeries, and existing medical conditions. A family history of cancer was also documented. Following this, participants were asked about current breast health symptoms, including the presence of lumps, nipple discharge, breast tenderness or pain, redness or swelling, prior breast injuries, and any additional concerns. This comprehensive questionnaire served as a vital tool for assessing breast cancer risk and identifying potential symptoms among participants. The subsequent mammographic examinations were conducted within a mobile unit deployed across diverse locations, facilitated through collaboration with NGOs, army camps, village panchayats, and urban cooperatives.
Mammographic imaging
Mammographic examinations were conducted within the mobile unit by trained technologists under strict quality control measures. Both craniocaudal and mediolateral views were obtained and compiled on a radiographic image reading system. Subsequently, these images were transmitted to a radiologist positioned at the hospital for analysis and categorization using the Breast Imaging Reporting and Data System (BI-RADS). The data presented were primary data collected directly from the population of Jammu Province, including remote peripheral border areas.
Post-mammographic examination questionnaire
Following the mammographic examination, an additional questionnaire (Questionnaire 2) was administered to gather comprehensive information relevant to breast health and medical history. The questionnaire commences by collecting referral details, such as the reason for the checkup and any prior mammograms. The data included obstetric and gynecological history, covering aspects such as hysterectomy, pelvic exams, pregnancy status, menstrual cycle particulars, menopausal status, pregnancies, childbirth history, and breastfeeding practices. Participants were also asked about their hormonal medical history, including the use of birth control pills, hormone replacement therapy, and infertility drugs. Furthermore, the questionnaire addresses breast surgery or treatment history, including breast cysts, needle biopsies, and previous breast cancer diagnoses, along with surgical procedures performed for breast cancer treatment. This comprehensive questionnaire aims to ensure thorough data collection, facilitating detailed patient profiling and nuanced analysis of breast cancer prevalence and risk factors in the studied population. Specific attention was given to information about children and breastfeeding habits to assess potential links to increased risk or prior trauma and discomfort. The questionnaires 1 and 2 used in our study were adapted based on a similar questionnaire available from NorthBay Healthcare [8].
Incentives and outreach strategies
Participants were informed about the screening camps through community outreach efforts, with incentives such as free screening and counselling services provided to encourage participation. Additionally, educational sessions highlighting the importance of early detection and dispelling myths about mammography were conducted to raise awareness and alleviate concerns among participants.
Statistical analysis
Data were analysed using IBM SPSS 21. Descriptive statistics are expressed in terms of percentages and proportions, and continuous data are expressed as the mean and standard deviation. Chi-square tests were used to compare follow-up rates between urban and rural populations.
The study methodology is depicted in Fig. 4 as a flowchart.
Results
Prevalence of breast lesions
A total of 1505 patients underwent screening, revealing diverse mammographic findings categorized according to the Breast Imaging Reporting and Data System (BI-RADS). Figure 5 presents the age-wise distribution of patients who underwent breast cancer screening, with the majority falling within the age range of 45–50 years.
Distribution of BIRADS classifications
Figure 6 illustrates an increasing trend in the number of patients screened each year, reaching a peak of 441 in 2022. The BI-RADS II category consistently had the highest count, indicating that benign findings were the most common outcome of the screenings. Each year, a significant number of patients fell into the BI-RADS 0 category, representing initial inconclusive findings that required further evaluation. The lower counts in BI-RADS III, IV, and V suggested fewer instances of higher suspicion or confirmed malignancies, highlighting the predominance of benign and indeterminate findings and the necessity for efficient follow-up protocols. Table 1 summarizes the overall mammographic findings from the screening program. BI-RADS 0 was 32.96%, showing that many patients needed additional imaging or follow-up. A total of 11.1% of the patients had negative findings according to the BI-RADS I, indicating that a smaller proportion of patients had no detectable abnormalities. The higher-risk categories, including BI-RADS III, IV, and V, had lower percentages, with BI-RADS V being the least common at 0.6%, underscoring the need for stratified follow-up care with increased vigilance for higher-risk patients.
Follow-up rates
Table 2 details the follow-up status of patients based on their initial BI-RADS category, highlighting the adherence to recommended follow-up protocols. Among patients with BI-RADS 0 findings, 320 out of 496 were followed up, although a significant portion (176) were lost to follow-up. This indicates a gap in the continuity of care for patients with initially inconclusive findings. In contrast, high follow-up adherence was observed in patients with higher suspicion categories (BI-RADS III, IV, and V), with BI-RADS V patients achieving a 100% follow-up rate. Overall, 404 out of 604 patients (66.89%) were followed up, while 200 (33.11%) were lost to follow-up. These figures suggest room for improvement in follow-up adherence, particularly for patients with BI-RADS 0 findings, to ensure early detection and intervention for any developing abnormalities.
Patients with BI-RADS 0 who followed up were referred to the appropriate department in our hospital for further management. Of the 53 patients with BI-RADS III, 7 were reclassified as BI-RADS IV, while the remainder were found to have benign conditions. Among the 22 patients with BI-RADS IV, 2 were downgraded to BI-RADS III, with the rest diagnosed as malignant. All 9 patients with BI-RADS V were confirmed to have malignant conditions, as illustrated in the flowchart (Fig. 4).
Regional variations
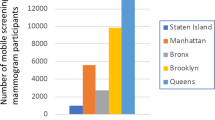
Table 3; and Fig. 7 provides insights into screening and follow-up rates according to region, distinguishing between urban and rural areas. While rural areas had higher screening uptake, urban areas exhibited higher follow-up rates, indicating potential disparities in access to follow-up care between the two regions.
Overall, these tables and figures offer valuable insights into several key aspects of mammographic screening, including the distribution of findings, follow-up rates, and disparities between urban and rural regions. Notably, our study reveals a concerning trend: while urban populations demonstrate greater awareness of breast cancer and greater adherence to follow-up procedures, rural communities lag behind in both aspects. This discrepancy underscores the critical need for targeted interventions aimed at improving access to screening and follow-up care, particularly in rural areas where awareness and healthcare infrastructure may be limited. It is evident that a lack of awareness about the consequences of neglecting follow-up care exists among rural populations, highlighting the importance of education and outreach efforts to enhance understanding and promote proactive management of breast cancer. By addressing these disparities and fostering greater awareness, we can strive to achieve better outcomes in breast cancer detection and management across all communities.
Discussion
The findings of this study shed light on the landscape of breast cancer screening in Jammu Province, India, and provide valuable insights into the prevalence, distribution, and effectiveness of screening efforts. The high prevalence of breast cancer among females in India, as highlighted by previous studies, underscores the urgency of implementing comprehensive screening programs [3,4,5].
The deployment of a mobile mammographic unit emerged as a promising strategy to overcome accessibility barriers and reach both urban and rural populations. This approach represents an opportunistic screening program, aimed at identifying breast lesions in population that may not have accessed regular screening services [9]. This strategy aligns with previous research emphasizing the importance of targeted screening efforts, particularly in regions with limited awareness and resources [7, 10]. The substantial surge in breast cancer incidence observed over the years in Jammu Province emphasizes the critical need for such interventions to address the growing burden of the disease [10, 11].
The findings of this study regarding the distribution of mammographic findings according to the BI-RADS classification system provide valuable insights into the spectrum of lesions encountered during screening. The predominance of benign findings (BI-RADS II) among the screened population is consistent with observations from other regions [7, 12], suggesting the importance of distinguishing between benign and potentially malignant lesions to optimize resource allocation and patient management.
Furthermore, the high proportion of indeterminate findings (BI-RADS 0) necessitating follow-up assessments underscores the complexity of interpreting mammographic results and the importance of comprehensive diagnostic pathways to ensure timely intervention [7, 12]. The high recall rate for follow-up (40%) has a negative impact, potentially causing anxiety and logistical challenges for many women. Strategies to reduce the proportion of women classified as BI-RADS 0, such as enhanced imaging techniques or additional diagnostic tools, should be considered. The disparities observed in follow-up rates between urban and rural regions highlight the need for targeted interventions to improve access to healthcare services, particularly in underserved areas [10, 13]. Facilities in rural areas may not be equivalent to those in urban areas, making it easier for urban women to attend follow-ups and potentially creating a barrier to attendance for rural women.
Monitoring outcomes such as cancers detected and mortality rates is crucial to confirm that the screening program has the anticipated benefit of improving health. By tracking these outcomes, we can assess the effectiveness of screening efforts and make data-driven adjustments to enhance program efficacy. This ongoing monitoring helps ensure that early detection leads to timely treatment, ultimately reducing breast cancer mortality. Without this vital component, it would be challenging to evaluate the true impact of the screening program and justify the resources allocated to such initiatives.
However, several limitations warrant consideration. The exclusion of data from 2020 to 2021 due to the COVID-19 epidemic may have introduced bias and affected the generalizability of the study. Additionally, the reliance on mammography as the sole screening modality may have led to overlooked cases of breast cancer not detectable by this method, emphasizing the need for complementary approaches, such as clinical breast examination and breast self-examination [7, 14].
Despite our efforts to extend outreach to the majority of the rural population in our study, the outcomes were limited by a significant loss of patients during follow-up. This loss can be attributed to various factors, including challenges related to education, awareness, and affordability. Despite our efforts, these barriers hindered the effectiveness of our outreach efforts in rural areas. These findings underscore the urgent need for targeted interventions to address these challenges comprehensively. Enhancing education and awareness campaigns, as well as implementing measures to improve the affordability of healthcare services, are imperative to overcome these obstacles and ensure more comprehensive engagement with rural communities in future healthcare initiatives (6,9). One of the strengths of this study was that it adhered to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines, which ensure comprehensive and transparent reporting of observational studies [15].
The study’s findings contribute significantly to the understanding of breast cancer epidemiology in India, providing valuable data to inform future interventions and policies. Comparing this opportunistic screening intervention with a coordinated national program, where invitation, attendance, follow-up, and diagnosis are systematically recorded for every eligible woman, could offer valuable insights into improving the current approach. By elucidating the prevalence and distribution of breast lesions in Jammu Province, this study lays the groundwork for region-specific strategies aimed at improving early detection, treatment, and patient outcomes.
-
Policies to prioritize breast cancer screening and early detection initiatives should be implemented, especially in high-incidence regions.
-
Allocate resources to support the deployment of mobile mammographic units and other innovative screening methods to effectively reach underserved populations.
-
Comprehensive diagnostic pathways should be introduced to ensure timely follow-up and management of indeterminate mammographic findings.
-
Complementary screening modalities, such as clinical breast examinations and breast self-examinations, should be incorporated to increase detection rates.
-
Conduct longitudinal studies to assess the long-term impact of mobile mammography units on breast cancer outcomes and mortality rates.
-
Investigate the effectiveness of education and awareness campaigns in improving screening uptake and follow-up rates in rural communities.
-
Explore novel approaches to address barriers to healthcare access in underserved areas, including telemedicine and community health worker programs.
Conclusion
This study emphasizes the critical role of targeted screening initiatives in mitigating the impact of breast cancer in Jammu Province. Through the innovative utilization of a mobile mammographic unit, the study showcases the practicality of extending screening services to diverse populations, thereby enhancing the prospects of early detection and intervention. By identifying individuals with breast lesions in their nascent stages, this research sets the stage for future interventions aimed at curtailing the morbidity and mortality rates linked with breast cancer. The incorporation of the ‘Chiraiya’ concept, symbolizing hope and nurturing care, further underscores the compassionate essence of these efforts, reinforcing the commitment to promoting women’s health and well-being.
This study underscores the efficacy of a mobile mammographic unit in reaching marginalized populations. Adherence to screening protocols has emerged as a linchpin for early detection, improved prognosis, and holistic public health enhancement. Addressing misconceptions surrounding mammographic screenings, especially in rural settings, is crucial. Consequently, there is a resounding call for intensified efforts in advocacy and education to elucidate the manifold benefits of breast cancer screening initiatives. The looming threat of cancerous lesions underscores the urgency for comprehensive awareness and education campaigns globally.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- BI-RADS:
-
Breast imaging reporting and data system
- NGO:
-
Non-governmental organization
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and Mortality Worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
DeSantis C, Siegel R, Bandi P, Jemal A. Breast cancer statistics, 2011. CA Cancer J Clin. 2011;61:409–18.
Saxena S, Szabo CI, Chopin S, Barjhoux L, Sinilnikova O, Lenoir G, Goldgar DE, Bhatanager D. BRCA1 and BRCA2 in Indian breast cancer patients. Hum Mutat. 2002;20:473–4.
India State-Level Disease Burden Initiative Cancer Collaborators. The burden of cancers and their variations across the States of India: the global burden of Disease Study 1990–2016. Lancet Oncol. 2018;19:1289–306.
Qurieshi MA, Khan SM, Masoodi MA, Qurieshi U, Ain Q, Jan Y, Haq I, Ahmad SZ. Epidemiology of cancers in Kashmir, India: an Analysis of Hospital Data. Adv Prev Med. 2016;2016:1896761. https://doi.org/10.1155/2016/1896761. PMID: 27478644; PMCID: PMC4949346.
Tabar L, Vitak B, Chen HH, et al. The Swedish two-County Trial twenty years later. Updated mortality results and new insights from long-term follow-up. Radiol Clin North Am. 2000;38:625–51.
Somdatta P, Baridalyne N. Awareness of breast cancer in women of an urban resettlement colony. Indian J Cancer. 2008;45(4):149–53. https://doi.org/10.4103/0019-509X.44662.
Breast Health Questionnaire. https://www.northbay.org/services/upload/Breast-Health-Questionnaire.pdf
The YC, Tan GH, Taib NA, et al. Opportunistic mammography screening provides effective detection rates in a limited resource healthcare system. BMC Cancer. 2015;15:405. https://doi.org/10.1186/s12885-015-1419-2.
Gupta A, Puri I, Gupta M. Patterns of Cancer in males and females in Jammu Region. JK Sci. 2021;23(1):47–51.
Khursheed WA, Thakur N, Sheikh K, Mir UA, Khursheed I. Epidemiological studies on breast Cancer in Kashmir Valley. J Community Med. 2021;4(1):1029.
Latha K, Sulthana A, Valarmathi S, Rathan R. Mapping disease: deciphering geographic patterns of breast cancer risk areas in the western region of Tamil Nadu, India. Int J Sci Res Publ. 2012.
Greater Kashmir. Health: Cancer cases witness a rise in Jammu. https://www.greaterkashmir.com/health/cancer-cases-witness-a-rise-in-jammu
Singh T, Khandelwal N, Singla V, et al. Breast density in screening mammography in Indian population - is it different from western population? Breast J. 2017;00:1–4. https://doi.org/10.1111/tbj.12949.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative. Strengthening the reporting of Observational studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335(7624):806–8. https://doi.org/10.1136/bmj.39335.541782.AD. PMID: 17947786; PMCID: PMC2034723.
Acknowledgements
We would like to express our gratitude to the administration, public relations department, and Radiology department of Shri Mata Vaishno Devi Super Specialty Hospital, Katra, with special acknowledgment to our diligent technicians, whose unwavering support and efforts were instrumental in the success of this project.
Funding
The authors declare that this study received no financial support.
Author information
Authors and Affiliations
Contributions
G.G. helped in designing the study, collecting and analyzing data, led the research process, and ensured adherence to ethical standards, scientific rigor, and methodological integrity. N.J. drafted the manuscript and helped with collecting and analyzing data. R.G. helped with statistics and data analysis.All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board (IRB) of Shri Mata Vaishno Devi Narayana Super Specialty Hospital and adhered to the principles of the Declaration of Helsinki. The IRB granted exemption of written informed consent because of the minimal risk associated with the print reminder and a guarantee of at least usual care for all eligible community members by the local government.
Consent for publication
All authors reviewed the manuscript and consented to its publication without any conflicts of interest.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it.The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Gupta, G., Jamwal, N. & Gupta, R. The Chiraiya project: a retrospective analysis of breast cancer detection gaps addressed via mobile mammography in Jammu Province, India. BMC Public Health 24, 2087 (2024). https://doi.org/10.1186/s12889-024-19622-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19622-3